Abstract
Background
Investigators in the US described large volume water infusion with marked benefits but acknowledged the limitation of male veteran predominance in the study subjects. The aim of this study was to assess the feasibility of large volume water infusion in Asian patients undergoing minimal sedation diagnostic colonoscopy in a community setting.
Methods
Consecutive patients who underwent colonoscopy were randomized to receive large volume (entire colon) (Group A, n=51), limited volume (rectum and sigmoid colon) (Group B, n=51) water infusion, or air insufflation (Group C, n=51). Pain during insertion, completion rate, cecal intubation and total procedure times, and patient satisfaction were evaluated. Pain and satisfaction were assessed with a 0–10 visual analog scale.
Results
The mean pain scores during insertion were lower in the Group A and Group B than in Group C, 3.3±2.4, 3.0±2.2 and 4.4±2.6, respectively (p=0.028 and p=0.004). The completion rates and cecal intubation times were similar among the three groups. The procedure time was significantly longer in Group A than in group C (15.3±5.9 min vs. 13.1±5.4 min, p=0.049). Overall satisfaction with the procedure was greater in Group B than in Group C only (9.7±0.5 vs. 9.4±0.8, p=0.044).
Conclusions
Diagnostic colonoscopy with large volume water infusion without air insufflation appears to be feasible in minimally sedated Asian patients in a community setting. Measures to improve the outcome further are discussed.
Key words: water, pain, colonoscopy, intubation time
Introduction
In minimally sedated Asian patients in a community setting we showed that a limited volume of water infusion instead of air insufflation in the rectal sigmoid colon significantly reduced pain score during colonoscopy from 3.4±2.8 to 2.5±2.5 (mean±SD, p=0.0213, t test) [0=no pain, 10=worst pain imaginable].1 Cecal intubation rate was not compromised. Insertion time was minimally but significantly increased by 1.9 min. Several US reports described the successful use of progressively larger volumes of water infused throughout the entire colon in patients undergoing colonoscopy with on-demand,2,3 minimal4 or no5,6 sedation. A major limitation acknowledged was the predominance of male veterans in these reports. Whether the findings are applicable to Asian non veteran patients undergoing minimally sedated colonoscopy in a community setting is not known. This prospective, randomized controlled trial compared large (entire colon) or limited (rectal sigmoid colon) water volume infusion with traditional air insufflation in patients undergoing minimally sedated diagnostic colonoscopy. We test the hypothesis that water infusion in lieu of air insufflation reduces pain in a dose-related manner in our practice setting. The limited volume group assesses the reproducibility of our previous result.
Methods
This prospective study was conducted between July and December 2010 at the Buddhist Dalin Tzu Chi General Hospital. Patients undergoing minimally sedated colonoscopy performed by 2 endoscopists (YHH and KCT) were included. Exclusions are shown in Figure 1. The study was approved by the local Institutional Review Board. Patients received purge preparation and premedication as previously described.1 Video colonoscope (EC-590WM, Fujinon, Saitama, Japan) was used. Colonoscopy began with the patient in the left lateral decubitus position. Intubation of the cecum was defined as successful if the base of the cecum could be touched with the tip of the colonoscope. Inspections were undertaken during the withdrawal phase.
Figure 1.
