SUMMARY
Study objective
To investigate incidence, risk factors and impact of falls on health related quality of life (HRQoL) in patients with chronic obstructive pulmonary disease (COPD).
Design
Observational cohort study
Methods
Patients completed these questionnaires at baseline and at 6-months: Medical Outcomes Study Short Form 36 (SF-36), Chronic Respiratory Questionnaire (CRQ), Activities Balance Confidence (ABC) Scale and a form to record demographic data, medications, co-morbidities, oxygen use, acute exacerbations, fall history and assistive device use. Physical activity was measured with the Physical Activity Scale for the Elderly (PASE) only at baseline. Fall incidence was monitored through monthly fall diaries. Patients were categorized as non-fallers (0 falls) or fallers (≥1 falls).
Results
Data from 101 patients with a forced expiratory volume in one second of 46.4±21.6% predicted were analyzed. Thirty-two patients (31.7%) reported at least one fall during the 6-months. Fall incidence rate was 0.1 (95% CI:0.06 to 0.14) falls per person-month. Fallers tended to be older (p=0.04), female (p=0.04) and oxygen dependent (p=0.02), have a history of previous falls (p<0.001), more co-morbidities (p=0.007) and take more medications (p=0.001). Previous falls (OR=7.36; 95% CI:2.39 to 22.69) and diagnosis of coronary heart disease (OR=7.07; 95% CI:2.14 to 23.36) were the most important predictors of falls. The Dyspnea Domain of the CRQ declined significantly more (p=0.02) in the fallers group at 6-months.
Conclusions
Patients with COPD have a high susceptibility to falls, which is associated with a worsening of dyspnea perception as related to HRQoL. Fall prevention programs in COPD are recommended.
INTRODUCTION
Falls in the elderly have devastating consequences for functional independence, social interaction and life expectancy.1 Well established risk factors for falls such as lower limb muscle weakness as well as deficits in functional performance and postural control are common in people with chronic obstructive pulmonary disease (COPD).2 Results from a recent study suggest that COPD is one of the chronic conditions with the highest prevalence of falls, second only to osteoarthritis.3 Fall incidence in people with COPD has been estimated to range between 25–46%.3–5
The studies exploring fall incidence in COPD,4,5 however, have collected data with regards to falls retrospectively. Current international guidelines for the design of fall prevention trials6 stress the importance of recording fall events prospectively in order to minimize the effect of recall bias that is inherent in most retrospective fall-risk studies.7 In addition, cross sectional designs are susceptible to reverse causality.3 Thus, a prospective study will likely provide more reliable data on fall incidence in COPD.
In addition to the incidence of falls, both the specific risk factors and impact of falls on health related quality of life (HRQoL) have not been investigated in COPD. It is widely accepted that falls in the elderly, especially those that are traumatic falls,8 generally have deleterious effects on HRQoL.9 Ascertaining the incidence, risk factors and implications of falls on HRQoL is important to determine the clinical relevance of preventing falls in COPD. The objectives of this study were to reliably determine the incidence, risk factors and impact of falls on HRQoL in patients with COPD. We hypothesized that, compared with the fall incidence rates reported in previous studies in the elderly, fall incidence in people with COPD would be high. We also hypothesized that the domains of HRQoL associated with physical status would decrease significantly in fallers.
METHODS
Patients
A convenience sample of people with COPD was recruited between February and June 2009 from the caseload of respirologists from three hospitals. The ethics boards of each hospital approved the study and all participants gave written informed consent prior to participation. Inclusion criteria were: diagnosis of COPD confirmed by spirometry based on the Global Initiative for Chronic Obstructive Disease (GOLD) guidelines;10 the ability to ambulate using both legs. Exclusion criteria were: hospitalized patients; with end-stage COPD; major neurological conditions that affect balance or gait (e.g., prior stroke, Parkinson’s disease); not fluent in English or cognitive impairment that interferes with the ability to provide informed consent or to complete the study.
Study design
This was a 6-months observational cohort study that utilized mailed surveys supplemented by follow-up phone calls and medical charts review. Participants were assessed at baseline and at 6-months. Fall incidence was monitored through monthly fall diaries on a daily basis. In short, two weeks before the start of the study, participants received a first package via mail with a stamped addressed return envelope containing: instructions for completion, a letter of invitation, a consent form, monthly fall diaries for 6 months and a set of questionnaires: the Medical Outcomes Study Short Form-36 (SF-36), the Chronic Respiratory Questionnaire (CRQ), the Activities Balance Confidence (ABC) Scale, the Physical Activity Scale for the Elderly (PASE) and a structured form to record demographic data, current medications, co-morbidities, oxygen use, acute exacerbations of COPD, falls during the preceding 6 months and use of an assistive device.
After receiving the first mailed package, participants were contacted by telephone to confirm consent to participate. Fall diaries were returned at the end of each month using pre-paid envelopes. Participants who had not returned the fall diaries within the 10 days after the end of each month were contacted by telephone. To ensure compliance with the study, follow-up telephone calls were made to participants at the third and fifth month. Five months after the beginning of the study, participants received a second package containing all the above-mentioned questionnaires except the PASE, which was completed only at baseline. Participants were instructed to complete this second set of questionnaires at the end of the sixth month and to mail them back.
