Abstract
Objectives
To compare the efficacy of acupuncture and conventional massage for the treatment of chronic neck pain.
Design
Prospective, randomised, placebo controlled trial.
Setting
Three outpatient departments in Germany.
Participants
177 patients aged 18-85 years with chronic neck pain.
Interventions
Patients were randomly allocated to five treatments over three weeks with acupuncture (56), massage (60), or “sham” laser acupuncture (61).
Main outcome measures
Primary outcome measure: maximum pain related to motion (visual analogue scale) irrespective of direction of movement one week after treatment. Secondary outcome measures: range of motion (3D ultrasound real time motion analyser), pain related to movement in six directions (visual analogue scale), pressure pain threshold (pressure algometer), changes of spontaneous pain, motion related pain, global complaints (seven point scale), and quality of life (SF-36). Assessments were performed before, during, and one week and three months after treatment. Patients' beliefs in treatment were assessed.
Results
One week after five treatments the acupuncture group showed a significantly greater improvement in motion related pain compared with massage (difference 24.22 (95% confidence interval 16.5 to 31.9), P=0.0052) but not compared with sham laser (17.28 (10.0 to 24.6), P=0.327). Differences between acupuncture and massage or sham laser were greater in the subgroup who had had pain for longer than five years (n=75) and in patients with myofascial pain syndrome (n=129). The acupuncture group had the best results in most secondary outcome measures. There were no differences in patients' beliefs in treatment.
Conclusions
Acupuncture is an effective short term treatment for patients with chronic neck pain, but there is only limited evidence for long term effects after five treatments.
What is already known on this topic
Acupuncture is a widespread complementary treatment
Evidence from trials have given conflicting results on its use in the treatment of neck pain because of methodological shortcomings and because effects were compared either with alternative treatments or with different sham procedures imitating acupuncture, but not both
What this study adds
Compared with sham laser acupuncture and massage, needle acupuncture has beneficial effects on mobility and pain related to motion in patients with chronic neck pain
Acupuncture was clearly more effective than massage, but differences were not always significant compared with sham laser acupuncture
Acupuncture was the best treatment for patients with the myofascial syndrome and those who had had pain for longer than five years
Introduction
Neck pain is a common complaint with a point prevalence from 10% to 18% and lifetime prevalence from 30% to 50%. In many cases symptoms persist, causing severe discomfort and inability to work.1,2 Neck pain is associated with limited cervical spine mobility.3 Frequent concomitant symptoms are headache, vertigo, visual disorders, tinnitus, and vegetative symptoms (sweating, dizziness, nausea).4,5 Common treatment consists of drugs, massage and other manual treatments, physiotherapy and exercise, local and epidural injections, and patient education.6,7 Systematic reviews have shown that the efficacy of these interventions remains questionable.7,8 Current treatment increasingly includes complementary methods, of which acupuncture is one of the most common.9 There is, however, a lack of evidence to support acupuncture as an effective treatment for chronic neck pain.10–12
We compared the efficacy of acupuncture with conventional massage and “sham” laser acupuncture for the treatment of neck pain.
Methods
Study design
The study was a randomised, placebo and alternative treatment controlled clinical trial performed at three outpatient departments at the universities in Munich and Würzburg, Germany, from 1996 to 1999.
Participants
Patients were consecutively preselected by the doctors of the three outpatient departments, who were informed about the inclusion and exclusion criteria. Patients who were eligible and willing to participate in the study were then assessed by an independent examiner. This assessment included a detailed physical examination and collection of baseline data. The main inclusion criteria were that patients had had a painful restriction of cervical spine mobility for longer than one month and that they had not received any treatment in the two weeks before entering the study. Patients who had undergone surgery or those with dislocation, fracture, neurological deficits, systemic disorders, or contraindications to treatment were excluded.
Neck pain was classified according to the system of Schöps and Senn on the basis of history, characteristics of pain, manual examination, and radiological findings.13 Patients' conditions were defined as the myofascial pain syndrome (pain and limited mobility associated with myofascial triggerpoints),14 the irritation syndrome (diffuse, intense pain with difficult access for manual examination), or segmental dysfunction (segmental hypomobility revealed by manual examination and functional radiograph analysis). The diagnosis was confirmed by a second assessor. Informed consent was obtained, and the study was approved by the local ethics committees.
Randomisation
Participants were randomly allocated to acupuncture or massage or sham laser acupuncture. A block randomisation stratified for two centres was performed by using a validated software program (PC Random, Biometric Center for Therapeutic Studies, Munich). Patients were told before randomisation that one of the three treatments might be a sham procedure.
