Abstract
In the latter half of the 20th century, research on behavioral treatments for addictions aimed to develop and test effective treatments. Among treatments found to be at least moderately effective, direct comparisons failed to reveal consistent superiority of one approach over another. This ubiquitous finding held true despite underlying theories that differed markedly in their proposed causal processes related to patient change. In the 21st century the focus of treatment research is increasingly on how treatment works for whom, rather than whether it works. Studies of active treatment ingredients and mechanisms of behavioral change, while promising, have yielded inconsistent results. Simple mediation analysis may need to be expanded by inclusion of models testing for moderated mediation, mediated moderation, and conditional indirect effects. Examples are offered as to how these more complex models can lead to increased understanding of the conditions under which specific treatment interventions will be effective and mechanisms of change operative in improving behavioral treatments for addictions.
Keywords: behavioral treatment, addictions, mechanisms of behavioral change, active ingredients of treatment, mediation analysis, mediated moderation, moderated mediation, conditional indirect effects, clinical trials, causal models, causal chains, model misspecification, treatment outcome studies
Introduction
In 1935 Alcoholics Anonymous was founded partly in response to the absence of professional treatment for alcoholism. It wasn't until much later that the federal government first created the Alcohol, Drug Abuse and Mental Health Administration (ADAMHA) to provide funds for the development and delivery of treatments for addictions and mental health disorders. Federal funding for research on the etiology, prevention, and treatment of addictions increased markedly with the addition of the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the National Institute on Drug Abuse (NIDA) to the National Institutes of Health in 1974. By 1998, 361 alcohol treatment outcome studies had been published, with 79% of them conducted with clinical populations [1]. Increasingly rigorous randomized clinical trials (RCT's) converged on three general conclusions: 1) some treatments were not effective, 2) other treatments were moderately effective, at least in the short term (i.e., significant positive outcomes were reported in 65% of studies on the ten most effective psychosocial treatments; computed from [1], page 272), and 3) among treatments judged to be effective, when directly compared to one another, they often did not differ in their effectiveness [2]. This lack of differential effectiveness was puzzling, and often disappointing, because the theories underlying these treatments were quite distinctive. Therefore, differing theorized causal mechanisms were producing similar outcomes. The implications drawn from this were that 1) different treatment approaches were achieving equivalent results via different pathways or 2) despite theoretical disparities; these different treatments were actually achieving their outcomes via the same pathways [3, 4].
In 1983, Moos and Finney wrote a seminal article “Expanding the Scope of Treatment” [5]. This work identified treatment, as studied at that time, as a “black box” with most characteristics and elements remaining unmeasured. Thus, if a treatment worked, we didn't know why it worked. Similarly, if it was not effective, we didn't know why. Over the subsequent years this void was filled by the development and requirement of treatment manuals. These manuals prescribed the central ingredients of the treatment and how it was to be delivered. If treatments were shown to be differentially effective, it could be inferred that this difference was the result of variability in treatment ingredients [6]. Even though distinctive treatments could now be reliably discriminated from one another, direct comparisons of ‘bona-fide’ interventions continued to produce equivalent outcomes [2]. Equivalent outcomes despite discriminate treatment approaches led to the initiation of research examining this discrepancy. In a 2003 meta-analytic review, Dunn et al. found evidence that Motivational Interviewing (MI) was an effective treatment for addictive behaviors, yet failed to find existing research identifying how MI produced its effects [7]. Subsequently in 2009, Apodaca and Longabaugh conducted a meta-analysis of treatment process studies published through 2007 that attempted to address the core question raised by Dunn. The authors were unable to identify a single study that fully supported the process through which MI was hypothesized to work [8]. Earlier work by Morgenstern and Longabaugh [9] reviewed 11 well controlled studies comparing Cognitive Behavioral Therapy (CBT) with other treatments or no- treatment controls for alcohol dependence. The study found no evidence that theoretically-relevant variables such as coping or self-efficacy accounted for the relationship between CBT and drinking outcome.
