Abstract
The term breech trial (TBT) has brought about radical changes but it is debatable whether it provides unequivocal evidence regarding the practice of breech deliveries. There is a need to publish the data of a study that was performed before the era of the TBT in a hospital where there was a high rate of breech vaginal delivery. The objectives were to ascertain the incidence, mode of delivery and fetal outcome in singleton breech deliveries. The study design was a retrospective cohort study where 165 consecutive breech and 165 controls (cephalic) were included. Statistical analysis, used were Chi squared and Fischer’s exact test. P<0.05 is taken as the level of significance. The incidence of breech deliveries was found to be 3% and has remained fairly constant but the rate of breech vaginal delivery has fallen and the CS rates have increased. Even though more breech compared to controls were significantly sectioned, majority of the breeches {n=137 (83%)} were planned for vaginal delivery and in these patients two-thirds attained vaginal delivery. There was 1 fetal death in the CS group compared to 12 deaths in the vaginally delivered breech. However, most death in the breech delivered vaginally are unavoidable. In conclusion, there is a high rate of breech vaginal delivery in this series of patients and most perinatal deaths were not related to the mode of delivery.
Keywords: Breech deliveries, vaginal deliveries, Caesarean section, perinatal mortality
Introduction
The incidence of breech delivery is only 3% (1) but it seems to be associated with a higher perinatal mortality (PMR) (2) and morbidity (3, 4). On the assumption that perinatal morbidity and mortality can be reduced (5), Wright (1959) proposed Caesarean section (CS) for all breeches (5). Prior to the era of Term Breech Trial (TBT) (6), the trend of increasing CS for breech presentation became widespread without evidence from randomized trials. However, current evidence from the Cochrane review (the analysis is mainly the TBT by Hannah et. al., (2000) (6) showed that perinatal or neonatal death (excluding fatal anomalies) or serious neonatal morbidity was reduced {relative risk (RR) 0.33, 95% confidence interval (CI) 0.19 to 0.56} with planned caesarean section (7). The TBT by Hannah et. al., (2000) (6) is a methodologically sound clinical trial as the sample size is large and it is randomized. However various authors are unsatisfied with the results and have questioned and criticized the trial for various reasons (8,9,10). Kotaska et al (2004) criticized the study for failing to appreciate the complex nature of breech delivery and the complex mix of operator variable (10). In addition, there is bias of license here as the practitioners are protected by the medico legal liability of a randomized trial, hence the protocol is considered rather liberal (10). Moreover the aspects of clinical care are also imprecisely defined (8). Furthermore, only a minority of the perinatal death is attributed to the mode of delivery and the countries included had varying degrees of perinatal mortality (9,11). In addition, serious neonatal morbidity is loosely defined (9,11). There is also no information on the consequences of a uterine scar for future pregnancies (12) and of the long-term consequences on reproductive function and emotional adjustment (7). The study is also too small to assess maternal mortality. In addition, the authors of the Cochrane review (7) are also the authors of the TBT and conflict may arise in the interpretation of data in the systematic review. Therefore, it is debatable whether the TBT provides unequivocal evidence that caesarean section is the answer to all term breech presentation (13).
In addition, Cesarean delivery has been shown to increase both short and long-term maternal morbidity and maternal mortality (14,15,16, 17). This policy will not only lead to an increase in CS rate but will also lead to an increased repeat Caesarean in subsequent pregnancies (18). Furthermore, there are studies (randomized and observational) that have found no increased in adverse perinatal or neonatal outcome with vaginal delivery (4,13, 19,20,21,22,23).
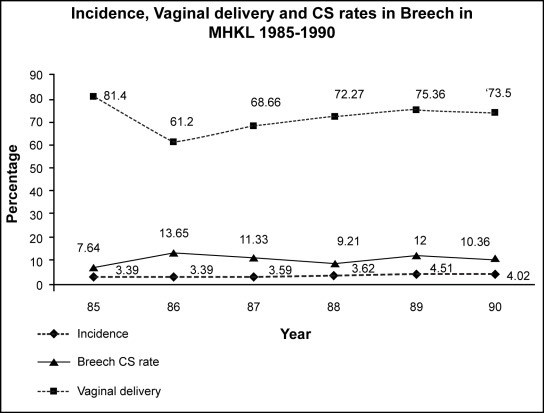
There is a need to publish this data now as the results from the term breech trial favors Caesarean section and in spite of the evidence from this randomized control trial, there were authors that disagreed with routine C-section for all term breech presentation. This study was performed in the era before the term breech trial in a center with a high workload i.e (10 000 deliveries per year) (24,25,26) and a high rate of vaginal breech delivery (figure 1) where experienced accouchers were available. In this center, cases were carefully selected for vaginal delivery with close monitoring during labour, and there was a low threshold for CS. The mode of delivery, fetal outcome and causes of perinatal mortality was ascertained. In addition, the incidence, rate of vaginal breech delivery and CS rates due to breech in this study population is ascertained in late eighties during the period of the study from 1985–1990 (24,25,26) and compared to the current rates in the late nineties and the new millennium from 1998 to 2001 (27,28).