Treatment protocols
Patients were treated five times over three weeks. Each treatment lasted 30 minutes. Acupuncture and sham laser acupuncture were performed by four experienced, licensed medical acupuncturists. Massages were performed by five experienced physiotherapists. Patients took no concomitant analgesics. Patients who rated their pain as over 20 on the visual analogue scale (0-100) or who had an inconvenient restriction of mobility at the primary study end point were referred for physiotherapy during follow up.
Acupuncture—Acupuncture was performed according to the rules of traditional Chinese medicine, including diagnostic palpation to identify sensitive spots.15 Remote and local acupuncture points were selected individually on the affected meridians. Relevant ear acupuncture points were included. In addition local myofascial triggerpoints were treated with the technique of dry needling to elicit a local twitch response of muscles.14,16 Criteria for point selection are described in detail.15–17 The most commonly used points were SI3, UB10, UB60, Liv3, GB20, GB34, TE5, and the ear point “cervical spine.” Active myofascial triggerpoints were located predominantly in the musculus trapezius (nearby GB20) and levator scapulae (nearby SI14).
Massage—Patients were treated with conventional Western massage. Techniques included effleurage, petrissage, friction, tapotement, and vibration.18 Mode and intensity were chosen by the physiotherapist in accordance with the patient's condition and diagnosis as usual in clinical routine. Spinal manipulation and non-conventional techniques were not performed.
Placebo—Sham laser acupuncture was performed with a laser pen, which was inactivated by the manufacturer (Laser Pen, Seirin International, Fort Lauderdale). Only red light was emitted. Patients were not informed about the inactivation of the laser pen. To strengthen the power of this sham procedure, visual and acoustic signals common for this type of laser pen accompanied the red light emission. Criteria for selection of points were identical with those used in the acupuncture group, including palpation of acupuncture points for diagnostic reasons. Every point was treated for 2 minutes, with the pen at a distance of 0.5-1 cm from the skin.
Assessments
Assessments were performed by a blinded observer before the intervention (M1), immediately after (M2) and three days after (M3) the first treatment, and immediately after (M4) and one week after (M5, primary end point) the last treatment. Follow up included an assessment at three months (M6, secondary end point). Patients were requested not to reveal any information about their treatment during assessment.
To evaluate the adequacy of control treatments we assessed patients' beliefs about the treatment.19 After randomisation and before the first treatment they had to answer four questions on a 100 point visual analogue scale: How confident do you feel that this treatment can alleviate your complaint? How confident would you be in recommending this treatment to a friend who suffered from similar complaints? How logical does this treatment seem to you? How successful do you think this treatment would be in alleviating other complaints?
Outcome measures
Primary outcome measure
—The primary outcome measure was the change in the maximum pain related to motion, irrespective of the direction of movement, evaluated before (M1) and one week after (M5) intervention. Patients were asked to move their head in the most affected direction and to score the intensity of pain on a 100 point visual analogue scale.
Secondary outcome measures—We measured the active range of motion with a 3D ultrasound real time motion analyser (Zebris Medizintechnik, Tübingen, Germany). It is a valid and reliable method to assess cervical mobility.20 We measured the range of six cervical spine movements (flexion, extension, rotation right/left, lateral flexion right/left). In addition, patients used a visual analogue scale to score the intensity of direction related pain for each of the six directions. We quantified the pressure pain threshold bilaterally at three anatomically defined sites (levator scapulae, trapezius descendens, paravertebral of the 6th cervical spine) and the individual maximum point using a digital pressure algometer.21 Two readings on each site were performed. We recorded changes of spontaneous pain, motion related pain, and global complaints on a seven point scale one week and three months after treatment. Patients were asked: “Did the severity of your spontaneous pain (motion related pain, global complaints) change after treatment?” If they answered yes, they were asked if the pain had improved or worsened and whether the change was slight, marked, or extreme. To assess quality of life the patients completed the SF-36 health survey.22
Statistical analyses
Our intention was to analyse 52 patients per group, which, given a standard deviation of 18, would have provided 80% power at the 5% significance level to detect a 10 point difference in the mean change of motion related pain. This calculation was based on a pilot study that compared acupuncture with sham laser on immediate changes of motion related pain after a single treatment. We estimated a drop out rate of 20% and therefore aimed to recruit 200 patients. However, the study was terminated after we recruited 177 patients because the study period was over and the drop out rate was mostly below 20%, leading to a sufficient number of eligible patients for analyses.
