Abstract
Epidemiological studies have found that young men who have sex with men (YMSM) represent the majority of young people infected with HIV annually in the U.S. Further, they are one of the few risk groups to show an increase in the rate of infections in recent years. In addition to these disparities in prevalence and infection rates, there is an inequity in prevention and intervention research on this population. The purpose of this article is to review the existing YMSM literature on HIV epidemiology, correlates of risk, and intervention research. We conclude that promising future directions for basic research include a focus on multiple clustering health issues, processes that promote resiliency, the role of family influences, and the development of parsimonious models of risk. In terms of intervention research, we suggest that promising future directions include Internet-based intervention delivery, integration of biomedical and behavioral approaches, and interventions that go beyond the individual level to address partnership, structural, community, and network factors.
In the U.S. in 2006, an estimated 56,300 people became infected with HIV, and of these, approximately one third were adolescents or young adults (Hall et al., 2008). HIV disproportionally affects specific groups of young people, with over two-thirds of infections in youth (ages 13-24) in 2008 resulting from male-to-male sexual contact (CDC, 2009c). Although this at-risk group of young men who have sex with men (YMSM) face an increased HIV-burden, there is a relative dearth of research and interventions targeting HIV-prevention among YMSM. The aim of this paper is to help address this inequity by reviewing and synthesizing the literature on HIV epidemiology, correlates of HIV risk, and existing interventions, to advance research and the creation of effective interventions for YMSM. We further describe a framework for understanding and intervening on HIV risk among YMSM and promising directions for future research. This review primarily includes data from Western countries and mostly from the U.S., given that the YMSM literature is in its nascence, especially in countries where YMSM remain invisible because of fear of discrimination, stigmatization, assault, or even arrest. Indeed, sex between men is illegal in 78 countries (Ottosson, 2010). We include discussion of research in other countries when possible.
Definitional Issues
Disagreement exists in approaches to labeling men who engage in same-sex behavior, have same-sex attractions, or identify as members of communities organized around these attractions and behaviors. Identity labels can include gay, bisexual, homosexual, and queer, among others. These labels may be unsatisfactory to researchers and individuals who object to these specific words, labels in general, or identifying with this community despite same-sex behaviors and attractions. Some researchers have sought to avoid these common sexual identity labels by using a parallel to the phrase “racial minority” and describing the sample as “sexual minority.” While the use of “sexual minority” seems to be increasing, particularly in research with youth, it has not become widely adopted by the public. The phrase “men who have sex with men” or the widely adopted acronym “MSM” is a behavioral categorization that emerged in the HIV literature in the early 1990s and has subsequently become more widely adopted. Ostensibly, the term was coined to identify a group of men at elevated HIV-transmission risk due to behavioral risk factors. Prior to “MSM,” identity labels excluded men who engaged in same-sex sexual behavior but who did not identify as gay or bisexual. Although the distinction that it is behavior, and not identity, that puts one at risk for HIV infection is imperative, the widening use of the “MSM” label has been criticized for ignoring social dimensions of sexuality that are critical to understanding sexual health (Young & Meyer, 2005).
This debate about labels is not purely academic, as research has shown that same-sex attractions, behaviors, and identity labels are not entirely overlapping and are differentially related to some outcomes, such as mental health (Savin-Williams, 2006). Because our review focuses on HIV risk, which results from behavior, not identity or attractions, we found most studies described their participants as MSM. We therefore defer to that label, while acknowledging the heterogeneity of identities that may be included.
What is meant by “young” or “youth” must also be defined, as these are not well delineated and universally accepted age groupings. The U.S. CDC often includes the age range of 13 – 24 in their reports on youth and young people (e.g. CDC, 2009b; CDC, 2009d). This age range spans the developmental periods of adolescence to emerging adulthood. Adolescence is generally broadly considered the period of life from puberty to “maturity” (Behrman, Kliegman, & Jenson, 2004). The term “emerging adulthood” (Arnett & Tanner, 2006) has been used to capture the period during which individuals are “too old” to be adolescents (~18), but not “old enough” to be adults (~mid-20’s).
Another key definitional issue is what is meant by “HIV risk.” Globally and in the U.S., HIV is primarily transmitted through sexual behavior. For example, among young men in the U.S., less than 5% of transmissions are categorized as being due to non-sexual behaviors like injection drug use (CDC, 2009c). As a result of this, “sexual risk taking” is sometimes used in the literature interchangeably with “HIV risk.” Obviously there can be consequences of sexual risk taking other than HIV, such as other sexually transmitted infections (STI). Similarly, not all unprotected sex puts one at risk for HIV, because the virus can only be transmitted if it is present in someone engaging in the sexual interaction. Even if a condom is used, high rates of condom errors among YMSM (DuBois, Mustanski, & Emerson, 2010) mean HIV transmission could occur in the context of user error, making condom use not always equivalent to “protected sex.” Further complicating matters, not all sexual contact is equivalent in potential for viral transmission, leading most HIV researchers to focus predominately on unprotected anal sex in research with MSM. In our literature review we included both anal sex and other sexual acts as potential HIV transmission behaviors. To distinguish between these, we generally defer to the descriptors “UAI” to indicate unprotected anal intercourse and “sexual risk” to indicate more general outcomes.
In this review we describe main effects, as well as mediating and moderating effects. Therefore we offer definitions of these terms. Frazier, Tix, and Barron (2004) describe moderators as explaining “when” or “for whom” a variable relates to an outcome, whereas mediators address “how” or “why” one variable influences another. Stated in different terms, moderators address the interaction of variables, or how one variable might depend on the level of another, and mediators examine the mechanism through which an independent variable influences an outcome variable (Baron & Kenny, 1986; Frazier, Tix, & Barron, 2004).
Approach to performing literature review
To our knowledge, no prior reviews have been conducted on HIV risk specific to the YMSM population. As such, our review of the literature includes all studies conducted on sexual risk in YMSM without limits on publication date. However, the primary aims of the article were to review the epidemiology of HIV in YMSM, describe the factors associated with sexual risk in this population, and provide recommendations for future research to better understand sexual risk in YMSM. To achieve these, we have emphasized more recent studies. The review also emphasized studies that investigated correlates of sexual risk in which the sample was entirely or primarily composed of YMSM. In many cases this limited our ability to describe potential risk factors that have been well studied in adult MSM and have potentially generalizable affects to YMSM. In those cases, the appropriate studies on adult MSM were cited and clearly demarcated. Studies in which the sample was not exclusively composed of MSM (or did not provide separate analyses for MSM and non-MSM) were rarely included in the review. However, in some cases we referenced research on heterosexual adolescents – when we compared them to YMSM or when no similar research was available on YMSM. We did not include studies that were not conducted or published in the English language. Literature search was conducted using the PubMed database with key terms for MSM (“MSM”, “YMSM”, “gay”, or “bisexual”), sexual behavior and/or risk (“HIV” or “sex”) and youth (“teen”, “youth”, “adolescent”, or “adolescence”). Initial literature search returned 1,688 citations. We reviewed each article’s abstract, finding 313 articles that were relevant to YMSM and HIV and considered for inclusion in the review.
Methodological Considerations in Research on YMSM
The majority of studies of MSM start their sample at age 18 (Mustanski, 2011), and with very few exceptions the youngest participants in studies of MSM are 15-16 years old (Choi, Han, Hudes, & Kegeles, 2002; Guenther-Grey et al., 2005; Mustanski, Garofalo, & Emerson, 2010; Mustanski, Garofalo, Herrick, & Donenberg, 2007; Remafedi, 2002; Valleroy, MacKellar, & Karon, 2000; Warren et al., 2007). The inclusion of YMSM under age 18 is critical to understanding HIV risk among YMSM, as many risk factors (e.g. substance use, sexual behavior, etc.) emerge during the transition from adolescence to emerging adulthood. Because the initiation of these behaviors may occur in the mid-teens (Garofalo, Wolf, Kessel, Palfrey, & DuRant, 1998), it may seem advisable to begin studying YMSM earlier than age 16. However, research on the age of psychosexual milestones among YMSM indicates that most have not disclosed their same-sex attractions or LGBT identity until around age 16 (D’Augelli, Hershberger, & Pilkington, 1998; Grov, Bimbi, Nanin, & Parsons, 2006; Savin-Williams & Diamond, 2000). Thus it is difficult to recruit a sample significantly younger than this age. This may change as social acceptance and research policy continue to evolve. While there are clear benefits in studying MSM under age 18, most studies have not included minors. This is partially due to local Institutional Review Board (IRB) policies or review approaches that create significant obstacles for investigators to conduct research to improve the health of this group (Mustanski, in press).
Research with adolescent and emerging adult MSM is necessary to address the growing HIV epidemic in this population. Studies of older MSM are insufficient in this regard, for a number of reasons. First, in the U.S., there are typically significant developmental changes in one’s life around age 18 (Arnett, 2000). At this time many young people move out of their parents’ home, dramatically changing the effect of parental influence (e.g. Mustanski, Newcomb, & Garofalo, 2011). Similarly other important life transitions are occurring in the domains of relationships, work, and education. Second, brain development continues through late adolescence, particularly the brain’s cognitive control system that improves capacity for self-regulation (Steinberg, 2008). Research suggests that during adolescence, neural mechanisms may lead to heightened responsiveness to both reward and emotional cues, while capacities for behavioral and emotional regulation are still relatively immature (Somerville, Jones, & Casey, 2010). Similarly, owing to brain development, drug and alcohol consumption during adolescence can have differential and more deleterious effects on behavior and brain injury than consumption in adulthood (e.g. Spear, 2002). Third, recall of past sexual events is subject to a number of forms of recall bias, such as telescoping and forgetting (Croyle & Loftus, 1993). Therefore retrospective accounts from older MSM may be biased. Fourth, the rapid change in the social status of homosexuality (Loftus, 2001) means even accurate retrospective reports of a current 18 year old may not match the current experiences of a younger person. These developmental factors and limitations of using older MSM to understand risk in adolescence suggest that accurately understanding risk and resiliency processes in YMSM requires the inclusion of participants under the age of 18.
In addition to the limitation that the majority of research on MSM starts at age 18, most studies of YMSM have also relied on relatively small samples with unknown representativeness, including convenience samples, snowball samples, or samples recruited from specific locations frequented by some MSM. Sampling issues have plagued research on LGBT populations for decades, because there is no established sampling frame to use for establishing external validity (Meyer & Wilson, 2009). A few rare exceptions have used probability sampling methods, including representative school-based samples that have included questions about sexual orientation or same-sex behaviors (e.g. Garofalo et al., 1998) and nationally representative samples (e.g. Russell, Driscoll, & Truong, 2002). However, these studies have focused on health issues other than HIV.
Epidemiology
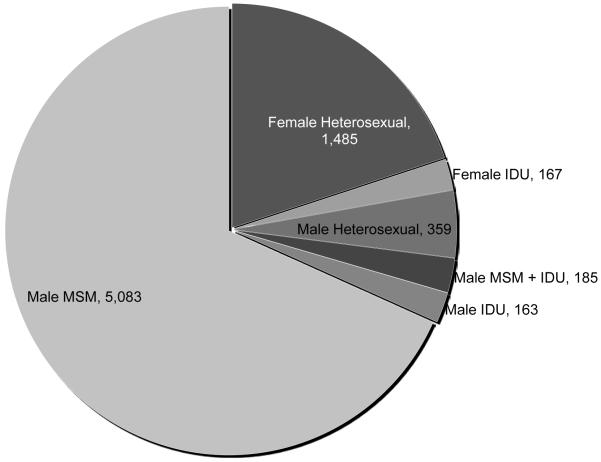
As shown in Figure 1, in the U.S., 68% of cases of HIV infection among all young people aged 13-24 in 2008 were among YMSM (CDC, 2009c). These data represent diagnoses among individuals who are tested, but to estimate the incidence rate requires knowing the size of the YMSM population. Based on a review of the literature, CDC scientists estimate the population proportion of MSM by recall period: 2.6% in past year, 4% in past five years, and 7% ever (Purcell et al., 2010). The 4% estimate led to an estimated HIV diagnosis rate among MSM that was 60 times the rate in other men and 54 times the rate in women. Studies of youth and young adults suggest similarly that somewhere between 3-5% of young men have had sex with another male (Savin-Williams, 2006). In terms of HIV prevalence among YMSM, the largest study conducted to-date was the CDC’s 1994-2000 survey of 3,492 15- to 22-year-old urban MSM in 7 US cities, which found an overall HIV prevalence of 7.2% (Valleroy et al., 2000). A more recent study of MSM in 21 U.S. cities conducted in 2008 reported 7% HIV prevalence in 18-19 year olds (N = 423) and 12% in 20-24 year olds (N = 1,466) (CDC, 2010c). In addition to an existing disparity in HIV prevalence, from 2001 – 2006 MSM were the only transmission group in the U.S. associated with an increasing number HIV diagnoses (CDC, 2008). There is similar evidence of a resurgence of the HIV epidemic among MSM in other western countries (Sullivan, Hamouda, et al., 2009), and in low- and middle-income countries (Baral, Sifakis, Cleghorn, & Beyrer, 2007). Interestingly, in their review of the global HIV epidemic, Baral and colleagues found that the disparity in HIV between MSM and the general population differed according to the background HIV prevalence; MSM were 58.4 times more likely to have HIV in very low-HIV prevalence countries, 14.4 times more likely in low-HIV prevalence countries, and 9.6 times more likely in medium-to high-HIV prevalence countries. This implies that that the more generalized the epidemic, the less the disproportionate burden among MSM. Globally very little is known about HIV disparities specifically among adolescent MSM.
Figure 1.
CDC estimated numbers of diagnoses of HIV infection among adolescents and young adults ages 13-24 years, by transmission category, in 37 States and 5 U.S. Dependent Areas with confidential name-based reporting, 2008.
Notes: Graph created by authors using data reported by the CDC (2010b). MSM = Male-to-male contact. IDU = Injection Drug Use. MSM + IDU = individual in both MSM and IDU transmission risk categories. Data from 3 youth with “other” cause of infection were removed to increase clarity of graph.
Racial disparities in HIV prevalence are nested on top of these other disparities among MSM. In the U.S., White MSM represent a greater number of new HIV infections than any other group, with most infections occurring in 30-39 year olds (CDC, 2010). However, the primary age at which MSM become infected differs by race. Most new infections in Black MSM occur among 13-29 year olds, with more Black MSM in this age group becoming infected than any other age and racial group (CDC, 2010). Specifically, of all MSM aged 13-24 in 2006, Blacks were more than twice as likely than Whites or Hispanics to be diagnosed with HIV or AIDS (CDC, 2008). Of all demographic subgroups, Black YMSM also showed the most dramatic increase in diagnoses—93% from 2001 to 2006 (CDC, 2008). Among Hispanic MSM, most new infections also occur at younger ages, although the age differences are not as pronounced as those in Black MSM (CDC, 2010). The reasons for these racial disparities are not well understood, as numerous studies have produced the paradoxical finding that on average Black YMSM report similar or lower rates of unprotected sex, condom errors and failures, and drug using behaviors than White YMSM (Clerkin, Newcomb, & Mustanski, 2010; DuBois et al., 2010; Garofalo, Mustanski, Johnson, & Emerson, 2010; Harawa et al., 2004; Ruiz, Facer, & Sun, 1998). This has led some to conclude that sexual network characteristics instead of individual behaviors are likely to account for these racial disparities (Clerkin et al., 2010; Harawa et al., 2004; Millett, Flores, Peterson, & Bakeman, 2007). Some individual-level risk processes have been found to differ by race in YMSM (Garofalo et al., 2010; Warren et al., 2007). For example, one study found that for only Black YMSM, being in a long-term relationship, having been kicked out of the home for having sex with men, and younger age of initiation of sexual behavior were associated with unprotected sex (Warren et al., 2007). These patterns unarguably call for greater attention focused on HIV prevention among Black YMSM. At the same time there is also unmet need for prevention programming with White and Latino YMSM. For example, in the U.S. in 2006 there were as many White and Latino MSM (ages 20-24) who were diagnosed with HIV as young women across all racial/ethnic groups (1,000 versus 1,046; (CDC, 2009d). Whereas there has been significant research and prevention work focused on young women in the U.S., there has been much less among YMSM of any racial/ethnic group.
Another important aspect of HIV epidemiology among YMSM is the prevalence of unrecognized infections. In the general U.S. population, it is estimated that 21.0% of those who were HIV positive were undiagnosed in 2006 (Campsmith, Rhodes, Hall, & Green, 2010). In this study, the frequency of undiagnosed infections was substantially higher among youth (47.8%) and slightly, but significantly, higher among MSM (23.5%) and lower in Whites (18.8%). Among YMSM however, there is an alarming percentage who do not know they are HIV infected. In a large urban YMSM sample, 77% of those 15-29 that tested positive in the study mistakenly believed they were not infected. Among Black YMSM this number was 90% (MacKellar et al., 2005).
Correlates and Predictors of Sexual Risk Taking in YMSM
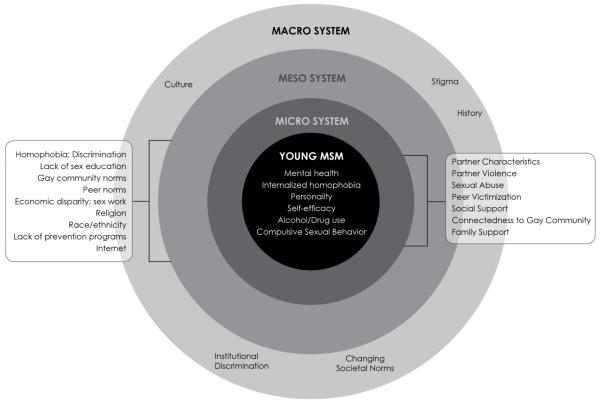
Correlates and predictors of sexual risk taking in YMSM can serve the purpose of identifying behavioral targets for prevention programs and also individuals who may be at relatively high risk for infection. This research has included factors at multiple levels, including individual characteristics, peer influences, intimate partner dyads, family factors, societal factors, and structural characteristics. As an organizational framework for this literature we utilize Bronfenbrenner’s (1979) ecological theory of development, which describes a multi-systemic model of child development that nests the individual within increasingly broad systems that influence the child either directly or indirectly, by shaping the environment. This model has been applied widely in prevention research with youth (O’Connell, Boat, & Warner, 2009). In this model, the microsystem is comprised of the relationships or contexts with which the child has direct contact, including romantic relationships, friendships and peer groups, and family relationships. Bronfenbrenner describes the relationships at this level as bi-directional (i.e, the child simultaneously has an influence on and is influenced by the individuals in his microsystem). The mesosystem includes the interrelations between the major settings in which the youth finds himself, and subsequently the impact of these interrelations upon the youth. Major settings in the mesosystem include local economy and work environment, government, religion, neighborhood, and mass media. At the broadest level, Bronfenbrenner describes the macrosystem, or the overarching structural or societal norms. These norms are described as “blueprints” that influence multiple aspects of the individual’s life and may be expressed at the ideological level or via written laws. We review the literature on correlates of sexual risk taking in YMSM in a manner consistent with Bronfenbrenner’s model; we begin with person-level factors and then describe factors contained in the external levels of his model.
Person-Level Factors
Drug Use
In comparison to their heterosexual counterparts, YMSM are more likely to use a variety of different substances (including alcohol and illicit drugs), to initiate drug use at an earlier age, and to experience more rapid increases in substance use over time (Garofalo et al., 1998; Marshall et al., 2008; Marshall et al., 2009). For example, in a sample of club attending 18-29 year olds stratified by sex and sexual orientation, Parsons, Grov, and Kelly (2009) found that YMSM were most likely to have ever used GHB and Methamphetamine, but were less likely to have used LSD. YMSM are more likely than older MSM to engage in heavy alcohol and drug use (Salomon et al., 2009). Within YMSM, Blacks and Latinos under 21 are less likely to use illicit drugs than Whites (Harawa et al., 2004; Kipke et al., 2007). In a very large study of YMSM, 66% of the 15-22 year-olds reported illicit drug use in the six months prior to the interview, 29% used drugs on a regular basis, and 28% reported polydrug use (Thiede et al., 2003). YMSM may be at particularly high risk for engaging in risky sexual behavior while under the influence of drugs; because of developmental factors they may be less able to monitor and moderate the effects of these substances.
In measuring drug use as a correlate of sexual risk, studies have operationalized drug use in a variety of ways. Some studies measured drug use as “any drug use,” while others focused on differentiating between categories of drugs (e.g., “stimulants” or “club drugs”) or differentiating between individual substances. Additionally, this association has been examined in some studies by measuring drug use as a global behavior variable (i.e., average rates of use within a given time period), while others have mapped drug use directly onto a sexual encounter (i.e., “drug use prior to last sex” or “being high during sex”). Studies examining the global association between “any drug use” and sexual risk in YMSM generally point to a positive association between these variables (Hays, Kegeles, & Coates, 1997; Meyer & Dean, 1995; Remafedi, 1994; Rosario, Scrimshaw, & Hunter, 2006; Rotheram-Borus, Rosario, Reed, & Koopman, 1995). Similarly, studies examining “drug use prior to sex” or “being high during sex” have found a positive association between these and sexual risk (Newcomb, Clerkin, & Mustanski, in press; Stueve, O’Donnell, Duran, San Doval, & Geier, 2002).
In terms of differentiating between classifications of drugs, “club drugs” have received the most attention in the last decade as correlates of sexual risk in YMSM. While definitions of club drugs differ somewhat, they are generally considered to be stimulants and hallucinogens, including ecstasy/MDMA, amphetamines (including methamphetamine), nitrates/poppers, ketamine, GHB, and cocaine. Studies have consistently found a positive association between the use of club drugs and UAI in general MSM populations (for a review see Drumright, Patterson, & Strathdee, 2006). Moreover, club drug use is high amongst urban YMSM. In a recent survey, 40% of YMSM (ages 18 to 22) reported lifetime use of club drugs, with 56% of these lifetime users reporting club drug use in the past three months and 40% reporting use in the past 30 days (Kipke et al., 2007). Polydrug use (i.e., the consecutive or simultaneous use of two or more substances) is an important emerging health issue among club drug using urban YMSM (Grov, Kelly, & Parsons, 2009). Evidence suggests that club drugs have played a role in recent increases in HIV/STI prevalence, particularly in YMSM populations in several urban centers (Clatts, Goldsamt, & Yi, 2005a, 2005b; Garofalo, Mustanski, McKirnan, Herrick, & Donenberg, 2007b; Stueve, O’Donnell, Duran, San Doval, & Geier, 2002; Waldo, McFarland, Katz, MacKellar, & Valleroy, 2000). Earlier studies pointed to a strong association between cocaine use and sexual risk in YMSM over and above the use of other club drugs (McNall & Remafedi, 1999; Molitor et al., 1999; Weber et al., 2001). However, more recent studies have highlighted the strong association between using amphetamines (including methamphetamine) and UAI in YMSM (Celentano et al., 2006; Garofalo et al., 2007; Waldo et al., 2000).