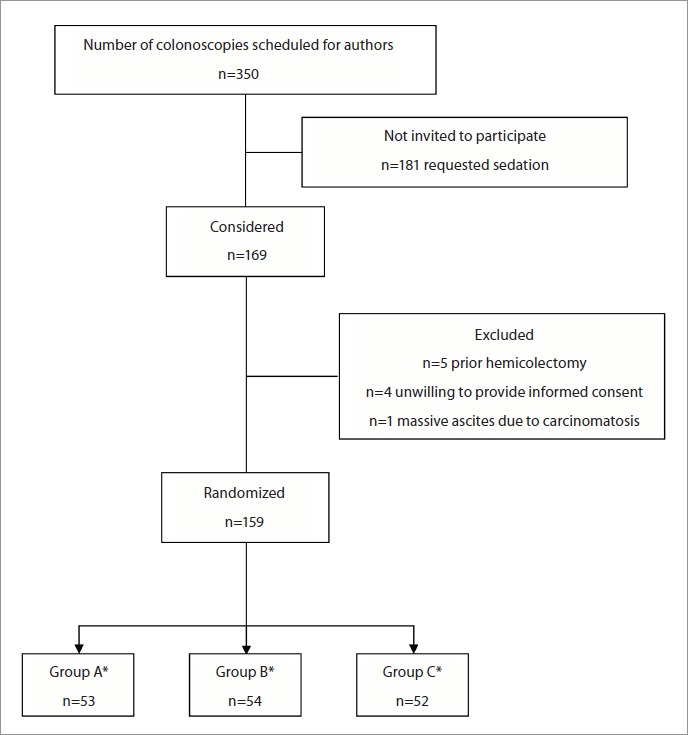
Flow diagram of the progress through enrollment and intervention allocation. Group A, water infusion was used throughout the entire colon. Group B, water infusion was limited to the distal colon. Group C, air insufflation was used throughout the procedure. The infused water in all groups was removed predominantly during withdrawal. *Five patients were excluded because of inadequate preparation (2 in group A, 2 in group B, and 1 in group C) and 1 in group B because of an obstructive tumor.
The patients were allocated into 3 groups by computerized randomization. In group A, water infusion was used throughout the entire colon during the insertion phase with the air pump turned off. Tap water at room temperature was infused through the accessory channel of the colonoscope using a foot-switch controlled water pump (JW2, Fujinon, Saitama, Japan). Air insufflation was not used until the cecum was reached. In group B, water infusion was limited to the distal colon. The air pump was turned off initially while water was infused into the rectum and the sigmoid colon. Water was not usually infused in the descending colon because the infused water already accumulated in this dependent segment. If the tip of the scope came out of the water, or could not find its way at the transverse colon, the air pump was then turned on.1 In group A and B, if the lumen could not be opened with water after attempting for 5 minutes, the air pump was turned on. In group C, air insufflation was used throughout the procedure. Aliquots of 30 to 50 mL of water were used for washing residual stool, as needed.1 In all groups, the infused water was removed predominantly during withdrawal.
Demographic and patient-specific data (Table 1) were obtained before colonoscopy. At the end of the procedure, procedure-related data (Tables 2 and 3) were recorded in the patient data sheet. A trained research assistant who was unaware of the randomization status administered the questionnaires to the subjects during and after the procedure. Patients were asked about pain during intubation when the tip of the colonoscope reached the cecum. Questions regarding pain during withdrawal of the colonoscope and post procedure bloating were asked immediately after the procedure was completed. Abdominal pain and bloating were graded on a visual analog scale (VAS) ranging from 0–10. Satisfaction was similarly assessed. Patients were asked whether they would receive the same method of intubation if needed in the future.
Table 1.
Baseline characteristics of the patients undergoing colonoscopy
| Group A (n=51) | Group B (n=51) | Group C (n=51) | p value | |
| Male | 29 (56.9%) | 29 (56.9%) | 29 (56.9%) | 1.00† |
| Age (year) | 52.4 ± 13.5 | 57.2 ± 13.2 | 56.3 ± 13.2 | 0.16* |
| BMI (kg/m2) | 24.2 ± 4.1 | 25.0 ± 4.2 | 23.7 ± 3.8 | 0.30* |
| Previous colonoscopy | 25 (49.0%) | 28 (54.9%) | 25 (49.0%) | 0.79† |
| Previous abdominal or pelvic surgery | 21 (41.2%) | 22 (43.1%) | 18 (35.3%) | 0.70† |
| Constipation | 14 (27.5%) | 11 (21.6%) | 6 (12.0%) | 0.15† |
| Inpatients | 4 (7.8%) | 2 (3.9%) | 1 (2.0%) | 0.50†† |
| Indication | 0.27† | |||
| Follow-up of polyps | 18 (35.3%) | 23 (46.0%) | 17 (33.3%) | |
| Abdominal pain | 4 (7.8%) | 3 (6.0%) | 5 (9.8%) | |