Figure 1:
The pattern of breech delivery in the university unit in MHKL. The incidence is fairly constant where it is around 3 to 4 %. This graph depicts the high rate of vaginal delivery in breech from 60 up to 80 percent. The CS rate showed fluctuations (Annual Report University Unit Maternity Hospital Kuala Lumpur 1987–1990).
Methodology
The study was carried out in the Maternity Hospital Kuala Lumpur in the university unit. The department approved the study proposal. The study design was a cohort study of all consecutive breech deliveries during a six-month period, where 165 consecutive breech deliveries and 165 controls were included. The case notes were traced from September 1989 retrospectively and analyzed in detail. Multiple pregnancies were excluded. Both term and the preterm breeches were included. The policy of the unit is to allow vaginal delivery in selected cases after the exclusion of cephalo pelvic disproportion. Assessment of the pelvis is by clinical pelvic assessment and if indicated, the ELP. The birth weight is estimated clinically and by ultrasound.
The groups were divided into elective CS and trial of vaginal delivery. The group under trial of vaginal delivery was further subdivided into those who achieved successful vaginal delivery and those who underwent emergency Caesarean section. The fetal outcome was assessed in terms of Apgar score and perinatal mortality. The control groups were patients with cephalic presentation and comprised of subsequent patients with cephalic presentation who delivered after the breech delivery. The mode of delivery of the primparae was also compared to the multiparae.
The overall incidence, CS rate due to breech deliveries and the rate of breech vaginal delivery from 1985 to 1990 (24,25,26) and 1998 to 2002 (27,28) were obtained from the annual reports and database and tabulated. Statistical analysis is by chi squared, student t test and odds ratio. The level of significance is p<0.05. Chi squared test, Fischer exact test and Mantel Hanzel tests were used where appropriate.
Results
Sociodemographic data
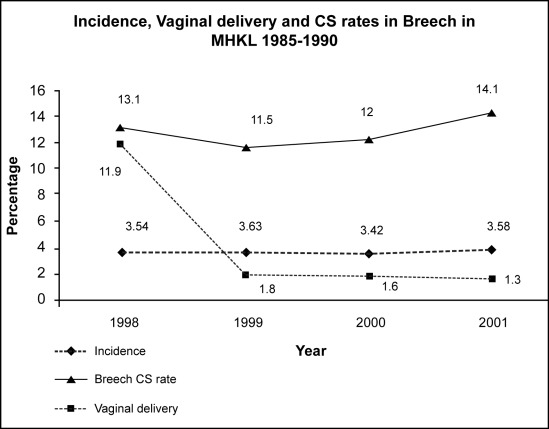
During the study period, there were a total of 165 breech deliveries and 165 controls. The incidence of breech deliveries over the six months period was found to be 3.8% (165 in 4334 deliveries). The incidence from 1985 to 1990 (Figure 1) compared to 1999 to 2002 (Figure 2) was similar and was fairly constant (Figure 2). There was however, a marked change in the management of breech delivery (Figure 1 & 2). The vaginal delivery rate was 56 % in the breech group in this study population. Comparatively, the rate of vaginal delivery in breech (Figure 1) ranges from 60 up to 80 percent in the late eighties, and there was a marked drop to 12% in 1999 and less than 2% in 2000–2001 (Figure 2). The CS rate due to breech as compared to other indications showed a wide fluctuation in the late eighties i.e. a rise from 7.64% in 1985 to 13.65% (1986) and the rate then ranged between 9–12% (1987–1990). In the late nineties, the rate of CS for the indication of breech presentation has shown an increased from 11.5% in 1999 to 14.1% in 2001 (Figure 1 & 2).