Several studies have examined the association between other types of drug use and sexual risk. Marijuana has gained some attention as a potential correlate of sexual risk in both youth and adult samples of MSM. Although fewer studies have been conducted on marijuana use as a correlate of risk as compared to club drugs, research generally supports a positive association between marijuana use and sexual risk in both YMSM (Celentano et al., 2006; Mustanski et al., 2007) and adult MSM (Clutterbuck, Gorman, McMillan, Lewis, & Macintyre, 2001; Drumright, Little, et al., 2006; Hirshfield, Remien, Humberstone, Walavalkar, & Chiasson, 2004). Research on adult MSM samples points to a positive association between the recreational use of Viagra and other erectile dysfunction drugs and sexual risk (Hirshfield et al., 2004; Kim, Kent, & Klausner, 2002; Mansergh et al., 2006; Nettles, Benotsch, & Uban, 2009; Ostrow et al., 2009). To our knowledge, erectile dysfunction drugs have not been examined as a correlate of sexual risk in YMSM. Evidence suggests that the recreational use of these drugs is not common in YMSM (Kipke et al., 2007). But, it remains unclear whether using these drugs is more prevalent among YMSM compared to heterosexual young men.
For both young and adult MSM, evidence suggests that the association between drug use and sexual risk differs based on situational variables associated with the sexual encounter (Drumright, Little, et al., 2006; Stueve et al., 2002). One such situational variable that may moderate this association is partner type (i.e., primary vs. casual partners). In general, the literature points to a stronger positive association between drug use and sexual risk with casual partners, particularly when these partners are serodiscordant or of unknown HIV status. Few studies have examined this moderating effect specifically in YMSM. In one notable exception, Stueve and colleagues (2002) found that YMSM who were “high” on either drugs or alcohol during their most recent sexual encounter had increased odds of unprotected receptive anal intercourse during this encounter if the partner was a casual partner, but not for main partners.
Other studies have examined whether the association between drug use and sexual risk differs based on the sex role adopted by the individual (i.e., insertive or receptive role in anal sex). One cross-sectional study, with a large sample (N = 3,492) of YMSM ages 15 to 22, found that certain drugs were associated with increased odds of unprotected receptive anal intercourse while others were associated with increased odds of unprotected insertive anal intercourse (Celentano et al., 2006). In this study, being under the influence of marijuana during sex was associated with increased odds of engaging in unprotected receptive anal intercourse only. Being under the influence of alcohol, amphetamines, or cocaine was associated with increased odds of engaging in unprotected receptive or insertive anal intercourse. Adult MSM studies have found recreational use of erectile dysfunction drugs was more strongly associated with unprotected insertive anal intercourse than receptive (Mansergh et al., 2006). However, like general research on erectile dysfunction drugs among YMSM, this association has not been studied in YMSM.
Overall, the literature on sexual risk in YMSM points to a positive association between drug use and UAI, particularly for “club drugs.” This association appears stronger when engaging in sex with casual versus primary partners. There is also some limited evidence that certain drugs may be more strongly associated with unprotected receptive anal intercourse compared to insertive, or vice versa (Celentano et al., 2006), although this has not been studied extensively in YMSM. Future research on the association between drug use and sexual risk should focus on disentangling which drugs put YMSM at most risk for engaging in UAI. There is considerable evidence pointing to a particularly strong link between methamphetamine use and UAI in adult MSM (Grov, Parsons, & Bimbi, 2008; Halkitis, Green, & Mourgues, 2005; Halkitis, Mukherjee, & Palamar, 2009; Halkitis, Parsons, & Stirratt, 2001; Nanin, Parsons, Bimbi, Grov, & Brown, 2006). However, fewer studies have been conducted on differential associations between use of specific drugs and UAI among YMSM. Research should also investigate whether certain drugs place YMSM at increased risk for unprotected sex in insertive versus receptive roles.
Alcohol Use
Several large surveys have found that compared to heterosexual youth, non-heterosexual youth report earlier initiation, and more frequent use, of alcohol (Blake et al., 2001; Corliss et al., 2008; Marshal et al., 2009). Non-heterosexual youth also report steeper drinking trajectories into young adulthood, compared to heterosexual youth (Hatzenbuehler, Corbin, & Fromme, 2008; Marshal et al., 2009). Further, research in the late 1990’s indicated that both alcohol and substance use had increased significantly among YMSM during that decade (McNall & Remafedi, 1999). Given these elevated rates of alcohol use in YMSM, it is critical to understand whether this behavior is associated with elevated rates of sexual risk taking in this population.
Alcohol use is one of the more frequently studied correlates of risky sex in both general populations and MSM. Accordingly, a number of theoretical models have been proposed to explain why alcohol use may be associated with failure to use condoms. For example, Steele and Josephs’ (1990) alcohol myopia theory posits that sexual risk taking is more likely when under the influence of alcohol because the psychoactive properties of alcohol intoxication limit cognitive capacity. With less cognitive capacity available, the individual has difficulty attending to the negative consequences of risky sexual behavior. Instead, the individual focuses on something that requires fewer cognitive resources – the most salient aspects of the situation, including engaging in the desired sexual activity. Another influential model, alcohol expectancy theory, posits that the mere belief that alcohol intoxication causes individuals to alter their sexual behavior is enough to influence risky sexual behavior (Dingle & Oei, 1997). Finally, McKirnan and colleagues’ (1996) cognitive escape theory proposes a more active process by which individuals strategically engage in alcohol and drug use to avoid thoughts about personal risk for HIV acquisition.
Multiple theoretical models notwithstanding, the association between alcohol use and risky sex is inconsistent, in both general and MSM populations, as well as within and across methodological approaches. Global association studies examine average rates of alcohol and condom use and make behavioral comparisons between-persons. Research using this methodology has found positive associations between risky sex and alcohol use in YMSM (Hirshfield et al., 2004; Stall & Purcell, 2000) as well as no significant associations (Choi, Operario, Gregorich, et al., 2005; McNall & Remafedi, 1999; Waldo et al., 2000). An important limitation of this methodology is that failing to map an episode of alcohol consumption directly onto an episode of sexual risk taking renders it difficult to make causal inference. Furthermore, alcohol use varies within-persons over time and across sexual encounters (Newcomb et al., In Press), and it is possible to find that certain variables predict risk between-persons while not predicting risk behaviors within-persons (Leigh, Vanslyke, & Hoppe, 2008; Mustanski, 2007a).
Others have examined this relationship using an event-specific approach in which alcohol use and sexual risk are mapped onto a single sexual encounter. Reviews of studies using this approach in general samples have concluded that alcohol use is not significantly related to condom use at last sex (Cooper, 2002; Leigh, 2002). Conversely, one YMSM study found that UAI was more likely during sexual encounters in which participants reported being “high” on alcohol (Stueve et al., 2002). Mustanski (2008) noted that when assessing only one sexual encounter it is not possible to disentangle stable personality characteristics from situational correlates of risk. Event-specific analyses of multiple occasions of alcohol use and sex in the same person over time improve on this approach by comparing a participant’s behavior across multiple situations, thereby controlling for between-person effects (i.e., the person serves as his/her own control by comparing behavior across multiple events). This type of analysis has been conducted using both retrospective accounts of behavior and prospective daily diaries. Both of these approaches have yielded mixed results in MSM. Although some of these studies have found positive associations between alcohol use and sexual risk in adult MSM (Colfax et al., 2004; Kalichman, Tannenbaum, & Nachimson, 1998b; Mustanski, 2008), these results have not been replicated consistently (Gillmore et al., 2002; Vanable et al., 2004; Weatherburn et al., 1993). Mustanski (2008) used a daily diary approach to examine age as a moderator of the relationship between alcohol consumption and risky sex in a sample of MSM ages 18 and older. Findings from this event-level analysis indicated that age moderated the relationship between these two variables, such that alcohol had significantly greater effects on risky sex in older MSM. Contrary to Mustanski’s findings, a meta-analysis of event-level studies in heterosexual populations found that alcohol use was related to risky sex for younger but not older participants (Leigh, 2002). These inconsistencies highlight the importance of further investigating the role that alcohol plays in sexual risk in YMSM.
Some evidence suggests that differences in personality characteristics and cognitive processes may influence which individuals will increase their risk-taking under the influences of alcohol and drugs. Particularly, sensation seeking has received significant attention because it is well-replicated as a correlate of substance use and sexual risk taking (Bancroft et al., 2003; Hittner & Swickert, 2006; Zuckerman, 1994). Research suggests that sensation seeking both mediates (Kalichman et al., 1998) and moderates (Newcomb et al., in press) the relationship between alcohol use and risky sexual behavior in MSM. In other words, sensation seeking partially explains the association between alcohol use and risky sexual behavior, and in addition alcohol has a greater impact on sexual behavior among those reporting high sensation seeking.
Sexual enhancement expectancies (i.e., the belief that alcohol and drugs will enhance sexual experiences) have also been proposed as a cognitive process that explains why some, but not all, individuals exhibit a positive association between alcohol use and sexual risk. Several studies have found an association between this cognitive dimension and sexual risk in adult MSM (Bimbi et al., 2006; Kalichman, Tannenbaum, & Nachimson, 1998a). These studies suggest alcohol expectancies may be a proximal determinant of which MSM engage in sexual risk while under the influence of alcohol. Unfortunately, to our knowledge no YMSM-specific studies have examined the relationship between alcohol use expectancies and sexual risk while under the influence.
Given the current state of the literature, it remains unclear how alcohol relates to sexual risk in YMSM and what mechanisms may underlie such an association. To better understand this relationship in YMSM, future research should examine within-persons variability in alcohol use and sexual behavior across multiple sexual encounters. Research should also focus on determining whether there is a positive association between alcohol use and sexual risk in certain groups of YMSM but not others, and whether or not third variables moderate this association.
Personality Characteristics
In addition to situational factors such as substance use, more enduring personality traits also may influence sexual risk among YMSM (e.g. Dudley, Rostosky, Korfhage, & Zimmerman, 2004). While stable personality characteristics are unlikely to serve as direct intervention targets (due to limited approaches to change personality), personality factors can be useful in identifying who is most likely to engage in HIV risk behaviors. Consequently, interventionists can target these at-risk individuals with prevention programs (Hoyle, Fejfar, & Miller, 2000) and tailor content to user personality characteristics (Donohew et al., 2000).
Past researchers have used psychobiological (e.g., Eysenck’s PEN) and taxonomic (e.g., Five-Factor) models to select specific personality variables to test as sexual risk correlates (Hoyle et al., 2000). Here we review several individual personality variables that have theoretical justification and empirical support for relating to sexual risk among YMSM. These include sensation seeking, impulsivity, and related constructs, as well as constructs from several major models of personality: openness, conscientiousness, and agreeableness from the Five-Factor Model, psychoticism from the PEN model, and from both models, extraversion and neuroticism.
Sensation seeking is defined as “the propensity for an individual to seek optimal arousal and sensory stimulating experiences” (Kalichman et al., 1998). Sensation seeking has received more attention than any other personality variable in the sexual risk literature; Hoyle et al. (2000) found that 64% of all studies investigating personality traits and sexual risk included sensation seeking as an independent variable. Theoretically, high sensation seekers are more likely to engage in sexual risk than low sensation seekers, because they have a greater value for high-risk activities and a higher threshold for determining what is subjectively “risky” (Hoyle et al., 2000). Empirically, research relates sensation seeking to sexual risk outcomes in various populations, including adolescents (Newcomb & McGee, 1991), MSM (Dolezal, Meyer-Bahlburg, Remien, & Petkova, 1997; Kalichman & Rompa, 1995), and YMSM (Dudley et al., 2004). However, the pattern of findings regarding the association between sensation seeking and sexual risk among YMSM is not wholly consistent. In a sample of YMSM, Newcomb et al. (2010) found no significant main effect of sensation seeking on the rate of UAI. However, sensation seeking did moderate the relationship between substance use and the rate of UAI, such that higher levels of sensation seeking increased the positive associations between UAI frequency and substance use prior to sex. In another study of YMSM, sensation seeking was correlated with two measures of sexual risk. However, when placed into a hierarchichal regression model after other variables such as demographics, substance use, and dating status, sensation seeking no longer significantly related to UAI (Dudley et al., 2004). Similarly, among adult MSM the relationship between sensation seeking and sexual risk has been inconsistent; two studies reported a significant association (Bancroft et al., 2003; Kalichman, Heckman, & Kelly, 1996), while one did not (McCoul & Haslam, 2001). This inconsistency in findings may be attributable to sensation seeking primarily influencing sexual risk behavior by increasing exposure to various situational influences (e.g. alcohol use, as aforementioned). In this case, the relationship between sensation seeking and sexual risk behavior would be highly dependent on the specific sample characteristics regarding exposure to various contexts and situations.
Research has been conducted on the relationship between sexual risk and a related set of constructs – impulsivity, sexual impulsivity, and impulsive decision-making. Impulsivity has been defined multiple ways, with most definitions referring to acting without thinking or considering the consequences of the action. One YMSM study found impulsive decision-making related significantly to UAI frequency beyond other related factors, including number of anal sex partners and partner HIV status (Dudley et al., 2004). Another study, of HIV positive and negative young adult MSM, found that sexual impulsivity was associated with UAI (Hays, Paul, Ekstrand, et al., 1997). Finally, in a sample of adult HIV positive MSM, sexual impulsivity related to UAI with serodiscordant or unknown status partners (Semple, Patterson, Grant, 2000).
Personality dimensions from the Five Factor Model (openness, conscientiousness, and agreeableness; e.g., Goldberg, 1993), the PEN model (psychoticism; e.g., Eysenck, 1990) and those in both models (extraversion, neuroticism) also have been investigated as they relate to sexual risk. Several constructs from these models have been linked to sexual risk-taking, as reported in reviews by Crepaz and Marks (2001) and Hoyle et al. (2000) – low conscientiousness, low agreeableness, and somewhat unreliably, high neuroticism. Notably, few studies of sexual risk and the Five Factor or PEN Model variables have focused on MSM or YMSM. In one study of HIV positive adult gay and bisexual men, McCown (1993) found that psychoticism related to failure to practice safe sex, even for those that scored highly on a measure of HIV disease knowledge. Neuroticism did not relate to sexual risk in this study, although a past study from McCown (1991) did show this association. Crepaz and Marks (2001) reported that several personality traits have been examined as correlates of sexual risk among HIV positive MSM but have shown no association, including neuroticism and extraversion (McCown, 1993) and obsessive-compulsiveness (Kalichman, 1999).
Personality variables may also relate to sexual risk outcomes indirectly, either as a mediator or moderator of other associations. For example, aspects of personality may lead individuals to seek out settings that increase their chances of engaging in high risk sex (e.g., to seek out the new experience of going to a bathhouse) or to be unprepared to protect themselves when sex occurs (e.g., lack of condom availability when making an impulsive decision to engage in sex). Alternatively, impulsive behaviors and seeking out new sensations may serve as coping strategies when experiencing emotional dysregulation or negative affect (Cooper, Agocha, & Sheldon, 2000). Personality variables may also moderate the relationship between substance use and sexual risk, such that higher/lower levels of a personality variable interact with the effect of substance use to produce higher levels of sexual risk. One aforementioned study by Newcomb et al. (in press) tested and found support for this hypothesis among YMSM. Other studies (e.g., Solomon, Kiang, Halkitis, Moeller, & Pappas, 2010), potentially provide support to this moderation hypothesis, but did not explicitly test for moderation.
Mental Health
The association between mental health and sexual risk has been explored more extensively among adult MSM than YMSM. Studies of adult gay and bisexual men have found them to exhibit a relatively high prevalence of depression (Salomon et al., 2009; Sandfort & de Keizer, 2001), anxiety (Cochran & Mays, 2005), and stress (Meyer, 1995). Samples of sexual minority youth comprised partially or solely of YMSM have demonstrated increased risk for depressive symptoms (Galliher, Rostosky, Hughes, 2004; Hatzenbuehler, McLaughlin, & Nolen-Hoeksema, 2008), suicidal ideation and attempts (Garofalo, Wolf, Wissow, Woods, & Goodman, 1999), Posttraumatic Stress Disorder (D’Augelli, Grossman, & Starks, 2006), behaviors associated with Eating Disorders (French, Story, Remafedi, Resnick, & Blum, 1996), and Generalized Anxiety Disorder and Conduct Disorder (Fergusson, Horwood, & Beautrais, 1999). However, a recent study calls for more precision in conceptualizing and measuring mental health when making these conparisons (Mustanski, Garofalo, et al., 2010).
Theoretically, depression, anxiety, and related mental health constructs could relate to sexual risk. Depression may lead to a lack of self-care and difficulty successfully initiating or maintaining health behaviors (Allgöwer, Wardle, & Steptoe, 2001). Anxiety may increase concern about HIV-infection and subsequent avoidance of sexual risk behaviors that could lead to transmission, or conversely anxiety may reduce assertiveness of health protective behaviors (Kashdan, Collins, & Elhai, 2006). Stress may lead to maladaptive or avoidant coping behaviors such as engaging in sexual risk taking (McKirnan et al., 1996). Of critical importance to this research is distinguishing between diagnoses of mental disorders, symptoms of those disorders, and core dimensions of positive and negative affect that are fundamental components of mood and anxiety disorders (Mustanski, 2007a). Much of this literature has focused on symptoms of mood disorders, and among adults a meta-analysis found the pattern of associations to be highly inconsistent across studies (Crepaz & Marks, 2001).
The limited studies of YMSM have been somewhat more reliable in regards to the association between depression and sexual risk taking compared to those of adult MSM (i.e. Crepaz & Marks, 2001). Perdue, Hagan, Thiede, and Valleroy (2003) found that YMSM with higher depression symptom scores had more sexual partners relative to low scorers. Mustanski and colleagues (2007) found an association between psychological distress and UAI in an urban YMSM sample. And, in a sample of emerging adult MSM (ages 18-30), Strathdee and colleagues (1998) reported that sexual risk-takers had higher depression scores than non risk-takers. Longitudinal YMSM research indicates that improvements in symptoms of depression relate to improved patterns of sexual risk behavior over time (Rotheram-Borus et al., 1995).
The association between anxiety and sexual risk has been inconsistent among adult MSM, YMSM, and other populations. In a meta-analysis investigating mental health correlates of sexual risk, Crepaz and Marks (2001) found a negligible effect of anxiety on sexual risk in MSM and other samples, with significant heterogeneity across studies. Of the 15 studies reviewed that investigated anxiety and risk, only three found correlations of .10 or more, and none of these three study samples were comprised solely of YMSM. More recently, Rosario and colleagues (2006) found that among YMSM, anxious symptoms related to increased number of sexual partners directly and to receptive UAI indirectly, through substance use. In the same study, however, anxious symptoms related to fewer sexual encounters overall. Research on general MSM samples points to low anxiety relating to increased sexual risk (e.g., Bancroft et al., 2003; Parsons et al., 2003). Mustanski (2007b) found that among MSM, state anxiety seems to affect MSM differentially. For those who are generally anxious (e.g., high trait anxiety), state anxiety serves as a protective factor against sexual risk. But, for MSM who are generally not anxious (e.g., low trait anxiety), state anxiety serves as a vulnerability factor for risk. These results reflect the complexity of the relationship between anxiety and sexual risk, as well as the need for continued research on these topics among MSM of all ages.
Future research investigating mental health and sexual risk among YMSM should attempt to address some of the limitations of the current body of research. First, more studies are needed that investigate the relationship between mental health and sexual risk among sexual minority populations generally and YMSM specifically. We know that these populations are at risk for problems associated with mental health (e.g., Fergusson et al., 1999). However, we remain unclear about the specific prevalence of many mental health problems within these populations, the extent to which these problems interplay with other health disparities experienced by MSM, and the range of psychological and behavioral health sequelae that result from these experiences. Also, research has not distinguished consistently between the constructs of depression and negative affect (e.g. Crepaz & Marks, 2001), which may have differential associations with sexual risk taking (Mustanski, 2007a). Related, oftentimes the construct of psychological distress is used to describe mental health. While this may be a useful conceptualization of general distress and vulnerability to psychopathology (Boulet & Boss, 1991), it lacks diagnostic specificity (Mustanski, Garofalo, et al., 2010). Future research on these topics among YMSM may benefit from using more precise conceptualizations of mental health constructs and disorders, as well as more precise diagnostic assessment tools. Given the inconsistencies in findings of bivariate relationships, it may also be useful to test models that include moderators. For example, social support may interact with mental health in predicting sexual risk.
Microsystem-Level Factors
Intimate Partner Dyads and Other Relationship Factors
Research on relationship status consistently points to a trend of engaging in UAI more often while in a steady versus casual relationship. This trend has been found among heterosexual adults (e.g. Baker, Morrison, Gillmore, & Schock, 1995) and youth (e.g. Crosby et al., 2000), adult MSM (e.g. Koblin et al., 2003b; Semple, Patterson, & Grant, 2003), and YMSM (Dudley, Rostosky, Korfhage, & Zimmerman, 2004; Hays, Kegeles, & Coates, 1990). Among MSM, YMSM seem particularly likely to engage in UAI with their primary partner; Crepaz and colleagues (2000) reported that among MSM of all ages in primary partnerships, UAI was most common in YMSM.
HIV transmission risk within adult MSM and YMSM relationships has been primarily described in two situations: incorrectly assuming one’s partner shares an HIV negative status (Dawson et al., 1994; McLean et al., 1994) and broken negotiated safety (NS) agreements (Guzman et al., 2005). YMSM, particularly, may be likely to incorrectly assume their partner’s negative status, given the low percentage of HIV positive YMSM that know their status (Valleroy et al., 2000), and the tendency for serial monogamy in adolescents increasing the likelihood of rapid primary partner turnover (Corbin & Fromme, 2002). Many of these YMSM with unrecognized infections misperceive themselves to be at low risk for acquiring or having HIV, and because of these misperceptions may engage in behaviors that could transmit HIV to their partners. Among adult MSM in couple relationships, one study reported that only 52% of participants knew the HIV status of both himself (by self-report) and his partner (by comparing reported partner status to partner’s self-report; (Moreau-Gruet, Jeannin, Dubois-Arber, & Spencer, 2001). Such a study has not been conducted among YMSM, but given trends towards more unrecognized infections among younger MSM, such research should be made a priority.
NS agreements typically involve partners enacting specific sexual strategies that maximize sexual pleasure within the relationship (e.g., by not using condoms) while reducing sexual risk outside the relationship (e.g., by not engaging in UAI with nonprimary partners) (Kippax et al., 1997). However, these agreements are not always kept. Both MSM (Crawford, Rodden, Kippax, & Van de Ven, 2001) and YMSM (Guzman et al., 2005) in relationships with NS agreements have reported simultaneously participating in UAI with casual partners. Notably, participants from the YMSM-only sample reported engaging in this behavior almost three times as much as participants from the age-aggregated MSM sample (18.0% to 6.6%, respectively).
