Abstract
Sebaceous cell carcinoma of the skin is a rare malignancy of the skin appendages. Most commonly noticed in the orbital region. Extra orbital sebaceous cell carcinoma is extremely rare. The aggressive behavior of this tumor is still a matter of controversy. We present a case of sebaceous cell carcinoma in scalp region in young women.
Keywords: sebaceous cell carcinoma, orbital, extra orbital, scalp, metastasis
Introduction
Sebaceous cell carcinoma (SC) is a rare malignancy of the skin appendages. SC is most commonly seen in the orbital region, extra orbital SC is very rare. So far only 150 cases of extra orbital SC were reported in the literature(1–2). The extra orbital SC commonly occurs on head and scalp due to the abundant sebaceous glands (3–4) the other sites involved by SC are external genetalia (5) extremities (6). The true SC is still a subject of discussion both from histopathological and clinical point of view due to its rarity and behavior pattern (7).The present literature is dividing in deciding the aggressive nature of extra ocular SC, Rulon and Helwig (8) noted no metastasis in their analysis of five cases. However the incidence of metastasis is less than 10% in extra orbital SC (9).
Sebaceous cell carcinoma is a disease of 6th and 7th decade of life occurs in men and women equally (3).The incidence varies from 0.2% to 4.6% of all skin cancers, the incidence is about 0.6% in people below 20 years of age (10). We present an extra orbital SC in young female with extensive lymph nodal, bone and lung metastasis.
Case Report
A 29 year old female mother of two children was referred to the oncology clinic of Hospital Universiti Sains Malaysia (HUSM) for further treatment from the general Hospital complaining of severe neck pain, head ache, awareness of nodule over the scalp. The neck pain was severe in nature with a history of restricted neck movement. The head ache was of one year duration associated with vomiting. The scalp nodule had been present at the same site 3 years earlier. A wide excision was done at a local hospital then and the histopathology reported the tumor as having a limited contact with the epidermis and extended into the dermis in columns. The architecture of the tumor was somewhat lobular. A few lumina resembling sebaceous ducts were present within the tumor. The tumor cells were cytologically malignant and there was variation in the diameter of the vacuoles within a given cell. This was reported as sebaceous cell carcinoma (Figure 1). The patient was asymptomatic for one year following the surgery but subsequently developed a recurrent nodule at the same site along with headache, not responding to analgesics.
Figure 1 :
Vacuolated tumor cells with pleomorphic nuclei. Necrosis is also present Hand E stain x 20
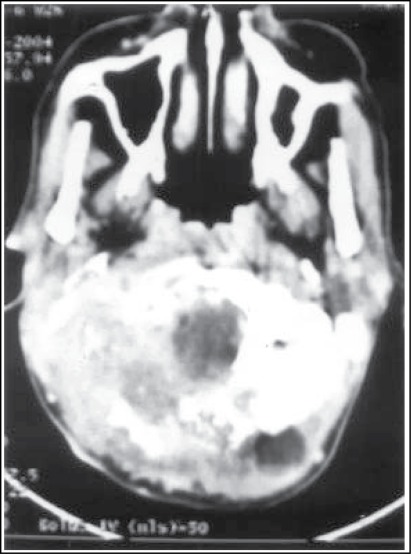
She was admitted to the General Hospital, Kota Bharu in Sept 2004 and underwent a CT scan of the brain and head and neck region. Tumor recurrence was seen in the occipital region with destruction of bone and local infiltration into the meninges (Figure 2).The patient was referred to the HUSM for further management. At examination although alert she was experiencing cervical neck pain. Proptosis of the right eye was noted. A nonhealing ulcer in the occipital region of the scalp was also seen. A detailed examination of the eyes and the CNS at presentation was not done due to poor cooperation from the patient. However she had a sixth and seventh nerve palsies on the right side. Multiple lymph node enlargement was noted in the cervical and supra clavicular regions. Fine needle aspiration cytology of the lymph node revealed a poorly differentiated carcinoma. A single fraction of 800 cGy external radiation was given to the thoracic spine for pain relief.