In summary, gains were achieved by developing and defining treatments for addiction yet we entered the 21st century with little empirical support for the proposed theories as to how these treatments worked. These conclusions have led to a diminished enthusiasm for conducting further studies that test the efficacy of new behavioral treatments in RCTs and for comparing the relative effectiveness of evidence-based approaches. The focus is shifting toward the study of how treatments work [10]. What are the effective components of specific behavioral interventions, what changes do they affect in patient behaviors, and are there intermediate changes in patients that lead to long term remission in addictive disorders? Such endeavors can refine our interventions theories, but more importantly, can inform treatment optimization in efficacy and efficiency as well as more general best clinical practices with substance using populations.
Mechanisms of Change Research
Lacking knowledge of how behavioral interventions worked was not unique to addictions researchers. A seminal paper by Kazdin and Nock [11] described this absence in behavioral treatment research for child and adolescent psychiatric disorders. The authors also suggested that this was a central problem for psychological treatments more generally, and until significant progress was made, further scientific advances would be limited. The zeitgeist for mechanisms of behavioral change research in the addictions field was facilitated by Request for Application (RFA) initiatives by NIAAA and NIDA. This has set in motion an increasing number of studies focused on mechanisms of behavioral change now making their way into research publications.
While the study of mechanisms of change occurs outside of treatment research as well, we will focus on research conducted in conjunction with clinical outcome studies. We have also found it conceptually useful to distinguish “active ingredients of treatment” from “patient mechanisms of change” [3]. While others [12] have defined these terms somewhat differently, we define mechanisms of changes as behaviors and processes occurring within the patient, either during or outside of treatment that have a causal effect on subsequent changes in addictive behavior. We define treatment ingredients as the entire treatment context including and especially all therapist behaviors that occur. Active treatment ingredients are those treatment elements or therapist behaviors empirically found to positively affect patient mechanisms of change or overall change in addictive behaviors. Treatment ingredients that do not affect patient mechanisms or outcomes are inert ingredients while those found to adversely affect the patient are contra-indicated treatment ingredients.
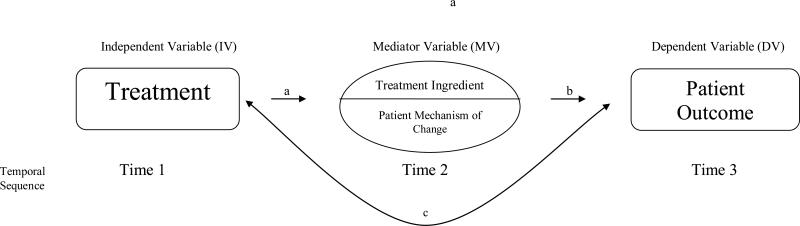
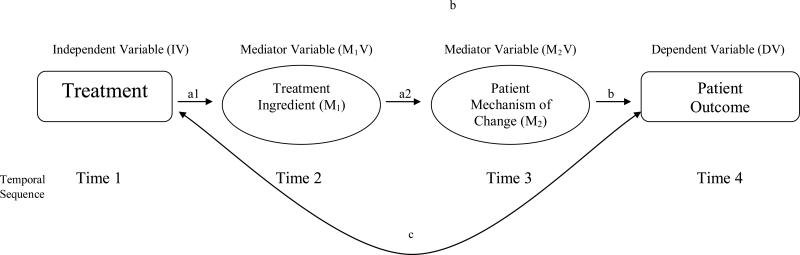
The primary approach for examining treatment ingredients and mechanisms of change has been available for sometime in statistical and modeling methodologies [13, 14], and has been applied extensively in other areas of research on human behavior. Until relatively recently this methodology has been under-utilized in clinical treatment studies. Most generically, it is the study of mediated relationships. The traditional randomized clinical trial is a two variable design where the key question is whether the independent variable, treatment, affects the dependent variable, outcome. In the study of mediated relationships, the number of variables studied expands to three or more. The question becomes whether an intervening variable accounts in whole or in part for the observed relationship between treatment and outcome. The argument for causality is greatly strengthened by temporal precedence of the predictor to the intervening variable, and subsequently, of the intervening variable to the outcome. To show evidence of mediation, the treatment variable must predict the intervening variable (the “a path”), and the intervening variable must predict the outcome variable (the “b path”). (See figure 1a). This latter relation must occur independently of any effect of treatment on outcome (i.e., controlling for treatment). If the combined effect of these two paths (the “ab” path), computed in one of several ways [14], is observed to change the strength of the relationship between the treatment variable and the outcome variable (the “c” path), then it is concluded that the relationship between treatment and outcome is in whole or in part transmitted by the intervening variable. To the extent that the strength of the treatment/outcome relationship is reduced (as opposed to strengthened) when the effects of the b path are partialed out, the intervening variable is judged to be a mediator of the treatment/outcome relationship [14]. As seen in figure 1b, this mediation model can be elongated to include both active treatment ingredients and patient mechanisms of change in the same causal model. This basic model has been expanded to include multiple mediator models, path analysis mediation models, latent variable mediation models, longitudinal mediation models, and moderated mediation models [14].