Figure 2:
The pattern of breech delivery in MHKL (1998–2001). The incidence is fairly constant around 3.4–3.6%. The breech vaginal delivery showed a decreasing trend and CS showed an increasing trend (Annual report Maternity Hospital Kuala Lumpur 1999/2000, 2001).
In the study population there were 39% (n=63) primigravida and 61% (n=102) multigravida. There was no association of breech pregnancies with parity (p=0.248), ethnicity (p =0.2039), or booking status (p=0.4041) (Table 1). Most were booked (Table 1) even though they were booked late in the third trimester (Table 1).
Table 1.
Socio demographic data, delivery and fetal outcome.
| Factor of Interest | Breech n=165 | Controls n=165 | p value | relative risk |
|---|---|---|---|---|
| Party | ||||
| Primip | 63 | 53 | ||
| Multip | 102 | 112 | ||
| 0.2489 | 1.139 (0.916;1.147) | |||
| Race | ||||
| Malay | 101 | 104 | ||
| Chinese | 38 | 30 | ||
| Indian | 19 | 21 | ||
| Others | 7 | 10 | ||
| 0.2039 | ||||
| Booking status | ||||
| Booked | 18 | 23 | ||
| Unbooked | 147 | 142 | ||
| 0.4041 | 0.863 (0.600;1.242) | |||
| Delivery | ||||
| Planned delivery | ||||
| Elective CS | 28 | 4 | ||
| Trial of vaginal del | 137 | 161 | ||
| ≤0.001 | 7.000(2.511;19.513) | |||
| Trial of vaginal delivery | ||||
| SVD | 92 | 150 | ||
| EM CS | 45 | 11 | ||
| ≤0.001 | 4.808 (2.590;8.925) | |||
| Final Mode of delivery | ||||
| CS (total) | 73 | 15 | ||
| SVD | 92 | 150 | ||
| ≤0.001 | 4.867 (2.917;8.121) | |||
| Fetal outcome | ||||
| PNM (total) | 13 | 5 | ||
| FSB | 3 | 1 | ||
| MSB | 5 | 2 | ||
| NND | 5 | 2 | 0.10 | |
| PNM (total) | ||||
| Vaginal | 12 | 5 | ||
| CS | 1 | 0 | ||
| 0.523 |
Mode of delivery
Overall, CS was significantly 4.8 times higher in the breech compared to controls. (p≤0.001 RR 4.867 CI 2.917 – 8.121). (Table 1) However, even though significantly more breech presentation (12%) were electively sectioned (p≤0.001 RR 7.000 CI 2.511–19.513) compared to controls, the majority {n=137 (83 %)} were planned for vaginal delivery (Table 1). In those breech presentation that were planned for trial of vaginal delivery, more breech were sectioned as emergency when compared to controls (p ≤0.001, RR 4.808 CI 2.590; 8.925). In those breech that were planned for trial of vaginal delivery, two thirds attained vaginal delivery and one third (45 out of the 137) ended in emergency CS. Finally, even though Caesarean section was found to be significantly higher in breech deliveries (p≤0.001), 55 % attained vaginal delivery. In addition, 50% of primigravid breeches (31/63) and 60% of multigravid (61/102) breeches achieved vaginal delivery (Table 1).
Mode of delivery in the different parity
However in the primipara there was no significant difference in elective CS and trial of vaginal delivery (p=0.141) compared to controls (Table 2). However, more multipara was planned for elective CS compared to controls (p≤0.001 RR 2.153 CI 1.749 – 2.650) Table 2. When comparing multips and primips, no significant difference was found between elective Caesarean section (p=0.015) (Table 2). In the trial of vaginal delivery groups, significantly more multips (n=82) compared to primips (n=38) attained vaginal delivery (p≤0.001 RR 2.024 CI 1.231 – 3.327) (Table 2).
Table 2.