Outcomes
Fall incidence
Fall incidence was investigated by asking participants to report, on a daily basis, any fall event in the monthly fall diary. Participants were asked: “Have you had any fall including a slip or trip in which you lost your balance and landed on the floor or ground or lower level?”6 If a fall was diarized, participants were telephoned to confirm that the event was consistent with the definition of fall and to detail the circumstances of the fall and any resultant injury, using a standardized questionnaire.11
Health related quality of life (HRQoL), balance confidence and physical activity level
Health-related quality of life (HRQoL) was assessed through the self-administered versions of SF-3612 and the CRQ.13 The SF-36, which provides information on HRQoL from eight different health-domain scales, was chosen because it has been shown to be easily administered with good psychometric properties (e.g., sensitivity) to measure generic aspects of HRQoL in people with COPD.14 Another factor that was taken into account is that the SF-12, a short version of the SF-36, has been shown to be sensitive when correlated to risk factors for falls.15 The CRQ is a disease-specific HRQoL instrument, which has proven to be valid, reliable and sensitive to detect changes in health status in people with COPD.14 The CRQ provides information regarding health status in four different domains: dyspnea, fatigue, emotional function and mastery (i.e., feeling of control over the disease and its effects).13
Balance confidence was assessed with the ABC scale,16 which has shown to be a valid and reliable measure to discriminate between levels of functional mobility in the elderly.17 Since postural instability18 and fear of falling19 have been commonly identified as risk factors for falls, it is reasonable to surmise that reduced balance confidence measured by the ABC scale might be associated with an increased risk for falling.5 Briefly, the ABC scale contains 16 items, with each item rated from 0% (no confidence) to 100% (complete confidence). The maximum score is 1600, which is then divided by the number of items (16) to obtain a composite score.
Physical activity level was assessed with the PASE,20,21 which has been validated by comparison to physical activity levels measured by portable accelerometers.22 The PASE is a 12-item self-administered questionnaire that measures physical activity levels based on scores ranging from 0 to 400.
Medications and co-morbidities
A structured form was used to self-report the number and types of current medications and co-morbidities, which in turn, was followed up by a retrospective medical chart review to confirm information. In cases of discrepancies, the participant and/or physician was contacted and asked to clarify the information. Any newly prescribed medication or diagnosed chronic condition during the study (reported in the form of the second mail-out package) was included in the analysis only if prescribed or diagnosed before the third month of the study. Medications were categorized according to the Canadian Medical Association.23 Co-morbidities were categorized using a scheme previously described to study risk factors for falls.3
Severity of COPD, oxygen use, exacerbations, use of assistive device and previous fall
Severity of COPD was determined by the most recent spirometry data recorded prior to the start of the study obtained from the medical chart review. The structured clinical form asked participants about: oxygen use (on exertion only, at night only, always); the number of exacerbations in the 6 months preceding the study (first package) and during the study (second package); and the use of an assistive device. Any disagreements between the data provided by the participant and the medical chart were followed up with telephone contact to the participants and/or physician to clarify information.
Statistical analyses
Normality for all continuous variables was explored through visual analysis of histograms and normality plots. Analyses included only those participants who had returned at least the first monthly fall diary. Fall incidence rate (IR), was calculated with negative binomial regression (NBR).24
To determine differences between prospective fallers and non-fallers at baseline, the Pearson’s chi square test for differences in proportions and either the Student’s-t-test or Mann Whitney test for continuous data were used. Differences between fallers and non-fallers in changes in measures of HRQoL (SF-36 and CRQ) as well as balance confidence (ABC) during the 6-month period were assessed by forced entry multivariable regression analyses, with baseline scores and experimental group as independent variables of the model.25
A logistic regression model with faller and non-faller as dependent dichotomous variable was used to examine potential risk factors for falls. Correlation analyses were used to explore associations between the dependent and independent variables. Pearson’s or Spearman’s assessed multicollinearity among independent variables. Variables with a p≤0.25 on bivariate analysis were entered into the regression model26 and analyzed using the likelihood ratio method with backward elimination.27 Data are presented as means and 95% confidence intervals (CI), medians and percentiles (P25, P75) and proportions (%). Results for risk factors for falls are presented as odds ratio (OR) with CI. All analyses were performed with the Statistical Package for the Social Sciences (SPSS Inc., Chicago., IL., USA) using two-tailed probability tests with a level of significance set at p≤0.05.