Figure 1.
In the conceptual model presented in Figure 1a, a prior occurring treatment variable is always the IV. Either (subsequently occurring) treatment variables (treatment ingredients) or patient mechanisms of change are the intervening variables, and subsequently occurring patient outcome is the DV. As can be easily imagined, the model is often elaborated to include as intervening variables both treatment ingredients and patient mechanisms of change, as in Figure 1b. For example, random assignment to treatment modality may be the independent variable that is hypothesized to lead to variability in the ingredients of treatment delivered, which are in turn hypothesized to affect the patient mechanism of change, which in turn is expected to affect the treatment outcome. The necessary condition to be met in this causal chain is that the temporal order of events is preserved. (However, this can be problematic for many treatment process studies, where therapist behaviors and patient behaviors are occurring in sequences where each both precedes and follows the other, compromising the requirement of temporal precedence; ref. 4, Longabaugh, Magill et al).
Results from a Concurrent Review of Behavioral Treatments for Addictions
Using this generic analytic model and some of its more complex variations, a knowledge base regarding active ingredients of treatment and patient mechanisms of change is emerging. Within this literature, there are some behavioral treatments that have made particularly notable strides. We will briefly discuss: Twelve Step and disease oriented treatments, cognitive behavioral therapy, motivational interviewing, and contingency management. In general, the emphasis of this work has been on post-treatment or short-term follow up measures of theory-driven constructs predicted to be affected by treatment and to, in turn, have a positive impact on patient outcome. Perhaps the most long-standing research has been conducted on naturalistic samples of individuals completing community-based disease model treatment and subsequently participating in Alcoholics Anonymous (AA). This work converges on the mediating role of changes in motivation, self-efficacy, coping, and social networks [15]. Interestingly, these are processes theorized as central to other treatments, motivation in motivational interviewing, self-efficacy or coping in cognitive behavioral therapy, and changes in social networks in relational therapies [16]. Recent work has also supported spirituality [17] as a mechanism, which in contrast to those noted above, has a central place within the AA philosophy and model for change. While increased coping has historically gone unsupported as a mechanism distinctive to cognitive behavioral therapy [9], a recent study involving computer-taught coping skills found that the quality of enacted coping skills partially mediated the relationship between treatment condition and outcome [18]. Similarly, coping behaviors have been shown to mediate the differential effect on alcohol use in an individualized compared to standard cognitive behavioral treatment [19]. These two studies provide an example of the level of specificity that may be required to discover mediated treatment effects.
Perhaps the most developed area of research on treatment ingredients and patient mechanisms of change is work conducted on the effects of motivational interviewing, and for treatment ingredients, contingency management. Studies have examined both within-session therapeutic processes and theory-driven post-treatment proximal outcomes. Within-treatment analyses have supported the hypothesis that behaviors of the therapist prescribed by motivational interviewing manuals (active ingredients), such as affirming, emphasizing client control, seeking permission to advise, and emphasizing exploration via use of open-ended questions and complex reflections, predict client language in favor of changing their addictive behavior (e.g., statements of ability, reasons, and commitment to change [20, 21], and that this language often predicts substance use outcome [22, 23]. Therapist behaviors proscribed by motivational interviewing have also shown a relationship with negative client statements [21] and subsequent poorer outcomes [24, 23]. There is also evidence that client change talk, as a mechanism of change, may not be specific to motivational interviewing [25, 26]. Of interest as well is that increased motivation to change, as measured via self-report, has been inconsistently supported as a mechanism of motivational interviewing treatment effects [3, 8]. Only one study to date has fully supported an unconditional model of client change talk partially mediating the relationship between therapist motivational interviewing prescribed behaviors and client outcomes [27]. Therefore, a story is emerging regarding empirical support for, as well as deviations from, the motivational interviewing theory of change. Finally, given its clear behavioral emphasis, contingency management has shown monetary and other contingent reward manipulation to be an active treatment ingredient that predicts abstinence from substance use [28]. A more detailed review of this research can be found in Longabaugh, Magill, Morgenstern and Huebner, in press [3].