| Rectal bleeding | 9 (17.6%) | 9 (18.0%) | 6 (11.8%) | |
| Stool occult blood | 7 (13.7%) | 5 (10.0%) | 13 (25.5%) | |
| Change of bowel habit | 12 (23.5%) | 9 (18.0%) | 6 (11.8%) | |
| Anemia | 0 | 0 | 3 (5.9%) | |
| Weight loss | 1 (2.0%) | 1 (2.0%) | 1 (2.0%) | |
| Bowel cleansing | 0.17† | |||
| Sodium phosphate | 39 (76.5%) | 33 (64.7%) | 41 (80.4%) | |
| MC & B | 12 (23.5%) | 18 (35.3%) | 10 (19.6%) | |
| Anxiety | 4.1±2.7 | 3.4±2.7 | 3.4±2.5 | 0.34** |
| Antispasmodic agent use | 41 (80.4%) | 42 (82.4%) | 42 (82.4%) | 0.96† |
| Colon preparation | 0.97† | |||
| Good | 32 (62.7%) | 35 (68.6%) | 35 (68.6%) | |
| Fair | 13 (25.5%) | 11 (21.6%) | 11 (21.6%) | |
| Poor | 6 (11.8%) | 5 (9.8%) | 5 (9.8%) |
Group A, water infusion was used throughout the entire colon. Group B, water infusion was limited to the distal colon. Group C, air insufflation was used throughout the procedure. The infused water in all groups was removed predominantly during withdrawal. BMI, body mass index, MC & B, magnesium citrate & bisacody.
ANOVA test
Kruskal-Wallis test
Chi-squared test
Fisher exact test.
Colon preparation: The quality of bowel cleansing was classified by the endoscopist as: (1) good: dry colon or only clear liquid; (2) fair: minimal solid stool or slightly turbid fluid that could be suctioned; (3) poor: significant amount of solid residue; (4) inadequate: when stool residue precludes complete insertion..
Table 2.
Patient discomfort and satisfaction
| Group A (n=50) | Group B (n=50) | Group C (n=50) | p value | |
| Pain during insertiona | 3.3 ± 2.4 | 3.0 ± 2.2 | 4.4 ± 2.6 | A vs. B: 0.492 t |
| A vs. C: 0.028 t | ||||
| B vs. C: 0.004 t | ||||
| Pain during withdrawala | 1.6 ± 2.1 | 0.8 ± 1.2 | 1.3 ± 1.8 | A vs. B: 0.029 t |
| A vs. C: 0.395 t | ||||
| B vs. C: 0.178 t | ||||
| Bloating after procedurea | 2.7 ± 2.4 | 3.0 ± 2.0 | 3.8 ± 2.0 | A vs. B: 0.463 t |
| A vs. C: 0.013 t | ||||
| B vs. C: 0.051 t | ||||
| Patient satisfaction scoreb | 9.6 ± 0.7 | 9.7 ± 0.5 | 9.4 ± 0.8 | A vs. B: 0.395 t |
| A vs. C: 0.285 t | ||||
| B vs. C: 0.044 t | ||||
| Willingness to repeat the procedure if needed | 49 (98%) | 50 (100%) | 48 (96%) 0.773†† |
0=no pain, 10=worst pain imaginable
0=not satisfied at all, 10=completely satisfied
Fisher's exact test
Student's t-test.
Table 3.
Outcomes of colonoscopy
| Group A (n=51) | Group B (n=51) | Group C (n=51) | p value | |
| Number of failed cecal intubations | 1 (2.0%) | 1 (2.0%) | 1 (2.0%) | 1.000†† |
| Cecal intubation time (min) | 5.6 ± 3.4 | 4.6 ± 2.3 | 4.6 ± 2.6 | 0.284** |
| Procedure time (min) | 15.3 ± 5.9 | 14.4 ± 4.6 | 13.1 ± 5.4 | A vs. B: 0.384t |
| A vs. C: 0.049t | ||||
| B vs. C: 0.188t | ||||
| Volume of water used (mL) | 629 ± 226 | 399 ± 197 | 22 ± 35 | A vs. B: <0.001t |
| A vs. C: <0.001t | ||||
| B vs. C: <0.001t | ||||
| Number of cases requiring abdominal pressure | 19 (37%) | 22 (43%) | 29 (57%) | 0.125† |
| Number of cases requiring change of position | 9 (18%) | 4(8%) | 9 (18%) | 0.306†† |
| Number of cases with polyps | 30 (58.8%) | 33 (64.7%) | 30 (58.8%) | 0.781† |
| Number of cases with adenomas | 15 (29.4%) | 17 (33.3%) | 13 (25.5%) | 0.685† |
| Tubulovillous adenoma | 1 (2.0%) | 2 (3.9%) | 1 (2.0%) | |
| Carcinoma | 2 (3.9%) | 2 (3.9%) | 0 |
Kruskal-Wallis test
Chi-squared test
Fisher exact test
Student's t-test.