RESULTS
Recruitment and follow-up
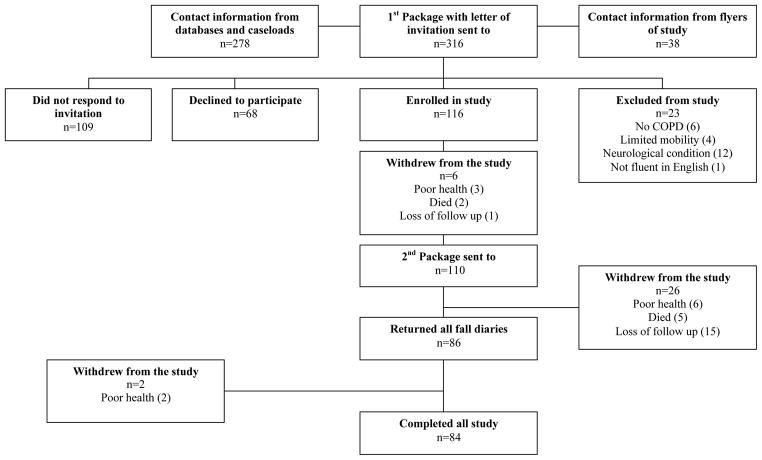
Of the 316 recipients of the first mail-out, 65.5% responded, which included: one hundred sixteen who met the inclusion criteria; sixty eight who declined primarily due to lack of time or poor health; twenty three who were excluded because they did not have a well-established diagnosis of COPD, lacked English fluency, had limited mobility or had neurological diagnoses. Of the 116 participants, 101 (45 females and 56 males) filled out one or more fall diaries, 86 (85.2%) returned 6 fall diaries and 9 (8.9%) returned 5 fall diaries. Eighty-four participants (83.2%) completed all study requirements (Figure 1).
Figure 1.
Flow chart showing the different stages of the recruitment process and the study
Participants
Compared to non-fallers, fallers were older (p=0.04), had a greater proportion of female participants (p=0.04), used more oxygen on exertion (p=0.02), fell more during the 6 months prior to the commencement of the study (p<0.001) (Table 1), took more medications (p=0.001), had more co-morbidities (p=0.007), and had a higher prevalence of coronary heart disease (p<0.001) (Table 2). The severity of COPD based on spirometry did not differ between fallers and non-fallers (Table 1). However, the frequency of fallers that required oxygen support tended to be greater compared to non-fallers (p=0.07) (Table 1). Twenty-one patients reported one or more exacerbations in the 6 months prior to the study, while only 14 patients reported exacerbations during the study. Only the number of exacerbations during the study was significantly greater (p=0.027) in the fallers’ group. Fallers showed a tendency towards lower scores in the PASE and ABC at baseline (Table 1). Mean balance confidence scores during the study decreased 4 and 6 points in the group of non-fallers and fallers, respectively. However, differences between groups were not significant (p=0.3).
Table 1.
Characteristics of participants at baseline. Data are presented as means and 95% CI or proportions (%).
| Non-fallers (n=69) | Fallers (n=32) | p-value | |
|---|---|---|---|
| Demographics | |||
| Mean age | 72.1 (69.6 to 74.5) | 75.5 (71.9 to 79.1) | 0.04* |
| Female (%) | 26 (37.7%) | 19 (59.4%) | 0.04* |
| Mean BMI | 24.9 (23.3 to 26.5) | 27.9 (25 to 30.8) | 0.9 |
| Spirometry (% predicted) | |||
| Mean FEV1 | 43.4 (36.9 to 49.8) | 43.6 (36.4 to 50.8) | 0.7 |
| Mean FVC | 71 (64.8 to 77.2) | 72.3 (64.3 to 80.4) | 1 |
| Mean FVE1/FVC | 50 (45 to 55.1) | 54 (46.6 to 61.3) | 0.4 |
| Oxygen use (%) | |||
| Never | 52 (75.4%) | 18 (56.3%) | 0.07 |
| Only on exertion | 2 (2.9%) | 5 (15.6%) | 0.02* |
| At nights | 5 (7.2%) | 2 (6.3%) | 0.8 |
| Always | 10 (10%) | 7 (21.9%) | 0.3 |
| Mean previous exacerbations | 0.3 (0.1 to 0.5) | 0.4 (0.1 to 0.6) | 0.1 |
| Mean PASE score | 108.8 (91.7 to 125.9) | 86.2 (66.4 to 105.9) | 0.1 |
| Use of assistive device (%) | 16 (23.2%) | 11 (34.4%) | 0.2 |
| Fell in previous 6 months (%) | 5 (7.2%) | 14 (43.8%) | <0.001* |
| Mean ABC score | 81.5 (76.9 to 86.1) | 74.4 (66.3 to 82.5) | 0.1 |
BMI: body mass index; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; PASE: Physical Activity Scale for the Elderly; ABC: Activities Balance Confidence Scale.
Indicates significant difference between groups at p<0.05
Table 2.