While recent evidence for active ingredients of treatment and mechanisms of change is encouraging, the limited number of these studies and patterns of inconsistent results is not. In addition to limiting growth of the knowledge base, use of this knowledge in everyday treatment delivery is thwarted by clinical uncertainty. When is it helpful to implement a particular treatment ingredient? When should the clinician focus on trying to activate a particular mechanism of change? Clinician resistance to using specific empirically-supported treatments is grounded in part by the belief that a particular treatment must be adapted to the needs and characteristics of the patient, as well as the treatment context [29]. Identifying active ingredients of treatment offers guidance to clinicians as to which relational or technical components of the treatment may be most helpful. Information as to which mechanism of change might be particularly effective for a given patient or patient circumstance then aids differential responding to patient needs. Exploring this additional level of complexity is an important next step for mechanisms of change research.
Mediated Moderation, Moderated Mediation and Conditional Indirect Effects (CIE)
Inconsistency in potential mediation effects across studies can be attributed to a number of possible explanations. One likely explanation is that the mediation model tested has been miss-specified because it has been under-specified, i.e., it has failed to differentiate the set of conditions under which mediation will occur as opposed to those conditions in which it will not. In other words, whether or not mediation occurs is conditional upon other variables, as yet unspecified. These variables may reside in the patient, the therapist, the treatment context, variables outside of treatment, or some combination of these.
Project MATCH: A Transitional Step from Main Effect Treatment Outcome Studies to the Study of Conditional Indirect Effects
An important historical step away from unsuccessful attempts to demonstrate outcome differences between empirically-supported treatments was a major effort to identify patient variables that would moderate the effects of treatments on outcome. A number of studies showed promise for patient-to-treatment matching in relation to differential treatment effects [30], and NIAAA subsequently initiated Project MATCH, a multi-site study of three distinctive treatments for alcohol use disorders [31]. This study, the largest psychosocial RCT undertaken to date, tested hypotheses that different kinds of patients would differentially respond to one or more of three treatments: Motivational Enhancement Therapy (MET), Cognitive Behavioral Therapy, and Twelve Step Facilitation (TSF). Despite the rigorous development of 21 a priori patient/treatment matching hypotheses, little support was found for the hypothesized matching effects on primary drinking outcomes [32, 33]. Treatment moderator hypotheses do not require specification of the mechanisms through which the moderating effect occurs. Rather, they remain tests of the c path, where the treatment variable is now an interaction term. Project MATCH, however, required that each matching hypothesis have a testable causal chain to examine the underlying processes through which the prediction went supported or unsupported [34]. As the intention was to test for mediators of hypothesized moderator effects, these analyses can be considered tests of mediated moderation [35]. Mediated moderation identifies one or more intervening variables that, through the ab path, affect the strength of the c path (i.e., the treatment by moderator interaction to treatment outcome relationship). A comprehensive review of the Project MATCH causal model results concluded that the theories underlying them were either under-developed and/or inadequately measured and therefore considerably at variance with what was empirically observed. While relationships of the mediator to post treatment outcome (the b path) were generally supported, the predicted relationships of the treatment/moderator interaction variable to the mediator variable were rarely supported [36].