The above evidence indicates that compared to older MSM, YMSM are more likely both to engage in UAI with their primary partner and to engage in UAI with someone outside the relationship concurrently. This is problematic, insofar as UAI with multiple partners concurrently increases all sexual partners’ risk for contracting an STI, including HIV (Gorbach & Holmes, 2003). Indeed, UAI in the context of MSM relationships is not without consequence. Research indicates that compared to single MSM, MSM in relationships are particularly at risk for HIV-infection. For example, Sullivan, Salazar, Buchbinder, and Sanchez (2009) reported that most HIV-transmissions occur in the context of relationships, with 68% of seroconversions among MSM due to one’s primary sex partner. These findings are supported by other research (Davidovich et al., 2001) which found that for YMSM, HIV-infection is trending toward acquisition from a steady, not casual partner.
Many other relationship- and individual-characteristics underlie high HIV-seroconversion rates in the context of steady YMSM and MSM relationships. Qualitative research indicates that among YMSM, factors related to UAI with a primary partner include trusting the partner, seeking greater intimacy and closeness in the relationship, instinctually feeling the partner is safe, joint HIV-testing to establish seroconcordance, and knowing the partner personally (e.g., the partner being a friend or ex-boyfriend; (Kubicek et al., 2008). A significantly larger body of quantitative and qualitative research among general MSM samples indicates that several domains may relate to UAI within steady relationships – behavioral, emotional, cognitive, and communication factors. Some behaviors that promote risk and potential HIV conversion within relationships are obvious, such as a higher number of sex acts, less frequent condom use during anal sex, and frequently engaging in unprotected receptive intercourse with one’s primary partner (Sullivan, Salazar et al., 2009). Other behaviors related to UAI among MSM in steady relationships include joint HIV testing and living with one’s partner (Folch et al., 2006). Emotional factors that promote UAI include a desire to express intimacy, trust, and love (Adam, Sears, & Schellenberg, 2000; Suarez & Miller, 2001), closeness to the partner (Zea, Reisen, Poppen, & Bianchi, 2009), and perceived interference with pleasure and intimacy (McLean et al., 1994). Cognitive factors include inaccurate or distorted perceptions of HIV (e.g. perceiving that one’s partner is not risky, regardless of knowledge of partner’s HIV status) (McLean et al., 1994), decreased worry about HIV/AIDS due to the advent and success of antiretroviral medications (Folch et al., 2006), and a lack of anxiety about STI while in a relationship (Macaluso, Demand, Artz, & Hook, 2000; Semple, Patterson, & Grant, 2000). Poor sexual communication, including avoiding the topic of sexual safety, likely also contributes to UAI in MSM relationships (McLean et al., 1994).
Another relationship characteristic that may be associated with increased sexual risk among YMSM specifically is having older sexual partners. The limited research on the association between sexual partner age and sexual risk in YMSM points to a positive association between having older sexual partners and increased sexual risk (Bingham et al., 2003; Morris, Zavisca, & Dean, 1995). In our own longitudinal research with YMSM, we found that sex with older partners increased the odds of unprotected sex relative to sex with same age partners (Mustanski & Newcomb, 2010). Another YMSM study (ages 23-29), investigating correlates of HIV infection, found that having partners 5 or more years older nearly quadrupled the odds of being HIV positive. Possibly, risky sex with older partners leads to HIV infection because older MSM are more likely to be HIV positive (Berry, Raymond, & McFarland, 2007; Hurt et al., in press). Therefore YMSM who have sex with older partners face higher per-sex-contact transmission risk. This hypothesis has not been tested, reflecting the pressing need for further research on these constructs among YMSM.
It is important to note that, despite the substantial amount of evidence pointing to increased UAI among partnered YMSM, steady relationships also relate to increased psychological and physical well-being. Research indicates that being in a partnered relationship relates to better physical and psychological health (Horwitz, White, & Howell-White, 1996; Ross, Mirowsky, & Goldsteen, 1990), as well as greater life satisfaction and happiness (Mastekaasa, 1993). Much of this research has been limited to heterosexuals. However, some research shows that partnership benefits are not exclusive to heterosexuals (Peplau & Fingerhut, 2007), and that in fact legalizing gay marriage may reduce HIV-transmission (Francis & Mialon, 2010). There is also evidence of positive effects of participating in same-sex relationships during adolescence (Bauermeister et a., 2010; Russell & Consolacion, 2003). We recognize that partnership may lead to increased UAI in the context of YMSM relationships, but that partnership likely relates to other substantial positive outcomes.
Future research to inform the development of HIV prevention programs for YMSM in couple relationships will need to grapple with defining what constitutes a steady/partnered relationship in which UAI is least risky. Unlike heterosexuals that may rely on marriage as a structural indicator that unprotected sex with their primary partner can be safer, YMSM and other sexual minorities can marry only in few states in the U.S. Since many YMSM cannot reach the relationship milestone of marriage, which typically implies sexual fidelity within the couple, they may engage in UAI with primary partners prematurely or without full consideration of the consequences. It is also worth considering that the majority of lesbian and gay youth asipire to being in a same-sex marital relationship (D’Augelli, Rendina, Grossman, & Sinclair, 2007). More research is needed to help conceptualize the role of condoms in primary and long term relationships among young male couples.
Family Factors
Families provide sources of social and emotional support, and are core models for socialization, passing along values, culture, and language. They teach explicitly and implicitly about gender roles, courtship, masculinity/femininity, and sexuality. Understandably, a family’s level of support of their son’s sexual identity as gay or bisexual, and knowledge that their son has sexual interest (or behavior) with members of the same sex, plays a direct role in healthy sexual identity development (Garofalo, Mustanski, & Donenberg, 2008; Ryan, Huebner, Diaz, & Sanchez, 2009). Such support can be modeled both actively (e.g., direct conversations about the “ethics” of homosexuality, same sex marriage, or “don’t ask, don’t tell” around the dinner table) and passively. Passive behavior can include heterosexist and homophobic comments that a parent may say during conversation, either to their child or to others but in witness of the child (e.g., “stop acting like a girl,” “that is so gay,” “when you grow up and marry a woman…”). Passive behavior can also include the failure to speak up against heterosexist or homophobic comments that others may say in front of one’s child (e.g., not saying something when an anti-gay expletive is used during a conversation).
Two decades ago, many men did not begin navigating the process of sexual identity disclosure as gay or bisexual until early adulthood, when they had established greater financial and social independence from their families. Recent research found that compared with older cohorts of MSM, younger MSM were crossing sexual milestones at earlier ages (Grov, Bimbi, Parsons, & Nanín, 2006). Specifically, among YMSM ages 18-24 in this study, the average age for coming out to self (i.e., admitting to oneself that he is gay) was 15, the mean age for telling others was 17, and the mean age for having sex with someone of the same sex was 16. Compared to previous generations of MSM, the timing of these sexual-developmental milestones seems to be more on-par with heterosexual counterparts (i.e., developmentally-appropriate time, versus “delayed,”; (Floyd & Stein, 2002).
The crossing of sexual identity development milestones for YMSM often coincides with when they are highly dependent on their families for food, shelter, and social/emotional support. The context in which a boy begins to explore same-sex attracted identity and engages in same-sex sexual behavior plays a vital role in his mental and sexual health. For example, coming out “early” has been connected with experiencing forced sex and gay-related harassment before adulthood, HIV seropositivity, partner abuse, and depression during adulthood (Friedman, Marshal, Stall, Cheong, & Wright, 2008). In YMSM, mental health consequences of stigma can lead to emotional distress, suicide attempts (Hershberger & D Augelli, 1995), drug use, and risky sex (CDC, 2009a). These negative outcomes are likely driven in part by family rejection, evidenced as poor familial support, being harassed by family members because of sexual identity, and/or being kicked out of the home (Ryan et al., 2009). More specifically, in a study of 224 White and Latino self-identified lesbian, gay, and bisexual young adults aged 21 to 25, Ryan and colleagues (2009) found that high rates of family rejection during adolescence were associated with 8.4 increased odds of a suicide attempt, 5.9 increased odds of depression, 3.4 increased odds of illegal drug use, and 3.4 increased odds of having unprotected sex, compared with peers from families that reported no or low levels of family rejection.
To improve the circumstances in which YMSM are coming out, it is necessary to reduce pervasive homophobia at the societal level. Families also need to be active participants in their child’s sexuality education, engaging in frank discussions about sexuality early in a child’s life. As noted by Ryan et al. (2009, p. 350), “Because families play such a critical role in child and adolescent development, it is not surprising that adverse, punitive, and traumatic reactions from parents and caregivers in response to their children’s LGB identity would have such a negative influence on their risk behaviors and health status as young adults.” In a study of 302 urban gay and bisexual YMSM aged 16 to 24, Garofalo et al. (2008) found the majority of parents—especially mothers—were both aware and accepting of their son’s sexual orientation. Garafalo and colleagues suggested that these supportive family members may be potential routes through which to deliver family-based HIV prevention efforts or programs—a currently underdeveloped area of research.
Sexual Abuse
Researchers have generally been in agreement that, on average, childhood sexual abuse (CSA) increases risk of negative emotional, psychological, social, and behavioral health outcomes, including contracting HIV (Arreola, Neilands, Pollack, Paul, & Catania, 2008; Arreola, Neilands, Pollack, Paul, & Catania, 2005; Catania et al., 2008; Fields, Malebranche, & Feist-Price, 2008; Holmes, Foa, & Sammel, 2005; Meade, Kershaw, Hansen, & Sikkema, 2009; Mimiaga et al., 2009; O’Leary, Purcell, Remien, & Gomez, 2003; O’Leary et al., 2005; Parsons, Bimbi, Koken, & Halkitis, 2005; Paul, Catania, Pollack, & Stall, 2001; Relf, 2001; Relf, Huang, Campbell, & Catania, 2004a; Senn, Carey, & Vanable, 2008; Sikkema, Hansen, Meade, Kochman, & Fox, 2009; Stall, Mills, Williamson, Hart, Greenwood, et al., 2003; Welles et al., 2009; Williams et al., 2008). What remains unclear is the exact mechanism through which CSA increases the risk of HIV transmission. Researchers suggest that those who experienced CSA are more likely to experience psychological distress (including depression, anxiety disorders, suicidality, and post-traumatic stress disorder) and substance use (including alcohol and prescription drug abuse, perhaps as a way to cope with experiencing CSA) as adults. CSA victims are also more likely to experience victimization as adults (e.g. physically abusive relationships and sexual victimization). Researchers propose that these factors, in turn, increase risky sexual behavior, thereby increasing one’s risk of contracting HIV. Notably, much of the research on the negative health outcomes associated with CSA has examined adult populations, an understandable phenomenon given that CSA occurs during childhood or adolescence and is often unreported. Relf and colleagues (2004b) proposed that negative health trajectories among those who experience CSA begin in childhood and are unrecognized largely because of social mores surrounding sexual behavior among men, coupled with overall, systemic neglect of the issue.
Much of our contemporary knowledge on the association between CSA and HIV among MSM has been taken from the Urban Men’s Health Study, a probability based sample of MSM over the age of 18 who resided in San Francisco, New York, Los Angeles, and Chicago (Arreola et al., 2008; Arreola et al., 2005; Paul et al., 2001; Stall, Mills, Williamson, Hart, Greenwood, et al., 2003). In this study, approximately 11% of men reported experiencing sexual abuse before age 13, although this figure was significantly higher among Latino MSM (22%, Arreola et al., 2005). Other researchers have estimated that as many as 39.7% of MSM have experienced CSA, again based on adult samples (Mimiaga et al., 2009).
Compared with heterosexual men, MSM are more likely to report CSA (Purcell, Patterson, & Spikes, 2007). For example, a prospective longitudinal case-control study following abused and matched non-abused children into adulthood found that individuals with documented histories of CSA were significantly more likely than controls to report ever having same-sex sexual partners (Wilson & Widom, 2010). However, this is not to suggest that CSA causes men to become gay or bisexual (Relf, 2001). Instead, adolescent males who are exploring their sexual identity may seek out and engage in sex with other men. Attempts to seek/initiate sex with other adolescents could lead to physical violence or verbal harassment. Given the limited number of adolescent males who may be available partners, these young men may seek out sex with older “out” partners, and some of these encounters may be coercive in nature. It is also possible that some of the childhood characteristics that are more often found among gay men (e.g., gender nonconformity) may increase the likelihood that they will be sought out by adult perpetrators of sexual abuse. And, importantly, it is possible that adult MSM are more likely to report CSA but that adult heterosexual men are equally likely to experience it. As of yet there is little research that explains the mechanism of this association.
Knowing the myriad negative outcomes that are associated with CSA (Purcell et al., 2007), what can be done to mitigate the risks of also contracting HIV? The EXPLORE study was one of the largest clinical trials of a behavioral intervention among MSM aged 16 or older (N = 4295) (Chesney et al., 2003; Koblin et al., 2003a). EXPLORE involved participants completing ten one-hour core counseling sessions delivered within four to six months, followed by up to seven maintenance booster sessions delivered every three months for up to 45 months. Participants also received HIV testing and counseling every six months. Among participants reporting CSA, and in contrast to those not reporting CSA, the EXPLORE intervention had no effect in reducing HIV infection rates (Mimiaga et al., 2009). Mimiaga and colleagues concluded that MSM with a history of CSA may derive less benefit from prevention programs. Catania and colleagues (2008), argue that the complex challenges men who have experienced CSA face may be impervious to typical short-term HIV risk reduction programs, and therefore require more long-term, intensive interventions. These researchers recommended that mental health care providers working with MSM who have experienced CSA address issues of sexual health with their clients, specifically assessing current sexual partnerships. Finally, they proposed initiating efforts to de-stigmatize reporting CSA among MSM, which likely would increase health and mental health service utilization among CSA victims. Adding to these, we propose initiating research and clinical work that helps identify CSA earlier in children and adolescent’s lives, as this would provide the opportunity for early intervention. This may ameliorate negative adult health outcomes that may be associated with CSA, including HIV infection. We also recognize significant gaps in the literature, particularly very few studies on CSA in younger samples of MSM and limited research on the mechanisms that link CSA to adult sexual risk taking.
Mesosystem-Level Factors
Sociosexual Contexts
A key task during late adolescence is integrating cognitive and psychological development within new and changing social contexts (Lerner & Galambos, 1998). The limited availability of supporting, accepting social outlets, coupled with community norms that are tolerant of substance use and casual sex, present YMSM with a diversity of risky settings (Harper, 2007a; McKirnan & Peterson, 1989). For example, bars and clubs are common places where MSM meet, socialize and find sexual partner. Consequently YMSM are exposed to settings where alcohol and drug use are prevalent, and they may learn to associate substance use with sex (McKirnan, Ostrow, & Hope, 1996; Stall et al., 2001). In a study of 428 YMSM, gay bar attendance was highly correlated with both alcohol and polydrug use as well as sexual risk behaviors (Greenwood et al., 2001). Underage MSM that are unable to access bars as a social outlet may seek friendship and companionship, but lack peer-based activities for socialization. This may drive them to other sexualized social settings (e.g., public sex venues), which may increase vulnerability to HIV acquisition (Garofalo & Harper, 2003; Garofalo, Herrick, Mustanski, & Donenberg, 2007; Garofalo, Mustanski, McKirnan, Herrick, & Donenberg, 2007a; Greenwood et al., 2001) and potentially to being the victim of violence. There is a paucity of YMSM research examining sexual and substance use risk within the context of public sex venues such as sex clubs or bathhouses. However, these contexts are highly correlated with risky behaviors among adult MSM (Crosby, Salazar, & Mettey, 2005; Elford, Bolding, & Sherr, 2001; Mettey, Crosby, DiClemente, & Holtgrave, 2003; Parsons & Halkitis, 2002; Parsons, Koken, & Bimbi, 2004). Further, emerging data suggests similar trends among YMSM (Garofalo, Herrick, Mustanski, & Donenberg, 2005). One study of YMSM ages 16-24 found that 25% engaged in commercial sex work and 26% had sex in a bathhouse or sex club (Garofalo et al., 2005). Sociosexual contexts are important to understanding HIV risk in YMSM, both because of emerging evidence of their role in risk for negative health consequences and their viability as targets for structural interventions (Fenton & Imrie, 2005; Sumartojo, 2000). Although the venues where YMSM meet their sex partners may be related to HIV transmission risks, these are also ideal locations for providing HIV testing and tailored education. Moreover, these venues may be effective mediums for linking YMSM into longer-term service provision.
Connectedness to the Gay Community
In addition to the contexts in which gay men meet, socialize, and form sexual relationships, we consider the norms and psychological effects resulting from a connection to a community of gay and bisexual men. Although the definition of the gay community (or “communities”) is constantly shifting, the gay community remains an integral nexus for socialization, mobilization, and political activism. Those who are active in the gay community, by definition, interact with other LGBT individuals. They are exposed to social norms and mores within gay culture. This activity and exposure can have effects on health that are fairly benign (e.g. music, clothing, vernacular), positive (e.g. social support, community identification), or potentially negative (e.g. more permissive norms around sexual behavior and substance use).
In terms of HIV risk, being connected with the gay community increases one’s chances of being exposed to HIV prevention, education, and testing, which are often present in bathhouses, gay bars/clubs, banners/advertisements on gay websites, events, etc ((Daskalakis et al., 2009; Grov, Parsons, & Bimbi, 2007; Mullens, Staunton, Debattista, Hamernik, & Gill, 2009). Young men who are actively involved with the gay community may be exposed to and take advantage of services specifically designed for YMSM, such as YMSM support/empowerment groups, gay-straight alliances, or medical care and HIV testing services designed for YMSM. Ramirez-Valles (2002) has laid out a conceptual framework for considering the protective effects of community involvement. This framework argues that the effects of community involvement largely operate by moderating the effects of socio-structural risk factors (e.g. homophobia) and via more proximal mediating processes (e.g. peer norms). While this model is based on literature on adult MSM, it may be useful to consider its developmental adapatation as a framework for understanding the positive effects of community involvement among YMSM.
In contrast, connection to the gay community also increases one’s chances of being exposed to factors that may increase risk of contracting HIV, such as more relaxed norms around drug use. This was well-documented within the “circuit party” scene that became popular in the late 1990s (c.f., Fernandez et al., 2005; Halkitis & Parsons, 2002; Ross, Mattison, & Franklin, 2003) and more recently with crystal methamphetamine (c.f., Halkitis, Green, & Mourgues, 2005; Nanín, Parsons, Bimbi, Grov, & Brown, 2006). In addition, YMSM may be exposed to events that combine drugs with sexual behavior (colloquially known as PnP or “Party n Play” (c.f., Grov, Bux, Parsons, & Morgenstern, 2009; Halkitis, Shrem, & Martin, 2005), “barebacking” subculture (Carballo-Dieguez & Bauermeister, 2004; Parsons & Bimbi, 2007), and more relaxed norms around sexual activity (e.g. “underground” private sex parties, gay bars with backrooms where sex is permitted, and public sex cruising areas; (c.f., Frankis & Flowers, 2009; Grov et al., 2007). Most simply, but possibly most importantly, greater engagement in the gay community provides greater access to other MSM, thereby increasing access to potential sexual partners.
As a result of this mixture of risk and protective factors, there seems to be contradictory findings as to whether attachment to the gay community facilitates or inhibits HIV risk (Fernandez, Jacobs, Warren, Sanchez, & Bowen, 2009; Flores, Mansergh, Marks, Guzman, & Colfax, 2009; O’Donnell et al., 2002). On one hand, researchers have noted how YMSM who come out “early” are often at increased risk of HIV transmission (Friedman et al., 2008). Friedman et al. (2008) noted that those out early were more likely, compared to others, to experience forced sex and gay-related harassment before adulthood. They were more likely to be HIV positive and experience gay-related victimization, partner abuse, and depression during adulthood. Those out early may face homophobia within their school (including teachers, administration, and friends), and within their local community, neighborhood, and family. These young men may also begin having sex with other men, sometimes with older MSM, who as a group have a higher HIV prevalence (Berry et al., 2007; Hurt et al., in press). However, these young men may not have received any formal sexuality education that addresses the unique sexual and HIV prevention needs of MSM (CDC, 2009b). In total, it seems these consequences may not be a result of coming out (and subsequent “participation” in the gay community), but rather a direct result of homophobia, poor social support around sexual identity, and simply accessing other men who serve as potential sex partners.
To complicate matters, research suggests the ways in which YMSM “participate” in gay communities are changing, particularly in concert with rapid advances in mobile Internet technology. Prior to the widespread use of the Internet, sexual minority individuals relied on physical spaces to mobilize and socialize (Simon Rosser, West, & Weinmeyer, 2008). Today, the Internet and mobile technologies, such as “smart phones” and mobile social networking applications (e.g., Grindr), have changed the way sexual minority individuals interact, meet, mobilize, and socialize. Rosser et al. (2008) noted how this Internet-transition among MSM is correlated with the decline of gay infrastructure, visibility, and community identification across gay communities. As a result, there has been a need to rethink traditional approaches to HIV prevention planning, interventions, treatment services, and policies for MSM (Simon Rosser et al., 2008). At the same time, these new technologies provide unprecedented opportunities to reach MSM at very early ages with programs that promote the development of sexual health (Mustanski, Lyons, & Garcia, in press).
In addition, it has become more difficult to define what constitutes participation in one’s gay community. For example, traditional definitions of gay community attachment include things like “number of gay friends” and “attendance at LGBT community events.” In contrast, measures of attachment may not include facets like “time spent online chatting with other MSM.” This, of course, begs the question, “Does chatting online ‘count’ as participation?” All told, it is clear that the methods in which YMSM integrate themselves into, and participate within, gay communities is rapidly evolving. The contexts of this integration can serve to inhibit or foster behaviors that may place YMSM at risk for HIV and STI transmission. Therefore these contexts represent critical points in which to deliver culturally competent HIV prevention messages that empower MSM to make positive sexual health decisions.
Internet
YMSM are frequent users of the Internet, reporting Internet use for multiple purposes related to sexual health, including making connections with the LGBT community, seeking sexual health information, and meeting partners for dating and/or having sex (Mustanski, Lyons, & Garcia, 2010a). YMSM report high levels of daily Internet use, with Black and Latino YMSM reporting slightly less frequent use than White YMSM (Mustanski et al., in press). In a large survey of British MSM under age 30, Bolding and colleagues (2007) found significant increases in the number of YMSM that met their first sexual partner on the Internet between 1993 and 2002 (2.6% - 61.0%). Simultaneously these researchers found decreases over time in the proportion of men who met their first partners at an offline gay venue (34.2% - 16.9%), school (23.7% - 1.3%), or a public sex environment, print ad or telephone chatline (10.5% - 1.3%). Research also indicates that MSM are significantly more likely to seek sexual partners online than non-MSM (Bull, McFarlane, & Rietmeijer, 2001). Given the frequency of Internet use in YMSM, particularly for meeting sexual partners, it is critical to understand the relationship between meeting partners online and HIV risk.