The mode of delivery in primiparae and multiparae.
| Group compared | ||||
|---|---|---|---|---|
| Delivery | Primips-63 | Control-53 | P value | Relative risk |
| Elective CS | 7 | 2 | ||
| Trial of vaginal delivery | 56 | 51 | ||
| 0.141 | 2.944 (0.639;13.576) | |||
| Delivery | Multips-102 | Control-112 | ||
| Elective CS | 21 | 81 | ||
| Trial of vaginal | 2 | 110 | ||
| ≤0.001 | 2.153 (1.749;2.650) | |||
| Mode of delivery | Primips n=63 | Multips n=102 | ||
| Elective CS | 7 | 21 | ||
| Trial | 56 | 81 | 0.115 | 0.540 (0.244;1.196) |
| EM CS | 25 | 20 | ||
| Vag delivery | 38 | 82 | 0.005 | 2.024 (1.231;3.327) |
Fetal outcome
Apgar score
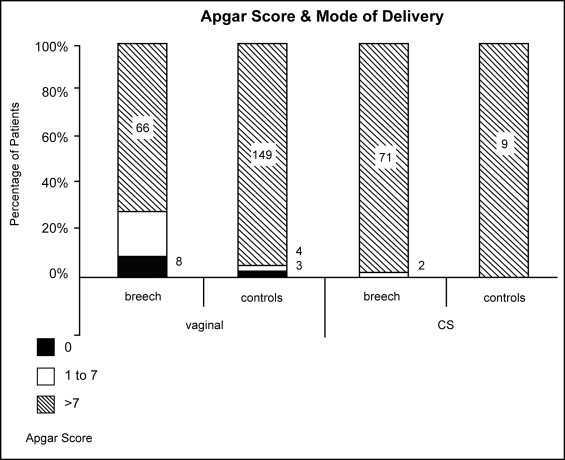
Apgar score (AS of >7) was significantly higher in the control group (149/156) (p≤0.001 RR 6.298 CI 0.658 – 0.858) compared to breech vaginal deliveries (66/92) even after the exclusion of stillbirths (p<0.001) (Figure 3). There was no significant difference in the AS in breeches delivered by CS compared to controls (p=0.612) (Figure 3). AS of >7 were significantly higher in the breeches that were sectioned (71/73) compared to breeches that were delivered vaginally (66 out of 92) (p≤0.001 RR1.443 CI 1.246 – 1.672) (Figure 3). In those breech babies with Apgar score of less than 7 whom delivered vaginally (excluding the 8 stillbirths), 14 out of 18 were discharged well. Unfortunately the 4 died due to complications of prematurity where the birth weight ranged from 1.5–2.0 g. In two of the babies that delivered via CS with Apgar score below 7, one died due to intrapartum asphyxia as a result of cord prolapse. The other baby survived and was discharged well.
Figure 3 :
Apgar score in breech and controls according to the mode of delivery P<0.001
Perinatal mortality
The causes of death, period of gestation and the weight of the babies are as listed in table 3. In this study, the perinatal mortality (PNM) of breech infants was 79/1000 compared to 30/1000 in the controls and 39/1000 for the hospital. PNM due to CS in breech is 6/1000 and in breech vaginal delivery is 72/1000. There was one PNM in the CS group (due to intrapartum asphyxia from cord prolapse) as compared to 12 in the vaginal delivery group. However, most of the perinatal deaths in the vaginal delivery group involved premature breech less than 34 weeks (n=11, 5 Intruterine deaths [IUD], 2 Fresh stillbirths [FSB], 4 Neonatal deaths [NND]) and most of these babies weighed between 1.5 to 2.0 kg (n= 11) (refer to table 3). Only 1 baby delivered vaginally was term but died due to congenital abnormality. These deaths were unavoidable and not related to the mode of delivery.
Table 3 :
Cause of perinatal mortality in breech pregnancies
| Type of PNM | Period of gestation (week) | Weight (kg) | Mode of Delivery | Cause of death |
|---|---|---|---|---|
| MSB n=5 | ||||
| Below 34 | 1500g | Unexplained | ||
| Below 34 | 2000g | Congenital syphilis | ||
| Below 34 | 1550g | Vaginal delivery | Unexplained | |
| Below 34 | 1600g | Unexplained | ||
| Below 34 | 1500g | Unexplained | ||
| FSB n=3 | ||||
| Above 38 | 2.25kg | Patau syndrome | ||
| Below 34 | 2.25kg | Vaginal delivery | Congenital abnormality | |
| Below 34 | 0.6kg | Severe prematurity | ||
| NND n=5 | ||||
| Above 38 | 2500g | CS | Cord prolapse (intrapartum asphyxia) | |
| Below 34 | 1600g | Necrotising enterocolitis | ||
| Below 34 | 1500g | Vaginal delivery | Septicaemia and RDS | |
| Below 34 | 1600g | Pulmonary haemorrhage | ||
| Below 34 | 1500g | RDS and prematurity | ||
Discussion
The incidence of breech deliveries over the six months period was found to be 3.8%, which was not so much different compared to the quoted incidence of 2.5–3.0% (29, 30).