Of the four matching hypotheses supported, mediated moderation analyses also supported two of the hypothesized causal chains, with a third supported in a subsequent secondary process analysis. Cooney et al. demonstrated that TSF patients who were more highly alcohol dependent had better drinking outcomes than CBT patients (the c path) because of TSF therapists’ emphasis on abstinence (the mediating active treatment ingredient). Conversely, CBT patients who were less alcohol dependent had better drinking outcomes than TSF patients because of a lack of emphasis on abstinence [37]. A clinician could take from these findings that for a patient with high dependence, the abstinence message could enhance drinking outcomes whereas for those with low dependence, emphasis on abstinence could be counterproductive. This example shows that therapist emphasis on abstinence as a mediator of the relationship between treatment modality (TSF vs. CBT) and drinking outcome is conditional upon a fourth variable, patient alcohol dependence. Longabaugh et al. [38] found that TSF improved the drinking outcomes of patients with social networks supportive of drinking more than MET, but not for patients with social networks unsupportive of drinking (the c path). Mediated moderation analysis revealed that part of this effect was attributable to more TSF than MET patients attending AA (the a path), and that AA involvement and attendance (the mechanism of change) improved the drinking outcomes of patients with social networks supportive of drinking, but not for those with social networks already supportive of abstinence (the b path). Again, the effect of the mediator, AA involvement, was conditional upon a fourth variable, pretreatment network support of patient drinking. The implication for the clinician is that it is especially important to get the patient with a network supportive of drinking to AA. In contrast, for patients with networks already highly supportive of abstinence prior to treatment, referral to a mutual help group such as AA may have no incremental treatment benefit. Finally, Karno and Longabaugh [39] in a post hoc process analysis identified in part why high anger patients who received MET had better drinking outcomes than comparable patients receiving CBT whereas those low in anger tended to have better outcomes in CBT compared to MET (the c path). Analyses showed that CBT had a more highly structured therapeutic approach than did MET (the a path), and that high and low anger patients differentially responded to structure. Specifically, high anger patients had worse drinking outcomes with high structure and low anger patients tended to have better drinking outcomes with high structure (the b path). Thus, the effect of the mediator, amount of structure in therapy, on drinking outcome was partly conditional upon a fourth variable, patient trait anger. The suggestion for the clinician is to tailor the amount of structure used in therapy, whether it be CBT or MET, to the assessed trait anger of the patient.
In the above three examples, tests of differences between the two treatments would not have demonstrated differential effects. Because the a priori hypotheses were based on predictions of moderated treatment effects, none would be expected. What was hypothesized, a relationship between the interaction of treatment modality with a patient variable and outcome (a treatment moderator hypothesis) was supported but how this effect was transmitted was unknown. Through mediated moderation analyses, mediators of these moderated effects were identified (two therapy variables, emphasis on abstinence and therapy structure and one extra-treatment variable, AA involvement).
Moderated Mediation and Mediated Moderation as Conditional Indirect Effects
Baron and Kenny's seminal publication [13] defined moderation and mediation, but only briefly focused on how the two analytic procedures could be combined. Only relatively recently was it made clear [35] that in most instances mediated moderation and moderated mediation were equivalent, different sides of the same coin. The primary differentiation was in the analytic sequence and interpretations. While tests of mediated moderation are conducted to establish mediators of the moderator effect, tests of moderated mediation are conducted to determine whether mediation is conditional upon a moderator variable. In effect, moderated mediation and prototypic mediated moderation are specific derivations from a more comprehensive analytic framework, which Preacher et al. have described and defined as conditional indirect effects [40]. Conditional indirect effects (CIE's) are mediated relationships where the existence or strength of the mediated effect is conditional upon the influence of one or more other variables. CIE models specify more clearly and comprehensively the ways in which mediation (the indirect effect) may be conditional upon these other variables. The CIE models to be tested can be differentiated on the basis of the number of moderating variables involved and the paths affected [40]. This comprehensive analytic approach enumerates the complexity of relationships necessary to address researcher and clinician questions as to the circumstances and kinds of patients for which attention to a given mechanism is appropriate. For example, Witkiewitz et al. [41] combined several analytic procedures to establish conditional indirect effects, using data from Project COMBINE [42], a large and rigorous NIAAA multi-site study of multiple pharmacological and behavioral treatments for alcohol use disorders. Starting with the knowledge that negative mood is a precipitant of relapse [43], they established a strong correlation between changes in negative mood and changes in heavy drinking during treatment. They further showed that patients reduced their craving after receiving a treatment module targeting reduced craving and subsequently had fewer heavy drinking days during and following treatment (a mediated effect). Specifically, the authors hypothesized and found that the material covered in the craving module (monitoring urges, urge avoidance/distraction and urge-surfing) allowed patients to experience negative mood without subsequent increases in craving, which then predicted a lower frequency of drinking in response to negative mood (moderation of the a and b paths). For the clinical researcher, the take away knowledge is that craving was a mediator of the relationship between negative mood and frequency of heavy drinking, but the relationship between negative mood and craving was reduced for patients receiving the craving module. The implication for the clinician is use of this craving module should reduce post treatment heavy drinking by decreasing patient cravings associated with negative mood.
