Abstract
This study’s goals were to examine coping strategies of women and their male partners as predictors of change in women’s adjustment over the year following breast cancer treatment and to test whether partners’ coping processes interact to predict adjustment. In a sample of women who had recently completed breast cancer treatment and were taking part in a psychoeducational intervention trial and their partners, patients’ and partners’ cancer-specific coping strategies were assessed at study entry (average of 10 months after diagnosis). Assessed at study entry and 20 months after diagnosis (n = 139 couples), dependent variables were women’s general (i.e., vitality, depressive symptoms, relationship satisfaction) and cancer-specific adjustment (i.e., cancer-specific distress, perceived benefits). Both patients’ and partners’ coping strategies at study entry predicted change in women’s adjustment at 20 months. Women’s use of approach-oriented coping strategies predicted improvement in their vitality and depressive symptoms, men’s use of avoidant coping predicted declining marital satisfaction for wives, and men’s approach-oriented strategies predicted an increase in women’s perception of cancer-related benefits. Patients’ and partners’ coping strategies also interacted to predict adjustment, such that congruent coping strategy use generally predicted better adaptation than did dissimilar coping. Findings highlight the utility of examining patients’ and partners’ coping strategies simultaneously.
Keywords: coping, breast cancer, marital satisfaction, marriage, psychological adjustment
Serious medical conditions typically are not experienced by individuals alone, but rather occur in a relational context. Intimate partners are likely to play vital roles in each other’s well-being (Revenson, 2003; Revenson, Kayser, & Bodenmann, 2005). In a meta-analysis of couples who experienced cancer (Hagedoorn et al., 2008), patients’ and partners’ distress was related significantly (r =.29); women reported more distress than men regardless of their role as patient or partner. Consistent with the recommendation of Hagedoorn et al. (2008) to investigate factors that mediate the impact of cancer on couples, the primary goal of this study was to identify women’s and their husbands’ coping strategies as contributors to women’s adjustment after breast cancer treatment.
In theories of coping with stressors, coping processes can be differentiated on the basis of whether the individual attempts to engage with or avoid the stressor (e.g., Suls & Fletcher, 1985). Approach-oriented coping includes attempts to problem-solve, to understand or express stressor-related emotions (i.e., coping through emotional approach), and other strategies. Avoidance-oriented coping involves cognitive and behavioral attempts to minimize the threat. Consistent with research on other medical threats (e.g., Duangdao & Roesch, 2008; Moskowitz et al., 2009), use of specific approach-oriented coping processes often predicts decreases in distress in cancer patients (e.g., Stanton, Danoff-Burg et al., 2000), whereas coping through avoidance predicts increased distress (e.g., Hack & Degner, 2004; Stanton, Danoff-Burg, & Huggins, 2002).
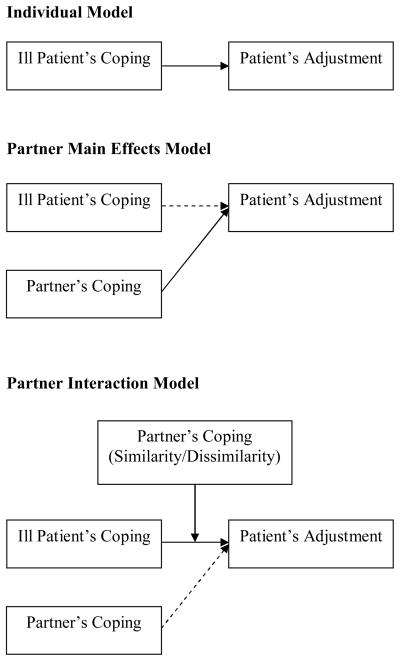
Although intensive attention has been devoted to the effects of individuals’ coping on adjustment to illness, fewer studies have examined the contribution of partners’ coping to patients’ adjustment. Figure 1 depicts three models of coping as predictors of adjustment (Berghuis & Stanton, 2002). An individual model holds that one’s adjustment is shaped primarily by one’s own coping. Even the individual model might be influenced by the relational context, however, in that partners’ unsupportive behaviors can prompt women’s coping with cancer through avoidance, which in turn can contribute to women’s distress (Manne, Ostroff, Winkel, Grana, & Fox, 2005). A partner main effects model suggests that individuals are influenced by their partner’s coping, either alone or along with their own coping. Theoretically, partners’ coping strategies that promote engagement with the stressor should reassure the ill person of the partner’s concern, promote intimacy, and decrease the burden on the affected person as the partner shares in the management of the illness (e.g., Manne & Badr, 2008; Rohrbaugh et al., 2008). For example, women evidence an improvement in distress and an increase in finding benefit in the stressor when their partners use more approach-oriented coping (e.g., problem solving, emotional approach; Berghuis & Stanton, 2002; Manne et al., 2004) and little avoidance coping (e.g., Peterson et al., 2009). In addition, the spouse engaging in “we” talk regarding coping with the patient’s medical problem (Rohrbaugh et al., 2008) predicts improvement in disease-related symptoms and general health in individuals with chronic disease.
Figure 1.
Models of coping as predictors of partners’ adjustment. (Solid lines depict the model’s essential relationships. Dashed lines represent additional potential relationships.)
Few studies have examined the partner interaction model, which posits that the relation of one partner’s coping to adjustment varies as a function of the other partner’s coping, stemming in part from transactional stress and coping theory (e.g. Lazarus & Folkman, 1984; for a review of dyadic coping literature, see Berg & Upchurch, 2007). Some evidence suggests that congruent coping predicts superior adjustment (Revenson, 2003); for example, spouses who are similar in active engagement experience greater marital satisfaction (Badr, 2004; also see Ben-Zur, Gilbar, & 2001). The adaptive value of partners’ similarity on other psychological constructs, such as personality attributes and emotional experience, has also been demonstrated (e.g., Anderson, Keltner, & John, 2003; Gonzaga, Campos, & Bradbury, 2007).