Medications and co-morbidities at baseline. Data are presented as medians (P25, P75) or proportions (%).
| Non-fallers (n=69) | Fallers (n=32) | p-value | |
|---|---|---|---|
| Medications (n) | 5 (3 to 8) | 8 (6 to 10.5) | 0.001* |
| Medication type (%) | |||
| Psychotropic | 14 (20.3%) | 9 (28.1%) | 0.4 |
| Peripheral nervous | 1 (1.4%) | 3 (9.4%) | 0.06 |
| Analgesic | 20 (29%) | 13 (40.6%) | 0.2 |
| Renal | 3 (4.3%) | 4 (12.5%) | 0.1 |
| Digestive | 14 (20.3%) | 5 (15.6%) | 0.6 |
| Immune | 8 (11.6%) | 3 (9.4%) | 0.7 |
| Reproductive & sexual | 1 (1.4%) | 0 (0%) | 0.5 |
| Endocrine | 21 (30.4%) | 14 (43.8%) | 0.2 |
| Respiratory | 58 (81.4%) | 25 (78.1%) | 0.5 |
| Visual | 4 (5.8%) | 5 (15.6%) | 0.1 |
| Cardiovascular | 38 (55.1%) | 22 (68.8%) | 0.2 |
| Co-morbidities (n) | 2 (1 to 4) | 4 (2.5 to 5.5) | 0.007* |
| Co-morbidity type (%) | |||
| Coronary | 14 (20.3%) | 19 (59.4%) | <0.001* |
| Circulatory | 34 (49.3%) | 19 (59.4%) | 0.3 |
| Digestive | 10 (14.5%) | 5 (16.1%) | 0.8 |
| Depression & mood | 8 (11.6%) | 7 (21.9%) | 0.2 |
| Renal | 1 (1.4%) | 3 (9.4%) | 0.06 |
| Immune | 8 (11.6%) | 1 (3.1%) | 0.2 |
| Musculoskeletal | 10 (14.5%) | 8 (25%) | 0.2 |
| Cancer | 9 (13%) | 3 (9.4%) | 0.6 |
| Endocrine | 27 (39.1%) | 16 (50%) | 0.3 |
| Peripheral nerve | 2 (2.9%) | 2 (6.3%) | 0.4 |
| Eye | 5 (7.2%) | 5 (15.6%) | 0.2 |
Indicates significant difference between groups at p<0.05
Fall Incidence
The NBR analysis showed an IR of 0.1 falls per person-month (95% CI: 0.06 to 0.14). Thirty-two participants (31.7%) reported at least one fall during the study. Of these 32 participants, 9 (28.1%) reported 2 or 3 falls and 4 (12.5%) participants reported 4 falls. The total number of falls was 57 with an average of 1.8 falls per participant in the fallers’ group. Most falls occurred during outdoor walking activities. Only one participant had a fall, which led to an injury (right arm fracture) and the others resulted in minor (e.g., bruises) or no injury.
Health related quality of life (HRQoL)
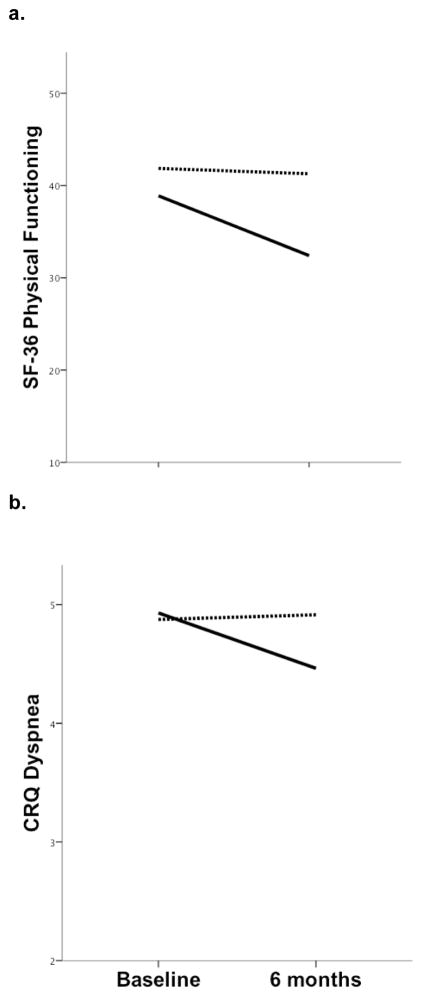
Fallers tended to show lower baseline scores in the physical (physical functioning and role physical) and general health domains of the SF-36 (Table 3). However, there were no significant between-group differences in the SF-36 at baseline, in spite of an increased body pain in the group of non-fallers (p=0.02) (Table 3). Although fallers tended to show a greater decline in the physical domains of the SF-36, no significant between-group differences in the change of scores during the 6 months were observed (Figure 2a). The fallers’ group tended to show lower scores, albeit non-significant, in the CRQ at baseline except for the dyspnea domain, which was similar between groups (Table 3). There was a general trend of a greater decline in the scores of the CRQ after the 6 months in the fallers’ group (Table 3). The dyspnea domain of the CRQ showed a significantly greater decline in fallers compared to non-fallers (p=0.02) (Figure 2b).
Table 3.