Preacher et al differentiate CIE's on the basis of which paths, a or b or both, are conditional upon other variables. In the work of Witkiewitz and colleagues [41], the conditional variable affected both the a and b paths. Karno et al. [25] provide an example of a CIE model where only the a path is conditional on another variable. Here the researchers found that increased patient speech regarding taking steps to maintain their abstinence (the mediator variable) was predictive of post treatment drinking (the b path). However, the relationship between the predictor, amount of structure in therapy across three different treatment conditions, and the mediator (the a path), taking steps, was conditional upon whether the patient was high or low in trait reactance (the conditional variable). For patients low in reactance, high structure predicted taking steps statements; for patients high in reactance, low structure tended to predict taking steps. This result can be directly applied by clinicians to help determine the amount of structure they should incorporate into their therapy with low and high reactant patients.
We use a hypothetical example to illustrate how the mediator model might be conditional upon a fourth variable affecting the b rather than the a path, with other clinical implications. In the above example, taking steps (conditionally) mediated the relationship between therapy structure and drinking outcomes (the c path), and taking steps was an unconditional predictor of drinking outcome (the b path). However, it is quite conceivable that instead of the relationship between therapy structure and patient talk of taking steps being conditional on another variable, the relationship between taking steps and drinking outcome (the b path) might be conditional upon another variable. For example, one hypothesis is that the relationship between discussion of taking behavioral steps and drinking outcome (the b path) is conditional upon the patient's capacity to self regulate. Specifically, for patients with high self regulation, talk about taking steps would be predictive of good drinking outcomes, but for patients with low self-regulation, taking steps during treatment would be unrelated to drinking outcomes. In this example, taking steps would mediate the relationship of therapy structure to drinking outcomes for high self regulators but not for low self regulators. Here the implication for the clinician could well be that while taking steps during treatment may be necessary, depending on the patient's capacity to self regulate, it might not be sufficient, and that some other or further intervention would be required for these low self regulators.
Preacher and colleagues have now developed the software for directly testing these and other CIE models they describe [44]. Given the availability of these (SAS and SPSS) software programs and the clarity of model specificity required to test conditional indirect effects, it is likely that discovery of the conditions under which an ingredient of treatment or a mechanism of change will be activated will become much clearer, reducing the inconsistencies of findings in mechanisms of change research. At our present state of knowledge it is extremely unlikely that we will establish mechanisms of change that will apply to all treatment/outcome relationships. Rather, we are more likely to discover how treatment works when we are able to determine the variables upon which mediation is conditional. The capacity to test CIE's gives the clinical researcher the opportunity to conceptualize and test fully specified models of treatment effectiveness.
Conclusion
The paradigmatic shift from studies on the effectiveness of treatment to identification of active treatment ingredients and mechanisms of change is an important sea change, necessary both for the advancement of the science of addictions treatment and for improving the efficacy and effectiveness of treatment. However, until the study of mechanisms progresses to systematic consideration of the conditions under which intervening variables produce their effects, mechanisms of change research will not achieve the promise inherent in its potential. The development of more sophisticated models for testing fully developed theory provides an opportunity for doing so.