There was however no association between parity with breech pregnancies, which was contrary to the reported findings that breech presentation, was commonest among primigravida (32.0%) and decreased with increasing parity (31).
The incidence of breech in the eighties and late nineties in MHKL has remained fairly constant. However the rate of breech vaginal delivery has dropped from 60–80% in the late eighties to 12% in 1998 and to less than 2% from 1999 onwards. This showed the impact of the term breech trial. The C-Section for breech in 1985–1990 widely fluctuated and this depicted the wide variation in the decision making process of breech deliveries at that time. However the C-Section rates for breech from 1999–2002 showed an increasing trend, which is not surprising (Figure 2).
Mode of Delivery
The increased C-section was expected in this study population. In the primigravida, it was unexpected that elective CS (7/65) was not much different as compared to controls. In addition, it was surprising that the elective Caesarean section was significantly higher in the multigravid breech pregnancies (21%, 21/102) as compared to the primigravid breech pregnancies (11%, 7/63). One would expect that the gynecologist would be more cautious in the primip as the pelvis has not been tested yet. However upon analysing the indications in the multigravida, it was found that the LSCS was unavoidable. The indications were big breech, cord presentation, previous LSCS, oblique breech, placenta praevia, post datism with unfavourable cervix, IUGR and premature rupture of membranes. In both the primips and multips, most patients were planned for trial of vaginal delivery and emergency CS was significantly higher when compared to controls. Therefore, it can be concluded that most of the obstetricians in this era tend to favour trial of vaginal delivery but has a low threshold for CS.
Fetal outcome
After the exclusion of stillbirths, as expected Apgar score of more than 7 in controls (cephalic presentation delivered through the vaginal route) were significantly higher compared to vaginal breech but no difference were noted in the CS group (breech 71/73, cephalic 9/9). Apgar score of above 7 of breech babies delivered via Caesarean section (71/73) was significantly better compared to vaginal breech delivery (66/84; p < 0.05). This is similar to the report where planned vaginal delivery was associated with a 15 times greater risk of low Apgar score than elective Caesarean section (32). However, in those with AS<7 (n=18), 4 died due to prematurity while the rest were discharged well.
Perinatal mortality
In the 8 stillbirths, this underlying situation influenced the mode of delivery rather than is caused by the vaginal delivery. The breech presentation in these instances was a predictor of poor perinatal outcome (33). It was found that after exclusion of antepartum stillbirths and congenital malformation, there was no significant difference in the intrapartum and early neonatal mortality rate in the breech delivered vaginally or by caesarean section (33). The four neonatal deaths in the breech pregnancies here were due to complications of prematurity. This was similar to the high incidence of prematurity as reported by various studies (30,34,35). However it is debatable whether these 4 neonatal deaths could be avoided if Caesarean sectioned has been performed. It was found that the main causes of death in the preterm breech differed compared to the term breech and they were prematurity (25%), congenital malformation (10%) and intraventricular haemorrhage (5%) (36). It was due to the increased perinatal mortality and morbidity that some authors advocate a more liberal or routine use of CS in the preterm breech. However, all the preterm neonatal deaths in this study series weighed between 1.5 to 2.0 kg, where it was found that the survival rate for these infants was not affected by mode of delivery (37). Unfortunately, this study by Crowley and Hawkins (1980) is retrospective in nature. The problem with the extreme low birth weight fetus is that the fetus is at the margins of viability where neonatal prognosis may be poor and difficult management decisions have to be made. A CS may leave the patient with a classical scar on the uterus and placed her at risk of uterine rupture in the subsequent pregnancy. Currently there is no convincing evidence that routine cesarean delivery results in improved perinatal outcome in the preterm breech (38).
Is vaginal delivery still a safe option?