Superior adjustment also might occur when couples are dissimilar in their use of the same strategies, with one partner’s adaptive coping efficiently addressing the problem or compensating for the other’s low use. Complementary use of protective buffering or avoidance coping predicts greater marital satisfaction (Badr, 2004). In infertile couples who had received a negative pregnancy result, husbands’ high use of emotional approach coping compensated for wives’ low use to help ward off depressive symptoms in wives (Berghuis & Stanton, 2002). Theorizing that a dissimilar approach to coping is a more efficient use of couple reserves, Pakenham (1998) found that dissimilar levels of problem-focused coping among couples managing multiple sclerosis was related to better adjustment. Which coping model (i.e., individual, partner main effects, partner interaction) best characterizes predictors of adjustment warrants study.
This study was designed to examine both partners’ coping strategies as predictors of change in women’s adjustment after completion of breast cancer treatment. We investigated whether patients’ and partners’ coping strategies predict patients’ sense of vitality, depressive symptoms, marital satisfaction, cancer-specific distress, and perceived cancer-related benefits. As suggested by stress and coping models (e.g., Revenson, 2003) and past research (e.g., Stanton, Danoff-Burg et al., 2000), we stipulated that patients’ and partners’ approach-oriented coping would independently benefit patients’ adjustment by helping patients deal with long-term threats and bolster their reserves such that recovery of vitality and finding benefit in the experience can occur. Use of avoidant coping by patients and partners was postulated to negatively predict women’s adjustment (e.g., Hack & Degner, 2004), as couples likely are devoting less effort to prevent long-term problems.
We also tested whether partners’ coping processes interact to predict patients’ adjustment, examining the distinct possibilities that women have superior adjustment when spouses engage in either uniformly high levels of approach-oriented forms of coping (i.e., similarity in problem-focused or emotional approach coping) or when they are dissimilar in approach-oriented coping, such that a partner’s high use of emotional approach and problem-focused coping compensate for a spouse’s low use. In addition, we examined the utility of similarity versus dissimilarity in avoidant coping (i.e., composite of coping through behavioral disengagement, mental disengagement, denial) to determine whether it is more important for couples to be uniform in their levels of this generally less-adaptive form of coping, or whether one partner’s low use of such coping may compensate for their partner’s high avoidance.
The present research is a companion study to the Moving Beyond Cancer (MBC) intervention trial to promote women’s transition to breast cancer survivorship (Ganz et al., 2004; Stanton et al., 2005). Women’s and partners’ coping processes during the re-entry phase (i.e., the period following completion of primary medical treatments) can set the stage for positive adjustment over the longer term and serve as targets for psychosocial interventions. We assessed cancer-specific coping strategies in women and their partners at 10 months after diagnosis (Time 1), on average (equivalent to four months after medical treatment completion). Dependent variables, which were identical to the MBC trial outcomes with the addition of marital satisfaction, were assessed at Time 1 and at 20 months after diagnosis (Time 2; analyses of dependent variables completed at 14 months post-diagnosis produced similar findings [data not shown]). Examination of predictors of adjustment over time was a key strength of the study and much called for in this research area (e.g., Berg & Upchurch, 2007). Effects of the randomized MBC intervention arms, as well as the significant interaction obtained in the parent trial between the intervention and women’s perceived preparedness for re-entry (Stanton et al., 2005), were controlled statistically.
Method
Participants
The sample consisted of 139 heterosexual couples within which the women had been treated for nonmetastatic breast cancer and participated in the Moving Beyond Cancer (MBC) psychoeducational intervention trial conducted during the re-entry transition after completion of primary medical treatments (Ganz et al., 2004; Stanton et al., 2005). Of the 558 trial participants, 393 had partners, and 288 (73%) consented to the research staff contacting their partners. Of the 288 partners, 200 (69%) completed the Time 1 assessment. Data from five lesbian couples were excluded because the group was too small to allow for reliable analysis. Data from couples in which the 139 women completed the Time 2 assessment (70% of Time 1 sample) were used in regression analyses. Of the Time 1 demographic, cancer-related, and outcome variables, the 139 women who completed the Time 2 assessment differed from the 56 who did not on one demographic variable, treatment site (χ2 (2) = 9.90, p < .01), with women who participated at Time 2 less likely to be located in Washington, DC. Site was controlled in major analyses.
The average age was 57 years for women and 59 years for men (range = 29 – 88 years). Participants were predominantly white (95%) and well educated (68% of women had a college or more advanced degree). On average, couples had been married for 26 years (SD = 13.7). Most women (68%) had breast-conserving surgery, 32% had mastectomy, 53% had chemotherapy, 69% had radiation, and 55% were taking tamoxifen. Average time between diagnosis and Time 1 for this study was 9.8 months (SD = 3.2). A full sample description is reported elsewhere (Ganz et al., 2004; Low, Stanton, Thompson, Kwan, & Ganz, 2006; Stanton et al., 2005).
Procedure
Oncologists from three sites (Los Angeles, CA; Washington, DC; Kansas City, KS) referred participants. Within four weeks after completion of medical treatments, nonmetastatic breast cancer patients provided informed consent, completed baseline questionnaires, and were randomized to one of three MBC trial arms: standard print information only (National Cancer Institute booklet, “Facing Forward”, 1994); standard information and a video developed for the trial that modeled realistic expectations and effective coping during re-entry; or standard information, the MBC videotape, and a two-session counseling intervention and educational workbook.
At two months post-randomization (approximately 10 months after diagnosis and 4 months after completion of primary medical treatments), research staff requested consent from women to contact partners, and they and consenting partners completed the Time 1 assessments for the study reported here. Partners were sent questionnaires in separate envelopes and asked to complete them independently, without discussion, and return them in separate envelopes. Women completed Time 2 assessments at approximately 20 months after diagnosis.