References
Papers of particular interest, published recently, have been highlighted as: * Of importance
- 1.Miller WR, Wilbourne PL. Mesa Grande: A methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- 2.Wampold BE. The great psychotherapy debate: models, methods, and findings. Lawrence Erlbaum Associates; Mahwah, N.J.: 2001. [Google Scholar]
- 3.Longabaugh R, Magill M, Morgenstern J, Huebner R. Mechanisms of Behavior Change. In: McCrady BS, Esptein EE, editors. Addictions: A Comprehensive Guidebook. Oxford University Press; In Press. [Google Scholar]
- 4.Longabaugh R. The search for mechanisms of change in behavioral treatments for alcohol use disorders: A commentary. Alcohol Clin Exp Res. 2007;31:21S–32S. doi: 10.1111/j.1530-0277.2007.00490.x. [DOI] [PubMed] [Google Scholar]
- 5.Moos RH, Finney JW. Expanding the scope of alcoholism treatment. Am Psychol. 1983;38(10):1036–1044. doi: 10.1037//0003-066x.38.10.1036. [DOI] [PubMed] [Google Scholar]
- 6.Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psych. 1998;66(1):7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- 7.Dunn C, DeRoo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001;96(12):1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- 8.Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2009;104(5):705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morgenstern J, Longabaugh R. Cognitive-behavioral treatment for alcohol dependence: A review of evidence for its hypothesized mechanisms of action. Addiction. 2000;95(10):1475–1490. doi: 10.1046/j.1360-0443.2000.951014753.x. [DOI] [PubMed] [Google Scholar]
- 10.Huebner RB, Tonigan JS. The search for mechanisms of behavior change in evidence-based behavioral treatments for alcohol use disorders: Overview. Alcohol Clin Exp Res. 2007;31(S3):1S–3S. doi: 10.1111/j.1530-0277.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- 11.Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendation. J Child Psychol Psyc. 2003;44(8):1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- 12.Nock MK. Conceptual and design essentials for evaluating mechanisms of change. Alcohol Clin Exp Res. 2007;31(S3):4S–12S. doi: 10.1111/j.1530-0277.2007.00488.x. [DOI] [PubMed] [Google Scholar]
- 13.Baron RM, Kenney DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 14*.MacKinnon DP. Introduction to Statistical Mediation Analysis. Lawrence Erlbaum Associates; NY: 2008. [Google Scholar]
- 15.Kelly JF, Magill M, Stout RL. How do people recover from alcohol dependence? A systematic review of the research on mechanisms of behavior change in Alcoholics Anonymous. Addict Res Theory. 2009;17(3):236–259. [Google Scholar]
- 16.Longabaugh R. Involvement of support networks in treatment. In: Galanter, editor. Recent Developments in Alcoholism, Volume 16: Research on alcoholism treatment. Plenum Publishers; New York: 2003. pp. 133–147. [DOI] [PubMed] [Google Scholar]
- 17.Kelly JF. Spirituality in Recovery: A Lagged Mediational Analysis of Alcoholics Anonymous’ Principal Theoretical Mechanism of Behavior Change. Alcohol Clin Exp Res. 2011;35(3):454–463. doi: 10.1111/j.1530-0277.2010.01362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kiluk BD, Nich C, Babuscio T, et al. Quality versus quantity: acquisition of coping skills following computerized cognitive–behavioral therapy for substance use disorders. Addiction. 2010 doi: 10.1111/j.1360-0443.2010.03076.x. advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Litt MD, Kadden RM, Kabela-Cormier E, et al. Coping skills training and contingency management treatments for marijuana dependence: Exploring mechanisms of behavior change. Addiction. 2009;103:638–648. doi: 10.1111/j.1360-0443.2008.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaume J, Gmel G, Faouzi M, et al. Counsellor behaviours and patient language during brief motivational interventions: A sequential analysis of speech. Addiction. 2008;103(11):1793–1800. doi: 10.1111/j.1360-0443.2008.02337.x. [DOI] [PubMed] [Google Scholar]