Figure 2 :
CT Scan picture showing destruction of occipital bone and local infiltration.
The patient was reviewed a month later in the oncology clinic. She had significant pain relief from the radiation treatment. She was started on oral morphine for better pain control. Single agent chemotherapy with mitomycin-C was proposed she declined. A CT scan of the abdomen was planned to evaluate abdominal involvement or liver metastasis. A colonoscopy was deferred in view of her poor general condition. She succumbed to the disease three months after the presentation.
Discussion
Extra orbital sebaceous cell carcinoma (SC) has a different behaviour compared to the orbital SC which is considered less aggressive than orbital SC (11). The clinical behavior and characteristics are still a mater of controversy in the literature (7). Mellette et al for instance found that the biological behavior of extra orbital SC is not different from the orbital SC (12). The other sites reported in the literature are the parotid and the submandibular glands, buccal mucosa, laryngeal and pharyngeal cavities, the trunk and the upper extremities and the external genitalia.
The histological criteria for SC are high mitotic activity, nuclear pleomorphism, lobular architecture and foamy vacuolization of the cytoplasm (9). Histologically SC divided into three types sebaceous adenoma, basal cell carcinoma with sebaceous differentiation and sebaceous carcinoma (13). The present literature is divided on the aggressive nature and metastasis potential of extra ocular SC (5,8,14). Extra ocular SC is known to recur locally and spread to lymph nodes and visceral organs (15). Histologically the poor prognostic indicators are poor differentiation, presence of lymphatic or vascular permeation, presence of Pagetoid cells shown in histology and immuno histochemical staining (16, 17).
The biological behavior of SC is still open for discussion as there are varied opinions about the incidence of local and distant failure in patients with extra orbital SC (18). Due to its rarity with only about 150 cases reported in the literature so far there is no single opinion on the aggressive nature of the disease. However the series by Wick, King and Hernandaz showed the distant metastasis occurred inpatients with extra orbital SC. The present case is different from that in the literature in that this malignancy occurred in the 3rd decade of life. The patient had recurrence of disease at the primary site one year after the initial surgery and very locally aggressive with bone, meningeal and regional lymph nodes infiltration. The lungs and vertebral columns were also involved with metastasis.
The role of adjuvant treatment with radiation and chemotherapy after surgery is not clear in the extra ocular SC due to its rare presentation. We treated the patient with external radiation with a palliative intent and advised chemotherapy as the patient was young.
We conclude that the extra ocular SC is an aggressive skin malignancy and needs to be radically treated by surgery followed by additional treatment depending on the prognostic features as discussed above. Patients with extra orbital SC have to be followed up closely for assessment of recurrence and distant metastasis.
References
- 1.Akhtar S, Oza KK, Roulier RG. Multiple sebaceous adenomas and extraocular sebaceous carcinoma in a patient with multiple sclerosis: case report and review of literature. J Cutan Med Surg. 2001 Nov-Dec;5(6):490–5. doi: 10.1007/s10227-001-0011-3. [DOI] [PubMed] [Google Scholar]
- 2.Duman DG, Ceyhan BB, Celikel T, et al. Extraorbital sebaceous carcinoma with rapidly developing visceral metastasis. Dermatol Surg. 2003 Sep;29(9):987–9. doi: 10.1046/j.1524-4725.2003.29268.x. [DOI] [PubMed] [Google Scholar]