Measures
Among other measures, breast cancer patients and their partners completed measures of coping at Time 1, and women completed adjustment measures at Times 1 and 2.
Coping processes
Both members of the couple completed items from a widely-used inventory of coping strategies (COPE; Carver, Scheier, & Weintraub, 1989) and the Emotional Approach Coping scales (Stanton et al., 2000) in reference to their experience with their own or their partners’ breast cancer on a response scale of 1 (I don’t do this at all) to 4 (I do this a lot). We used three composite scales that had predicted adjustment in research with cancer patients (e.g., Carver et al., 1993; Low et al., 2006; Stanton, Danoff-Burg et al., 2000; Stanton, Danoff-Burg, & Huggins, 2002): Emotional Approach Coping (16 items; composite of Emotional Expression, Emotional Processing, Seeking Social Support for Instrumental Reasons, Seeking Social Support for Emotional Reason; e.g., “I feel free to express my emotions”, “I get emotional support from others”); Problem-Focused Coping (8 items; composite of Active Coping and Planning subscales, e.g., “I make a plan of action”); and Avoidance-Oriented Coping (12 items; composite of Denial, Mental Disengagement, and Behavioral Disengagement subscales; e.g., “I say to myself ‘this isn’t real’”). Internal consistency estimates ranged from α = .70 to .96.
General adjustment
The 4-item SF-36 Vitality subscale from the Medical Outcomes Study Short Form (SF-36) is a reliable measure of energy (e.g., “feel full of pep”) and fatigue (e.g., “feel worn out”) that is associated with physical and mental health (Ware, 1993). Internal consistency reliability in this study was estimated at α = .89.
The Center for Epidemiologic Studies-Depression Scale (CES-D) is a psychometrically sound 20-item scale (α = .70 in this study) assessing frequency of depressive symptoms over the past week (Radloff, 1977). The 4-point rating scale yields total scores ranging from 0 to 60 with higher scores indicating more depressive symptoms.
The 14-item Revised Dyadic Adjustment Scale (RDAS; Busby, Crane, Larson, & Christensen, 1995) assesses perceived relationship quality. On several Likert-type scales, it measures level of agreement on various relationship issues and frequency with which the couple engages in specific behaviors. Scores range from 0 to 69, with higher scores indicating greater marital satisfaction (α = .90; Busby et al., 1995). The measure has been used in cancer populations (e.g., McLean et al., 2008).
Cancer-specific adjustment
The Revised Impact of Event Scale (IES-R; Horowitz, Wilner, & Alvarez, 1979; Weiss & Marmar, 1997) is a 22-item measure. Participants rated how distressing cancer-specific intrusive thoughts, avoidance, and hyperarousal had been for them over the past week on a 5-point response scale (not at all to extremely; α = .89). Responses were skewed toward lower scores; log-transformed scores were used (log[IES-R + 1]).
The 21-item Posttraumatic Growth Inventory (PTGI; Tedeschi & Calhoun, 1996) assesses perceived positive life changes reported after stressful experiences (e.g., enhanced relationships, greater life appreciation). Participants responded on a scale from 0 (I did NOT experience this change as a result of my experience with cancer) to 5 (I experienced this change to a VERY GREAT degree . . .; α = .96).
Perceived preparedness for re-entry after treatment completion
Discovered to be a significant moderator in the MBC trial (Stanton et al., 2005) and included as a covariate in this study, perceived preparedness for re-entry was assessed at the trial’s baseline with two items: “Overall, I feel very well-prepared for what to expect during my recovery” and “Overall, I feel the medical team has done a great deal to prepare me for what to expect during my recovery from breast cancer treatment.” The highly correlated items (r = .84, p < .0001) were averaged.
Data Analysis
Descriptive statistics and repeated-measures analyses of variance were conducted to assess change on dependent variables. Primary analyses were hierarchical multiple regressions conducted to evaluate the predictive utilities of study entry patient coping strategy, partner coping strategy, and their interaction on the five patient outcomes at Time 2. The Time 1 value on the relevant dependent variable was entered first to evaluate whether coping strategies predicted change in the dependent variables. Covariates included study site, intervention arm, perceived preparation for re-entry, and the intervention × preparedness interaction (Stanton et al., 2005). We identified additional covariates by examining relations between the following demographic and cancer-related variables with patients’ Time 2 dependent variables: patient and partner age, patient education (college or more advanced degree/no college degree), patient and partner ethnicity (European American/other ethnicity), patient and partner employment (at least part-time/not employed), days from surgery to Time 1, chemotherapy (yes/no), radiotherapy (yes/no), surgery (mastectomy/lumpectomy), tamoxifen (yes/no), and years in relationship.
Hierarchical multiple regressions for each dependent variable included the covariates (i.e., Time 1 values on the relevant dependent variable, MBC intervention trial variables, and relevant demographic and medical covariates), one of three patient coping strategies, the identical partner coping strategy, and the patient coping × partner coping interaction. Regression analyses were conducted on all cases available. Scores on the patient and partner coping strategies were centered around the group mean (i.e., each coping strategy score was subtracted from the sample mean). To evaluate significant interactions, we computed the relations between patients’ coping and change in the dependent variable as a function of husbands’ coping score 1 SD above and below the mean, as described by Aiken and West (1991).
Results
Preliminary Analyses
Table 1 displays descriptive statistics. Consistent with other cancer samples (Stanton et al., 2002), approach-oriented coping strategies (i.e., emotional approach coping, problem-focused coping) were frequently used and avoidance coping was rarely used by women and partners. Average SF-36 Vitality was similar to or greater than the general population norm for women aged 55–64 (population M = 58.08; Ware, 1993). Mean CES-D scores were below 16, the cutoff suggestive of clinical depression, and comparable to other cancer patient samples (Hann, Winter, & Jacobsen, 1999). In this sample, 14% of women at Time 1 and 12% at Time 2 scored at or above 16. Mean RDAS scores were above 48 and comparable to nonclinical sample means (Busby et al., 1995); scores below 48 suggest marital distress (Crane, Middleton, & Bean, 2000). Approximately 27% of women scored below 48 across assessments. PTGI scores were comparable to those in other cancer samples (Stanton, Bower, & Low, 2006; Manne et al., 2004), as were cancer-specific adjustment scores (Pitman et al., 2001).