Measures of health related quality of life (HRQoL) at baseline and at 6-month. Data are presented as means ± SD.
| Baseline | 6-month | |||
|---|---|---|---|---|
|
| ||||
| Non-fallers (n=69) | Fallers (n=32) | Non-fallers (n=69) | Fallers (n=32) | |
| SF-36 | ||||
| Physical functioning | 42.9 ± 25.3 | 41.6 ± 22.5 | 42 ± 25.7 | 34.3 ± 19.9 |
| Role physical | 49.7 ± 30.1 | 43.5 ± 24.2 | 50.6 ± 27.6 | 42.1 ± 26.3 |
| Bodily pain | 23.7 ± 21.4 | 32.6 ± 22* | 25.3 ± 22.4 | 37.8 ± 22.5 |
| General health | 56 ± 12.1 | 51.7 ± 14.6 | 56.4 ± 11.6 | 54.6 ± 12.8 |
| Vitality | 51.9 ± 11.5 | 52.7 ± 10.2 | 53.8 ± 11.7 | 57.3 ± 8.6 |
| Social functioning | 49.2 ± 13.6 | 51.6 ± 7.8 | 50 ± 8.1 | 54.3 ± 9.7 |
| Role emotional | 72.9 ± 28.7 | 68.2 ± 29.8 | 65.8 ± 29.6 | 66.7 ± 25.7 |
| Mental Health | 63.8 ± 7.5 | 65.6 ± 11 | 62.7 ± 11.2 | 65 ± 7.4 |
| CRQ | ||||
| Dyspnea | 4.9 ± 1.3 | 4.9 ± 1.3 | 5 ± 1.2 | 4.5 ± 1.1** |
| Fatigue | 4.1 ± 1.4 | 3.9 ± 1.7 | 4.2 ± 1.3 | 3.9 ± 1.2 |
| Emotional | 5.1 ± 1.2 | 4.8 ± 0.7 | 4.9 ± 1.3 | 4.7 ± 1 |
| Mastery | 5.4 ± 1.4 | 5.2 ± 1.2 | 5.2 ± 1.5 | 5 ± 1.2 |
SF-36: Health Survey Short Form
CRQ: Chronic Respiratory Questionnaire
Indicates significant differences between groups at baseline (p<0.05).
Indicates significant between-group differences in the trajectory of HRQoL (p<0.05).
Figure 2.
Trajectory of the SF-36 physical functioning (a) and CRQ dyspnea (b) scores in fallers (solid line) and non-fallers (dashed line) during the 6-months.
Compared to non-fallers, fallers showed a tendency (p=0.15) towards a more pronounced decline in the SF-36 physical functioning domain during the 6-months (a). The decline in the CRQ dyspnea domain was significantly larger (p=0.02) in the fallers group (b).
Risk factors for falls
The correlation analyses showed significant associations between fall incidence and the number of previous falls (r=0.44;p<0.001), number of co-morbidities (r=0.27;p=0.006) and medications (r=0.32;p=0.001), age (r=0.21;p=0.036) and female gender (r=0.20;p=0.04). Coronary heart disease was also associated with fall occurrence (r=0.39;p<0.001). Oxygen use (r=0.19;p=0.053), balance confidence scores at baseline (r=-0.17;p=0.1), and previous exacerbation (r=0.16;p=0.1) showed trends suggestive of association with fall incidence and thus were included in the initial regression model. The final model accounted for 49% of the variance in predicting a fall (Table 4). Previous fall history was the best predictor of fall incidence (p=0.001) with an OR of 7.36 times greater than those who did not report a previous fall. The second most important predictor was coronary heart disease with an OR of 7.07. Other risk factors for falls were age and being female. Oxygen use appeared to increase the risk for falling (OR=2.83) but its effect was not statistically significant (p=0.08).
Table 4.
Logistic regression model for assessing risk factor for falls. Data are provided as coefficient (B) values with standard errors (SE) and odds ratio (OR) with 95% CI. The model explained 49% of the variance in fall risk (pseudo R2=0.49).
| Predictor | B (SE) | OR (95% CI) | p-value |
|---|---|---|---|
| Previous fall | 1.99 (0.57) | 7.36 (2.39 to 22.69) | 0.001* |
| Age | 0.08 (0.04) | 1.09 (1.01 to 1.17) | 0.020* |
| Gender (F) | 1.32 (0.60) | 3.73 (1.14 to 12.16) | 0.016* |
| Coronary disease | 1.96 (0.61) | 7.07 (2.14 to 23.36) | 0.001* |
| Oxygen use | 1.04 (0.59) | 2.83 (0.88 to 9.08) | 0.080 |
Indicates significant difference between groups at p<0.05.
DISCUSSION
To the best of our knowledge, this is the first prospective study analyzing the incidence, risk factors and association between falls and HRQoL in COPD patients. The main finding of this study is that people with COPD show a high incidence of falls. The second main finding is that HRQoL associated with dyspnea declined significantly in the group of fallers during the 6-months’ study period. Of particular interest, fall incidence is relatively independent of the stage of COPD. The number of previous falls and diagnosis of coronary heart disease were the most important risk factors for falls in people with COPD. Age and female gender also significantly increased the risk for falls in our cohort.