Research investigating the association between Internet use to find sexual partners and UAI/sexual risk has produced inconsistent findings in both YMSM and adult MSM. Several studies have found evidence for a link between a history of sexual risk taking and meeting partners online (Benotsch, Kalichman, & Cage, 2002; Elford et al., 2001; Garofalo, Herrick, et al., 2007; Horvath, Bowen, & Williams, 2006; Kim, Kent, McFarland, & Klausner, 2001). Others have found no relationship between these variables (Bolding, Davis, Hart, Sherr, & Elford, 2005; Chiasson et al., 2007; Mettey et al., 2003; Mustanski, Lyons, & Garcia). And, some studies have found evidence for less risk-taking with partners met online ((Bull et al., 2001; Horvath, Rosser, & Remafedi, 2008; Mustanski, 2007b).
Few studies have examined the association between seeking partners online and sexual risk in YMSM specifically. In one notable exception, researchers found that 48% of YMSM reported using the Internet to meet sex partners, and only 53% of these individuals reported using condoms consistently (Garofalo, Herrick, et al., 2007). Furthermore, 47% of the individuals who had met sex partners online reported that these sex partners were significantly older (> 4 years). Only a previous history of UAI related to risky sexual behavior with partners met online. This suggests YMSM who have a history of engaging in UAI may use the Internet as an efficient means to find UAI partners. Another recent study of YMSM (ages 18-24) found that meeting partners online may not, in and of itself, relate to sexual risk (Horvath et al., 2008). This study grouped YMSM into one of three venue-based categories – meeting partners offline only, online only, or both online and offline – to identify where young men meet their sexual partners and whether these venues differentially associated with risk. Of the three groups, YMSM who met partners both online and offline reported the highest number of sexual partners and highest rates of UAI. YMSM who met partners offline reported the fewest number of partners overall, but the highest percentage of partners with whom they engaged in UAI. In a study of young gay and bisexual men in the Netherlands, 45% of the sample reported UAI with their first partner, with no differences by partner type (met online or offline; Franssens, Hospers, & Kok, in press).
Several studies examining the association between meeting sexual partners online and sexual risk in adult MSM indicate that there may be no direct bivariate association between these variables but that certain third variables may help to explain why they are positively associated in certain contexts. For example, communication with sexual partners about HIV status and prior agreements to avoid UAI are associated with less frequent sexual risk with partners met online (Horvath, Nyhaard, & Rosser, 2009; Horvath, Oakes, & Rosser, 2008). McKirnan and colleagues (2007) found evidence that the positive association between meeting partners online and sexual risk was mediated by a history of having anonymous partners and meeting partners in public sex environments, substance use, and “burnout” with regards to safer sex. Taken together, these studies indicate that meeting partners online may not be directly associated with sexual risk but that other, more proximal variables may determine which individuals will engage in UAI with partners met online. One such proximal factor may be greater distrust and suspicion of partners met online (Mustanski, Lyons, et al., in press).
There are several limitations to the literature investigating the relationship between online sexual partners and sexual risk. Much of it is cross-sectional and few studies have used accounts of multiple sexual encounters within-persons. This type of methodology may shed light on the inconsistency in research findings by mapping the venues in which partners were met onto individual sexual encounters. For example, in his daily diary study, Mustanski (2007b) used a combined retrospective and prospective approach to investigate meeting partners online and sexual risk in MSM. Results indicated that the association between these two variables was opposite when comparing retrospective versus prospective accounts. In retrospective accounts of sexual behavior, history of meeting sex partners online was associated with a higher number of sex partners, more frequent UAI, increased number of one-time partners, and failure to discuss sexual history with partners. However, daily diary data indicated that meeting partners online actually was associated with less risky sexual behavior. These results suggest that men who are already engaging in high risk sex may be using the Internet as a tool to find sex partners, but that meeting partners online is not directly associated with occasions of relatively greater sexual risk.
Sex Work
Some YMSM experience homelessness or intermittent housing as a result of being forced or driven away from their homes, pervasive homophobia, and social rejection (Padilla, 2007; Smith & Grov, 2011). These YMSM may lack the necessary paperwork (e.g., social security card, birth certificate), education, or the minimum age to secure stable employment. As a result, they may pursue non-traditional or illegal means of earning money, food, or housing. This may include the sale of drugs, theft, or becoming involved in the sex trade industry (Clatts, Goldsamt, Yi, & Gwadz, 2005; Lankenau, Clatts, Welle, Goldsamt, & Gwadz, 2005). Studies have noted a correlation between sex work, particularly street-based sex work, and HIV seropositivity and risky sexual behavior (Allman & Myers, 1999; Bacon et al., 2006a; Bacon et al., 2006b; Belza & EPI-VIH Study Group, 2005; Rietmeijer, Wolitski, Fishbein, Corby, & Cohn, 1998).
Certainly the exchange of sex for money is not inherently risky for HIV transmission—HIV is not passed via a financial transaction. However, the contexts surrounding the transaction can potentiate unprotected sex (Bimbi, 2007; Parsons, Koken, & Bimbi, 2007). Because they are young by nature, YMSM sex workers may lack essential skills to negotiate condom use and communicate about HIV/STIs with clients. Some YMSM may not know where free condoms are available and place the purchase of condoms low in their hierarchy of needs, behind food, shelter, and clothing. As a result, YMSM involved in sex work might rely on their partners to supply condoms. Even if free condoms are available, YMSM who engage in street-based sex work may be less likely to carry them out of fear of being stopped, searched, and arrested for solicitation by law enforcement. Furthermore, clients may offer additional incentives to YMSM if they are willing to engage in sex without a condom—incentives that may be difficult for YMSM to refuse given their lack of financial wherewithal. Similarly, some clients may refuse to hire a YMSM, or turn violent, if he insists on using a condom.
YMSM engage in sex work in nations across the globe. However, social/economic circumstances within each country likely impact YMSM motives for sex work and HIV transmission risks. Specifically, the social and economic situations surrounding YMSM play a major role in the type of work he will do (e.g. street-, agency-, brothel-, or Internet-based), his own autonomy (e.g. ability to refuse clients or certain sexual behaviors), and his abilities to minimize his HIV transmission risk (Padilla, 2007; Smith & Grov, 2011). Research in many developing nations has noted associations between male sex work and HIV transmission risks. Underlying these may be homophobia, sexism, classism, or overall lack of economic and social mobility in these cultures (Brahmam et al., 2008; Chemnasiri et al., 2010; Finlinson, Colon, Robles, & Soto, 2006; Kong, 2008; Liu, Cai, Rhodes, & Hong, 2009; Newman, Chakrapani, Cook, Shunmugam, & Kakinami, 2008; Padilla et al., 2008; Pisani et al., 2004; Tun, de Mello, Pinho, Chinaglia, & Diaz, 2008; Wong et al., 2008).
Macrosystem-Level Factors
Minority Stress
Meyer (1995) first introduced the concept of LGBT minority stress by expanding the literature on the relationship between ethnic minority stressors, SES, and health outcomes. His work focused primarily on gay men, and he posited that these individuals face a unique set of stressors that can act both independently and in combination to negatively affect mental health and well-being. In particular, he concluded that internalized homophobia, perceived stigma, and experiences of discrimination and violence are the three core stressors that constitute minority stress in gay men. Because these stressors are perpetrated at the societal level, we conceptualize minority stress as part of the macrosystem.
Internalized homophobia (IH) refers to the internalization of society’s antigay attitudes within the LGBT individual (Meyer, 1995). It is argued that these negative attitudes emerge and are adopted early in life; thus a challenge for LGBT young people is to navigate the formation of a healthy identity in the midst of antigay attitudes and marginalization (D’Augelli, 1998). Meyer and Dean (1998) found a negative correlation between the passage of time and levels of IH amongst men who had come out. It follows that YMSM, who are more likely than their older counterparts to have come out recently, may experience IH. YMSM also may lack important emotional and instrumental mechanisms to cope with IH. This may result in unhealthy behaviors, including risky sexual behavior. However, few studies have examined the association between IH and risky sexual behavior in YMSM specifically. While one study found evidence for a direct positive association between these two variables (Meyer & Dean, 1995), others have not replicated this finding (Dudley et al., 2004; Rosario, Hunter, Maguen, Gwadz, & Smith, 2001). In fact, a recent meta-analysis of the association between IH and risky sexual behavior in general samples of MSM found a small overall effect size that did not differ by mean age of the sample, but did significantly decrease over time (i.e., year of publication; Newcomb & Mustanski, in press). It is plausible that the decrease in the effect size over time may be attributable to the ongoing social changes regarding homosexuality and same-sex attraction/exploration.
Some have proposed that while IH may not have a direct effect on risky sexual behavior, it may have an indirect effect (Ross, Rosser, & Smolenski, 2010). For example, using path analysis Rosario and colleagues (2001) found evidence for an indirect effect of IH on UAI in YMSM through a positive association between IH and anxiety symptoms. However, to our knowledge no explanations have been put forward for the presence of an indirect effect in the absence of a direct effect (i.e. statistical suppression; (Newcomb & Mustanski, 2010). There are several important limitations to studies of the association between IH and risky sex that may help explain these inconsistent findings. Most notable is that IH has been studied most frequently in older cohorts of MSM who were more likely impacted by AIDS-related stigma (Meyer, 1995). This may account for stronger associations between IH and risky sex in earlier studies (Newcomb & Mustanski, 2009). Also, there is evidence suggesting that IH may have changed in recent decades, such that YMSM experience a different form of IH compared to MSM born in the pre-HAART era, before 1996 (David & Knight, 2008). It is also possible that implicit or unconscious experiences of IH may have a stronger impact on health behaviors than explicit self-reports of IH. For example, Hatzenbeuhler and colleagues (2008) conducted a longitudinal analysis of adult gay men with a loved one that recently died due to HIV/AIDS. They found that implicit IH was the only measure of minority stress that, over time, was significantly associated to both number of sexual partners and UAI. This distinction between implicit and explicit IH warrants further investigation in samples of young and adult MSM.
Perceived stigma due to one’s sexual orientation involves a heightened sensitivity to rejection that is marked by anticipation, or even the expectation, of being treated as an unequal (Meyer, 2003). This heightened sensitivity to rejection is thought to make the LGBT individual more prone to a number of negative health outcomes (Pachankis, 2007). Using path analysis, Preston and colleagues (2007) found evidence for an indirect association between perceived stigma from one’s community and sexual risk in rural MSM 18 and older. MSM in this study who perceived higher rates of stigma from their community were more likely to report sexual sensation seeking behavior, which were positively associated with sexual risk. However, while other aspects of perceived stigma (i.e., family and health care provider stigma) were positively correlated with perceived stigma from the community, they were not associated with sexual risk, directly or indirectly. Finlayson (2007) provides another perspective; using a subsample of 287 Black YMSM in New York City, she found that both perceived stigma and behavioral manifestations of stigma (e.g., sexual orientation-based victimization) related to UAI after controlling for a variety of demographic variables.
Together, these analyses provide some limited evidence that aspects of sexual minority perceived stigma may elevate HIV risk behavior among MSM. However, it is possible that perception of stigma from different sources may be differentially associated with risk. In an attempt to better describe these nuances, Herek, Gillis, & Cogan (1999) expanded upon Meyer’s (1995) perceived stigma categorization by proposing four specific types of sexual-minority related stigmas: societal stigma (i.e., heterosexism, which involves a more global anti-gay climate), enacted sexual stigma (i.e., overt negative actions such as hate crimes), felt sexual stigma (i.e., being aware of society’s anti-gay attitudes), and internalized sexual stigma (i.e., adapting anti-gay attitudes, similar to IH). While this may be a promising approach, there is very little research examining these different components of stigma and their relationships with sexual risk taking in YMSM.
Violence is perhaps the most explicit forms of minority stress, and regrettably YMSM experience high rates of both harassment and victimization. In fact, evidence suggests that YMSM suffer higher risks of criminal victimization, but in particular hate crimes, compared to adult MSM and women (Herek & Sims, 2007; Herek, 2009; Herek, Gillis, & Cogan, 1999). While the antecedents for victimization are beyond the scope of this paper, it is clear that victimization exacerbates psychological distress among YMSM (Huebner, Rebchook, & Kegeles, 2004; Koblin et al., 2006; Mustanski et al., 2011; Stall, Friedman, & Catania, 2008). Although the correlation between victimization and poor mental health is well established, few studies have examined the direct effect of victimization on YMSM sexual risk taking.
Koblin and colleagues (2006) found that a majority of YMSM in their study (68%) reported a history of threats and violence by family members, intimate partners, or both. More alarming, however, is that experiencing a history of threats and violence by both family members and intimate partners nearly doubled the odds of engaging in UAI (Koblin et al., 2006). Marsiglia and colleagues (2009) also found a positive association between a history of violence and HIV risk among urban YMSM, and there appears to be a link between interpersonal violence with sexual partners and UAI in adult samples of MSM (Feldman et al., 2007; Relf et al., 2004). It is important to note, however, that these studies did not examine whether these experiences with violence were directly related to one’s sexual orientation.
Using the Youth Risk Behavior Survey, a large-scale survey of 9th —12th-grade adolescents, Bontempo and D’Augelli (2002) found that the combination of LGB identity and experiencing high rates of at-school victimization was associated with increased mental health problems, substance use, suicidality, and sexual risk behavior, compared to heterosexual youth. Fisher Raymond and colleagues (2009) examined retrospective accounts of harassment and discrimination between the ages of 12 and 18 in adult MSM and the association of these with adult HIV serostatus. Conversely, another study – one using adult MSM retrospective accounts of harassment – reported HIV negative MSM experienced significantly more discrimination during adolescence than HIV positive MSM. The authors explain this surprising finding by suggesting that experiences with discrimination and harassment may have acted as sexual inhibitors, postponing sexual activity in these young men. Consequently these men had fewer cumulative opportunities for sexual activity and decreased likelihood of HIV exposure. While theoretically possible, this hypothesis lacks empirical evidence. Therefore, more research is needed to clarify the exact effect that victimization, discrimination, and harassment play have on sexual risk.
Overall, the minority stress model is a widely used approach to understanding the mental health outcomes and experiences of LGBT individuals. However, few studies have examined the effects of minority stress on health in YMSM specifically, and even fewer have examined the potential effects of these constructs on risky sexual behavior in this population. Moreover, few viable models have been articulated and tested for the proposed indirect effects of minority stress on sexual risk behaviors. More research is needed on mechanisms linking these stressors to risk, and protective factors that may amelioriate their effects.
HIV prevention programs and related interventions
Significant HIV prevention intervention gains have been made since the advent of the epidemic. Nonetheless, some have argued convincingly that recent prevention efforts have been woefully insufficient to curb the HIV epidemic among MSM (Fenton, 2010; Jaffee, Valdiserri, & De Cock, 2007; Wolitski, Valdiserri, Denning, & Levine, 2001). Others argue that the needs of YMSM in particular have not been addressed adequately (Harper, 2007a; Mustanski et al., 2007). In describing the current status of HIV prevention efforts, Stall and colleagues (2009, p. 625) argue, “In terms of our effectiveness in the fight against AIDS among MSM in the United States, we are currently running in place.” YMSM, and in particular YMSM of color, have received relatively little attention in terms of behavioral intervention development. This reflects a general trend of HIV intervention research in this population that is not commensurate to the magnitude of the epidemic in the population (Harper, 2007b).
The development of effective behavioral HIV prevention interventions is particularly important given that most school-based sexual education programs in the U.S. do not address the needs of YMSM. Most sex-education programs in the U.S. have been mandated to incorporate an abstinence-based curriculum, which underscores sexual abstinence (until marriage) as the best behavioral prevention method to HIV/STI (Santelli et al., 2006). Abstinence-based programs historically have excluded discussions on same-sex sexuality and its associated health risks. Excluding this material from curricula is harmful to youth, not only because of its inscribed heteronormative assumptions, but because abstinence-only programs can leave adolescents, but in particular YMSM, misinformed about the benefits of condom use and the risks associated with unprotected anal sex (Fine & McClelland, 2006; Santelli et al., 2006). Furthermore, because same-sex marriage is currently illegal on a federal level and in the majority of U.S. states, abstinence until marriage messages are, at best, irrelevant to sexual minority youth.
Overall, recent meta-analyses suggest that HIV behavioral interventions for adult MSM are efficacious (Herbst, Beeker, et al., 2007; Johnson et al., 2008; Vergidis & Falagas, 2009). Behavioral interventions administered at three levels – individual, group, and community – appear to effectively reduce risky sexual behaviors associated with HIV and STI transmission. For example, Johnson and colleagues (2008) found that among 40 interventions compared to a minimal or no HIV prevention control group, the average reduction in occasions of or partners for unprotected anal sex was 27%. Herbst and colleagues (2007a) similarly found significant reductions in UAI in their meta-analysis of individually-administered, group level, and community level intervention for MSM. Group and community level interventions in particular are promising, due to cost effectiveness (Herbst, Fielding, et al., 2007). However, many projects have described difficulty with recruitment and participation in group-based interventions. Meta-analysis also has found behavioral interventions are efficacious in reducing sexual risk in a variety of adolescent populations (Johnson, Carey, Marsh, Levin, & Scott-Sheldon, 2003).
Reviews of HIV behavioral interventions highlight the paucity of published, YMSM-specific HIV prevention interventions (Harper, 2007a; Mustanski et al., 2007). Accordingly, reviews of existing interventions have led to a call for more attention to YMSM (Lyles et al., 2007). For example, of the 26 currently CDC endorsed DEBIs (Diffusion of Effective Behavioral Intervention; www.effectiveinterventons.org), none are tailored for adolescent MSM, and only one is targeted at emerging adult MSM (MPowerment). Given that federal prevention funding can be tied to implementation of a DEBI, the lack of DEBIs tested among YMSM can limit prevention work with this population.
There are a few notable YMSM-specific HIV prevention projects and interventions worthy of mention. Remafedi (1994) conducted one of the first YMSM-specific individual-level HIV interventions. He examined the effects of cognitive-behavioral HIV risk-assessment and reduction counseling on short-term changes in HIV knowledge, beliefs, and behaviors among a YMSM sample. Results showed a significant pre-post reduction in anal intercourse as well as an increase in condom use. Equally important is that this was one of the first studies to highlight HIV risk differences between YMSM and adult MSM. However, the lack of a control group and random assignment to condition limit knowledge about this intervention’s efficacy.
The Mpowerment Project, the aforementioned CDC DEBI, is perhaps the most widely disseminated intervention designed specifically for young adult MSM (ages 18-29; (Kegeles, Hays, Pollack, & Coates, 1999). The theory underlying Mpowerment is based on two premises – that learned behavior (e.g. safe sex) occurs through modeling and peer influence; and that a diffusion process is required to spread the new behavior through the community (Zimmerman et al, 1997; Hays et al., 2003). Accordingly Mpowerment is categorized as a community-level intervention, and it employs a multi-systemic approach by advocating for personal empowerment at the individual level as well as community outreach and development. To this end, it is dependent upon a group of core members and volunteers to provide outreach to the community in the form of safer sex materials and information (Hays, Rebchook, & Kegeles, 2003; Kegeles, Hays, & Coates, 1996). The intervention has been implemented widely in a variety of settings, and several studies lend support to Mpowerment’s efficacy, both in terms of cost effectiveness and HIV sexual risk reduction (Hays et al., 2003; Kahn, Kegeles, Hays, & Beltzer, 2001; Rebchook, Kegeles, Huebner, & Team, 2006).
Although not YMSM specific, Blake and colleagues (2001) conducted one of the only studies to examine the effect of a school/community-level intervention related to LGB youth health. Using data from the 1995 Massachusetts Youth Risk Behavior Survey (YRBS), these researchers found that LGB youth were significantly more likely to endorse higher rates of substance use, sexual risk behaviors, and suicide attempts compared to their heterosexual classmates. At the time of the study, 28% of Massachusetts high schools had applied for and received “Safe School Grants.” These allowed schools to supplement teacher training related to LGB issues, including LGB health and LGB sensitive HIV instruction. LGB youth in these schools engaged in fewer sexual risk behaviors than LGB youth in regular health classes. Overall, the authors conclude that LGB affirming school environments matter because they make a positive difference in the lives of LGB youth. However, due to the intervention design, it is not possible to disentangle effects of school climates that may lead to applying for grants to support LGB sensitive instruction, from the effects of such instruction.
Social networks also serve as a potential medium for behavioral intervention administration. Amirkhanian and colleagues (2003) developed an innovative social network intervention in Russia and Bulgaria for YMSM. This intervention makes use of “friendship network leaders” who provide members in their social network information on HIV transmission and risk reduction. It is based on the premise that individuals in the same social network are behaviorally similar and are amenable to behavioral change via group norms, attitudes, and expectations (Amirkhanian et al., 2005). Evaluation of this intervention indicated that it led to reductions in unprotected sex compared to a control group of YMSM.
The use of the Internet as an HIV risk reduction strategy has gained popularity in recent years. The Internet is a potentially effective tool for administering HIV prevention interventions because it is cost-effective and can be used to reach wider and less accessible populations (Dufour et al., 2000; Mustanski, 2001). A recent meta-analysis examined the efficacy of computer or technology-based behavioral interventions on HIV risk reduction and found similar efficacy rates between these and traditional behavioral interventions (Noar, Black, & Pierce, 2009). Moreover, the Internet appears to be a promising HIV intervention platform for YMSM in particular (Seal et al., 2000). A recent study found that among urban YMSM, many used the Internet to obtain information about their sexual health and to connect to gay community (Mustanski, Lyons, & Garcia, 2010b). Evidence also suggests that increasing rates of YMSM are meeting their first sexual partners online (Bolding et al., 2007).
Biomedical interventions
Given the general dearth of published YMSM-specific HIV prevention interventions, it is not surprising that there are a very limited number of YMSM-tested biomedical interventions. HIV biomedical interventions in which adult MSM have participated include: circumcision, HIV vaccine candidates, and the use of preexposure/ postexposure prophylaxis medications. Currently, the efficacy of biomedical HIV interventions in adult MSM populations remains unclear. If one or more of these approaches proves to be effective among adult MSM, it will be important to further evaluate their efficacy among YMSM before they are deployed in this population, as biological and behavioral differences across development may moderate their effectiveness.
The efficacy of male circumcision in preventing HIV infection in MSM populations is doubtful. A recent meta-analysis examining the association of circumcision status and HIV infection in approximately 53,567 MSM across fifteen observational studies failed to find a strong relationship between circumcision status and HIV status, and between circumcision and STI incidence (Millett, Flores, Marks, Reed, & Herbst, 2008). The effect was not significant even among MSM who primarily engaged in insertive anal sex. Researchers have suggested that the efficacy of circumcision as an HIV prevention strategy is likely dependent upon a number of other behavioral correlates of sexual risk (Sawires et al., 2007).