Statistical analysis
The primary endpoint of the study was to compare the patient abdominal pain scores during the insertion phase of colonoscopy among the three study groups. A sample size of 50 patients was chosen to detect a difference of 1.5 in the pain score given a standard deviation of 2.61 with a two-tailed alpha of 0.05 and a beta of 0.20. Statistical analysis was performed using SPSS version 12.0 software (SPSS Inc., Chicago, IL, USA). All continuous variables were expressed as mean±standard deviation (SD). The analysis of variance (ANOVA) and the Kruskal-Wallis test to compare three groups of continuous variables were used, where appropriate. When the normal assumption is unmet, we apply the Kruskal-Wallis test to compare the means of continuous variables instead of ANOVA. To check the normality assumption, we considered the Shapiro-Wilk normality test. We used the Student's t-test to compare two samples for continuous variable. The chi-squared test, with Yates' correction for continuity, was used for comparison of categorical data, while the Fisher's exact test was used when numbers were small. A p value <0.05 was considered to be significant.
Results
Figure 1 shows the flow of patients between July and December 2010. The baseline characteristics in the 3 groups were similar (Table 1). The mean pain score during insertion was higher in group C than in group A and group B (4.4±2.6 vs. 3.3±2.4 and 3.0±2.2, p=0.028 and p=0.004, respectively). The mean pain score during withdrawal was greater in group A than in group B (1.6±2.1 vs. 0.8±1.2, p=0.029), while no difference was found between groups A and C or between groups B and C. Post-procedure bloating was less in group A than group C (2.7±2.4 vs. 3.8±2.0, p=0.013), but there was no difference between group A and B or between group B and C. Overall satisfaction with the procedure was greater in group B than in group C (9.7±0.5 vs. 9.4±0.8, p=0.044), while no difference was found between groups A and B or between groups A and C. The willingness to repeat colonoscopy was similar among the groups (Table 2).
Incomplete colonoscopy due to an acute angle occurred in 1 patient (2%) in each group. Air insufflation had to be used in 5 patients (4 at the transverse and 1 at the descending colon) in group A, and 1 patient (at the sigmoid colon) in group B before reaching the transverse colon due to poor visibility. These 6 patients were all subsequently intubated to the cecum using air insufflation. There was no significant difference regarding polyp and adenoma detection rates among the groups (Table 3). The need for abdominal compression, need for changing position, and cecal intubation time were similar among the groups. Total procedure time was significantly longer in group A than in group C (15.3±5.9 min vs. 13.1±5.4 min, p=0.049), but there were no differences between groups A and B or between groups B and C. Among the 3 groups, patients in group A received the largest mean volume of water (629±226 mL, 399±197 mL, and 22±35 ml, for groups A, B and C, respectively, p<0.001) (Table 3).
Discussion
The primary outcome of pain score during insertion revealed that both the small and large volume water infusion method significantly reduced pain. The result is in agreement with previous studies of small7–10 or large2–6 volume water infusion method, showing that water infusion could reduce discomfort in patient undergoing colonoscopy under full sedation,7 minimal sedation,4,9 sedation on-demand2,3,8,10 or no sedation.5,6 The results indicate that the water infusion in lieu of air insufflation method is feasible in minimally sedated Asian patients undergoing diagnostic colonoscopy in a community setting, comparable to the findings in Europe8,10 and the US2–7,9.