Fall incidence
An annual projection of the falls IR (0.1) of this study indicates that people with COPD would show an annual rate of 1.2 falls per person-year, which is a considerably higher rate compared to the incidence previously reported in the elderly (IR=0.24).28 The proportion of COPD patients who sustained a fall (31.7%) was closer to the upper range previously reported.29 In our study, approximately one-third of people with COPD sustained at least one fall during the 6-month period of the study, which is similar to that reported prospectively in older adults for a one year period,30,31 and retrospectively, in people with COPD (range: 25% to 46%).3–5 Fall incidence does not follow a regular pattern and some people experience recurrent falls while some others do not fall. Thus, projections and comparisons with other studies should be done cautiously. However, given that our follow-up was only 6 months, even a conservative annual projection of the proportion of fallers would provide higher estimates than those of previous studies. Differences in disease severity, definition of a fall32 as well as the fact that these previous studies3–5 used retrospective designs, which possibly underestimated fall incidence, might contribute to the disparity of results.
Impact of falls on health related quality of life (HRQoL)
We used both general (SF-36) and disease specific (CRQ) HRQoL measures to capture different aspects of health status in people with COPD.33 Although the act of falling per se was not associated with an overall decline in HRQoL, the dyspnea domain of the CRQ, decreased significantly in fallers compared to non-fallers. Dyspnea is important because is the most common and disabling symptom of COPD. Of interest, the decline in the dyspnea domain was 0.4 points, which is close to the minimal clinically important difference of 0.5 points for this questionnaire.34 Because of the relatively short duration of the study and the fact that only one fall resulted in a fracture, the decline of the dyspnea domain is a significant detriment worthy of further evaluation over a longer follow-up. We had expected to observe a decrease in physical function scores of the SF-36 and CRQ, however, the non-traumatic nature of falls8 and the contribution of multiple other co-morbidities may have confounded the ability to detect how falls impact these constructs over a 6-month period.
Risk factors for falls
Previous fall history, age, female gender and the presence of coronary heart disease are independent risk factors that predict falls in people with COPD. The associations between fall incidence being related to previous falls,4 advanced age30 and female gender,35 are consistent with previous studies in the elderly. The risk associated with previous fall history is clinically relevant because it emphasizes the importance of avoiding fall events to reduce the risk of further falls or targeting frequent fallers with more aggressive preventive measures. Recurrent falls are important because previous fall history can substantially increase fear of falling (OR=1.75; 95% CI:1.3 to 2.36)18 and, more importantly, the odds of experiencing injurious falls (OR=6.7; 95% CI: 2.1 to 21.5).36 This might be clinically relevant for people with COPD who show a higher prevalence of osteoporosis compared to healthy subjects37 and therefore a potential increased risk for fall-related bone fractures. Another risk factor was diagnosis of coronary heart disease. A recent cross-sectional study found that coronary heart disease was the third most common chronic condition associated with an increased fall risk (OR=1.82; 95% CI: 1.47 to 2.25) after depression and arthritis.3 Further studies are required to identify the underlying mechanisms explaining the association between coronary heart disease and fall risk in COPD. However, the high prevalence of coronary disease among people with COPD38 indicates that fall risk might be increased in these individuals.
Although fallers took more medications and had more co-morbidities, these two factors were not predictive of falls in our population. A possibility is that not all co-morbidities contribute to the same extent towards increasing the risk for falls3 and, alternatively, some may not have been self-reported or detected by our study methodology. For example, in contrast with previous estimates,39 the prevalence of depression, a disease associated with increased fall occurrence (OR=2.01; 95% CI: 1.63 to 2.48),3 was relatively small (14.8%) in this cohort of patients. Our methodology may also have been insensitive or underpowered to detect the presence of common co-morbidities such as arthritis. Another explanation for the lack of association between number of medications and co-morbidities with fall occurrence might be related to the fact that our dichotomous classification of fallers and non-fallers did not discriminate between fallers and occasional fallers.40 When participants were classified as non-fallers, fallers (1 fall) and frequent fallers (>1 fall), the number of medications and co-morbidities showed a marked trend towards increase in the frequent faller’s group.
In spite of lower scores in the ABC scale in the group of fallers, balance confidence was not predictive of falls. This finding was surprising given a previous retrospective study that found the ABC scale to be sensitive enough to discriminate fallers and non-fallers in a COPD group.5 However, retrospective studies should be interpreted with caution because they are susceptible to reverse causality. For example, a recent study shows that previous falls increase fear of falling and vice versa.41 Thus, we cannot rule out the possibility that previous fall history reduced balance confidence in the retrospective study.5 Normative data from older adults establishes a threshold at 80 points for the ABC score below which functional impairment starts to decline.17 Perhaps, the relatively high balance confidence scores reported at baseline by the fallers (74.4; 95% CI: 66.3 to 82.5) diluted the capacity of the ABC scale to predict falls in our study.
A recent cross sectional study reported that patients with COPD on oxygen therapy were six times more likely to experience a fall than those who did not use supplemental oxygen.5 In our study, although oxygen use appeared to increase the risk for falling (OR=2.83), its effect was not statistically significant (p=0.08). Nevertheless, fallers showed a significantly greater use of oxygen on exertion compared to non-fallers at baseline. The underlying mechanisms for the potential association between oxygen use and increased fall risk are unclear. A possibility is that oxygen use is simply more prevalent in patients with functional impairment and thus with and increased susceptibility to fall.5 Another explanation that deserves further investigations includes the potential deleterious effects of chronic hypoxemia on motor control.42
Fallers also tended to show lower physical activity levels and a more frequent use of an assistive device at baseline. Mobility impairments and the use of an assistive device have been associated with increased fall risk in the elderly.43 However, due to our study design, it is impossible o determine if a causal association between these two factors and fall incidence exists in people with COPD. Perhaps the lower physical activity level and prevalent use of assistive device among fallers simply reflect a greater level of functional impairment consistent with an increased fall risk.