The use of either preexposure (PrEP) or postexposure (PEP) prophylaxis medications as a biomedical intervention to combat HIV has gained steady attention in the MSM community in recent years (Voetsch, Heffelfinger, Begley, Jafa-Bhushan, & Sullivan, 2007). Nonetheless, awareness and use of these as HIV prevention strategies remains modest (Liu et al., 2008). Grant and colleagues (2010) recently published the first multinational study examining the efficacy of PrEP among MSM. Result of the study showed that a once-daily pill provided an average of 44% additional protection against HIV infection to MSM and transgendered women who have sex with men, who also received a comprehensive package of traditional prevention services. The level of protection shown varied widely depending on how consistently participants used PrEP. Among those whose took their daily dose on 90% of days, HIV risk was reduced by roughly 73%. Among those who missed more than 10% of their doses, HIV risk was reduced by only about 21%. Given these effects, pharmacological prevention in the near term is likely to require both high levels of adherence and also continued practice of safer sex behaviors. This is not always the case; Golub and colleagues (2008) found that 21% of their PEP-using sample reported engaging in risky sexual behavior during their 28-day medication period. No studies have published results testing the efficacy of prophylaxis medications in YMSM, however such trials are ongoing and results are expected in the next few years.
Finally, similar to prophylaxis medications, rectal microbicides are another biological approach to prevent HIV infection. Rectal microbicides are applied directly to the rectal mucosa to prevent HIV acquisition. Currently, no clinical trials have demonstrated the efficacy of microbicides among MSM and in women, no vaginal microbicide has yet to be found effective (McGowan, 2010). Although more than 50 potential microbicides are being investigated for possible vaginal use, it’s not clear yet which of them will be suitable for rectal use. The rectum and the vagina differ significantly in structure and natural ecologies. Although most microbicides research is now focused on vaginal use, research and development of rectal microbicides is a growing segment in the field.
Secondary Prevention
Secondary prevention refers to prevention efforts targeting HIV positive individuals. Given that participants in these interventions have HIV, the ultimate goal is to reduce HIV transmission to others. For a variety of reasons, research on secondary prevention was not initiated in the U.S. until much later than research on primary prevention (Fisher, Smith, & Lenz, 2010). Crepaz and colleagues (2009) recently provided evidence suggesting a higher prevalence of UAI among HIV positive MSM compared to HIV negative or unknown HIV status MSM, indicating a particular need for secondary prevention among MSM. Like much of HIV prevention research, few secondary prevention interventions have focused on YMSM. Moreover, the secondary prevention work among adult MSM is scant, and findings are mixed. Crepaz and colleges (2006) published a meta-analysis suggesting that secondary prevention is an efficacious HIV prevention approach. Notably the analysis included studies of all HIV at-risk groups, not just MSM. Rotheram-Borus and colleagues (2004) conducted a secondary prevention intervention comprised of a majority (69%) of young gay and bisexual participants (ages 16-29). They found that, compared to participants in a delayed-intervention condition, intervention arm participants increased their proportion of protected sexual acts. Conversely, Rosser and colleagues (2010) conducted a randomized control trial to test the efficacy an MSM-specific secondary prevention intervention. Results indicated participants reported similar decreases in serodiscordant UAI across groups tailored for HIV positive MSM, HIV negative MSM, and a contrast prevention video arm. In this case, tailoring the intervention to HIV positive MSM did not provide benefits beyond the generic intervention.
Perhaps secondary prevention interventions are not consistently effective because we do not know the mechanisms that underlie their success. Consistent with this claim, few studies have investigated effective components of positive prevention interventions. Sikkema and colleagues (2010) argue that the reduction of psychological distress is the underlying mechanism of success in secondary prevention. These researchers theorize that enhancing psychological health will positively influence sexual risk behavior (Sikkema et al., 2010); therefore, secondary prevention intervention efforts should include mental health enhancement as a core focus. We suggest further research investigating these mechanisms of change in secondary prevention research, as well as more research among YMSM.
Synthesis
Given the number of risk and protective factors outlined above, and the nearly complete lack of validated prevention interventions for this population, a cogent model of HIV risk in YMSM would be extremely useful to move the field forward in basic and applied research. To date there have been almost no studies testing the relevance of existing models of HIV risk taking among YMSM or developing novel models that specifically address the contexts and risk processes that may be unique to YMSM. We were unable to locate any studies that tested established models of HIV risk behaviors among YMSM, such as the Theory of Reasoned Action (Fishbein & Ajzen, 1975), Transtheoretical model (Prochaska & Velicer, 1997), or Information-Motivation-Behavioral Skills (IMB) model (Fisher, Fisher, Williams, & Malloy, 1994). Recently, a new framework for HIV prevention has been developed – one that expands beyond the focus on the individual to include networks and resources (Johnson et al., 2010). This Network-Individual-Resource (NIR) framework incorporated specific examples from the literature on YMSM. Given its focus on facets of networks, this approach may be particularly relevant to HIV among racial minority YMSM. Stall and colleagues (2007) proposed a framework for the development of a cluster of health issues in MSM that incorporates a developmental perspective (see discussion of syndemics below). However, neither of these frameworks have yet to be formally tested in YMSM. To our knowledge, the only study testing a YMSM-specific model of sexual risk taking came from Rosario, Schrimshaw, and Hunter (2006). Their model incorporated some facets of existing health behavior theory (i.e., safer sex intentions) with other YMSM-specific risk factors, including CSA, the coming-out process, gay-related stress, self-esteem, anxious symptoms, and substance abuse. Using one-year longitudinal data collected from 1993 to 1995, they tested this multiple component model in 80 MSM ages 14-21. They found that more negative attitudes towards homosexuality, more substance abuse symptoms, and poorer intentions for safer sex were directly associated with greater likelihood of unprotected anal sex. Lower self-esteem, more anxious symptoms, and CSA were related to unprotected anal sex indirectly, through more sexual partners, sexual encounters, and substance abuse symptoms. This paper made an important contribution to the literature by developing and testing a model that helped to identify factors that were more proximal or distal to risk. The next step will be to replicate these findings in a larger and contemporary YMSM sample.
In reviewing the literature, one of our goals was to develop a testable model of HIV risk among YMSM, which if validated could serve as groundwork for the development of HIV prevention programs. As a foundation for the creation of this model, we created Table 1, which summarizes the risk factors reviewed above, places them within an ecological framework (Bronfenbrenner, 1979; Johnson et al., 2010), and appraises the degree of support found in the literature. As indicated in the table, much of the literature in this area has focused on individual level risk factors. The only individual level factor that we classify as having strong consistent empirical support for being associated with sexual risk in YMSM is drug use. Other individual level factors have strong empirical support among adult MSM and require further research on their developmental relevance to YMSM, including sensation seeking, compulsive sexual behavior, self-efficacy for HIV prevention behaviors, and CSA. Other factors have had inconsistent findings among adult MSM and limited research among YMSM. These include connectedness to the gay community, alcohol use, depression, anxiety, and IH. At the level of peer influence, there is strong empirical support among adults for the role of social support in risk reduction behaviors, and among emerging adults for the role of peers as agents of behavioral change. At the level of romantic relationships, identifying a partner as serious or primary has consistently been linked to greater rates of UAI, and there has been inconsistent or lacking research on partner characteristics such as age, race, and mode of meeting (online or offline). Some studies have found family support and acceptance to be associated with sexual risk taking, but more research is needed in this area. There has been substantial theorizing about the importance of societal factors, but limited empirical research. This likely reflects the difficulties in designing studies that allow for strong tests of society-level effects on individual outcomes or population health.
Our attempts to create a graphical model of the inter-relationships among these factors, their associations with sexual risk taking, and putative mediating pathways was unproductive given the number of interrelated variables and pathways. Models with so many variables and pathways have limited usefulness in informing research directions and developing interventions, because they do little to reduce the constellation of relevant risk and protective factors into a coherent framework. The implausibility of crafting a parsimonious model of HIV risk in YMSM based on the currently available literature stemmed from several issues. First, as reviewed above, the epidemic of HIV among YMSM does not exist in a vacuum; instead YMSM experience multiple biopsychosocial health disparities, among them greater prevalence of drug use, suicide attempts, experiences of violence, and STI (Mustanski et al., 2007). The strong interdependence among these health outcomes made it important to consider HIV risk as a multi-faceted, not an isolated outcome. This inherently increases the complexity of the model. Second, there was important interplay between many of the risk and protective factors. For example, the effects of alcohol use are best considered in the context of the relationship to the sexual partner, personality characteristics influence both predisposition to have risky sex and also to enter contexts in which risky sex is facilitated, and victimized youth tend to have less family support. That risk factors tend to co-occur, be negatively correlated with protective factors, and have cumulative effects is not unique to YMSM. Instead it is a phenomenon frequently identified in prevention research among populations that experience health disparities (Biglan, Brennan, Foster, & Holder, 2004; Jessor & Jessor, 1977; O’Connell, Boat, & Warner, 2009). Nevertheless, the interdependence of risk and protective factors makes it difficult to generate a straightforward model of risk processes.
Similarly, many risk factors are related to all of the clustering health outcomes described above. For example, family support and acceptance is associated with sexual risk taking, substance use, depression, and exposure to violence (Hershberger & D’Augelli, 1995; Mustanski et al., 2011; Ryan et al., 2009). A rigorous test of the specific versus the general effects of risk factors would require prospective longitudinal research to ensure that the risk factors occur before the onset of the health outcome and the assessment of possible confounding risk factors. This leads to the third issue, which is that most of the research on sexual risk taking in YMSM has not been multivariate. Consequently, few tests of mediating and moderating processes have been performed. Multivariate research allows for consideration of the relative explanatory value of various risk and protective factors, which can help evaluate the importance of including specific variables in a model of risk. Mediation analysis identifies processes that explain the associations between more distal factors and sexual risk taking and therefore serve as important targets for prevention or treatment programs. Moderation analysis helps identify what risk and protective factors are most relevant to specific sub-populations of YMSM (i.e., “what works for whom”). To advance the development YMSM HIV risk models, more multivariate, mediation, and moderation analyses are needed. These will contextualize risk and protective effects, allowing the factors of greatest importance to emerge.
Another complexity in developing models to describe HIV risk in YMSM is the need to explain why YMSM are at greater risk for HIV than heterosexual young men, and why some YMSM are at greater risk than other YMSM. In other words, in creating these models we must elucidate both health disparities and individual differences (Hatzenbuehler, 2009). Some of the factors that explain these group differences in HIV risk may also explain individual differences in risk, whereas others may not. For example, YMSM report more frequent drug use, which may increase their risk as a group, while at the same time YMSM who have higher than average use for their group may be at even higher risk. Conversely, institutional discrimination may explain why YMSM have a higher prevalence of HIV than heterosexual young men (Hatzenbuehler, McLaughlin, Keyes, & Hasin, 2010), but we do not know if it explains risk variability among YMSM. Characterizing these two types of processes requires samples of young heterosexuals and large, diverse samples of YMSM; only in this case could we investigate differences both between-groups (YMSM and heterosexual young men) and within-groups (YMSM of different races, SES, IH levels, etc.). At present few studies have included both of these samples; therefore, the literature on health disparities and YMSM risk processes is fragmented.
In the absence of a parsimonious model of risk process, a conceptual framework may be useful. After exploring the inter-relationships among multiple clustering health issues among adult MSM, Stall and colleagues (2003) concluded that urban gay male communities are suffering from the effects of a syndemic, or a set of simultaneous epidemics. Singer and colleagues (1996) coined the term syndemic to describe what they saw as inextricable and mutually reinforcing connections between substance abuse, violence, and AIDS among the urban poor (i.e., the “SAVA syndemic”). These researchers argued that syndemics were culturally produced, and resulted from cultural marginalization. In 2007, we extended this work by reporting on a syndemic of psychosocial health problems (substance use, mental health, and violence) that increased risk for sexual risk taking and ultimately HIV among YMSM (Mustanski et al., 2007). This focus on co-occurring diseases and afflictions differs from the traditional biomedical approach of treating these as distinct entities. Beyond the focus on disease clustering, the term syndemic also implies a focus on health disparities and social conditions that perpetrate them (Singer et al., 2006). With this in mind, the syndemic perspective offers a broader framework for understanding how multiple health problems coexist in particular communities. To qualify as a syndemic, multiple health issues must be epidemic in a community, they need to cluster together in that community, and they need to increase negative health outcomes either in an additive or multiplicative fashion. With this frame of reference, a syndemic approach identifies links among the entire set of issues that create excess burden of disease in the community’s members.
Consistent with the focus on culture marginalization underlying the syndemic approach (Singer, 1994, 1996), Stall laid out a model for syndemic development in MSM (Stall et al., 2007). Noting that these syndemic health issues tend to emerge in adolescence and young adulthood among MSM, Stall’s model focuses on phenomena that occur during childhood and/or adolescence that can shape health problems into adulthood. His model posits that two predominant dynamics are the cause of syndemic production among gay men: (1) socially produced damages associated with early adolescent male socialization, including gender policing of boys who do not conform to masculine ideals, violence and victimization for not meeting those ideals, and abusive sexual initiation; and (2) migration to large cities that contain “gay ghettos.” Moving into gay identified neighborhoods offers resources like suitable partners, community organizations, economic opportunities, etc. At the same time, relocating to a larger city can break linkages to family resources, present difficulties in creating new social networks, and provide a context of risk – a geographic location and community with high prevalence of substance abuse, violence, HIV, STIs, etc. An important limitation of Stall’s model is that it was developed based on research with middle-class American gay-identified men who came of age during the latter part of the 20th century. That is, it has not yet been tested among diverse YMSM.
Recommendations and Conclusions
In the context of existing research on YMSM, we consider a number of promising areas needing further investigation. In terms of basic research on risk processes, it is important to consider factors that may promote healthy development in spite of risk exposure. For example, in our research on syndemics, we found the largest group of YMSM (53%) were those who reported zero or only one psychosocial health problem (Mustanski et al., 2007). Similar results were found for adult MSM (Stall, Mills, Williamson, Hart, Greendwood, et al., 2003). A recent review of the public health literature on resiliency in adolescence found an underrepresentation of research on sexual minority youth (Fergus & Zimmerman, 2005). Future research should investigate protective and promotive factors among YMSM, such as positive attributes (e.g. future goals), supportive relationships, and social contexts (e.g. education attainment). Further, more research should use within-person approaches (e.g., longitudinal, trajectory analyses) and identify moderators that may explain inconsistent findings across YMSM and MSM samples. These approaches will help clarify some of the inconsistent findings on risk factors in the existing literature. We also consider more research on family factors to be a high priority (Garofalo et al., 2008; Mustanski & Hunter, 2011). There has been substantial research on family factors and family-based intervention among heterosexual youth (Pequegnat & Szapocznik, 2000), and it is time to turn that same lens to the needs of YMSM. We also suggest that research on HIV among YMSM would advance through further development of multivariate models of risk processes that identify mediators of effects and help develop a parsimonious framework to inform intervention development. Comparing the value added by YMSM-specific factors above and beyond general health behavior models also would advance our understanding of risk in this population.
In terms of intervention research, YMSM relationships are a promising area in need of further investigation. Research has already identified that among YMSM, serious relationships are the context for the majority of HIV transmissions (Sullivan, Salazar, et al., 2009) and higher rates of unprotected sex (Crepaz et al., 2000; Hart, Peterson, & Community Intervention Trial for Youth Study, 2004; Stueve et al., 2002). It is important that future research identify processes within relationships that may lead to unprotected sex, while also acknowledging the health benefits that frequently come with being in a stable and loving relationship. As such, one promising future direction for prevention science is HIV prevention interventions delivered to both YMSM in the dyad and focused on skills for healthy and happy relationships. We also consider the online delivery of interventions a promising approach for reaching YMSM, because of the unique opportunity it may provide to reach them at an early developmental stage (before risk taking occurs), and because we can provide important messages online that may not be delivered in other contexts (e.g., schools; (Mustanski, Lyons, et al., 2010a). Pragmatically, online interventions also provide the opportunity to reach rural and disenfranchised groups of YMSM that may not be accessible using offline means.
Another future goal for intervention research, among YMSM and other populations, is to understand and maximize the interconnectedness between multiculturalism and evidence-based practices (Morales & Norcross, 2010). Cultural competency is typically thought of as having the knowledge and skills necessary to perform effectively in cross-cultural situations (Hernandez, Nesman, Mowery, Acevedo-Polakovich, & Callejas, 2009). While this concept is most often associated with racial/ethnic diversity, it is also applicable to understanding youth, and particularly YMSM, culture.
Future intervention research is clearly moving in the direction of biomedical approaches (i.e., PrEP, microbicides, circumcision, earlier detection of infection) and it will be important to integrate behavioral science into approaches for dissemination and adherence in order to maximize their effects. Developmental and contextual differences in the lives of YMSM mean that such research will be needed even if these approaches are found to be effective among other young people or adult MSM. Finally, as suggested in the recent U.S. National HIV Strategy, a promising future direction is interventions that move beyond the individual-level to address structural, community, network, and/or dyadic factors. Examples of such structural and community factors include comprehensive sexuality education that is inclusive of LGBT youth, removal of punitive policies, and legal recognition of same-sex marriage.
In conclusion, we call for greater attention to understanding and preventing HIV among YMSM, who are at particularly high risk and yet the prevention response has not been commensurate. We have identified a limited number of factors with strong empirical support and a number of promising areas for further investigation. Our review of the literature highlighted the many health outcomes cluster together with HIV (e.g., drug abuse, mental health) and that many of the same predictors are related to all of these heath outcomes. This pattern suggests the needs to reconsider our focus on individual health issues and when possible develop approaches for addressing multiple health issues in concert. Consistent with the increasing attention towards translational research that moves research findings into application, future research should focus on identifying risk and protective factors and then rapidly using this information to develop, evaluate, and disseminate prevention programs.
Figure 2.
A visual depiction of Bronfenbrenner’s (1979) multi-systemic ecological theory of development, applied to HIV risk and protective factors among YMSM. We used this model to structure our review, placing each risk-related variable into one of the categories below and discussing each category successively.
Table 1.
Correlates of sexual risk among YMSM
| Correlates of Sexual Risk |
Theoretical and/or Empirical Evidence |
Degree of Support |
|
|---|---|---|---|
| Structural Factors | Lack of relevant school- based sexual health education |
Santelli et al., 2006 | Policy review and school-based survey |
| Lack of evidence-based prevention programs |
Johnson et al., 2008; Lyles et al., 2007 | Systematic review and meta- analysis |
|
| Societal Factors | Institutional Discrimination |
Hatzenbuehler, McLaughlin, Keyes, & Hasin, 2010 | Theoretical |
| Minority Stress | Meyer, 2003 | Theoretical | |
| Stigma |
Hatzenbuehler, 2009; Pachankis, 2007 |
Theoretical | |
| Family Factors | Support/rejection | Garofalo, Mustanski, & Donenberg, 2008; Mustanski et al., 2010; Ryan, Huebner, Diaz, & Sanchez, 2009 | More research needed |
| Intimate Partner Dyads |
Primary v. Casual Partners |
Crepaz et al., 2000; Davidovich et al., 2001; Dudley et al., 2004; Guzman et al., 2005; Hays et al., 1997; Kubicek et al., 2008; Stueve et al., 2002; Adams, Sears, & Schellenberg, 2000 |
Strong empirical support |
| Partner Age | Bingham et al., 2003; Morris, Zavisca, & Dean, 1995 | More research needed |
|
| Partner Race/Ethnicity | Clerkin, Newcomb, & Mustanski, 2010 | More research needed |
|
| Internet sex-seeking |
Garofalo et al., 2007; Horvath et al., 2006; Horvath et al., 2008; Mustanski, Lyons, & Garcia, in press |
Inconsistent empirical support |
|
| Sex work |
Allman & Myers, 1999; Bacon et al., 2006; Belza & EPI-VIH Study Group, 2005; Rietmeijer, Wolitski, Fishbein, Corby, & Cohn, 1998; Allman & Myers, 1999; Bimbi, 2007; Parsons, Koken, & Bimbi, 2007; Smith & Grov, 2011; Padilla, 2007 |
Strong theoretical and empirical support |
|
| Peer influences | Peers as agents of behavioral change |
Amirkhanian, Kelly, Kabakchieva, McAuliffe, & Vassileva, 2003; Hays et al., 2003; Kegeles, Hays, Pollack, & Coates, 1999 | Strong empirical support among emerging adult MSM, more research needed on adolescent MSM |
| Individual Characteristics |
Alcohol use |
Celentano et al., 2006; Choi et al., 2005; Dufour et al., 2000; Hays et al., 1997; Horvath et al., 2008; McNall & Remafedi, 1999; Newcomb, Clerkin, Mustanski, 2010; Mustanski, 2008; Stueve et al., 2002; Waldo et al., 2000 |
Inconsistent empirical support |
| Drug use |
Celentano et al., 2006; Choi et al., 2005; Clatts, Goldsamt, & Yi, 2005a, 2005b; Garofalo, Mustanski, McKirnan, Herrick, & Donenberg, 2007; Hays et al., 1997; McNall & Remafedi, 1999; Meyer & Dean, 1995; Molitor et al., 1999; Newcomb, Clerkin, & Mustanski, 2010; Remafedi, 1994; Rosario et al., 2006; Rotheram-Borus et al., 1995; Stueve et al., 2002; Waldo et al., 2000; Weber et al., 2001 |
Strong empirical support |
|
| Connectedness to gay community |
Daskalakis et al., 2009; Fernandez, Jacobs, Warren, Sanchez, & Bowen, 2009; Flores, Mansergh, Marks, Guzman, & Colfax, 2009; Grov, Parsons, & Bimbi, 2007; Mullens, Staunton, Debattista, Hamernik, & Gill, 2009; O'Donnell et al., 2002 |
Inconsistent empirical in adult MSM, more research needed in YMSM |
|
| Sensation Seeking |
Dudley et al., 2004; Newcomb, Clerkin, & Mustanski, 2010 |
Strong empirical support in adult MSM, more research needed in YMSM |
|
| Impulsivity/Impulsive decision-making |
Dudely, Rostosky, Korfhage, & Zimmerman, 2004; Hays et al., 1997 | More research needed |
|
| Compulsive Sexual Behavior |
Coleman et al., 2009; Kalichman & Rompa, 1995; Miner, Coleman, Center, Ross, & Rosser, 2007; Parsons & Bimbi, 2007; Reece, 2003 |
Strong empirical support in adult MSM, more research needed in YMSM |
|
| Self-efficacy | Amirkhanian, Kelly, Kabakchieva, McAuliffe, Vassileva, 2003 | Strong empirical support in adult MSM, more research needed in YMSM |
|
| Depression |
Crepaz & Marks, 2001; Perdue, Hagan, Thiede, and Valleroy, 2003; Rotheram-Borus, Rosario, Reid, Koopman, 1995; Salomon et al., 2008 |
Inconsistent empirical support, more research needed in YMSM |
|
| Anxiety |
Crepaz & Marks, 2001; Rosario, Schrimshaw, & Hunter, 2006 |
Inconsistent empirical support, more research needed in YMSM |
|
| Psychological distress | Mustanski, Garofalo, Herrick, and Donenberg, 2007 | More research needed |
|
| State Affect | Mustanski, 2007b | More research needed |
|
| Sexual Abuse |
Arreola et al., 2005; Arreola et al., 2008; Catania et al., 2008; Fields et al., 2008; Holmes, Foa, & Sammel, 2005; Meade et al., 2009; Mimiaga et al., 2009; O’Leary et al., 2003; O’Leary et al., 2005; Parsons et al., 2005; Paul et al., 2001; Relf, 2001; Relf et al., 2004; Senn, Carey, & Vanable, 2008; Sikkema et al., 2009; Stall et al., 2003; Welles et al., 2009; Williams et al., 2008 |
Strong empirical support in adult MSM, more research needed in YMSM |
|
| Internalized Homophobia |
Dudley et al., 2004; Hatzenbuehler et al., 2008; Newcomb & Mustanski, in press; Meyer & Dean, 1995; Rosario et al., 2001 |
Inconsistent empirical support, more research needed in YMSM |
Acknowledgments
During the preparation of this manuscript, Brian S. Mustanski was supported as a Principal Investigator on grants for research on HIV among young men who have sex with men from the National Institute of Mental Health (R34MH079714), the National Institute of Drug Abuse (R01DA025548), and the William T. Grant Foundation. He acknowledges his role as a participating scientist in the Fenway Institute Center for Population Research in LGBT Health (R21HD051178) and the Chicago Center for AIDS Research (P30AI082151). Michael E. Newcomb was supported by a National Research Service Award from the National Institute of Mental Health (F31MH088942). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, the National Institute of Drug Abuse, the National Institutes of Health, or the William T. Grant Foundation.