Table 1.
Descriptive Statistics on Major Variables for Breast Cancer Patients and Partners (n = 137–139)
| Variable | Breast Cancer Patients
|
Partners
|
||||
|---|---|---|---|---|---|---|
| Time 1
|
Time 2
|
Time 1
|
||||
| M | SD | M | SD | M | SD | |
| Coping Processes | ||||||
| Avoidance-oriented coping | 1.45 | 0.35 | 1.35 | 0.27 | ||
| Problem-focused coping | 2.80 | 0.77 | 2.48 | 0.77 | ||
| Emotional approach coping | 2.84 | 0.63 | 2.28 | 0.59 | ||
| Dependent Variables | ||||||
| SF-36 Vitality | 57.93 | 20.23 | 62.71 | 19.67 | ||
| CES-D | 8.52 | 8.08 | 7.51 | 6.34 | ||
| Revised Dyadic Adjustment Scale | 50.65 | 7.59 | 51.31 | 6.86 | ||
| Cancer-Specific Adjustment | 0.36 | 0.27 | 0.29 | 0.24 | ||
| Posttraumatic Growth Inventory | 50.60 | 24.38 | 51.55 | 24.63 | ||
Note. CES-D = Center for Epidemiologic Studies-Depression Scale. Cancer-specific adjustment assessed with the Revised Impact of Event Scale (log-transformed scores).
Repeated-measures ANOVAs indicated that, from Time 1 to Time 2, women improved significantly in vitality, F(1, 138) = 9.12, p = .003, and cancer-specific distress, F(1, 137) = 14.43, p < .001. Women’s depressive symptoms F(1, 138) = 2.11, p = .15, marital satisfaction, F(1, 137) = 1.49, p = .23, and cancer-related benefits, F(1, 137) = .59, p = .44, did not change significantly.
As expected, women’s approach-oriented coping processes (i.e., emotional approach, problem-focused coping) were significantly correlated (r = .74, p < .001), as were those of men (r = .68, p < .001). In light of their conceptual distinction, they were examined separately in analyses. Avoidance-oriented coping was uncorrelated or negatively correlated with emotional approach coping (r = −.21, p = .02 for women; r = −.00, p = .97 for men) and with problem-focused coping (r = −.04, p = .61 for women; r = .09, p = .30 for men). Between-partner correlations on identical coping strategies ranged from r = .05 to .08, and none was significant at p < .05. Women’s inter-correlations of absolute values on dependent variables averaged r = .26 at Time 1 and r = .23 at Time 2 (p < .01; Fisher’s r to z transformation).
Regression Analyses
We examined whether coping processes of patients and partners at Time 1, as well as their interactions, predicted patient outcomes at Time 2 (refer to Table 2). With regard to selection of covariates, women reported more depressive symptoms at Time 2 if their partners were not employed. Women reported greater marital satisfaction if they were older, not employed, had European American partners, and had more days since surgery. Patients with European American partners reported more cancer-specific distress. Women reported more cancer-related benefits if they had fewer years in their relationship. These variables were included as covariates in relevant regression analyses. No coping strategy significantly predicted a change in IES-R scores at Time 2, and those findings are not described further.
Table 2.
| SF-36 Vitality | CES-D | RDAS | PTGI | SF-36 Vitality | CES-D | RDAS | PTGI | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Emotional Approach Coping Model | Problem-Focused Coping Model | ||||||||||
| Wife Coping | β | .23 | −.15 | .04 | −.06 | Wife Coping | β | .15 | .00 | .08 | −.03 |
| R2 Δ | 0.05 ** | 0.02 * | 0.00 | 0.00 | R2 Δ | 0.02 * | 0.00 | 0.01 | 0.00 | ||
| Husband Coping | β | −.06 | .01 | .08 | .13 | Husband Coping | β | −.09 | −.09 | .09 | .12 |
| R2 Δ | 0.00 | 0.00 | 0.01 | 0.01 * | R2 Δ | 0.01 | 0.01 | 0.01 | 0.02 * | ||
| Wife Coping x | β | −.05 | .03 | −.15 | .12 | Wife Coping x | β | .08 | −.07 | .01 | .13 |
| Husband Coping | R2 Δ | 0.00 | 0.00 | 0.02 * | 0.01 * | Husband Coping | R2 Δ | 0.01 | 0.00 | 0.00 | 0.02 * |
| Full Model | df | 11, 126 | 12, 125 | 15, 118 | 12, 121 | Full Model | df | 11, 125 | 12, 124 | 14, 120 | 12, 120 |
| F | 8.53 ** | 4.40 ** | 10.52 ** | 16.71 ** | F | 7.48 ** | 4.03 ** | 10.76 ** | 16.72 ** | ||
| Total R2 | 0.43 | 0.30 | 0.57 | 0.62 | Total R2 | 0.40 | 0.28 | 0.56 | 0.63 | ||
| Avoidance-Oriented Coping Model | |||||||||||
| Wife Coping | β | −.02 | .10 | .06 | .04 | ||||||
| R2 Δ | 0.00 | 0.01 | 0.00 | 0.00 | |||||||
| Husband Coping | β | −.06 | .08 | −.15 | .10 | ||||||
| R2 Δ | 0.00 | 0.01 | 0.02 * | 0.01 | |||||||
| Wife Coping x | β | .22 | −.16 | .10 | .09 | ||||||
| Husband Coping | R2 Δ | 0.04 ** | 0.02 * | 0.01 | 0.01 | ||||||
| Full Model | df | 11, 126 | 12, 125 | 14, 121 | 12, 121 | ||||||
| F | 8.24 ** | 4.76 ** | 11.09 ** | 15.89 ** | |||||||
| Total R2 | 0.42 | 0.31 | 0.56 | 0.61 | |||||||
Note. CES-D = Center for Epidemiologic Studies-Depression Scale. RDAS = Revised Dyadic Adjustment Scale. PTGI = Posttraumatic Growth Inventory. The covariates (not included in this table) included Time 1 values on the relevant dependent variable, MBC intervention, perceived preparedness, and intervention × preparedness interactions, study site, and relevant demographic and medical covariates. Standardized betas (β) displayed are for the final regression models.
p < .05.
p < .01.