- 21.Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions. J Subst Abuse Treat. 2006;30(3):245–251. doi: 10.1016/j.jsat.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Amrhein PC, Miller WR, Yahne CE, et al. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psych. 2003;71(5):862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- 23.Vader AM, Walters ST, Prabhu GC, et al. The language of motivational interviewing and feedback: Counselor language, client language, and client drinking outcomes. Psychol Addict Behav. 2010;24(2):190–197. doi: 10.1037/a0018749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baer JS, Beadnell B, Garrett S, et al. Adolescent change language within a brief motivational intervention and substance use outcomes. Psychol Addict Behav. 2008;22(4):570–575. doi: 10.1037/a0013022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25*.Karno MP, Longabaugh R, Herbeck D. What explains the relationship between the therapist structure × patient reactance interaction and drinking outcome? An examination of potential mediators. Psychol Addict Behav. 2010 doi: 10.1037/a0020526. advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moyers TB, Martin T, Christopher PJ, et al. Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcohol Clin Exp Res. 2007;31(S3):40S–47S. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- 27*.Moyers TB, Martin T, Houck JM, et al. From in-session behaviors to drinking outcomes: A causal chain for motivational interviewing. J Consult Clin Psych. 2009;77(6):1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higgins ST, Wong CJ, Badger JG, et al. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. J Consult Clin Psych. 2000;68:64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- 29.Beutler LE, Williams RE, Wakefield PJ, et al. Bridging scientist and practitioner perspectives in clinical psychology. Am Psychol. 1995;50(12):984–994. doi: 10.1037//0003-066x.50.12.984. [DOI] [PubMed] [Google Scholar]
- 30.Mattson ME, Allen JP, Longabaugh R, et al. A chronological review of empirical studies matching alcoholic clients to treatment. J Stud Alcohol. 1994;S12:16–29. doi: 10.15288/jsas.1994.s12.16. [DOI] [PubMed] [Google Scholar]
- 31.Project MATCH Research Group Alcoholism treatment matching research: Methodological and clinical approaches. J Stud Alcohol. 1994;(Supplement 12) [PubMed] [Google Scholar]
- 32.Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project MATCH three year drinking outcomes. Alcohol Clin Exp Res. 1998;22(6):1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- 33.Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Treatment main effects and matching effects on drinking during treatment. J Stud Alcohol. 1998;59(6):631–639. doi: 10.15288/jsa.1998.59.631. [DOI] [PubMed] [Google Scholar]
- 34.Project MATCH Hypotheses . In: Results and Causal Chain Analyses. Longabaugh R, Wirtz PW, editors. Vol. 8. Government Printing Office; Washington, DC: 2001. NIAAA Project MATCH Monograph Series. Publication No. (ADM) 01-4238) [Google Scholar]
- 35.Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. J Pers Soc Psychol. 2005;89(6):852–863. doi: 10.1037/0022-3514.89.6.852. [DOI] [PubMed] [Google Scholar]
- 36.Longabaugh R, Wirtz PW. Substantive Review and Critique. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and Causal Chain Analyses. Vol. 8. US Department of Health and Human Services, NIH; Bethesda, MD: 2001. pp. 305–325. National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- 37.Cooney NL, Babor TF, Litt MD. Matching clients to alcoholism treatment based on severity of alcohol dependence. In: Longabaugh RH, Wirtz PW, editors. Project MATCH Hypotheses. Results and Causal Chain Analyses. Vol. 8. NIAAA; Rockville, MD: 2001. pp. 30–43. NIAAA Project MATCH Monograph Series. [Google Scholar]
- 38.Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network support for drinking, alcoholics anonymous and long term matching effects. Addiction. 1998;93(9):1313–1333. doi: 10.1046/j.1360-0443.1998.93913133.x. [DOI] [PubMed] [Google Scholar]
- 39.Karno MP, Longabaugh R. What do we know? Process analysis and the search for a better understanding of project MATCH'S anger-by-treatment matching effect. J Stud Alcohol. 2004;65(4):501–512. doi: 10.15288/jsa.2004.65.501. [DOI] [PubMed] [Google Scholar]
- 40*.Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivar Behav Res. 2007;42(1):185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- 41.Witkiewitz K, Bowen S, Donovan DM. Moderating effects of a craving intervention on the relation between negative mood and heavy drinking following treatment for alcohol dependence. J Consult Clin Psych. 2011;79(1):54–63. doi: 10.1037/a0022282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anton RF, O'Malley SS, Ciraulo DA, et al. Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence: The COMBINE Study: A Randomized Controlled Trial. JAMA. 2006;295(17):2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- 43.Marlatt GA, Gordon JR. Relapse Prevention. Guilford; New York: 1985. [Google Scholar]
- 44.Preacher KJ. [March 2011];Calculations for the test of conditional indirect effects [Computer software] Available at http://www.quantpsy.org.