References
- Adam BD, Sears A, Schellenberg EG. Accounting for unsafe sex: Interviews with men who have sex with men. Journal of Sex Research. 2000;37:24–36. [Google Scholar]
- Allman D, Myers T. Male sex work and HIV/AIDS in Canada. In: Aggleton P, editor. Men who sell sex: International perspectives on male prostitution and HIV/AIDS. Temple University Press; Philadelphia: 1999. pp. 61–81. [Google Scholar]
- Amirkhanian YA, Kelly JA, Kabakchieva E, Kirsanova AV, Vassileva S, Takacs J, Mocsonaki L. A randomized social network HIV prevention trial with young men who have sex with men in Russia and Bulgaria. AIDS. 2005;19:1897–1905. doi: 10.1097/01.aids.0000189867.74806.fb. doi: 10.1097/01.aids.0000189867.74806.fb. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- Arnett JJ, Tanner JL. Emerging adults in America : coming of age in the 21st century. 1st ed American Psychological Association; Washington, DC: 2006. [Google Scholar]
- Arreola SG, Neilands T, Pollack L, Paul J, Catania J. Childhood sexual experiences and adult health sequelae among gay and bisexual men: defining childhood sexual abuse. J Sex Res. 2008;45:246–252. doi: 10.1080/00224490802204431. doi: 901397765 [pii] 10.1080/00224490802204431. [DOI] [PubMed] [Google Scholar]
- Arreola SG, Neilands TB, Pollack LM, Paul JP, Catania JA. Higher prevalence of childhood sexual abuse among Latino men who have sex with men than non-Latino men who have sex with men: data from the Urban Men’s Health Study. Child Abuse Negl. 2005;29:285–290. doi: 10.1016/j.chiabu.2004.09.003. doi: S0145-2134(05)00056-6 [pii] 10.1016/j.chiabu.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Bacon O, Lum P, Hahn J, Evans J, Davidson P, Moss A, Page-Shafer K. Commercial sex work and risk of HIV infection among young drug-injecting men who have sex with men in San Francisco. Sex Transm Dis. 2006a;33:228–234. doi: 10.1097/01.olq.0000204914.91923.ad. [DOI] [PubMed] [Google Scholar]
- Bacon O, Lum P, Hahn J, Evans J, Davidson P, Moss A, Page-Shafer K. Commercial sex work and risk of HIV infection among young drug-injecting men who have sex with men in San Francisco. Sex Transm Dis. 2006b;33:228–234. doi: 10.1097/01.olq.0000204914.91923.ad. doi: 10.1097/01.olq.0000204914.91923.ad 00007435-200604000-00005 [pii] [DOI] [PubMed] [Google Scholar]
- Baker SA, Morrison DM, Gillmore MR, Schock MD. Sexual Behaviors, Substance Use, and Condom Use in a Sexually-Transmitted Disease Clinic Sample. Journal of Sex Research. 1995;32:37–44. [Google Scholar]
- Bancroft J, Janssen E, Strong D, Carnes L, Vukadinovic Z, Long JS. Sexual risk-taking in gay men: the relevance of sexual arousability, mood, and sensation seeking. Archives of Sexual Behavior. 2003;32:555–572. doi: 10.1023/a:1026041628364. [DOI] [PubMed] [Google Scholar]
- Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated Risk for HIV Infection among Men Who Have Sex with Men in Low- and Middle-Income Countries 2000-2006: A Systematic Review. PLoS Medicine. 2007;4:e339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrman RE, Kliegman R, Jenson HB. Nelson textbook of pediatrics. 17th ed Saunders; Philadelphia, PA: 2004. [Google Scholar]
- Belza MJ, EPI-VIH Study Group Risk of HIV infection among male sex workers in Spain. Sex Transm Infect. 2005;81:85–88. doi: 10.1136/sti.2003.008649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Arch Sex Behav. 2002;31:177–183. doi: 10.1023/a:1014739203657. [DOI] [PubMed] [Google Scholar]
- Berry M, Raymond HF, McFarland W. Same race and older partner selection may explain higher HIV prevalence among black men who have sex with men. Aids. 2007;21:2349–2350. doi: 10.1097/QAD.0b013e3282f12f41. doi: 10.1097/QAD.0b013e3282f12f41 00002030-200711120-00015 [pii] [DOI] [PubMed] [Google Scholar]
- Biglan A, Brennan PA, Foster SL, Holder HD. Helping adolescents at risk : prevention of multiple problem behaviors. Guilford Press; New York, NY: 2004. [Google Scholar]
- Bimbi DS. Male prostitution: Pathology, paradigms and progress in research. Journal of Homosexuality. 2007;53:7–35. doi: 10.1300/J082v53n01_02. [DOI] [PubMed] [Google Scholar]
- Bimbi DS, Nanin JE, Parsons JT, Vicioso KJ, Missildine W, Frost DM. Assessing gay and bisexual men’s outcome expectancies for sexual risk under the influence of alcohol and drugs. Subst Use Misuse. 2006;41:643–652. doi: 10.1080/10826080500411080. [DOI] [PubMed] [Google Scholar]
- Bingham TA, Harawa NT, Johnson DF, Secura GM, MacKellar DA, Valleroy LA. The effect of partner characteristics on HIV infection among African American men who have sex with men in the Young Men’s Survey, Los Angeles, 1999-2000. AIDS Education and Prevention. 2003;15:39–52. doi: 10.1521/aeap.15.1.5.39.23613. [DOI] [PubMed] [Google Scholar]
- Blake SM. Preventing sexual risk behaviors among gay, lesbian, and bisexual adolescents: the benefits of gay-sensitive HIV instruction in schools. Am Public Health Assoc; 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolding G, Davis M, Hart G, Sherr L, Elford J. Gay men who look for sex on the Internet: is there more HIV/STI risk with online partners? AIDS. 2005;19:961–968. doi: 10.1097/01.aids.0000171411.84231.f6. [DOI] [PubMed] [Google Scholar]
- Bolding G, Davis M, Hart G, Sherr L, Elford J. Where young MSM meet their first sexual partner: the role of the Internet. AIDS and Behavior. 2007;11:522–526. doi: 10.1007/s10461-007-9224-9. [DOI] [PubMed] [Google Scholar]
- Brahmam GN, Kodavalla V, Rajkumar H, Rachakulla HK, Kallam S, Myakala SP, Ramesh BM. Sexual practices, HIV and sexually transmitted infections among self-identified men who have sex with men in four high HIV prevalence states of India. Aids. 2008;22(Suppl 5):S45–57. doi: 10.1097/01.aids.0000343763.54831.15. doi: 10.1097/01.aids.0000343763.54831.15 00002030-200812005-00004 [pii] [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Harvard University Press; Cambridge: 1979. [Google Scholar]
- Bull SS, McFarlane M, Rietmeijer C. HIV and sexually transmitted infection risk behaviors among men seeking sex with men on-line. American Journal of Public Health. 2001;91:988–989. doi: 10.2105/ajph.91.6.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campsmith ML, Rhodes PH, Hall HI, Green TA. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006. Journal of Acquired Immune Deficiency Syndromes. 2010;53:619–624. doi: 10.1097/QAI.0b013e3181bf1c45. doi: 10.1097/QAI.0b013e3181bf1c45. [DOI] [PubMed] [Google Scholar]
- Carballo-Dieguez A, Bauermeister J. “Barebacking”: Intentional condomless anal sex in HIV-risk contexts. Reasons for and against it. Journal of Homosexuality. 2004;47:1–16. doi: 10.1300/J082v47n01_01. [DOI] [PubMed] [Google Scholar]
- Catania JA, Paul J, Osmond D, Folkman S, Pollack L, Canchola J, Neilands T. Mediators of childhood sexual abuse and high-risk sex among men-who-have-sex-with-men. Child Abuse Negl. 2008 doi: 10.1016/j.chiabu.2007.12.010. doi: S0145-2134(08)00161-0 [pii] 10.1016/j.chiabu.2007.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Trends in HIV/AIDS diagnoses among men who have sex with men-33 states, 2001-2006. MMWR. 2008;57:681–686. [PubMed] [Google Scholar]
- CDC HIV and AIDS among Gay and Bisexual Men. 2009a Retrieved from http://www.cdc.gov/hiv/topics/msm/resources/factsheets/msm.htm.
- CDC . HIV/AIDS and young men who have sex with men. US Department of Health and Human Services, Center for Disease Control and Prevention; Atlanta, GA: 2009b. [Google Scholar]
- CDC . HIV/AIDS surveillance in adolescents and young adults (through 2007) US DHHS; Atlanta: 2009c. Retrieved from http://www.cdc.gov/hiv/topics/surveillance/resources/slides/adolescents/index.htm. [Google Scholar]
- CDC Surveillance Summaries: Sexual and Reproductive Health of Persons Aged 10–24 Years — United States, 2002–2007. WWMR. 2009d;58 [PubMed] [Google Scholar]
- CDC . HIV and AIDS among Gay and Bisexual Men. US Department of Health and Human Services; Atlanta: 2010. [Google Scholar]
- Celentano DD, Valleroy LA, Sifakis F, MacKellar DA, Hylton J, Thiede H, Torian LV. Associations between substance use and sexual risk among very young men who have sex with men. Sexually Transmitted Diseases. 2006;33:265–271. doi: 10.1097/01.olq.0000187207.10992.4e. [DOI] [PubMed] [Google Scholar]
- Chemnasiri T, Netwong T, Visarutratana S, Varangrat A, Li A, Phanuphak P, van Griensven F. Inconsistent condom use among young men who have sex with men, male sex workers, and transgenders in Thailand. AIDS Educ Prev. 2010;22:100–109. doi: 10.1521/aeap.2010.22.2.100. doi: 10.1521/aeap.2010.22.2.100 10.1521/aeap.2010.22.2.100 [pii] [DOI] [PubMed] [Google Scholar]
- Chesney M, Koblin B, Barresi P, Husnik M, Celum C, Colfax G, Team, E. S. An individually tailored intervention for HIV prevention: baseline data from the EXPLORE Study. Am J Public Health. 2003;93:933–938. doi: 10.2105/ajph.93.6.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: An event-based on-line survey. Journal of Acquired Immune Deficiency Syndromes. 2007;44:235–243. doi: 10.1097/QAI.0b013e31802e298c. [DOI] [PubMed] [Google Scholar]
- Choi KH, Han CS, Hudes ES, Kegeles S. Unprotected sex and associated risk factors among young Asian and Pacific Islander men who have sex with men. AIDS Education and Prevention. 2002;14:472–481. doi: 10.1521/aeap.14.8.472.24114. [DOI] [PubMed] [Google Scholar]
- Clatts MC, Goldsamt L, Yi H, Gwadz MV. Homelessness and drug abuse among young men who have sex with men in New York city: a preliminary epidemiological trajectory. J Adolesc. 2005;28:201–214. doi: 10.1016/j.adolescence.2005.02.003. doi: S0140-1971(05)00020-5 [pii] 10.1016/j.adolescence.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clatts MC, Goldsamt LA, Yi H. Club drug use among young men who have sex with men in NYC: a preliminary epidemiological profile. Subst Use Misuse. 2005a;40:1317–1330. doi: 10.1081/JA-200066898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clatts MC, Goldsamt LA, Yi H. Drug and sexual risk in four men who have sex with men populations: evidence for a sustained HIV epidemic in New York City. J Urban Health. 2005b;82:i9–17. doi: 10.1093/jurban/jti019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clerkin E, Newcomb M, Mustanski B. Black young men who have sex with men (MSM) engage in less sexual risk taking: a longitudinal dyad-level analysis. 2010. under review.
- Clutterbuck DJ, Gorman D, McMillan A, Lewis R, Macintyre CC. Substance use and unsafe sex amongst homosexual men in Edinburgh. AIDS Care. 2001;13:527–535. doi: 10.1080/09540120120058058. doi: 10.1080/09540120120058058 4PJN3EBRR4GJ4JYM [pii] [DOI] [PubMed] [Google Scholar]
- Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, Coates TJ. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. American Journal of Epidemiology. 2004;159:1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Alcohol use and risky sexual behavior among college students and youth: evaluating the evidence. Journal of Studies on Alcohol. 2002;14:101–117. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- Corbin WR, Fromme K. Alcohol use and serial monogamy as risks for sexually transmitted diseases in young adults. Health Psychology. 2002;21:229–236. doi: 10.1037//0278-6133.21.3.229. [DOI] [PubMed] [Google Scholar]
- Crawford JM, Rodden P, Kippax S, Van de Ven P. Negotiated safety and other agreements between men in relationships: risk practice redefined. International Journal of STD and AIDS. 2001;12:164–170. doi: 10.1258/0956462011916965. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychology. 2001;20:291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marks G, Mansergh G, Murphy S, Miller LC, Appleby PR. Age-related risk for HIV infection in men who have sex with men: examination of behavioral, relationship, and serostatus variables. AIDS Education and Prevention. 2000;12:405–415. [PubMed] [Google Scholar]
- Crosby R, Salazar LF, Mettey A. Gay men who attend sex resorts: a typology associated with high-risk sexual behaviour. International Journal of STD and AIDS. 2005;16:158–162. doi: 10.1258/0956462053057530. [DOI] [PubMed] [Google Scholar]
- Crosby RA, DiClemente RJ, Wingood GM, Sionean C, Cobb BK, Harrington K. Correlates of unprotected vaginal sex among African American female adolescents: importance of relationship dynamics. Archives of Pediatrics and Adolescent Medicine. 2000;154:893–899. doi: 10.1001/archpedi.154.9.893. [DOI] [PubMed] [Google Scholar]
- Croyle R, Loftus E. Recollection in the Kingdom of AIDS. In: Ostrow DG, Kessler RC, editors. Methodological Issues in AIDS Behavioral Research. Plenum Press; New York: 1993. pp. 163–180. [Google Scholar]
- D’Augelli A. Developmental Implications of Victimization of Lesbian, Gay, and Bisexual Youths. Stigma and sexual orientation: understanding prejudice against lesbians, gay men, and bisexuals. 1998:1187. [Google Scholar]
- D’Augelli AR, Hershberger SL, Pilkington NW. Lesbian, gay, and bisexual youth and their families: Disclosure of sexual orientation and its consequences. American Journal of Orthopsychiatry. 1998;68:361–371. doi: 10.1037/h0080345. discussion 372-365. [DOI] [PubMed] [Google Scholar]
- Daskalakis D, Silvera R, Bernstein K, Stein D, Hagerty R, Hutt R, Marmor M. Implementation of HIV testing at 2 New York City bathhouses: from pilot to clinical service. Clin Infect Dis. 2009;48:1609–1616. doi: 10.1086/598979. doi: 10.1086/598979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David S, Knight BG. Stress and coping among gay men: Age and ethnic differences. Psychology and Aging. 2008;23:62–69. doi: 10.1037/0882-7974.23.1.62. doi: 10.1037/0882-7974.23.1.62. [DOI] [PubMed] [Google Scholar]
- Davidovich U, de Wit J, Albrecht N, Geskus R, Stroebe W, Coutinho R. Increase in the share of steady partners as a source of HIV infection: a 17-year study of seroconversion among gay men. AIDS. 2001;15:1303–1308. doi: 10.1097/00002030-200107060-00013. [DOI] [PubMed] [Google Scholar]
- Dawson JM, Fitzpatrick RM, Reeves G, Boulton M, McLean J, Hart GJ, Brookes M. Awareness of sexual partners’ HIV status as an influence upon high-risk sexual behaviour among gay men. AIDS. 1994;8:837–841. [PubMed] [Google Scholar]
- Donohew L, Zimmerman R, Cuppa PS, Novakb S, Colonc S, Abella R. Sensation seeking, impulsive decision-making, and risky sex: implications for risk-taking and design of interventions. Personality & Individual Differences. 2000;28:1079–1091. [Google Scholar]
- Drumright LN, Little SJ, Strathdee SA, Slymen DJ, Araneta MR, Malcarne VL, Gorbach PM. Unprotected anal intercourse and substance use among men who have sex with men with recent HIV infection. Journal of Acquired Immune Deficiency Syndromes. 2006;43:344–350. doi: 10.1097/01.qai.0000230530.02212.86. doi: 10.1097/01.qai.0000230530.02212.86. [DOI] [PubMed] [Google Scholar]
- Drumright LN, Patterson TL, Strathdee SA. Club drugs as causal risk factors for HIV acquisition among men who have sex with men: a review. Substance Use and Misuse. 2006;41:1551–1601. doi: 10.1080/10826080600847894. doi: M374820677387050 [pii] 10.1080/10826080600847894. [DOI] [PubMed] [Google Scholar]
- DuBois SN, Mustanski B, Emerson E. Condom errors, failures, and erection problems among a diverse sample of young men who have sex with men. 2010. under review.