Our published study showed that the limited volume method significantly reduced colonoscopy pain by 26.5%.1 The result of the current study revealed a 32% reduction by the limited volume method, indicating the result has been reproducible. The reduction of colonoscopy pain with the large volume water infusion was in fact of a somewhat lower order of magnitude (25%) compared with the limited water volume method. The result with the large volume appeared to suggest that the more favorable findings (pain reduction of 50%) in the studies performed on scheduled unsedated US veterans6 was not replicated in Asian patients undergoing minimally sedated diagnostic colonoscopy in a community setting. Thus, while feasible, additional work is necessary to derive maximum benefits, and this will be further discussed below.
Our data showed that the mean pain score during withdrawal was greater in group A than in group B and post procedure bloating was less in group A than in group C. The limited volume water infusion method was associated with less pain during insertion, similar pain during withdrawal, and a trend toward less bloating after the procedure (3.0±2.0 vs. 3.8±2.0, p=0.051) as compared with the air insufflation method. The precise explanation is not fully understood, but is likely related to the varying degrees of colonic distention associated with each method during insertion and withdrawal. The observation suggests that use of water infusion may have an impact on post colonoscopy-related emergency department visit and hospitalization for abdominal pain.11 This hypothesis with potential implications in modifying cost of care definitely should be further evaluated.12
Reports describing the use of large volume water infusion mentioned removal of residual feces obscuring the view by suction2–6 but suction of infused water per se during insertion was otherwise not emphasized. These proof-of-principle studies3,6 showed that water infusion could reduce procedure-related discomfort without compromising the technical performance of the colonoscopy. The insertion times of both the limited and large volume water infusion groups in our study were intended to be kept as short as possible. We were able to navigate through the colon without having to resort to removal of water. Therefore, in order not to devote additional time to suction during insertion, as in other earlier reports.8–10,13 we removed the infused water predominantly during withdrawal in this study.
The prolonged procedure time of the water method in the scheduled unsedated patients without any sedation back up5 is a potential deterrent to the more widespread use of the water method.14 Nonetheless, in the scheduled unsedated patients the deliberate “slow” insertion was associated with unequivocal reduction of pain in the water method group,5,6 proving the principle that not all colonoscopy need to be painful; and painful colonoscopy is more likely due to suboptimal techniques. The insertion and procedure times appeared to be influenced by whether sedation back up is available. As in our current study with minimal sedation (Table 3), others have shown that with minimal sedation or on-demand sedation, the time for cecal intubation with the water method does not need to be excessively prolonged, and in some instances, can be even shorter than the times in the air insufflation group.4,8,9 A large volume of water to be removed during withdrawal will certainly require more time compared with small volume. These considerations highlight the importance of removal of the infused water also during the insertion phase, i.e. diligent application of the water exchange maneuver.15,16
When patients are in the left lateral decubitus position, the ascending colon and proximal transverse colon are in non-dependent areas. Much more water is needed to distend these parts adequately, while a small amount of insufflated air can easily achieve this goal. This appeared to offer an advantage of small, over large volume water infusion. However, the potential disadvantage is elongation of the colon causing increased difficulty in intubation of the cecum, at least in the subgroup of scheduled unsedated patients.5,6 The landmarks at the cecum can be more easily identified with air insufflation because colonoscopists have been trained to do so from the very beginning of their career. Nonetheless, recognition of the appendix opening and red suction marks in the cecum under water are well-described features of cecal intubation.5,6,17,18
The polyp detection rates were similar in our study groups. In the present study, we inspected the mucosa closely as we withdrew the colonoscope in both groups, after opening the lumen adequately with air insufflation and aspirating the residual stool and fluid. Previous studies showed mixed results.5,10,19–21 The reason for the variations is unclear and could be linked to the impaired visibility if the residual feces were not all removed.22,23
In the present study, we infused water at room temperature. Some previous studies used warm water,2–6 while others used water at room temperature.13,22 Church7 showed that warm water minimized colon spasms and decreased patient discomfort. Most of our patients received standard intravenous buscopan before colonoscopy, so we rarely encountered colon spasms. Whether warm water or an antispasmodic is more efficacious warrants further study.