Hierarchical Multiple Regression Analyses on Breast Cancer Patients’ Dependent Variables
SF-36 Vitality
Women’s greater emotional approach coping (R2Δ = .05, p < .001) and problem-focused coping (R2Δ = .02, p = .05) at Time 1 (10 months after diagnosis) predicted an increase in vitality over the next 10 months. Husbands’ approach-oriented coping did not predict women’s vitality.
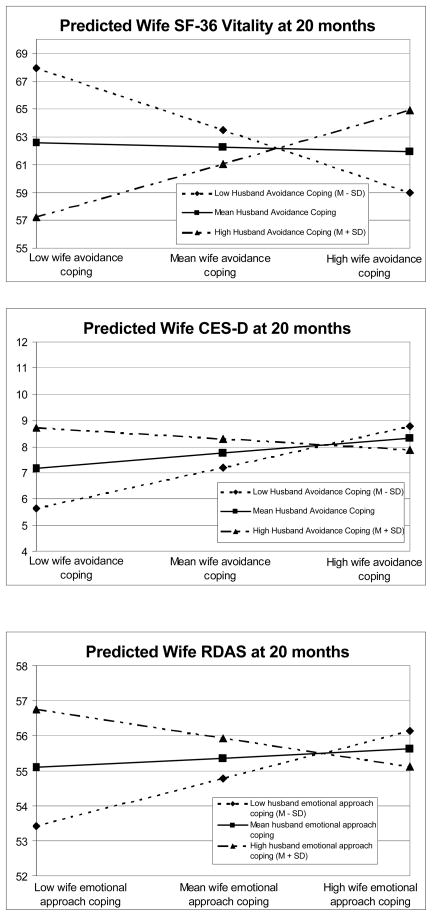
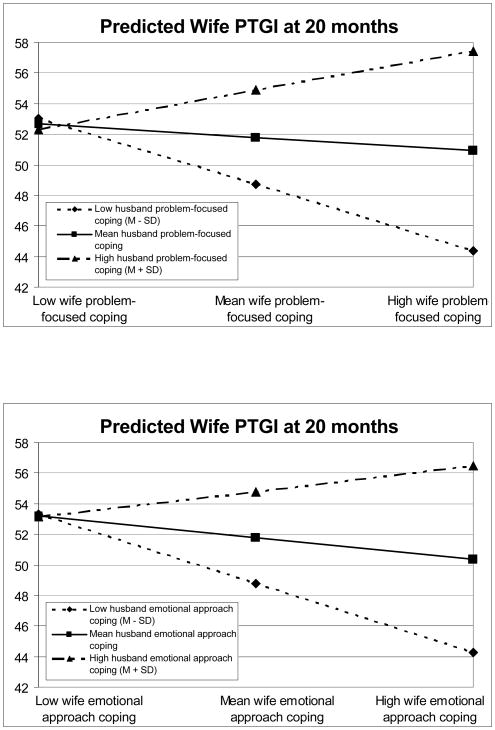
Partners’ avoidant coping interacted to predict change in women’s vitality (F(1, 126) = 9.35, R2Δ = .04, p = .003; refer to Figure 2a). Wives whose husbands exhibited low avoidance coping at Time 1 experienced a significant increase in vitality when they also exhibited low avoidance (p = .02). Indeed, the predicted increase in vitality was greatest when both partners were low in avoidance coping.
Figure 2.
Figure 2a. Interaction of patient avoidance coping with partner avoidance coping on patient SF-36 Vitality at 20 months after diagnosis, controlling for vitality at study entry and other covariates.
Figure 2b. Interaction of patient avoidance coping with partner avoidance coping on patient depressive symptoms (CES-D) at 20 months after diagnosis, controlling for CES-D at study entry and other covariates.
Figure 2c. Interaction of patient emotional approach-oriented coping with partner emotional approach-oriented coping on patient relationship satisfaction (RDAS) at 20 months after diagnosis, controlling for RDAS at study entry and other covariates.
Figure 2d. Interaction of patient problem-focused coping with partner problem-focused coping on cancer-related benefits (PTGI) at 20 months after diagnosis, controlling for PTGI at study entry and other covariates.
Figure 2e. Interaction of patient emotional approach-oriented coping with partner emotional approach-oriented coping on cancer-related benefits (PTGI) at 20 months after diagnosis, controlling for PTGI at study entry and other covariates.
CES-D
Only women’s high coping through emotional approach (R2Δ = .02, p = .049) at Time 1 predicted a decline in depressive symptoms. Patient and partner avoidance coping interacted to predict depressive symptoms (F(1, 125) = 4.12, R2Δ = .02, p = .045; refer to Figure 2b). Wives whose husbands exhibited low avoidance coping at Time 1 experienced a decline in depressive symptoms when they also exhibited low avoidance coping (p = .02). No other coping interaction term was significant.