- Dudley MG, Rostosky SS, Korfhage BA, Zimmerman RS. Correlates of high-risk sexual behavior among young men who have sex with men. AIDS Education and Prevention. 2004;16:328–340. doi: 10.1521/aeap.16.4.328.40397. doi: 10.1521/aeap.16.4.328.40397. [DOI] [PubMed] [Google Scholar]
- Dufour A, Alary M, Otis J, Noel R, Remis RS, Masse B, Vincelette J. Correlates of risky behaviors among young and older men having sexual relations with men in Montreal, Quebec, Canada. Omega Study Group. J Acquir Immune Defic Syndr. 2000;23:272–278. doi: 10.1097/00126334-200003010-00011. [DOI] [PubMed] [Google Scholar]
- Elford J, Bolding G, Sherr L. Seeking sex on the Internet and sexual risk behaviour among gay men using London gyms. AIDS. 2001;15:1409–1415. doi: 10.1097/00002030-200107270-00010. [DOI] [PubMed] [Google Scholar]
- Fenton KA. Prevention with HIV-positive men who have sex with men: regaining lost ground. Sexually Transmitted Infections. 2010;86:2–4. doi: 10.1136/sti.2009.038935. [DOI] [PubMed] [Google Scholar]
- Fenton KA, Imrie J. Increasing rates of sexually transmitted diseases in homosexual men in Western europe and the United States: why? Infectious Disease Clinics of North America. 2005;19:311–331. doi: 10.1016/j.idc.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annual Review of Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- Fernandez MI, Bowen GS, Varga LM, Collazo JB, Hernandez N, Perrino T, Rehbein A. High rates of club drug use and risky sexual practices among Hispanic men who have sex with men in Miami, Florida. Subst Use Misuse. 2005;40:1347–1362. doi: 10.1081/JA-200066904. doi: W02W12M5408J3885 [pii] 10.1081/JA-200066904. [DOI] [PubMed] [Google Scholar]
- Fernandez MI, Jacobs RJ, Warren JC, Sanchez J, Bowen GS. Drug use and Hispanic men who have sex with men in South Florida: Implications for intervention development. AIDS Educ Prev. 2009;21:45–60. doi: 10.1521/aeap.2009.21.5_supp.45. [DOI] [PubMed] [Google Scholar]
- Fields SD, Malebranche D, Feist-Price S. Childhood sexual abuse in black men who have sex with men: results from three qualitative studies. Cultural Diversity and Ethnic Minority Psychology. 2008;14:385–390. doi: 10.1037/1099-9809.14.4.385. doi: 2008-14898-013 [pii] 10.1037/1099-9809.14.4.385. [DOI] [PubMed] [Google Scholar]
- Fine M, McClelland S. Sexuality Education and Desire: Still Missing after All These Years. Harvard Educational Review. 2006;76:297–338. [Google Scholar]
- Finlinson HA, Colon HM, Robles RR, Soto M. Sexual identity formation and AIDS prevention: an exploratory study of non-gay-identified Puerto Rican MSM from working class neighborhoods. AIDS Behav. 2006;10:531–539. doi: 10.1007/s10461-006-9107-5. doi: 10.1007/s10461-006-9107-5. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Addison-Wesley; Reading, MA: 1975. [Google Scholar]
- Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13:238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- Fisher Raymond H, Chen YH, Stall RD, McFarland W. Adolescent Experiences of Discrimination, Harassment, Connectedness to Community and Comfort with Sexual Orientation Reported by Adult Men Who have Sex with Men as a Predictor of Adult HIV Status. AIDS and Behavior. 2009 doi: 10.1007/s10461-009-9634-y. doi: 10.1007/s10461-009-9634-y. [DOI] [PubMed] [Google Scholar]
- Flores SA, Mansergh G, Marks G, Guzman R, Colfax G. Gay identity-related factors and sexual risk among men who have sex with men in San Francisco. AIDS Education and Prevention. 2009;21:91–103. doi: 10.1521/aeap.2009.21.2.91. doi: 10.1521/aeap.2009.21.2.91 10.1521/aeap.2009.21.2.91 [pii] [DOI] [PubMed] [Google Scholar]
- Floyd FJ, Stein TS. Sexual orientation identity formation among gay, lesbian, and bisexual youths: Multiple patterns of milestone experiences. Journal of Research on Adolescence. 2002;12:167191. [Google Scholar]
- Folch C, Marks G, Esteve A, Zaragoza K, Munoz R, Casabona J. Factors associated with unprotected sexual intercourse with steady male, casual male, and female partners among men who have sex with men in Barcelona, Spain. AIDS Education and Prevention. 2006;18:227–242. doi: 10.1521/aeap.2006.18.3.227. [DOI] [PubMed] [Google Scholar]
- Francis AM, Mialon HM. Tolerance and HIV. Journal of Health Economics. 2010;29:250–267. doi: 10.1016/j.jhealeco.2009.11.016. [DOI] [PubMed] [Google Scholar]
- Frankis JS, Flowers P. Public sexual cultures: A systematic review of qualitative research investigating men’s sexual behaviors with men in public spaces. Journal of Homosexuality. 2009;56:861–893. doi: 10.1080/00918360903187846. [DOI] [PubMed] [Google Scholar]
- Friedman MS, Marshal MP, Stall R, Cheong J, Wright ER. Gay-related development, early abuse and adult health outcomes among gay males. AIDS and Behavior. 2008;12:891–902. doi: 10.1007/s10461-007-9319-3. doi: 10.1007/s10461-007-9319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Harper GW. Not all adolescents are the same: addressing the unique needs of gay and bisexual male youth. Adolescent Medicine. 2003;14:595–611. doi: 10.1016/S1041349903500470. [DOI] [PubMed] [Google Scholar]
- Garofalo R, Herrick A, Mustanski B, Donenberg GR. Tip of the iceberg: Young men who have sex with men, the Internet, and HIV risk. American Journal of Public Health. 2005 doi: 10.2105/AJPH.2005.075630. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Herrick A, Mustanski B, Donenberg GR. Tip of the iceberg: Young men who have sex with men, the Internet, and HIV risk. American Journal of Public Health. 2007;97:1113–1117. doi: 10.2105/AJPH.2005.075630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Mustanski B, Donenberg G. Parents know and parents matter; is it time to develop family-based HIV prevention programs for young men who have sex with men? Journal of Adolescent Health. 2008;43:201–204. doi: 10.1016/j.jadohealth.2008.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Mustanski B, Johnson A, Emerson E. Exploring Factors That Underlie Racial/Ethnic Disparities in HIV Risk among Young Men Who Have Sex with Men. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2010;87:318–323. doi: 10.1007/s11524-009-9430-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Mustanski B, McKirnan DJ, Herrick A, Donenberg DR. Methamphetamine and young men who have sex with men: Understanding patterns and correlates of use and the association with HIV-related sexual risk. Archives of Pediatrics and Adolescent Medicine. 2007a;161:591–596. doi: 10.1001/archpedi.161.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Mustanski BS, McKirnan DJ, Herrick A, Donenberg GR. Methamphetamine and young men who have sex with men: understanding patterns and correlates of use and the association with HIV-related sexual risk. Arch Pediatr Adolesc Med. 2007b;161:591–596. doi: 10.1001/archpedi.161.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Wolf CR, Kessel S, Palfrey J, DuRant RH. The association between health risk behaviors and sexual orientation among a school-based sample of adolescents. Pediatrics. 1998;101:895–902. doi: 10.1542/peds.101.5.895. [DOI] [PubMed] [Google Scholar]
- Gillmore M, Morrison D, Leigh BC, Hoppe M, Gaylord J, Rainey D. Does “High = High Risk”? An Event-Based Analysis of the Relationship Between Substance Use and Unprotected Anal Sex Among Gay and Bisexual Men. AIDS and Behavior. 2002;V6:361–370. [Google Scholar]
- Gorbach PM, Holmes KK. Transmission of STIs/HIV at the partnership level: beyond individual-level analyses. Journal of Urban Health. 2003;80:iii15–25. doi: 10.1093/jurban/jtg079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood GL, White EW, Page-Shafer K, Bein E, Osmond DH, Paul J, Stall RD. Correlates of heavy substance use among young gay and bisexual men: The San Francisco Young Men’s Health Study. Drug and Alcohol Dependence. 2001;61:105–112. doi: 10.1016/s0376-8716(00)00129-0. [DOI] [PubMed] [Google Scholar]
- Grov C, Bimbi DS, Nanin JE, Parsons JT. Race, ethnicity, gender, and generational factors associated with the coming-out process among lesbian, and bisexual individuals. Journal of Sex Research. 2006;43:115–121. doi: 10.1080/00224490609552306. [DOI] [PubMed] [Google Scholar]
- Grov C, Bimbi DS, Parsons JT, Nanín JE. Race, ethnicity, gender, and generational factors associated with the coming-out process among gay, lesbian, and bisexual individuals. Journal of Sex Research. 2006;43:115–121. doi: 10.1080/00224490609552306. [DOI] [PubMed] [Google Scholar]
- Grov C, Bux DA, Parsons JT, Morgenstern J. Recruiting hard-to-reach drug-using men who have sex with men into an intervention study: Lessons learned and implications for applied research. Substance Use and Misuse. 2009;44:1855–1871. doi: 10.3109/10826080802501570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. Sexual risk behavior and venues for meeting sex partners: an intercept survey of gay and bisexual men in LA and NYC. AIDS and Behavior. 2007;11:915–926. doi: 10.1007/s10461-006-9199-y. [DOI] [PubMed] [Google Scholar]
- Guenther-Grey CA, Varnell S, Weiser JI, Mathy RM, O’Donnell L, Stueve A, Remafedi G. Trends in sexual risk-taking among urban young men who have sex with men, 1999-2002. Journal of the National Medical Association. 2005;97:38S–43S. [PMC free article] [PubMed] [Google Scholar]
- Guzman R, Colfax GN, Wheeler S, Mansergh G, Marks G, Rader M, Buchbinder S. Negotiated safety relationships and sexual behavior among a diverse sample of HIV-negative men who have sex with men. Journal of Acquired Immune Deficiency Syndromes. 2005;38:82–86. doi: 10.1097/00126334-200501010-00015. doi: 00126334-200501010-00015 [pii] [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Green KA, Mourgues P. Longitudinal investigation of methamphetamine use among gay and bisexual men in New York City: Findings from Project Bumps. Journal of Urban Health. 2005;82:i18–i25. doi: 10.1093/jurban/jti020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT. Recreational drug use and HIV-risk sexual behavior among men frequenting gay social venues. Journal of Gay & Lesbian Social Services. 2002;14:19–38. [Google Scholar]
- Halkitis PN, Shrem MT, Martin FW. Sexual behavior patterns of methamphetamine-using gay and bisexual men. Subst Use Misuse. 2005;40:703–719. doi: 10.1081/ja-200055393. [DOI] [PubMed] [Google Scholar]
- Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, Janssen RS. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harawa NT, Greenland S, Bingham TA, Johnson DF, Cochran SD, Cunningham WE, Valleroy LA. Associations of race/ethnicity with HIV prevalence and HIV-related behaviors among young men who have sex with men in 7 urban centers in the United States. Journal of Acquired Immune Deficiency Syndromes. 2004;35:526–536. doi: 10.1097/00126334-200404150-00011. [DOI] [PubMed] [Google Scholar]
- Harper GW. Sex isn’t that simple: culture and context in HIV prevention interventions for gay and bisexual male adolescents. American Psychologist. 2007a;62:803–819. doi: 10.1037/0003-066X.62.8.806. [DOI] [PubMed] [Google Scholar]
- Harper GW. Sex isn’t that simple: Culture and context in HIV prevention interventions for gay and bisexual male adolescents. American Psychologist. 2007b;62:806–819. doi: 10.1037/0003-066X.62.8.806. doi: 10.1037/0003-066x.62.8.806. [DOI] [PubMed] [Google Scholar]
- Hart T, Peterson JL, Community Intervention Trial for Youth Study, T. Predictors of risky sexual behavior among young African American men who have sex with men. American Journal of Public Health. 2004;94:1122–1124. doi: 10.2105/ajph.94.7.1122. doi: 94/7/1122 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin. 2009;135:707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RB, Kegeles SM, Coates TJ. High HIV risk-taking among young gay men. AIDS. 1990;4:901–907. doi: 10.1097/00002030-199009000-00011. [DOI] [PubMed] [Google Scholar]
- Hays RB, Rebchook GM, Kegeles SM. The Mpowerment Project: community-building with young gay and bisexual men to prevent HIV1. American Journal of Community Psychology. 2003;31:301–312. doi: 10.1023/a:1023966905973. [DOI] [PubMed] [Google Scholar]
- Herbst JH, Beeker C, Mathew A, McNally, Passin WF, Kay LS, Johnson RL. The effectiveness of individual-, group-, and community-level HIV behavioral risk-reduction interventions for adult men who have sex with men: A systematic review. American Journal of Preventive Medicine. 2007;32:S38–S67. doi: 10.1016/j.amepre.2006.12.006. doi: 10.1016/j.amepre.2006.12.006. [DOI] [PubMed] [Google Scholar]
- Herbst JH, Fielding JE, Abraido-Lanza A, Calonge N, Clymer J, Dickersin K, Task Force Community Preventive, S. Recommendations for use of behavioral interventions to reduce the risk of sexual transmission of HIV among men who have sex with men. American Journal of Preventive Medicine. 2007;32:S36–S37. doi: 10.1016/j.amepre.2006.12.005. doi: 10.1016/j.amepre.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Herek G, Sims C. Sexual orientation and violent victimization: Hate crimes and intimate partner violence among gay and bisexual males in the United States. In: Wolitski RJ, Stall R, Valdiserri R, editors. Unequal opportunity: Health disparities affecting gay and bisexual men in the United States. Oxford University Press; USA: 2007. pp. 35–71. [Google Scholar]
- Herek GM. Sexual Stigma and Sexual Prejudice in the United States: A Conceptual Framework. In: Hope DA, editor. Contemporary Perspectives on Lesbian, Gay, and Bisexual Identities. Vol. 54. 2009. pp. 65–111. [DOI] [PubMed] [Google Scholar]
- Herek GM, Gillis JR, Cogan JC. Psychological sequelae of hate-crime victimization among lesbian, gay, and bisexual adults. Journal of Consulting and Clinical Psychology. 1999;67:945–951. doi: 10.1037//0022-006x.67.6.945. [DOI] [PubMed] [Google Scholar]
- Hershberger S, D’Augelli AR. The impact of victimization on the mental health and suicidality of lesbian, gay, and bisexual youths. Developmental Psychology. 1995;31:65–74. [Google Scholar]
- Hershberger SL, D Augelli AR. The impact of vicitmization on mental health and suicidality of lesbian, gay, and bisexual youths. Developmental Psychology. 1995;31:65–74. [Google Scholar]
- Hirshfield S, Remien RH, Humberstone M, Walavalkar I, Chiasson MA. Substance use and high-risk sex among men who have sex with men: a national online study in the USA. AIDS Care. 2004;16:1036–1047. doi: 10.1080/09540120412331292525. [DOI] [PubMed] [Google Scholar]
- Hittner JB, Swickert R. Sensation seeking and alcohol use: a meta-analytic review. Addictive Behaviors. 2006;31:1383–1401. doi: 10.1016/j.addbeh.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Holmes WC, Foa EB, Sammel MD. Men’s pathways to risky sexual behavior: role of co-occurring childhood sexual abuse, posttraumatic stress disorder, and depression histories. Journal of Urban Health. 2005;82:i89–99. doi: 10.1093/jurban/jti028. doi: jti028 [pii] 10.1093/jurban/jti028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath KJ, Bowen AM, Williams ML. Virtual and physical venues as contexts for HIV risk among rural men who have sex with men. Health Psychology. 2006;25:237–242. doi: 10.1037/0278-6133.25.2.237. doi: 2006-03515-013 [pii] 10.1037/0278-6133.25.2.237. [DOI] [PubMed] [Google Scholar]
- Horvath KJ, Rosser BR, Remafedi G. Sexual risk taking among young internet-using men who have sex with men. Am J Public Health. 2008;98:1059–1067. doi: 10.2105/AJPH.2007.111070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle RH, Fejfar MC, Miller JD. Personality and sexual risk taking: A quantitative review. Journal of Personality. 2000;68:1203–1231. doi: 10.1111/1467-6494.00132. [DOI] [PubMed] [Google Scholar]
- Huebner DM, Rebchook GM, Kegeles SM. Experiences of harassment, discrimination, and physical violence among young gay and bisexual men. American Journal of Public Health. 2004;94:1200–1203. doi: 10.2105/ajph.94.7.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurt CB, Matthews DD, Calabria MS, Greene KA, Adimora AA, Golin CE, Hightow-Weidman LB. Sex with older partners is associated with primary HIV infection maong men who have sex with men in North Carolina. J Acquir Immune Defic Syndr. doi: 10.1097/QAI.0b013e3181c99114. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee HW, Valdiserri RO, De Cock KM. The Reemerging HIV/AIDS Epidemic in Men Who Have Sex With Men. JAMA. 2007;298:2412–2414. doi: 10.1001/jama.298.20.2412. [DOI] [PubMed] [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development : a longitudinal study of youth. Academic Press; New York: 1977. [Google Scholar]
- Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Sheldon LAJ. Interventions to Reduce Sexual Risk for the Human Immunodeficiency Virus in Adolescents, 1985-2000: A Research Synthesis. Arch Pediatr Adolesc Med. 2003;157:381–388. doi: 10.1001/archpedi.157.4.381. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- Johnson BT, Redding CA, DiClemente RJ, Dodge B, Mustanski BS, Sheeran P, Fishbein M. Toward a network-individual-resource framework for HIV prevention. AIDS and Behavior. 2010 doi: 10.1007/s10461-010-9803-z. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD001230.pub2. CD001230. [DOI] [PubMed] [Google Scholar]
- Kahn JG, Kegeles SM, Hays R, Beltzer N. Cost-effectiveness of the Mpowerment Project, a community-level intervention for young gay men. Journal of Acquired Immune Deficiency Syndromes. 2001;27:482–491. doi: 10.1097/00126334-200108150-00010. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Heckman T, Kelly JA. Sensation seeking as an explanation for the association between substance use and HIV-related risky sexual behavior. Archives of Sexual Behavior. 1996;25:141–154. doi: 10.1007/BF02437933. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Tannenbaum L, Nachimson D. Personality and cognitive factors influencing substance use and sexual risk for HIV infection among gay and bisexual men. Psychology Addictive Behaviors. 1998a;12:262–271. [Google Scholar]
- Kalichman SC, Tannenbaum L, Nachimson D. Personality and cognitive factors influencing substance use and sexual risk for HIV infection among gay and bisexual men. Psychology of Addictive Behaviors. 1998b;12:262–271. [Google Scholar]
- Kegeles S, Hays R, Pollack L, Coates T. Mobilizing young gay and bisexual men for HIV prevention: a two-community study. AIDS. 1999;13:1753. doi: 10.1097/00002030-199909100-00020. [DOI] [PubMed] [Google Scholar]
- Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: a community-level HIV prevention intervention for young gay men. American Journal of Public Health. 1996;86:1129–1136. doi: 10.2105/ajph.86.8_pt_1.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim AA, Kent C, McFarland W, Klausner JD. Cruising on the internet highway. Journal of Acquired Immune Deficiency Syndromes. 2001;28:89–93. doi: 10.1097/00042560-200109010-00013. [DOI] [PubMed] [Google Scholar]
- Kippax S, Noble J, Prestage G, Crawford JM, Campbell D, Baxter D, Cooper D. Sexual negotiation in the AIDS era: negotiated safety revisited. AIDS. 1997;11:191–197. doi: 10.1097/00002030-199702000-00009. [DOI] [PubMed] [Google Scholar]
- Koblin B, Chesney M, Husnik M, Bozeman S, Celum C, Buchbinder S, Team, E. S. High-Risk Behaviors Among Men Who Have Sex With Men in 6 US Cities: Baseline Data From the EXPLORE Study. Am J Public Health. 2003a;93:926–932. doi: 10.2105/ajph.93.6.926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Chesney MA, Husnik MJ, Bozeman S, Celum CL, Buchbinder S, Team, E. S. High-risk behaviors among men who have sex with men in 6 US cities: baseline data from the EXPLORE Study. American Journal of Public Health. 2003b;93:926–932. doi: 10.2105/ajph.93.6.926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Torian L, Xu G, Guilin V, Makki H, MacKellar D, Valleroy L. Violence and HIV-related risk among young men who have sex with men. AIDS Care: Psychological and Socio-medical Aspects of AIDS/HIV. 2006;18:961–967. doi: 10.1080/09540120500467182. [DOI] [PubMed] [Google Scholar]
- Kong TS. Risk factors affecting condom use among male sex workers who serve men in China: a qualitative study. Sex Transm Infect. 2008;84:444–448. doi: 10.1136/sti.2008.030650. doi: 84/6/444 [pii] 10.1136/sti.2008.030650. [DOI] [PubMed] [Google Scholar]
- Kubicek K, Carpineto J, McDavitt B, Weiss G, Iverson EF, Au CW, Kipke MD. Integrating professional and folk models of HIV risk: YMSM’s perceptions of high-risk sex. AIDS Education and Prevention. 2008;20:220–238. doi: 10.1521/aeap.2008.20.3.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankenau SE, Clatts MC, Welle D, Goldsamt LA, Gwadz MV. Street careers: homelessness, drug use, and sex work among young men who have sex with men (YMSM) Int J Drug Policy. 2005;16:10–18. doi: 10.1016/j.drugpo.2004.07.006. [Google Scholar]
- Leigh BC. Alcohol and condom use: a meta-analysis of event-level studies. Sexually Transmitted Diseases. 2002;29:476–482. doi: 10.1097/00007435-200208000-00008. [DOI] [PubMed] [Google Scholar]
- Lerner RM, Galambos NL. Adolescent development: Challenges and opportunities for research, programs, and policies. Annual Review of Psychology. 1998;49:413–446. doi: 10.1146/annurev.psych.49.1.413. [DOI] [PubMed] [Google Scholar]
- Liu H, Cai Y, Rhodes AG, Hong F. Money boys, HIV risks, and the associations between norms and safer sex: a respondent-driven sampling study in Shenzhen, China. AIDS Behav. 2009;13:652–662. doi: 10.1007/s10461-008-9475-0. doi: 10.1007/s10461-008-9475-0. [DOI] [PubMed] [Google Scholar]
- Loftus J. America’s liberalization in attitudes toward homosexuality, 1973 to 1998. American Sociological Review. 2001;66:762–782. [Google Scholar]
- Lyles CM, Kay LS, Crepaz N, Herbst JH, Passin WF, Kim AS, Mullins MM. Best-evidence interventions: findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000-2004. American Journal of Public Health. 2007;97:133–143. doi: 10.2105/AJPH.2005.076182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macaluso M, Demand MJ, Artz LM, Hook EW., 3rd Partner type and condom use. AIDS. 2000;14:537–546. doi: 10.1097/00002030-200003310-00009. [DOI] [PubMed] [Google Scholar]
- MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, Janssen RS. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. Journal of Acquired Immune Deficiency Syndromes. 2005;38:603–614. doi: 10.1097/01.qai.0000141481.48348.7e. [DOI] [PubMed] [Google Scholar]
- Mastekaasa A. Marital-Status and Subjective Well-Being - a Changing Relationship. Social Indicators Research. 1993;29:249–276. [Google Scholar]
- McKirnan DJ, Ostrow DG, Hope B. Sex, drugs and escape: a psychological model of HIV-risk sexual behaviours. AIDS Care. 1996;8:655–669. doi: 10.1080/09540129650125371. [DOI] [PubMed] [Google Scholar]
- McKirnan DJ, Peterson PL. Psychosocial and cultural factors in alcohol and drug abuse: an analysis of a homosexual community. Addictive Behaviors. 1989;14:555–563. doi: 10.1016/0306-4603(89)90076-2. [DOI] [PubMed] [Google Scholar]
- McLean J, Boulton M, Brookes M, Lakhani D, Fitzpatrick R, Dawson J, Hart G. Regular partners and risky behaviour: why do gay men have unprotected intercourse? AIDS Care. 1994;6:331–341. doi: 10.1080/09540129408258645. [DOI] [PubMed] [Google Scholar]
- Meade CS, Kershaw TS, Hansen NB, Sikkema KJ. Long-term correlates of childhood abuse among adults with severe mental illness: adult victimization, substance abuse, and HIV sexual risk behavior. AIDS Behav. 2009;13:207–216. doi: 10.1007/s10461-007-9326-4. doi: 10.1007/s10461-007-9326-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mettey A, Crosby R, DiClemente RJ, Holtgrave DR. Associations between internet sex seeking and STI associated risk behaviours among men who have sex with men. Sexually Transmitted Infections. 2003;79:466–468. doi: 10.1136/sti.79.6.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Minority stress and mentahl-health in gay men. Journal of Health and Social Behavior. 1995;36:38–56. [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. doi: 10.1097/QAD.0b013e3282e9a64b00002030-200710010-00011 [pii] [DOI] [PubMed] [Google Scholar]
- Mimiaga MJ, Noonan E, Donnell D, Safren SA, Koenen KC, Gortmaker S, Mayer KH. Childhood Sexual Abuse Is Highly Associated With HIV Risk-Taking Behavior and Infection Among MSM in the EXPLORE Study. J Acquir Immune Defic Syndr. 2009 doi: 10.1097/QAI.0b013e3181a24b38. doi: 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreau-Gruet F, Jeannin A, Dubois-Arber F, Spencer B. Management of the risk of HIV infection in male homosexual couples. AIDS. 2001;15:1025–1035. doi: 10.1097/00002030-200105250-00011. [DOI] [PubMed] [Google Scholar]
- Morris M, Zavisca J, Dean L. Social and sexual networks: their role in the spread of HIV/AIDS among young gay men. AIDS Education and Prevention. 1995;7:24–35. [PubMed] [Google Scholar]
- Mullens AB, Staunton S, Debattista J, Hamernik E, Gill D. Sex on premises venue (SOPV) health promotion project in response to sustained increases in HIV notifications. Sexual Health. 2009;6:41–44. doi: 10.1071/sh07087. doi: SH07087 [pii] [DOI] [PubMed] [Google Scholar]
- Mustanski B. The influence of state and trait affect on HIV risk behaviors: A daily diary study of MSM. Health Psychology. 2007a;26:618–626. doi: 10.1037/0278-6133.26.5.618. [DOI] [PubMed] [Google Scholar]
- Mustanski B. Moderating Effects of Age on the Alcohol and Sexual Risk Taking Association: An Online Daily Diary Study of Men Who have Sex with Men. AIDS and Behavior. 2008;12:118–126. doi: 10.1007/s10461-007-9335-3. [DOI] [PubMed] [Google Scholar]
- Mustanski B. Ethical and regulatory issues with conducting sexuality research with LGBT adolescents: A call to action for a scientifically informed approach. Archives of Sexual Behavior. 2011;40:673–686. doi: 10.1007/s10508-011-9745-1. doi: 10.1007/s10508-011-9745-1. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Emerson E. Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual, and transgender youth. American Journal of Public Health. 2010 doi: 10.2105/AJPH.2009.178319. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial Health Problems Increase Risk for HIV Among Urban Young Men Who Have Sex With Men: Preliminary Evidence of a Syndemic in Need of Attention. Annals of Behavioral Medicine. 2007;34:37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Hunter J. Parents as agents of HIV prevention for gay, lesbian, and bisexual youth. In: Pequegnat W, Bell C, editors. Family and HIV/aids : cultural and contextual issues in prevention and treatment. Springer; New York: 2011. (pp. Chapter 12) [Google Scholar]
- Mustanski B, Lyons T, Garcia SC. Internet Use and Sexual Health of Young Men Who Have Sex with Men: A Mixed-Methods Study. Arch Sex Behav. doi: 10.1007/s10508-009-9596-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Lyons T, Garcia SC. Internet use and sexual health of young men who have sex with men: A mixed-methods study. Archives of Sexual Behavior. 2010a doi: 10.1007/s10508-009-9596-1. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Lyons T, Garcia SC. Internet Use and Sexual Health of Young Men Who Have Sex with Men: A Mixed-Methods Study. Arch Sex Behav. 2010b doi: 10.1007/s10508-009-9596-1. doi: 10.1007/s10508-009-9596-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Lyons T, Garcia SC. Internet use and sexual health of young men who have sex with men: A mixed-methods study. Arch Sex Behav. doi: 10.1007/s10508-009-9596-1. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Newcomb M. Longitudinal effects of partner and relationship characteristics on sexual risk taking in ethnically-diverse young men who have sex with men. 2010. under review.