We used a foot-switch controlled water pump to infuse water through the accessory channel of the colonoscope. The cecal intubation time was comparable among the study groups. In contrast, the limited volume water infusion method using a syringe to infuse water in 50 mL aliquots had a significantly longer cecal intubation time (6.4±3.1 vs. 4.5±2.4 min, p<0.001) than the air insufflation method in our previous study.1 The water pump appeared to be more efficient because there was no need to interrupt the examination to infuse the water manually.
Our data highlight a plausible short-coming of removal of the infused water predominantly during withdrawal. While most authors removed the infused water predominantly during withdrawal,7–10,13 one group in the US repeatedly alluded to the removal of residual feces during insertion.2,24 What was not obvious to other investigators when they tried to apply the method2,24 has been clarified - removal of the infused water during insertion or “water exchange” is critical to the success of the large volume water infusion method.15,16 Most recently a review of ten RCTs comparing water-related methods and air insufflation, water exchange has been identified with a greater attenuation of pain during colonoscopy.25 The outcome in our current study might have been improved by the addition of water exchange.
This study has limitations. This was a single-center report and the endoscopists were not blinded to the methods of insertion. In conclusion large volume water infusion without air insufflation appears to be feasible in minimally sedated Asian patients undergoing diagnostic colonoscopy in the community setting. The hypothesis that the addition of the maneuver of water exchange may further improve the outcome deserves to be tested.
Acknowledgement
This study was supported by research funds from Buddhist Dalin Tzu Chi General Hospital.
Abbreviations
- VAS
visual analog scale
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
Disclosure
The authors have no conflicts of interest to disclose.
References
- 1.Hsieh YH, Lin HJ, Tseng KC. Limited water infusion decreases pain during minimally sedated colonoscopy. World J Gastroenterol. 2011;17:2236–2240. doi: 10.3748/wjg.v17.i17.2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leung JW, Mann S, Leung FW. Options for screening colonoscopy without sedation: a pilot study in United States veterans. Aliment Pharmacol Ther. 2007;26:627–631. doi: 10.1111/j.1365-2036.2007.03404.x. [DOI] [PubMed] [Google Scholar]
- 3.Leung JW, Mann SK, Siao-Salera RM, Ransibrahmanakul K, Lim BS, Canete W, et al. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103–110. doi: 10.1016/j.gie.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 4.Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim B, Cabrera H, et al. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009;70:505–510. doi: 10.1016/j.gie.2008.12.253. [DOI] [PubMed] [Google Scholar]
- 5.Leung FW, Aharonian HS, Leung JW, Guth PH, Jackson G. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. 2009;69:546–550. doi: 10.1016/j.gie.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, et al. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 7.Church JM. Warm water irrigation for dealing with spasm during colonoscopy: simple, inexpensive, and effective. Gastrointest Endosc. 2002;56:672–674. doi: 10.1067/mge.2002.128916. [DOI] [PubMed] [Google Scholar]
- 8.Brocchi E, Pezzilli R, Tomassetti P, Campana D, Morselli-Labate AM, Corinaldesi R. Warm water or oil-assisted colonoscopy: toward simpler examinations? Am J Gastroenterol. 2008;103:581–587. doi: 10.1111/j.1572-0241.2007.01693.x. [DOI] [PubMed] [Google Scholar]
- 9.Leung CW, Kaltenbach T, Soetikno R, Wu KK, Leung FW, Friedland S. Colonoscopy insertion technique using water immersion versus standard technique: a randomized trial showing promise for minimal-sedation colonoscopy. Endoscopy. 2010;42:557–562. doi: 10.1055/s-0029-1244231. [DOI] [PubMed] [Google Scholar]