There are studies that did not find statistically significant differences in mortality between the vaginally delivered group and the Caesarean section group (33,39). Unfortunately most of these studies that advocated vaginal delivery in the term breech are observational. However there are studies, which are performed on frank (7) and incomplete or footling breech presentation that are methodologically sound where it was found that in selected patients, vaginal delivery was still a safe option. (40,41). This contradicted the findings of TBT, which is a multi-centered trial with sufficient power. In the TBT however, the selection criteria for breech for planned vaginal delivery was not optimized where only 60 % of patients had assessment of fetal weight by ultrasound, less than 10 % had X ray pelvimetry performed (9) and there is the possibility of the inclusion of the growth retarded fetuses (8). 6 % of infants were more than 4 kg in the planned for vaginal delivery group compared to only 3.1% in the planned for CS group (9). Patients were induced; augmented and other forms of breech e.g. footling and the uncertain type were also included (9). When these were excluded, the perinatal mortality and morbidity was much reduced in the subgroup analysis. This showed that with better selection criteria and careful management in labor, the outcome of the breech delivered vaginally could be improved. In the breech presentation, labor augmentation (p=0.007) and birth weight less than 2.8 kg (p=0.003) increased the risk to the fetus, and these criteria should be used to exclude patients from undergoing vaginal deliveries (42). Safe breech vaginal delivery at term can be achieved with strict selection criteria, adherence to a careful intrapartum protocol and with an experienced obstetrician in attendance (23).
There is increased reluctance in many centers to allow vaginal birth in patients with breech presentation, after the publication of the Term Breech Trial (6). The alternative now to elective caesarean section is the external cephalic version. Young et al. (2001) suggested that the focus should now be on increasing the rate of offering external cephalic version (ECV), increasing its uptake and also its success to reduce the incidence of breech deliveries (43). ECV is by far superior to planned vaginal or planned CS (8).
The limitation of this study was that it was observational and retrospective in nature and some records and data may not be available or retrievable. Due to funding and time constraints, there was no data on long-term fetal and maternal morbidity. Even though TBT has been performed, it has been questioned whether a randomized trial is an appropriate method to apply to study such a complex procedure (10).
Conclusion
In this study, it was found that majority of the breech pregnancies (after careful selection) were planned for vaginal delivery and half of the primigravida (31 out of 56) and three quarters of the multigravida (61 out of 81) achieved vaginal delivery. The high rate of vaginal delivery showed the adequate exposure of the accouchers during this era. Most of the perinatal mortality was due to IUD, congenital abnormality and prematurity and there were no perinatal death related to mode of delivery or due to birth trauma.
Acknowledgments
Noranida Salehuddin and Noor Aisyah binti Abdul Mutholid for their technical assistance. This study received no funding.
References
- 1.Johanson RB. Malposition and Malpresentation and Cephalopelvic Disproportion. In: Edmonds DK, editor. Dewhurst’s Textbook of Obstetrics and Gynaecology for Postgraduates. London: Blackwell Sciences; 1999b. [Google Scholar]
- 2.Rovinsky JJ, Miller JA, Kaplan S. Management of breech presentation at term. Am J Obstet Gynecol. 1973;130:558–61. doi: 10.1016/0002-9378(73)90398-0. [DOI] [PubMed] [Google Scholar]
- 3.Gimovsky ML, Petrie LH. Neonatal performance of the selected term vaginal breech. Obstet Gynecol. 1980;142:643–48. [PubMed] [Google Scholar]
- 4.Gimovsky ML, Paul RH. Singleton breech presentation in labor: experience in 1980. Am J Obstet Gynecol. 1982 Aug 1;143(7):733–39. doi: 10.1016/0002-9378(82)90001-1. [DOI] [PubMed] [Google Scholar]