RDAS
Women’s own coping did not predict marital satisfaction, but their marital satisfaction increased over 10 months when husbands reported low cancer-related avoidance at Time 1 (R2Δ = .02, p = .03). No other main effects were significant. Change in women’s relationship satisfaction also was predicted by the interaction between patient and partner emotional approach coping (F(1, 118) = 5.72, R2Δ = .02, p = .02; refer to Figure 2c). Women low in emotional approach became more satisfied when their husbands reported high emotional approach (p = .01), with the highest expected value for marital satisfaction. Women whose husbands were low in emotional approach became more satisfied when they themselves were high in emotional approach (p = .03). No other coping interaction predicted women’s marital satisfaction.
PTGI
Women’s coping did not predict their own perceived benefit. However, husbands’ high use of problem-focused coping (R2 Δ = .02, p = .03) and emotional approach (R2 Δ = .01, p = .04) (but not avoidance-oriented coping) predicted an increase in women’s perceived benefits related to cancer over 10 months.
These main effects were qualified by significant partner interactions for problem-focused coping (F(1, 120) = 5.24, R2 Δ = .02, p = .02; refer to Figure 2d) and emotional approach coping (F(1, 121) = 4.44, R2 Δ = .01, p = .04; refer to Figure 2e), which assumed the same form. Wives who exhibited more approach-oriented coping experienced more cancer-related benefits when their husbands also exhibited more approach-oriented coping (p = .002 for problem-focused coping and p = .003 for emotional approach coping). Further, wives whose husbands exhibited less approach-oriented coping experienced more cancer-related benefits when they also exhibited less approach-oriented coping (p = .05 for problem focused and p = .03 for emotional approach coping).
Discussion
The current study tested cancer-related coping strategies of women who recently had completed breast cancer treatment and their male partners, as well as between-partner coping interactions, as predictors of women’s change in adjustment over 10 months. Findings support a first observation that no single coping strategy emerged as central to promoting patients’ well-being, and women’s cancer-specific distress (IES-R) was not predicted by any coping strategy. Once medical treatment is complete, experiences that serve as strong reminders of the cancer experience, such as lingering side effects, might be stronger predictors of cancer-specific distress (e.g., Jim, Andrykowski, Munster, & Jacobsen, 2007). For other outcomes, a pattern emerged whereby use of approach-oriented strategies (i.e., coping through emotional approach, problem-focused coping) at Time 1 predicted improved adjustment on specific outcomes. Regarding these main effects of coping, both women’s and their partners’ coping made a difference. Women’s own approach-oriented coping predicted improvements in their vitality and depressive symptoms, whereas their husbands’ approach-oriented coping predicted an increase in women’s perceived cancer-related benefits. Findings suggest that active engagement both by the patient and partner can have salutary effects on patient adjustment. These findings are consistent with research demonstrating the advantages of approach-oriented coping on adjustment to several chronic diseases (e.g., Duangdao & Roesch, 2008; Moskowitz et al., 2009).
Findings also underline the potential of the partner’s coping to influence the patient’s adjustment. That approach-oriented coping by husbands predicted enhanced benefit finding by wives complements research suggesting that actively engaging in the breast cancer experience (Dorval et al., 2005), talking about the marital relationship (Badr, Acitelli, & Taylor, 2008), and the spouse engaging in “we” talk regarding coping with the medical problem of the patient (Rohrbaugh et al., 2008) are associated with improved well-being and health in the couple or patient experiencing chronic disease. In addition, avoidance-oriented coping evidenced one significant direct effect, such that men’s coping through avoidance with their wives’ breast cancer predicted a decline in women’s marital satisfaction 10 months later. Men’s attempts to avoid thoughts, feelings, and perhaps discussion regarding their partners’ cancer might erode the quality of the marital relationship for women.
A partner interaction model also received some support, with interactions predicting four of the five dependent variables. The utility of coping similarity received somewhat more support than did coping dissimilarity. Partners’ similarity in low avoidant coping predicted improvements in both vitality and depressive symptoms over 10 months; that is, low use of cancer-related avoidance by both partners predicted the most favorable outcomes (Figures 2a and 2b). This is consistent with research demonstrating a strong relation between avoidance coping and maladjustment (e.g., Moskowitz et al., 2009) and highlights the particular advantage of both partners engaging in little cancer-related avoidance.
Partners’ similarity in their use of emotional approach and problem-focused coping predicted an increase in women’s cancer-related benefit finding over 10 months; the greatest increase in women’s benefit finding occurred when both partners engaged in approach-oriented coping. Both partners’ active engagement in expressing cancer-related feelings, seeking support, and problem-solving might promote women’s finding benefit in the cancer experience through acknowledgment of women’s strength in confronting the disease, deepened relationships, and behavioral instantiation of women’s deeply held goals.
Partners’ coping dissimilarity predicted adjustment in one instance: women who reported low coping through emotional approach evidenced an improvement in marital satisfaction when their husbands exhibited high approach. Husbands’ high emotional approach appeared to compensate for women’s low use, perhaps because women interpreted husbands’ cancer-related expression as a sign of marital engagement and caring or benefitted from providing support to their husbands. In addition, women with husbands low in emotional approach became more satisfied when they themselves were high in emotional approach. In light of the finding that men are likely to report that their partner serves as their sole confidante (Reis, 1998), women actively involved in expressing cancer-related emotions and seeking support from others, including their husbands, might be more satisfied with their marriages when they do not feel compelled to attend to their husbands’ support seeking or emotional expression.