- 10.Radaelli F, Paggi S, Amato A, Terruzzi V. Warm water infusion versus air insufflation for unsedated colonoscopy: a randomized, controlled trial. Gastrointest Endosc. 2010;72:701–709. doi: 10.1016/j.gie.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 11.Leffler DA, Kheraj R, Garud A, Neeman N, Nathanson LA, Kelly CP, et al. The incidence and cost of unexpected hospital use after scheduled outpatient endoscopy. Arch Intern Med. 2010;170:1752–1757. doi: 10.1001/archinternmed.2010.373. [DOI] [PubMed] [Google Scholar]
- 12.Leung FW, Leung JW, Mann SK, Friedland S, Ramirez FC, Olafsson S. DDW 2011 Cutting edge colonoscopy techniques - state of the art lecture master class — warm water infusion/CO2 insufflation for colonoscopy. J Interv Gastroenterol. 2011;1:78–82. doi: 10.4161/jig.1.2.16830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park SC, Keum B, Kim ES, Jung ES, Lee SD, Park S, et al. Usefulness of warm water and oil assistance in colonoscopy by trainees. Dig Dis Sci. 2010;55:2940–2944. doi: 10.1007/s10620-009-1096-6. [DOI] [PubMed] [Google Scholar]
- 14.Wasan SK, Schroy PC., 3rd Water-assisted unsedated colonoscopy: does the end justify the means? Gastrointest Endosc. 2009;69:551–553. doi: 10.1016/j.gie.2008.10.045. [DOI] [PubMed] [Google Scholar]
- 15.Leung FW. Is there a place for sedationless colonoscopy? J Interv Gastroenterol. 2011;1:19–22. doi: 10.4161/jig.1.1.14592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leung FW, Leung JW, Mann SK, Friedland S, Ramirez FC. Innovation Forum - The water method significantly enhances the outcome of colonoscopy in sedated and unsedated patient. Endoscopy. 2011;43:816–821. doi: 10.1055/s-0030-1256407. [DOI] [PubMed] [Google Scholar]
- 17.Ramirez FC, Leung FW. The water method for aiding colonoscope insertion: the learning curve of an experienced colonoscopist. J Interv Gastroenterol. 2011;1:97–101. doi: 10.4161/jig.1.3.18507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedland S, Leung FW. Learning and teaching the water method (with videos) J Interv Gastroenterol. 2011;1:127–129. doi: 10.4161/jig.1.3.18511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leung JW, Do L, Siao-Salera RM, Parikh DA, Mann SK, Leung FW. Retrospective data showing the water method increased adenoma detection rate — a hypothesis generating observation. J Interv Gastroenterol. 2011;1:3–7. doi: 10.4161/jig.1.1.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leung FW, Leung JW, Siao-Salera RM, Mann SK. The water method significantly enhances proximal diminutive adenoma detection rate in unsedated patients. J Interv Gastroenterol. 2011;1:8–13. doi: 10.4161/jig.1.1.14587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leung FW, Leung JW, Siao-Salera RM, Mann SK, Guy Jackson G. The water method significantly enhances detection of diminutive lesions (adenoma and hyperplastic polyp combined) in the proximal colon in screening colonoscopy - data derived from two RCT in US veterans. J Interv Gastroenterol. 2011;1:48–52. doi: 10.4161/jig.1.2.16826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamamoto N, Nakanishi Y, Morimoto N, Inoue H, Tatukawa M, Nakata S, et al. A new water instillation method for colonoscopy without sedation as performed by endoscopists-in-training. Gastrointest Endosc. 2002;56:825–828. doi: 10.1067/mge.2002.129608. [DOI] [PubMed] [Google Scholar]
- 23.Friedland S. The water immersion technique for colonoscopy insertion. Gastroenterol Hepatol. 2010;6:555–556. [PMC free article] [PubMed] [Google Scholar]
- 24.Leung FW. Water-related method for performance of colonoscopy. Dig Dis Sci. 2008;53:2847–2850. doi: 10.1007/s10620-008-0259-1. [DOI] [PubMed] [Google Scholar]
- 25.Leung FW, Leung JW, Siao-Salera RM, Mann SK, Ramirez FC, Friedland S, et al. Removal of infused water predominantly during insertion (water exchange) is consistently associated with a greater reduction of pain score — review of data in randomized controlled trials (RCTs) of water method colonoscopy. Abstract submitted to 2011 Asian Pacific Digestive Week meeting. doi: 10.4161/jig.1.3.18510. [DOI] [PMC free article] [PubMed] [Google Scholar]