- 5.Wright RC. Reduction of perinatal mortality and morbidity in breech delivery through routine use of Caesarean section. Obstet Gynecol. 1959;14:748–52. [PubMed] [Google Scholar]
- 6.Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet. 2000 Oct 21;356(9239):1375–83. doi: 10.1016/s0140-6736(00)02840-3. [DOI] [PubMed] [Google Scholar]
- 7.Hofmeyr GJ, Hannah ME. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2003;(3):CD000166. doi: 10.1002/14651858.CD000166. [DOI] [PubMed] [Google Scholar]
- 8.Keirse Marc JNC. Evidence-Based Childbirth Only For Breech Babies? BIRTH. 2002 Mar 29;(1):55–59. doi: 10.1046/j.1523-536x.2002.00157.x. [DOI] [PubMed] [Google Scholar]
- 9.Hauth John C, Gary Cunningham F. Vaginal Breech Delivery Is Still Justified. Obstetrics & Gynecology. 2002 Jun;99(6):1115–16. doi: 10.1016/s0029-7844(02)02031-8. [DOI] [PubMed] [Google Scholar]
- 10.Kotaska Andrew. Inappropriate use of randomized trials to evaluate complex phenomena: case study of vaginal breech delivery. BMJ. 2004 Oct 30;329(7473):1039–42. doi: 10.1136/bmj.329.7473.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roosmalen J, Rosendaal F. There is stillroom for disagreement about vaginal delivery of breech infants at term. BJOG. 2002;109:967–69. [PubMed] [Google Scholar]
- 12.Roumen FJ, Nijhuis JG. Term breech presentation: an indication for Caesarean section. Ned Tijdschr Geneeskd. 2001 Aug 11;145(32):1533–36. [PubMed] [Google Scholar]
- 13.Somerset D. Managing term breech deliveries: Term breech trial does not provide unequivocal evidence. BMJ. 2002 Jan 5;324(7328):50–1. [PubMed] [Google Scholar]
- 14.Sanchez-Ramos L, Wells TL, Adair CD, Arcelin G, Kaunitz AM, Wells DS. Route of breech delivery and maternal and neonatal outcomes. Int J Gynaecol Obstet. 2001;73:7–14. doi: 10.1016/s0020-7292(00)00384-2. [DOI] [PubMed] [Google Scholar]
- 15.Schuitemaker N, Van Roosmalen J, Dekker G, van Don-gen P, van Geijn H, Gravenhorst JB. Maternal mortality after Caesarean section in the Netherlands. Acta Obstet Gynecol Scand. 1997;76:332–34. doi: 10.1111/j.1600-0412.1997.tb07987.x. [DOI] [PubMed] [Google Scholar]
- 16.Greene R, Gardeil F, Turner MJ. Long-term implications of cesarean section. Am J Obstet Gynecol. 1997;176:254–55. doi: 10.1016/s0002-9378(97)80046-4. [DOI] [PubMed] [Google Scholar]
- 17.Hemminiki E, Merilainen J. Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol. 1996;174:1569–74. doi: 10.1016/s0002-9378(96)70608-7. [DOI] [PubMed] [Google Scholar]
- 18.Shennan A, Bewley S. How to manage term breech deliveries. Avoid vaginal breech deliveries but offer external cephalic version. BMJ. 2001;323:244–45. doi: 10.1136/bmj.323.7307.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collea JV, Chein C, Quilligan EJ. A randomized management of term frank breech presentation: a study of 208 cases. Am J Obstet Gynecol. 1980;137:235–44. doi: 10.1016/0002-9378(80)90780-2. [DOI] [PubMed] [Google Scholar]
- 20.Daniel Y, Fait G, Lessing JB, Jaffa A, David MP, Kupferminc MJ. Outcome of 496 term singleton breech deliveries in a tertiary center. Am J Perinatol. 1998 Feb;15(2):97–101. doi: 10.1055/s-2007-993906. [DOI] [PubMed] [Google Scholar]
- 21.Tatum RK, Orr JW, Soong S, Huddleston JF. Vaginal breech delivery of selected infants weighing more than 2000 grams. A retrospective analysis of seven years’ experience. Am J Obstet Gynecol. 1985 May 15;152(2):145–55. doi: 10.1016/s0002-9378(85)80015-6. [DOI] [PubMed] [Google Scholar]
- 22.Giuliani A, Scholl WM, Basver A, Tamussino KF. Mode of delivery and outcome of 699 term singleton breech deliveries at a single center. Am J Obstet Gynecol. 2002 Dec;187(6):1694–98. doi: 10.1067/mob.2002.127902. [DOI] [PubMed] [Google Scholar]
- 23.Alarab M, Regan C, O’Connell MP, Keane DP, O’Herlihy C, Foley ME. Singleton vaginal breech delivery at term: still a safe option. Obstet Gynecol. 2004 Mar;103(3):407–12. doi: 10.1097/01.AOG.0000113625.29073.4c. [DOI] [PubMed] [Google Scholar]
- 24.1987. Annual report unit UKM Maternity Hospital Kuala Lumpur.
- 25.1988. Annual report unit UKM Maternity Hospital Kuala Lumpur.
- 26.1990. Annual report unit UKM Maternity Hospital Kuala Lumpur.
- 27.1999/2000. Annual report Maternity Hospital Kuala Lumpur.
- 28.2001. Annual report Maternity Hospital Kuala Lumpur.