It is important to consider the limitations of this research. First, in light of the demonstrated importance of gender in adjustment to cancer (e.g., Hagedoorn et al., 2008; Berg & Upchurch, 2007), generalizability of findings to the context of women acting as partners for an ill male partner and to same-sex partners warrants study. Although it is likely that women’s own coping had more influence on their vitality and distress because it more directly shaped the behaviors that influenced their adjustment, it is also possible that women’s coping is the more influential irrespective of which spouse is medically ill, and this question merits further examination. Second, although findings did reveal the importance of considering partners’ use of coping strategies in their influences on women’s adjustment, coping variables were not uniformly significant predictors of outcomes, and single coping strategies or interactions accounted for no more than 5% of the variance in individual dependent variables. Replicability of the findings awaits further research. Third, coping strategies were examined at only one point in time, and the influence of coping at different points or changes in coping is not clear. Further, because coping was assessed with regard to the experience of breast cancer it is possible that each partner was coping with distinct cancer-related stressors. This issue also warrants further study, as does whether coping similarity is itself beneficial to couples or whether it stems from another interpersonal phenomenon, such as couple selection for similarity or mutual socialization. Future research might also add assessment of more relationship-focused coping domains (Revenson, 2003) as well as interactional/observational data to assess coping processes. Finally, this study is potentially limited in generalizability due to its sample of predominantly white and well-educated women with nonmetastatic cancer who were doing well physically and were willing to be randomized to a psychoeducational trial; extension to diverse groups is essential.
In conclusion, this research highlights the importance of examining patients’ and partners’ coping strategies simultaneously. Coping strategies assessed at study entry predicted adjustment over ten months’ time and emerged as significant predictors over and above the influence of the randomized intervention arms and other covariates. Although not without exception, findings generally lend support to the adaptiveness of approach-oriented coping strategies, supporting individual and partner main effects coping models, and partners’ use of congruent coping strategies, supporting a partner interaction coping model, once the acute phase of disease diagnosis and primary treatment is complete. With regard to implications for psychosocial intervention, naturally elected coping strategies can moderate the effects of couple-oriented treatment. Specifically, Manne, Ostroff, and Winkel (2007) demonstrated that women who coped with breast cancer through emotional approach prior to intervention benefitted more from a couples-focused group intervention than those who did not. Accordingly, experimental interventions for couples facing cancer could benefit from examination of couples’ elected coping approaches. Whether instruction in approach-oriented coping strategies and clinical attention to congruence in couples’ coping processes are therapeutically indicated are questions for future investigation.
Acknowledgments
Supported by Public Health Service grant R01-CA63028 (to P. A. Ganz) from the National Cancer Institute, National Institutes of Health, and by California Breast Cancer Research Program grant 5PB-0172 (to B. E. Meyerowitz).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/fam
Contributor Information
Lia M. Kraemer, University of California, Los Angeles
Annette L. Stanton, University of California, Los Angeles
Beth E. Meyerowitz, University of Southern California
Julia H. Rowland, National Cancer Institute
Patricia A. Ganz, University of California, Los Angeles
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Anderson C, Keltner D, John OP. Emotional convergence between people over time. Journal of Personality and Social Psychology. 2003;84:1054–1068. doi: 10.1037/0022-3514.84.5.1054. [DOI] [PubMed] [Google Scholar]
- Badr H. Coping in marital dyads: A contextual perspective on the role of gender and health. Personal Relationships. 2004;11:197–211. doi: 10.1111/j.1475-6811.2004.00078.x. [DOI] [Google Scholar]
- Badr H, Acitelli LK, Carmack Taylor CL. Does talking about their relationship affect couples’ marital and psychological adjustment to lung cancer? Journal of Cancer Survivorship. 2008;2:53–64. doi: 10.1007/s11764-008-0044-3. [DOI] [PubMed] [Google Scholar]
- Ben-Zur H, Gilbar O, Lev S. Coping with breast cancer: Patient, spouse, and dyad models. Psychosomatic Medicine. 2001;63:32–39. doi: 10.1097/00006842-200101000-00004. [DOI] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Berghuis JP, Stanton AL. Adjustment to a dyadic stressor: A longitudinal study of coping and depressive symptoms in infertile couples over an insemination attempt. Journal of Consulting and Clinical Psychology. 2002;70:433–438. doi: 10.1037/0022-006X.70.2.433. [DOI] [PubMed] [Google Scholar]
- Busby DM, Crane DR, Larson JH, Christensen C. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: Construct hierarchy and multidimensional scales. Journal of Marital and Family Therapy. 1995;21:289–308. doi: 10.1111/j.1752-0606.1995.tb00163.x. [DOI] [Google Scholar]
- Carver CS, Pozo C, Harris SD, Noriega V, Scheier MF, Robinson DS, et al. How coping mediates the effect of optimism on distress: A study of women with early stage breast cancer. Journal of Personality and Social Psychology. 1993;65:375–390. doi: 10.1037/0022-3514.65.2.375. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Crane DR, Middleton KC, Bean RA. Establishing criterion scores for the Kansas Marital Satisfaction Scale and the Revised Dyadic Adjustment Scale. American Journal of Family Therapy. 2000;28:53–60. doi: 10.1080/019261800261815. [DOI] [Google Scholar]
- Dorval M, Guay S, Mondor M, Masse B, Falardeau M, Robidoux A, et al. Couples who get closer after breast cancer: frequency and predictors in a prospective investigation. Journal of Clinical Oncology. 2005;23:3588–3596. doi: 10.1200/JCO.2005.01.628. [DOI] [PubMed] [Google Scholar]