- 3.Pickford MA, Hogg FJ, Fallowfield ME, et al. Sebaceous carcinoma of the periorbital and extraorbital regions. Br J Plast Surg. 1995 Mar;48(2):93–6. doi: 10.1016/0007-1226(95)90103-5. [DOI] [PubMed] [Google Scholar]
- 4.Moreno C, Jacyk Wk, Judd MJ, Requena L. Highly aggressive extraocular sebaceous carcinoma. Am J Dermatopathol. 2001 Oct;23(5):450–5. doi: 10.1097/00000372-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Wick MR, Goellner JR, Wolfe JT, 3rd, et al. Adenexal carcinoma of the skin.II. Extraocular sebaceous carcinomas. Cancer. 1985 Sep;56(5):1163–72. doi: 10.1002/1097-0142(19850901)56:5<1163::aid-cncr2820560533>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 6.Pricolo VE, Rodil JV, Vezeridis MP. Extraorbital sebaceous carcinoma. Arch Surg. Jul;120(7):853–5. doi: 10.1001/archsurg.1985.01390310085019. [DOI] [PubMed] [Google Scholar]
- 7.Bassetto F, Baraziol R, Sottosanti MV, et al. Bilogical behaviour of the sebaceous carcinoma of the head. Dermatol Surg. 2004 Mar;30(3):472–6. doi: 10.1111/j.1524-4725.2004.30025.x. [DOI] [PubMed] [Google Scholar]
- 8.Rulon DB, Helwig EB. Cutaneous sebaceous neoplasms. Cancer. 1974 Jan;33(1):82–102. doi: 10.1002/1097-0142(197401)33:1<82::aid-cncr2820330115>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 9.Bailet JW, Zimmerman MC, Arnstein DP, et al. Sebaceous Carcinoma of the head and neck. Case report and literature review. Arch Otolaryngol Head Neck Surg. 1992 Nov;118(11):1245–9. doi: 10.1001/archotol.1992.01880110113020. [DOI] [PubMed] [Google Scholar]
- 10.Margo CE, Mulla ZD. Malignant tumors of the eyelid: a population-based study of non-basal cell and nonsquamous cell malignant neoplasms. Arch Ophthalmol. 1998 Feb;116(2):195–8. doi: 10.1001/archopht.116.2.195. [DOI] [PubMed] [Google Scholar]
- 11.Rao NA, Hidayat AA, McLean IW, et al. Sebaceous carcinoma of the ocular adnexa: A clinicopathologic study of 104 cases, with five-year follow-up data. Hum Pathol. 1982 Feb;13(2):113–22. doi: 10.1016/s0046-8177(82)80115-9. [DOI] [PubMed] [Google Scholar]
- 12.Mellette JR, Amonette RA, Gardner JH, Chesney TM. Carcinoma of sebaceous glands on the head and neck. A report of four cases. J Dermatol Surg Oncol. 1981 May;7(5):404–7. doi: 10.1111/j.1524-4725.1981.tb00665.x. [DOI] [PubMed] [Google Scholar]
- 13.Misago N, Mihara I, Ansai S, et al. Sebaceoma and related neoplasms with sebaceous differentiation: a clinicopathologic study of 30 cases. Am J Dermatopathol. 2002 Aug;24(4):294–304. doi: 10.1097/00000372-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 14.King DT, Hirose FM, Gurevitch AW. Sebaceous carcinoma of the skin with visceral metastasis. Arch Dermatol. 1979 Jul;115(7):862–3. [PubMed] [Google Scholar]
- 15.Verlooy H, Mortelmans L, Schiepers C, et al. A rare case of sebaceous carcinoma with very malignant characteristics. Clin Nucl Med. 1993 May;18(5):425–7. doi: 10.1097/00003072-199305000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Hasebe T, Mukai K, Yamaguchi N, et al. Prognostic value of immunohistochemical staining for proliferating cell nuclear antigen, p53 and c-erbB-2 in sebaceous gland carcinoma and sweat gland carcinoma: comparision with histopathological parameter. Mod Pathol. 1994 Jan;7(1):37–43. [PubMed] [Google Scholar]
- 17.Valenzuela-Flores G, Mozas-Davila D, Rodriguez-Reyes AA, et al. Sebaceous gland carcinoma of eye lids. Cir Cir. 2004 Jan-Feb;72(1):47–53. [PubMed] [Google Scholar]
- 18.O’Neal ML, Brunson A, Spadafora J. Ocular sebaceous carcinoma: case report and review of the literature. Compr Ther. 2001 summer;27(2):144–7. doi: 10.1007/s12019-996-0009-2. [DOI] [PubMed] [Google Scholar]