Sir,
Fluoroquinolone-resistant Pseudomonas aeruginosa is associated with a negative impact on patient outcome,1 and treatment of these organisms can be challenging. Increases in fluoroquinolone-resistant P. aeruginosa have been reported across hospitals and these were related to fluoroquinolone use.2–4 These studies were conducted in periods during which fluoroquinolone use was increasing; more recent data show that their use appears to be stabilizing or decreasing.5
The purpose of this study was to examine recent trends in fluoroquinolone-resistant P. aeruginosa and to determine relationships to fluoroquinolone use in US hospitals. This multi-year cross-sectional study used data from academic medical centres that participated in the University HealthSystem Consortium (UHC). Specifically, UHC member hospitals that subscribed to the Clinical Resource Manager (CRM) database provided drug usage and demographic data. Systemic fluoroquinolones (ciprofloxacin, gatifloxacin, moxifloxacin and levofloxacin) administered to adult patients (age ≥18 years) discharged from 1 January 2002 to 31 December 2009 from 20 hospitals were recorded as days of therapy (DOT) per 1000 patient days (PD). Resistance data (the proportion of ciprofloxacin-resistant isolates) were obtained from the antibiograms that hospitals provided. General linear mixed models were used to assess the significance of changes in antibiotic use and resistance. To assess the relationship between use of individual fluoroquinolones and fluoroquinolone-resistant P. aeruginosa, we used population-averaged longitudinal models, generalized estimating equation (GEE) models, to adjust for correlation among hospitals across time. Quasi-likelihood under the independence model criterion (QIC; an extension of Akaike's information criterion to the GEE method) was used to determine the best distribution and link functions, as well as the working correlation structure. Based on comparison of QIC values, a binomial distribution, logit link and an exchangeable working correlation structure were chosen for this model. We also controlled for the use of other Gram-negative antibacterials (carbapenems, third- and fourth-generation cephalosporins, β-lactam/β-lactamase inhibitor combinations and aminoglycosides). A P value <0.05 was considered significant and all tests were two-tailed. The statistical software used was SAS (version 9.2; SAS Institute, Cary, NC, USA). The Institutional Review Board at Virginia Commonwealth University approved this study.
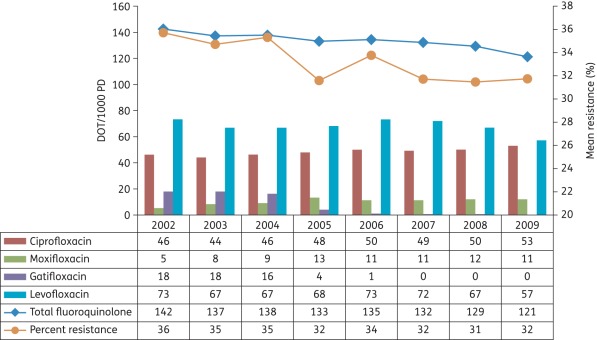
Antibiotic-use data were available from all 20 hospitals for all 8 years. Antibiogram data were available from all 20 hospitals for at least 3 years, while 19 hospitals provided antibiogram data for ≥5 years and 12 provided data for all 8 years. Hospitals were located in all US geographical regions; the average hospital bed capacity was 536. From 2002 to 2009 there was a steady decrease in the mean use of fluoroquinolones: from 142 (SD = 35) to 121 (SD = 43) DOT/1000 PD; the trend was significant (P = 0.04). See Figure 1. Across hospitals, the mean use of levofloxacin decreased, use of moxifloxacin increased, ciprofloxacin use was variable and gatifloxacin use fell to zero when it was withdrawn from the US market. The formulary mix of fluoroquinolones was diverse among hospitals and changed throughout the study period.
Figure 1.
Trends in mean total and individual fluoroquinolone use (DOT/1000 PD) and fluoroquinolone-resistant P. aeruginosa (proportion of resistant isolates) in 20 US academic health centres from 2002 to 2009. The decline in total fluoroquinolone use and the proportion of resistance are statistically significant. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
There was a significant decrease in the mean proportion of fluoroquinolone-resistant P. aeruginosa, from 36% in 2002 to 32% in 2009 (P = 0.01; Figure 1). The GEE model results show that both ciprofloxacin use (coefficient = 0.0030; P = 0.006) and levofloxacin use (coefficient = 0.0028; P < 0.0006) were significantly related to the proportion of ciprofloxacin-resistant P. aeruginosa, while moxifloxacin use (coefficient = 0.0011; P = 0.55) and gatifloxacin use (coefficient = 0.0013, P = 0.55) were not significantly associated.