- Duangdao KM, Roesch SC. Coping with diabetes in adulthood: A meta-analysis. Journal of Behavioral Medicine. 2008;31:291–300. doi: 10.1007/s10865-008-9155-6. [DOI] [PubMed] [Google Scholar]
- Ganz PA, Kwan L, Stanton AL, et al. Quality of life at the end of primary treatment of breast cancer: First results from the Moving Beyond Cancer randomized trial. Journal of the National Cancer Institute. 2004;96:376–387. doi: 10.1093/jnci/djh060. [DOI] [PubMed] [Google Scholar]
- Gonzaga GC, Campos B, Bradbury T. Similarity, convergence, and relationship satisfaction in dating and married couples. Journal of Personality and Social Psychology. 2007;93:34–48. doi: 10.1037/0022-3514.93.1.34. [DOI] [PubMed] [Google Scholar]
- Hack TF, Degner LF. Coping responses following breast cancer diagnosis predict psychological adjustment three years later. Psycho-Oncology. 2004;13:235–247. doi: 10.1002/pon.739. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) Journal of Psychosomatic Research. 1999;46:437–443. doi: 10.1016/S0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Events Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Jim HS, Andrykowski MA, Munster PN, Jacobsen PB. Physical symptoms/side effects during breast cancer treatment predict posttreatment distress. Annals of Behavioral Medicine. 2007;34:200–208. doi: 10.1007/BF02872674. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Low CA, Stanton AL, Thompson N, Kwan L, Ganz PA. Contextual life stress and coping strategies as predictors of adjustment to breast cancer survivorship. Annals of Behavioral Medicine. 2006;32:235–244. doi: 10.1207/s15324796abm3203_10. [DOI] [PubMed] [Google Scholar]
- Manne S, Badr H. Intimacy and relationship processes in couples’ psychosocial adaptation to cancer. Cancer. 2008;112(11 supplement):2541–2555. doi: 10.1002/cncr.23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Ostroff JS, Winkel G. Social-cognitive processes as moderators of a couple-focused group intervention for women with early stage breast cancer. Health Psychology. 2007;26:735–744. doi: 10.1037/0278-6133.26.6.735. [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Winkel G, Goldstein L, Fox K, Grana G. Posttraumatic growth after breast cancer: Patient, partner, and couple perspectives. Psychosomatic Medicine. 2004;66:442–454. doi: 10.1097/01.psy.0000127689.38525.7d. [DOI] [PubMed] [Google Scholar]
- Manne SL, Ostroff J, Winkel G, Grana G, Fox K. Partner unsupportive responses, avoidant coping, and distress among women with early stage breast cancer: Patient and partner perspectives. Health Psychology. 2005;6:635–641. doi: 10.1037/0278-6133.24.6.635. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT, Hult JR, Bussolari C, Acree M. What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychological Bulletin. 2009;135:121–141. doi: 10.1037/a0014210. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Facing forward: A guide for cancer survivors. Bethesda, MD: National Institutes of Health; 1997. NIH publication 94–2424. [Google Scholar]
- Pakenham KI. Couple coping and adjustment to multiple sclerosis in care receiver-carer dyads. Family Relations. 1998;47:269–277. doi: 10.2307/584977. [DOI] [Google Scholar]
- Peterson BD, Pirritano M, Christensen U, Boivin J, Block J, Schmidt L. The longitudinal impact of partner coping in couples following 5 years of unsuccessful fertility treatments. Human Reproduction. 2009;24:1656–1664. doi: 10.1093/humrep/dep061. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Lanes DM, Williston SK, Guillaume JL, Metzger LJ, Gehr GM, Orr SP. Psychophysiologic assessment of posttraumatic stress disorder in breast cancer patients. Psychosomatics. 2001;42:133–140. doi: 10.1176/appi.psy.42.2.133. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Reis HT. Gender differences in intimacy and related behaviors: Context and process. In: Canary DJ, Dindia K, editors. Sex differences and similarities in communication: Critical essays and empirical investigations of sex and gender in interaction. Mahwah, NJ: Lawrence Erlbaum; 1998. pp. 203–231. [Google Scholar]
- Revenson TA. Scenes from a marriage: Examining support, coping, and gender within the context of chronic illness. In: Suls J, Wallston KA, editors. Social psychological foundations of health and illness. Malden, MA: Blackwell Publishing; 2003. pp. 530–559. [DOI] [Google Scholar]
- Revenson TA, Kayser K, Bodenmann G, editors. Couples coping with stress: Emerging perspectives on dyadic coping. Washington, DC: American Psychological Association; 2005. [DOI] [Google Scholar]
- Rohrbaugh MJ, Mehl MR, Shoham V, Reilly ES, Ewy GA. Prognostic significance of spouse we talk in couples coping with heart failure. Journal of Consulting and Clinical Psychology. 2008;76(5):781–789. doi: 10.1037/a0013238. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Bower JE, Low CA. Posttraumatic growth after cancer. In: Calhoun LG, Tedeschi RG, editors. Handbook of posttraumatic growth: Research and practice. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2006. pp. 138–175. [Google Scholar]
- Stanton AL, Danoff-Burg S, Cameron CL, Bishop MM, Collins CA, Kirk S. Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. Journal of Consulting and Clinical Psychology. 2000;68:875–882. doi: 10.1037/0022-006X.68.5.875. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Ganz PA, Kwan L, Meyerowitz BE, Bower JE, Krupnick JL, Rowland JH, Leedham B, Belin TR. Outcomes from the Moving Beyond Cancer psychoeducational, randomized, controlled trial with breast cancer patients. Journal of Clinical Oncology. 2005;23:6009–6018. doi: 10.1200/JCO.2005.09.101. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Kirk SB, Cameron CL, Danoff-Burg S. Coping through emotional approach: Scale construction and validation. Journal of Personality and Social Psychology. 2000;78:1150–1169. doi: 10.1037/0022-3514.78.6.1150. [DOI] [PubMed] [Google Scholar]
- Suls J, Fletcher B. The relative efficacy of avoidance and nonavoidant coping strategies: A meta-analysis. Health Psychology. 1985;4:249–288. doi: 10.1037/0278-6133.4.3.249. [DOI] [PubMed] [Google Scholar]
- Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9:455–471. doi: 10.1002/jts.2490090305. [DOI] [PubMed] [Google Scholar]
- Ware JE. SF-36 Health Survey: Manual and Interpretation Guide. Boston: New England Medical Center; 1993. [Google Scholar]
- Weiss DS, Marmar CR. The Impact of Event Scale-Revised. In: Wilson J, Keane T, editors. Assessing Psychological Trauma and PTSD. New York, NY: Guilford Press; 1997. pp. 399–411. [Google Scholar]