LIMITATIONS
This study has some limitations worthy of consideration. Firstly, our dichotomous classification of fallers and non-fallers did not discriminate between fallers and occasional fallers. Some previous studies suggest that the use of three fall frequency levels such as non-faller, faller, and frequent faller might be more appropriate.40 We performed a sensitivity analysis that showed frequent fallers tended to have greater levels of impairment compared to fallers, however, the differences were not statistically significant. Further, we explored the appropriateness of a multinomial regression model using these three fall frequency levels but the multinomial model failed to accommodate all independent variables. Considering the relatively small sample size and the short follow-up period, the use of a binary logistic regression was considered more appropriate. An important limitation of the study is that a control healthy group was not included. We circumvented this limitation by comparing our results with existing normative data from elderly subjects with similar demographic characteristics.28 Other potential limitations include the fact that postural control and muscle strength, important risk factors for falls in the elderly, were not assessed and that physical activity level was assessed through a self-administered questionnaire. While the PASE has been validated to assess physical activity in the elderly,22 the use of more objective methods (e.g., accelerometers) would possibly have provided more reliable data.
CONCLUSIONS
People with COPD have a high incidence rate of falls that is associated with a decline in dyspnea related activities associated with HRQoL. Previous fall history and diagnosis of coronary heart disease are the most important predictors of falls in COPD patients. Further larger and longer prospective studies investigating the incidence of falls on HRQoL are needed. In the meantime, fall prevention strategies in people with COPD are encouraged.
Acknowledgments
The authors acknowledge the assistance of Giselle Gerdak and Jill Greczmiel (Vancouver General Hospital, Vancouver) in the recruitment of patients. We also acknowledge the assistance of Jenny Ying during the testing procedures and the help of Jennifer Rurak in editing a previous version of this manuscript.
FUNDING
This project was funded by grants from the Canadian Respiratory Health Professionals (CRHP) and the Physiotherapy Foundation of Canada (PFC). Support was received through a Strategic Training Fellowship in Rehabilitation Research from the CIHR Musculoskeletal and Arthritis Institute (MR), a Fellowship in Respiratory Rehabilitation from the BC Lung Association (MR), a Graduate Fellowship from the University of British Columbia (MR), and a Career Scientist Award (JJE) from CIHR (MSH-63617).
References
- 1.Tinetti ME. Preventing falls in elderly persons. N Engl J Med. 2003;348:42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 2.Roig M, Eng JJ, Road JD, Reid DW. Falls in patients with chronic obstructive pulmonary disease: A call for further research. Respir Med. 2009;103:1257–1269. doi: 10.1016/j.rmed.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ. 2003;327(712):1–6. doi: 10.1136/bmj.327.7417.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hellstrom K, Vahlberg B, Urell C, Emtner M. Fear of falling, fall-related self-efficacy, anxiety and depression in individuals with chronic obstructive pulmonary disease. Clin Rehabil. 2009;23:1136–1344. doi: 10.1177/0269215509342329. [DOI] [PubMed] [Google Scholar]
- 5.Beauchamp MK, Hill K, Goldstein RS, Janaudis-Ferreira T, Brooks D. Impairments in balance discriminate fallers from non-fallers in COPD. Respir Med. 2009;103:1885–1891. doi: 10.1016/j.rmed.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc. 2005;53:1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 7.Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36:613–616. doi: 10.1111/j.1532-5415.1988.tb06155.x. [DOI] [PubMed] [Google Scholar]
- 8.Iglesias CP, Manca A, Torgerson DJ. The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int. 2009;20:869–878. doi: 10.1007/s00198-008-0753-5. [DOI] [PubMed] [Google Scholar]
- 9.Salkeld G, Cameron ID, Cumming RG, Easter S, Seymour J, Kurrle SE, et al. Quality of life related to fear of falling and hip fracture in older women: A time trade off study. BMJ. 2000;320:341–346. doi: 10.1136/bmj.320.7231.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. Global Initiative for Obstructive Pulmonary Disease (GOLD) [Date last accessed: June 2009];Global strategy for the diagnosis management and prevention of chronic obstructive pulmonary disease. www.goldcopd.com. Date last updated: 2009.