- 29.Erkaya S, Tuncer RA, Kutlar I, Onat N, Ercakmak S. Outcome of 1040 consecutive breech deliveries: clinical experience of a maternity hospital in Turkey. Int J Gynaecol Obstet. 1997 Nov;59(2):115–18. doi: 10.1016/s0020-7292(97)00197-5. [DOI] [PubMed] [Google Scholar]
- 30.Fawole AO, Adeyemi AS, Adewole IF, Omigbodun AO. A ten-year review of breech deliveries at Ibadan. Afr J Med Med Sci. 2001 Mar-Jun;30(1–2):87–90. [PubMed] [Google Scholar]
- 31.Biswas A, Johnstone MJ. Term breech delivery: does X-ray pelvimetry help? Aust N Z J Obstet Gynaecol. 1993 May;33(2):150-3ELP. doi: 10.1111/j.1479-828x.1993.tb02380.x. [DOI] [PubMed] [Google Scholar]
- 32.Krebs L, Langhoff-Roos J. Breech delivery at term in Denmark, 1982–92: a population-based case-control study. Paediatr Perinat Epidemiol. 1999 Oct;13(4):431–41. doi: 10.1046/j.1365-3016.1999.00202.x. [DOI] [PubMed] [Google Scholar]
- 33.Lindqvist A, Norden-Lindeberg S, Hanson U. Perinatal mortality and route of delivery in term breech presentations. Br J Obstet Gynaecol. 1997 Nov;104(11):1288–91. doi: 10.1111/j.1471-0528.1997.tb10976.x. [DOI] [PubMed] [Google Scholar]
- 34.Hall JE, Kohl SC, O Brien R. Breech Presentation. A study of 1 456 cases. Am J Obstet Gynaecol. 1956;72:977–82. [PubMed] [Google Scholar]
- 35.Diugnan NM. Breech delivery. Has it a place in modern obstetrics. Matern Child Health J. 1980;5:482–84. [Google Scholar]
- 36.Kauppila O. Perinatal mortality in breech deliveries and observations on affecting factors. A retrospective study of 2227 cases. Acta Obstet Gynaecol Scand Suppl. 1975;39:1–79. [PubMed] [Google Scholar]
- 37.Crowley P, Hawkins DS. Premature breech delivery–the Caesarean section debate. J Obstet Gynaecol. 1980;1:2–6. [Google Scholar]
- 38.Wolf H, Schaap AH, Bruinse HW, Smolders-de Haas H, van Ertbruggen I, Treffers PE. Vaginal delivery compared with caesarean section in early preterm breech delivery: a comparison of long term outcome. Br J Obstet Gynaecol. 1999 May;106(5):486–91. doi: 10.1111/j.1471-0528.1999.tb08303.x. [DOI] [PubMed] [Google Scholar]
- 39.De Leeuw JP, De Haan J, Derom R, Thiery M, Martens G, van Maele Mortality and early neonatal morbidity in vaginal and abdominal deliveries in breech presentation. J Obstet Gynaecol. 2002 Mar;22(2):127–39. doi: 10.1080/0144361012023256. [DOI] [PubMed] [Google Scholar]
- 40.Lashen H, Fear K, Sturdee D. Trends in the management of the breech presentation at term; experience in a District General hospital over a 10-year period. Acta Obstet Gynecol Scand. 2002 Dec;81(12):1116–22. doi: 10.1034/j.1600-0412.2002.811204.x. [DOI] [PubMed] [Google Scholar]
- 41.Gimovsky ML, Wallace RL, Schifrin BS, Paul RH. Randomized management of the nonfrank breech presentation at term: a preliminary report. Am J Obstet Gynecol. 1983;146:34–40. doi: 10.1016/0002-9378(83)90923-7. [DOI] [PubMed] [Google Scholar]
- 42.Su M, McLeod L, Ross S, et al. Term Breech Trial Collaborative Group. Factors associated with adverse perinatal outcome in the Term Breech Trial. Am J Obstet Gynecol. 2003 Sep;189(3):740–45. doi: 10.1067/s0002-9378(03)00822-6. [DOI] [PubMed] [Google Scholar]
- 43.Young PF, Johanson RB. The management of breech presentation at term. Curr Opin Obstet Gynecol. 2001 Dec;13(6):589–93. doi: 10.1097/00001703-200112000-00007. [DOI] [PubMed] [Google Scholar]