- Mustanski B, Newcomb M, Garofalo R. Mental health of lesbian, gay, and bisexual youth: A developmental resiliency perspective. J Gay Lesbian Soc Serv. 2011;23:204–225. doi: 10.1080/10538720.2011.561474. doi: 10.1080/10538720.2011.561474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski BS. Getting Wired: Exploiting the Internet for the collection of valid sexuality data. Journal of Sex Research. 2001;38:292–301. [Google Scholar]
- Mustanski BS. Are sexual partners met online associated with HIV/STI risk behaviours? Retrospective and daily diary data in conflict. AIDS Care. 2007b;19:822–827. doi: 10.1080/09540120701237244. [DOI] [PubMed] [Google Scholar]
- Nanín JE, Parsons JT, Bimbi DS, Grov C, Brown J. Community reactions to campaigns addressing crystal methamphetamine use among gay and bisexual men in New York City. Journal of Drug Education. 2006;36:285–303. doi: 10.2190/9818-1W43-1876-2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Mustanski B. Moderators of the Relationship Between Internalized Homophobia and Risky Sexual Behavior in Men Who Have Sex with Men: A Meta-Analysis. Archives of Sexual Behavior. 2009 doi: 10.1007/s10508-009-9573-8. [DOI] [PubMed] [Google Scholar]
- Newcomb ME, Mustanski B. The Importance of Measuring Internalized Homophobia/Homonegativity: Reply to Ross, Rosser, and Smolenski (2010) Archives of Sexual Behavior. 2010;39:1209–1211. doi: 10.1007/s10508-010-9634-z. doi: 10.1007/s10508-010-9655-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman PA, Chakrapani V, Cook C, Shunmugam M, Kakinami L. Correlates of paid sex among men who have sex with men in Chennai, India. Sex Transm Infect. 2008;84:434–438. doi: 10.1136/sti.2008.031484. doi: 84/6/434 [pii] 10.1136/sti.2008.031484. [DOI] [PubMed] [Google Scholar]
- Noar SA, Black HG, Pierce LB. Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. AIDS. 2009;23:107–115. doi: 10.1097/QAD.0b013e32831c5500. doi: 10.1097/QAD.0b013e32831c5500. [DOI] [PubMed] [Google Scholar]
- O’Connell ME, Boat TF, Warner KE. Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities. National Academies Press; Washington, D.C.: 2009. [PubMed] [Google Scholar]
- O’Donnell L, Agronick G, San Doval A, Duran R, Myint-U A, Stueve A. Ethnic and gay community attachments and sexual risk behaviors among urban Latino young men who have sex with men. AIDS Educ Prev. 2002;14:457–471. doi: 10.1521/aeap.14.8.457.24109. [DOI] [PubMed] [Google Scholar]
- O’Leary A, Purcell D, Remien RH, Gomez C. Childhood sexual abuse and sexual transmission risk behaviour among HIV-positive men who have sex with men. AIDS Care. 2003;15:17–26. doi: 10.1080/0954012021000039725. [DOI] [PubMed] [Google Scholar]
- O’Leary A, Wolitski RJ, Remien RH, Woods WJ, Parsons JT, Moss S, Lyles CM. Psychosocial correlates of transmission risk behavior among HIV-seropositive gay and bisexual men. Aids. 2005;19(Suppl 1):S67–75. doi: 10.1097/01.aids.0000167353.02289.b9. doi: 00002030-200504001-00007 [pii] [DOI] [PubMed] [Google Scholar]
- Padilla M. Caribbean Pleasure Industry: Tourism, Sexuality, and AIDS in the Dominican Republic. University of Chicago Press; Chicago: 2007. [Google Scholar]
- Padilla M, Castellanos D, Guilamo-Ramos V, Reyes AM, Sanchez Marte LE, Soriano MA. Stigma, social inequality, and HIV risk disclosure among Dominican male sex workers. Soc Sci Med. 2008;67:380–388. doi: 10.1016/j.socscimed.2008.03.014. doi: S0277-9536(08)00147-0 [pii] 10.1016/j.socscimed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Bimbi DS. Intentional unprotected anal intercourse among sex who have sex with men: barebacking - from behavior to identity. AIDS Behav. 2007;11:277–287. doi: 10.1007/s10461-006-9135-1. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Bimbi DS, Koken JA, Halkitis PN. Factors related to childhood sexual abuse among Gay/Bisexual male Internet escorts. Journal of Child Sexual Abuse. 2005;14:1–23. doi: 10.1300/J070v14n02_01. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Grov C, Kelly BC. Club drug use and dependence among young adults recruited through time-space sampling. Public Health Reports. 2009;124:246–254. doi: 10.1177/003335490912400212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN. Sexual and drug-using practices of HIV-positive men who frequent public and commercial sex environments. AIDS Care. 2002;14:815–826. doi: 10.1080/0954012021000031886. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Koken JA, Bimbi DS. The use of the Internet by gay and bisexual male escorts: sex workers as sex educators. AIDS Care. 2004;16:1021–1035. doi: 10.1080/09540120412331292405. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Koken JA, Bimbi DS. Looking beyond HIV: Eliciting individual and community needs of male Internet escorts. Journal of Homosexuality. 2007;53:219–240. doi: 10.1300/J082v53n01_10. [DOI] [PubMed] [Google Scholar]
- Paul JP, Catania J, Pollack L, Stall R. Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: The Urban Men’s Health Study. Child Abuse Negl. 2001;25:557–584. doi: 10.1016/s0145-2134(01)00226-5. [DOI] [PubMed] [Google Scholar]
- Peplau LA, Fingerhut AW. The close relationships of Lesbians and gay men. Annual Review of Psychology. 2007;58:405–424. doi: 10.1146/annurev.psych.58.110405.085701. [DOI] [PubMed] [Google Scholar]
- Pequegnat W, Szapocznik J. Working with families in the era of HIV/AIDS. Sage; Thousand Oaks, Calif.: 2000. [Google Scholar]
- Pisani E, Girault P, Gultom M, Sukartini N, Kumalawati J, Jazan S, Donegan E. HIV, syphilis infection, and sexual practices among transgenders, male sex workers, and other men who have sex with men in Jakarta, Indonesia. Sex Transm Infect. 2004;80:536–540. doi: 10.1136/sti.2003.007500. doi: 80/6/536 [pii] 10.1136/sti.2003.007500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American Journal of Health Promotion. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Johnson C, Lansky A, Prejean J, Stein R, Denning P, Crepaz N. Calculating HIV and Syphilis rates for risk groups: Estimating the national population size of men who have sex with men. Paper presented at the National STD Prevention Conference; Atlanta, GA. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell DW, Patterson JD, Spikes PS. Childhood sexual abuse experienced by gay and bisexual men: understanding the disparities and interventions to help eliminate them. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity : health disparities affecting gay and bisexual men in the United States. Oxford University Press; New York: 2007. pp. 72–96. [Google Scholar]
- Rebchook GM, Kegeles SM, Huebner D, Team, T. R. Translating research into practice: the dissemination and initial implementation of an evidence-based HIV prevention program. AIDS Educ Prev. 2006;18:119–136. doi: 10.1521/aeap.2006.18.supp.119. doi: 10.1521/aeap.2006.18.supp.119. [DOI] [PubMed] [Google Scholar]
- Relf MV. Childhood sexual abuse in men who have sex with men: the current state of the science. J Assoc Nurses AIDS Care. 2001;12:20–29. doi: 10.1016/S1055-3290(06)60260-4. [DOI] [PubMed] [Google Scholar]
- Relf MV, Huang B, Campbell J, Catania J. Gay identity, interpersonal violence, and HIV risk behaviors: an empirical test of theoretical relationships among a probability-based sample of urban men who have sex with men. J Assoc Nurses AIDS Care. 2004a;15:14–26. doi: 10.1177/1055329003261965. doi: 10.1177/1055329003261965. [DOI] [PubMed] [Google Scholar]
- Relf MV, Huang B, Campbell J, Catania J. Gay Identity, Interpersonal Violence, and HIV Risk Behaviors: An Empirical Test of Theoretical Relationships Among a Probability-Based Sample of Urban Men Who Have Sex With Men. Journal of the Association of Nurses in AIDS Care. 2004b;15:14–26. doi: 10.1177/1055329003261965. [DOI] [PubMed] [Google Scholar]
- Remafedi G. Cognitive and behavioral adaptations to HIV/AIDS among gay and bisexual adolescents. Journal of Adolescent Health. 1994;15:142–148. doi: 10.1016/1054-139x(94)90541-x. [DOI] [PubMed] [Google Scholar]
- Remafedi G. Suicidality in a venue-based sample of young men who have sex with men. Journal of Adolescent Health. 2002;31:305–310. doi: 10.1016/s1054-139x(02)00405-6. [DOI] [PubMed] [Google Scholar]
- Rietmeijer CA, Wolitski RJ, Fishbein M, Corby NH, Cohn DL. Sex hustling, injection drug use, and non-gay identification by men who have sex with men. Associations with high-risk sexual behaviors and condom use. Sex Transm Dis. 1998;25:353–360. doi: 10.1097/00007435-199808000-00006. [DOI] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, Hunter J. A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS Education and Prevention. 2006;18:444–460. doi: 10.1521/aeap.2006.18.5.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross MW, Mattison AM, Franklin D. Club drugs and sex on drugs are associated with different motivations for gay circuit party attendance in men. Subst Use Misuse. 2003;38:1173–1183. doi: 10.1081/ja-120017657. [DOI] [PubMed] [Google Scholar]
- Ross MW, Rosser BR, Smolenski D. The Importance of Measuring Internalized Homophobia/Homonegativity. Archives of Sexual Behavior. 2010 doi: 10.1007/s10508-010-9634-z. doi: 10.1007/s10508-010-9634-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz J, Facer M, Sun RK. Risk factors for human immunodeficiency virus infection and unprotected anal intercourse among young men who have sex with men. Sexually Transmitted Diseases. 1998;25:100–107. doi: 10.1097/00007435-199802000-00007. [DOI] [PubMed] [Google Scholar]
- Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123:346–352. doi: 10.1542/peds.2007-3524. [DOI] [PubMed] [Google Scholar]
- Santelli J, Ott MA, Lyon M, Rogers J, Summers D, Schleifer R. Abstinence and abstinence-only education: a review of U. S. policies and programs. Journal of Adolescent Health. 2006;38:72–81. doi: 10.1016/j.jadohealth.2005.10.006. doi: S1054-139X(05)00467-2 [pii] 10.1016/j.jadohealth.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Savin-Williams RC. Who’s Gay? Does It Matter? Current Directions in Psychological Science. 2006;15:40–44. [Google Scholar]
- Savin-Williams RC, Diamond LM. Sexual identity trajectories among sexual-minority youths: gender comparisons. Archives of Sexual Behavior. 2000;29:607–627. doi: 10.1023/a:1002058505138. [DOI] [PubMed] [Google Scholar]
- Sawires SR, Dworkin SL, Fiamma A, Peacock D, Szekeres G, Coates TJ. Male circumcision and HIV/AIDS: challenges and opportunities. The Lancet. 2007;369:708–713. doi: 10.1016/S0140-6736(07)60323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal DW, Kelly JA, Bloom FR, Stevenson LY, Coley BI, Broyles LA. HIV prevention with young men who have sex with men: What young men themselves say is needed. AIDS Care. 2000;12:5–26. doi: 10.1080/09540120047431. doi: 10.1080/09540120047431. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Grant I. The sexual negotiation behavior of HIV-positive gay and bisexual men. Journal of Consulting and Clinical Psychology. 2000;68:934–937. [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Grant I. HIV-positive gay and bisexual men: predictors of unsafe sex. AIDS Care. 2003;15:3–15. doi: 10.1080/713990434. [DOI] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: evidence from controlled studies, methodological critique, and suggestions for research. Clin Psychol Rev. 2008;28:711–735. doi: 10.1016/j.cpr.2007.10.002. doi: S0272-7358(07)00181-X [pii] 10.1016/j.cpr.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Meade CS, Kochman A, Fox AM. Psychosocial predictors of sexual HIV transmission risk behavior among HIV-positive adults with a sexual abuse history in childhood. Arch Sex Behav. 2009;38:121–134. doi: 10.1007/s10508-007-9238-4. doi: 10.1007/s10508-007-9238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon Rosser BR, West W, Weinmeyer R. Are gay communities dying or just in transition? Results from an international consultation examining possible structural change in gay communities. AIDS Care. 2008;20:588–595. doi: 10.1080/09540120701867156. doi: 793154625 [pii] 10.1080/09540120701867156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M. AIDS and the health crisis of the U.S. urban poor; the perspective of critical medical anthropology. Social Science and Medicine. 1994;39:931–948. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- Singer M. A dose of drugs, a touch of violence and case of AIDS: Conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology. 1996;24:99–110. [Google Scholar]
- Singer MC, Erickson PI, Badiane L, Diaz R, Ortiz D, Abraham T, Nicolaysen AM. Syndemics, sex and the city: understanding sexually transmitted diseases in social and cultural context. Soc Sci Med. 2006;63:2010–2021. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MD, Grov C. In The Company of Men: Inside the Lives of Male Prostitutes. Praeger; Santa Barbara: 2011. [Google Scholar]
- Somerville LH, Jones RM, Casey BJ. A time of change: behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain and Cognition. 2010;72:124–133. doi: 10.1016/j.bandc.2009.07.003. doi: S0278-2626(09)00112-2 [pii] 10.1016/j.bandc.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and the college drinker: biological basis of propensity to use and misuse alcohol. Journal of Studies on Alcohol. Supplement. 2002:71–81. doi: 10.15288/jsas.2002.s14.71. [DOI] [PubMed] [Google Scholar]
- Stall R, Duran L, Wisniewski SR, Friedman MS, Marshal MP, McFarland W, Mills TC. Running in place: implications of HIV incidence estimates among urban men who have sex with men in the United States and other industrialized countries. AIDS and Behavior. 2009;13:615–629. doi: 10.1007/s10461-008-9509-7. doi: 10.1007/s10461-008-9509-7 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Friedman M, Catania J. Interacting Epidemics and Gay Men’s Health: A Theory of Syndemic Production among Urban Gay Men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity : health disparities affecting gay and bisexual men in the United States. Oxford University Press; New York: 2007. [Google Scholar]
- Stall R, Friedman M, Catania J. Interacting epidemics and gay menís health: A theory of syndemic production among urban gay men. In: Wolitski RJ, Stall R, Valdiserri R, editors. Unequal opportunity: Health disparities affecting gay and bisexual men in the United States. Oxford University Press; 2008. pp. 251–275. [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greendwood G, Paul JP, Catania J. Association of co-occuring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby G, Catania JA. Alcohol use, drug use and alcohol-related problems among men who have sex with men: The Urban Men’s Health Study. Addiction. 2001;96:1589–1601. doi: 10.1046/j.1360-0443.2001.961115896.x. [DOI] [PubMed] [Google Scholar]
- Stall RD, Purcell DW. Intertwining Epidemics: A Review of Research on Substance Use Among Men Who Have Sex With Men and its Connection to the AIDS Epidemic. AIDS and Behavior. 2000;4:181–192. [Google Scholar]
- Steinberg L. A Social Neuroscience Perspective on Adolescent Risk-Taking. Developmental Review. 2008;28:78–106. doi: 10.1016/j.dr.2007.08.002. doi: 10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stueve A, O’Donnell L, Duran R, San Doval A, Geier J. Being high and taking sexual risks: findings from a multisite survey of urban young men who have sex with men. AIDS Education and Prevention. 2002;14:482–495. doi: 10.1521/aeap.14.8.482.24108. [DOI] [PubMed] [Google Scholar]
- Suarez T, Miller J. Negotiating risks in context: a perspective on unprotected anal intercourse and barebacking among men who have sex with men--where do we go from here? Archives of Sexual Behavior. 2001;30:287–300. doi: 10.1023/a:1002700130455. [DOI] [PubMed] [Google Scholar]
- Sullivan PS, Hamouda O, Delpech V, Geduld JE, Prejean J, Semaille C, Annecy, M. S. M. E. S. G. Reemergence of the HIV epidemic among men who have sex with men in North America, Western Europe, and Australia, 1996-2005. Annals of Epidemiology. 2009;19:423–431. doi: 10.1016/j.annepidem.2009.03.004. doi: S1047-2797(09)00075-1 [pii] 10.1016/j.annepidem.2009.03.004. [DOI] [PubMed] [Google Scholar]
- Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–1162. doi: 10.1097/QAD.0b013e32832baa34. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- Sumartojo E. Structural factors in HIV prevention: concepts, examples, and implications for research. Aids. 2000;14(Suppl 1):S3–10. doi: 10.1097/00002030-200006001-00002. [DOI] [PubMed] [Google Scholar]
- Thiede H, Valleroy LA, MacKellar DA, Celentano DD, Ford WL, Hagan H, Torian LV. Regional patterns and correlates of substance use among young men who have sex with men in 7 US urban areas. American Journal of Public Health. 2003;93:1915–1921. doi: 10.2105/ajph.93.11.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tun W, de Mello M, Pinho A, Chinaglia M, Diaz J. Sexual risk behaviours and HIV seroprevalence among male sex workers who have sex with men and non-sex workers in Campinas, Brazil. Sex Transm Infect. 2008;84:455–457. doi: 10.1136/sti.2008.031336. doi: 84/6/455 [pii] 10.1136/sti.2008.031336. [DOI] [PubMed] [Google Scholar]
- Valleroy LA, MacKellar DA, Karon JM. HIV prevalence and associated risks in young men who have sex with men: Young Men’s Survey Study Group. Journal of the American Medical Association. 2000;284:198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- Vanable PA, McKirnan DJ, Buchbinder SP, Bartholow BN, Douglas JM, Jr., Judson FN, MacQueen KM. Alcohol use and high-risk sexual behavior among men who have sex with men: the effects of consumption level and partner type. Health Psychology. 2004;23:525–532. doi: 10.1037/0278-6133.23.5.525. [DOI] [PubMed] [Google Scholar]
- Vergidis PI, Falagas ME. Meta-analyses on Behavioral Interventions to Reduce the Risk of Transmission of HIV. Infectious Disease Clinics of North America. 2009;23:309. doi: 10.1016/j.idc.2009.02.001. +. doi: 10.1016/j.idc.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Voetsch AC, Heffelfinger JD, Begley EB, Jafa-Bhushan K, Sullivan PS. Knowledge and use of preexposure and postexposure prophylaxis among attendees of Minority Gay Pride events, 2005 through 2006. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2007;46:378–380. doi: 10.1097/QAI.0b013e3181576874. doi: 10.1097/QAI.0b013e3181576874. [DOI] [PubMed] [Google Scholar]
- Waldo CR, McFarland W, Katz MH, MacKellar D, Valleroy LA. Very young gay and bisexual men are at risk for HIV infection: the San Francisco Bay Area Young Men’s Survey II. J Acquir Immune Defic Syndr. 2000;24:168–174. doi: 10.1097/00126334-200006010-00012. [DOI] [PubMed] [Google Scholar]
- Warren JC, Fernandez MI, Harper GW, Hidalgo MA, Jamil OB, Torres RS. Predictors of Unprotected Sex among Young Sexually Active African American, Hispanic, and White MSM: The Importance of Ethnicity and Culture. AIDS and Behavior. 2007 doi: 10.1007/s10461-007-9291-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weatherburn P, Davies PM, Hickson FC, Hunt AJ, McManus TJ, Coxon AP. No connection between alcohol use and unsafe sex among gay and bisexual men. AIDS. 1993;7:115–119. doi: 10.1097/00002030-199301000-00018. [DOI] [PubMed] [Google Scholar]
- Welles SL, Baker AC, Miner MH, Brennan DJ, Jacoby S, Rosser BR. History of childhood sexual abuse and unsafe anal intercourse in a 6-city study of HIV-positive men who have sex with men. Am J Public Health. 2009;99:1079–1086. doi: 10.2105/AJPH.2007.133280. doi: AJPH.2007.133280 [pii] 10.2105/AJPH.2007.133280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JK, Wyatt GE, Rivkin I, Ramamurthi HC, Li X, Liu H. Risk Reduction for HIV-Positive African American and Latino Men with Histories of Childhood Sexual Abuse. Arch Sex Behav. 2008 doi: 10.1007/s10508-008-9366-5. doi: 10.1007/s10508-008-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson HW, Widom CS. Does physical abuse, sexual abuse, or neglect in childhood increase the likelihood of same-sex sexual relationships and cohabitation? A prospective 30-year follow-up. Archives of Sexual Behavior. 2010;39:63–74. doi: 10.1007/s10508-008-9449-3. doi: 10.1007/s10508-008-9449-3. [DOI] [PubMed] [Google Scholar]
- Wolitski RJ, Valdiserri RO, Denning PH, Levine WC. Are we headed for a resurgence of the HIV epidemic among men who have sex with men? American Journal of Public Health. 2001;91:883–888. doi: 10.2105/ajph.91.6.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong FY, Huang ZJ, He N, Smith BD, Ding Y, Fu C, Young D. HIV risks among gay- and non-gay-identified migrant money boys in Shanghai, China. AIDS Care. 2008;20:170–180. doi: 10.1080/09540120701534707. doi: 790753340 [pii] 10.1080/09540120701534707. [DOI] [PubMed] [Google Scholar]
- Young RM, Meyer IH. The Trouble With “MSM” and “WSW”: Erasure of the Sexual-Minority Person in Public Health Discourse. American Journal of Public Health. 2005;95:1144–1149. doi: 10.2105/AJPH.2004.046714. doi: 10.2105/ajph.2004.046714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zea MC, Reisen CA, Poppen PJ, Bianchi FT. Unprotected anal intercourse among immigrant Latino MSM: the role of characteristics of the person and the sexual encounter. AIDS and Behavior. 2009;13:700–715. doi: 10.1007/s10461-008-9488-8. doi: 10.1007/s10461-008-9488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M. Behavioral Expressions and Biosocial Bases of Sensation Seeking. Cambridge University Press; Cambridge: 1994. [Google Scholar]