- 11.Harris JE, Eng JJ, Marigold DS, Tokuno CD, Louis CL. Relationship of balance and mobility to fall incidence in people with chronic stroke. Phys Ther. 2005;85:150–158. [PubMed] [Google Scholar]
- 12.Ware JE, Kosinski M, Bjorner JB. User’s manual for the SF-36v2 health survey. 2. Lincoln, IL, USA: QualityMetric Incorporated; 2008. [Google Scholar]
- 13.Williams J, Singh S, Sewell L, Guyatt G, Morgan M. Development of a self-reported chronic respiratory questionnaire (CRQ-SR) Thorax. 2001;56:954–959. doi: 10.1136/thorax.56.12.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Curtis JR, Patrick DL. The assessment of health status among patients with COPD. Eur Repir J. 2003;41:36s–45s. doi: 10.1183/09031936.03.00078102. [DOI] [PubMed] [Google Scholar]
- 15.Ozcan A, Donah H, Gelecek N, et al. The relationship between risk factors for falling and the quality of life in older adults. BMC Public Health. 2005;5:90. doi: 10.1186/1471-2458-5-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Powell LE, Myers AM. The activities-specific balance confidence (ABC) scale. J Gerontol A Biol Sci. 1995;50A:M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 17.Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the activities-specific balance confidence (ABC) scale. J Gerontol A Biol Sci. 1998;53:M287–294. doi: 10.1093/gerona/53a.4.m287. [DOI] [PubMed] [Google Scholar]
- 18.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35:37–41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 19.Friedman SM, Munoz B, West SK, et al. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–35. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 20.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 21.Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): Development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 22.Washburn RA, Fickler JL. Physical activity scale for the elderly (PASE): The relationship with activity measured by a portable accelerometer. J Sports Med Phys Fitness. 1999;39:336–340. [PubMed] [Google Scholar]
- 23.Canadian Medical Association. Prescription & over the counter drugs for Canadians. Toronto, Canada: Reader’s Digest; 2002. [Google Scholar]
- 24.Robertson MC, Campbell AJ, Herbison P. Statistical analysis of efficacy in falls prevention trials. J Gerontol A Biol Sci Med Sci. 2005;60:530–534. doi: 10.1093/gerona/60.4.530. [DOI] [PubMed] [Google Scholar]
- 25.Barnett A, Smith B, Lord SR, Williams M, Baumand A. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing. 2003;32:407–414. doi: 10.1093/ageing/32.4.407. [DOI] [PubMed] [Google Scholar]
- 26.Hosmer DW, Lemeshow S. Wiley Series in Probability and Statistics. 2. New York, NY, USA: John Wiley & Sons; 2000. Applied logistic regression. [Google Scholar]
- 27.Field A. Discovering statistics using SPSS. 2. London, UK: Sage; 2005. [Google Scholar]
- 28.O’Loughlin JL, Boivin JF, Robitaille Y, Suissa S. Falls among the elderly: distinguishing indoor and outdoor risk factors in Canada. J Epidemiol Comm Health. 1994;48:488–491. doi: 10.1136/jech.48.5.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coimbra AMV, Ricci NA, Coimbra IB, Costallat LTL. Falls in the elderly of the family health program. Arch Gerontol Geriatr. 2010 Feb 11; doi: 10.1016/j.archger.2010.01.010. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 30.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 31.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–1056. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 32.Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C PROFANE-Group. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing. 2006;35:5–10. doi: 10.1093/ageing/afi218. [DOI] [PubMed] [Google Scholar]
- 33.Malý M, Vondra V. Generic versus disease-specific instruments in quality-of-life assessment of chronic obstructive pulmonary disease. Methods Inf Med. 2006;45:211–215. [PubMed] [Google Scholar]
- 34.Jaeschke E, Singer J, Guyatt GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 35.Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev. 2005;11:115–119. doi: 10.1136/ip.2004.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol. 1991;46:164–170. doi: 10.1093/geronj/46.5.m164. [DOI] [PubMed] [Google Scholar]
- 37.Graat-Verboom L, Wouters EF, Smeenk FW, van den Borne BE, Lunde R, Spruit MA. Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J. 2009;34:209–218. doi: 10.1183/09031936.50130408. [DOI] [PubMed] [Google Scholar]
- 38.Crisafulli E, Costi S, Luppi F, Cirelli G, Cilione C, Coletti O, et al. Role of comorbidities in a cohort of patients with COPD undergoing pulmonary rehabilitation. Thorax. 2008;63:487–492. doi: 10.1136/thx.2007.086371. [DOI] [PubMed] [Google Scholar]
- 39.Mikkelsen RL, Middelboe T, Pisinger C, Stage KB. Anxiety and depression in patients with chronic obstructive pulmonary disease (COPD) A review Nord J Psychiatry. 2004;58:65–70. doi: 10.1080/08039480310000824. [DOI] [PubMed] [Google Scholar]
- 40.Campbell AJ, Reinken J, Allan BC, Martinez GS. Falls in old age: a study of frequency and related clinical factors. Age Ageing. 1981;10:264–270. doi: 10.1093/ageing/10.4.264. [DOI] [PubMed] [Google Scholar]
- 41.Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 42.Grant I, Heaton RK, McSweeny AJ, Adams KM, Timms RM. Neuropsychologic findings in hypoxemic chronic obstructive pulmonary disease. Arch Intern Med. 1982;142:1470–1476. [PubMed] [Google Scholar]
- 43.Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am. 2006;90:807–824. doi: 10.1016/j.mcna.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 44.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989;261:2663–2668. [PubMed] [Google Scholar]