This hospital-level longitudinal study among a consortium of academic medical centres found several new findings concerning trends in fluoroquinolone use and resistance in P. aeruginosa. First, to the best of our knowledge, this is the only study to report a significant decline in the use of fluoroquinolones across a group of hospitals. Second, there was a significant decrease in the mean proportion of fluoroquinolone-resistant P. aeruginosa. Third, we found that both ciprofloxacin and levofloxacin use, but not that of moxifloxacin or gatifloxacin, was associated with the resistance proportion. One of the main differences in our study is that it reflects data from a more recent time period in which fluoroquinolone use was decreasing and overall resistance of P. aeruginosa to fluoroquinolones was decreasing. Our finding that moxifloxacin use was not related to the proportion of resistance may be related to its lower in vitro activity against P. aeruginosa compared with the other fluoroquinolones lacking a US FDA indication for P. aeruginosa infections. Its use in practice is preferred for the treatment of Gram-positive organisms. Hospitals that used moxifloxacin likely had another fluoroquinolone (e.g. ciprofloxacin) on the drug formulary for use against Gram-negative infections. The lack of association between gatifloxacin use and resistance may be due to its minimal use after 2006.
There are several limitations to this investigation. The relationships between fluoroquinolone use and resistance to P. aeruginosa represent the hospital-level perspective, not that of the patient. Therefore, the results may be subject to ecological bias,6 meaning that findings may not reflect patient-level relationships. Also, we did not account for any infection-control measures that may have influenced the development of fluoroquinolone-resistant P. aeruginosa within hospitals, and nor did we account for community fluoroquinolone use. In conclusion, fluoroquinolone use and fluoroquinolone-resistant P. aeruginosa are decreasing in US academic health centres. Despite the decline in use of fluoroquinolones, it may be prudent to continue to limit the use of these agents as a strategy to decrease the resistance of this important pathogen.
Funding
This work was supported by grant number K08HS018578 from the Agency for Healthcare Research and Quality and award number UL1TR000058 from the National Center for Research Resources and NIH Roadmap for Medical Research, National Institutes of Health (to A. L. P.).
Transparency declarations
A. L. P.: research funding from Cubist Pharmaceuticals for project unrelated to this investigation. R. E. P.: research funding from Cubist, Astellas and Merck for projects unrelated to this investigation. J. A. L., M. A. A., S. E. H. and M. J. O.: none to declare.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the National Center for Research Resources or the National Institutes of Health.
Acknowledgements
Presented in part at the Twenty-seventh International Conference for Pharmacoepidemiology and Therapeutic Risk Management, Chicago, IL, 2011 (Abstract 436).
We thank Sofia Medvedev, PhD, for assistance with data acquisition and compilation, and the persons from participating UHC hospitals that provided antibiogram data.
References
- 1.Hsu DI, Okamoto MP, Murthy R, et al. Fluoroquinolone-resistant Pseudomonas aeruginosa: risk factors for acquisition and impact on outcomes. J Antimicrob Chemother. 2005;55:535–41. doi: 10.1093/jac/dki026. doi:10.1093/jac/dki026. [DOI] [PubMed] [Google Scholar]
- 2.Ray GT, Baxter R, DeLorenze GN. Hospital-level rates of fluoroquinolone use and the risk of hospital-acquired infection with ciprofloxacin-nonsusceptible Pseudomonas aeruginosa. Clin Infect Dis. 2005;41:441–9. doi: 10.1086/431980. doi:10.1086/431980. [DOI] [PubMed] [Google Scholar]
- 3.Zervos MJ, Hershberger E, Nicolau DP, et al. Relationship between fluoroquinolone use and changes in susceptibility to fluoroquinolones of selected pathogens in 10 United States teaching hospitals, 1991–2000. Clin Infect Dis. 2003;37:1643–8. doi: 10.1086/379709. doi:10.1086/379709. [DOI] [PubMed] [Google Scholar]
- 4.Polk RE, Johnson CK, McClish D, et al. Predicting hospitals rates of fluoroquinolone-resistant Pseudomonas aeruginosa use in US hospitals and their surrounding communities. Clin Infect Dis. 2004;39:497–503. doi: 10.1086/422647. doi:10.1086/422647. [DOI] [PubMed] [Google Scholar]
- 5.Pakyz AL, MacDougall C, Oinonen M, et al. Trends in antibacterial use in US academic health centers: 2002 to 2006. Arch Intern Med. 2008;20:2254–60. doi: 10.1001/archinte.168.20.2254. doi:10.1001/archinte.168.20.2254. [DOI] [PubMed] [Google Scholar]
- 6.Harbarth S, Harris AD, Carmeli Y, et al. Parallel analysis of individual and aggregated data on antibiotic exposure and resistance in gram-negative bacilli. Clin Infect Dis. 2001;9:1462–8. doi: 10.1086/322677. doi:10.1086/322677. [DOI] [PubMed] [Google Scholar]