Statistical analyses of all study variables were based on intention to treat analysis. For analyses of range of motion and direction related pain we calculated mean values on the basis of the data for six movement directions (score). We used parametric variance to test quantitative variables for comparisons of mean differences, which were approximately normally distributed, followed by pairwise comparisons. For the main outcome measure and quantitative parameters we adjusted for multiple comparisons to keep the significance level to 0.05. We tested hypotheses on qualitative data with χ2 tests or Fisher's exact test. All calculations were carried out with the SAS software package, version 6.12.
Results
Randomisation and progress through the trial
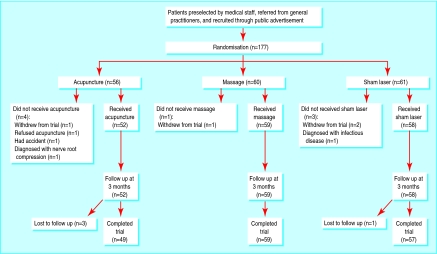
Of 182 patients referred for the first assessment, five did not meet entry criteria; 177 patients were included in the trial. Baseline characteristics of the study sample were equally balanced between groups for most variables, but there was some difference with regard to myofascial pain (table 1). In all three groups most patients believed in the potential benefit of the treatments. The figure shows the progress of patients through the trial and withdrawal from study.
Table 1.
Characteristics of 177 patients with chronic neck pain included in trial
| Acupuncture (n=56) | Massage (n=60) | Sham laser (n=61) | |
|---|---|---|---|
| Mean (SD) age (years) | 52.3 (13.3) | 52.7 (11.5) | 52.2 (13.2) |
| Women | 39 | 38 | 40 |
| Whiplash | 17 | 16 | 23 |
| Myofascial pain syndrome | 35 | 45 | 49 |
| Duration of pain >5 years | 23 | 24 | 28 |
| Slow onset | 36 | 47 | 45 |
| Concomitant symptoms*: | |||
| None | 9 | 13 | 10 |
| 1-3 | 26 | 24 | 23 |
| >3 | 20 | 22 | 26 |
| History of treatment: | 56 | 60 | 61 |
| Massage | 45 | 44 | 47 |
| Fango (warm pack) | 44 | 44 | 35 |
| Physiotherapy | 40 | 40 | 39 |
| Chiropractic | 25 | 32 | 30 |
| Infiltration with local anaesthetics | 18 | 25 | 23 |
| Relaxation methods | 18 | 23 | 19 |
| Acupuncture | 14 | 23 | 21 |
| Psychological pain therapy | 5 | 5 | 6 |
Headache, low back pain, vertigo, tinnitus, fatigue, sensitivity to noise and light, lack of motivation, nausea, unspecific visual disorders.
Main outcome measure
The results of the baseline measurements are shown in table 2. The mean improvement one week after intervention is shown in table 3. The reduction in pain related to motion was significantly greater in the acupuncture group compared with the massage group (P=0.0052) but not compared with sham laser (P=0.327). Differences between acupuncture and massage or sham laser were more distinct in the subgroup who had had pain for longer than five years and in patients with the myofascial pain syndrome (table 3).
Table 2.
Baseline measurement (M1) of primary and secondary outcome measures. Data are expressed as mean (SD) values
| Outcome measures | Acupuncture (n=56) | Massage (n=60) | Sham laser (n=61) |
|---|---|---|---|
| Pain related to motion (VAS) | 54.15 (21.91) | 54.71 (23.46) | 57.15 (26.71) |
| Range of motion (degrees)* | 277.9 (52.5) | 287.8 (50.3) | 286.5 (49.2) |
| Pain related to direction (VAS)† | 33.87 (16.06) | 34.88 (19.55) | 35.82 (21.10) |
| Pressure pain threshold (kg/cm2)‡ | 1.07 (0.57) | 1.07 (0.58) | 1.05 (0.57) |
| Health related quality of life (SF-36)§: | |||
| Role physical | 46.50 (41.65) | 41.82 (36.61) | 39.04 (42.26) |
| Pain index | 38.82 (17.38) | 36.70 (17.06) | 39.21 (17.21) |
VAS=visual analogue scale.
For analyses of range of motion, data of six movement directions were added for each patient.
Range 0-100. Scores for six movement directions averaged for each patient (score also includes less painful movement directions).
Measurements on individual maximum point. Results for three other sites were similar.
Only two of eight scales showed limitations. Range of scores is 0-100; 0 indicates maximum limitation.
Table 3.
Primary outcome measure: improvement of pain related to motion one week after treatment compared with baseline measurements. Group comparison and subgroup analyses
| Mean improvement on VAS (95% CI) | P value for comparison* | |
|---|---|---|
| All participants | ||
| Acupuncture (n=51) | 24.22 (16.5 to 31.9) | — |
| Massage (n=57) | 7.89 (0.6 to 15.2) | — |
| Sham acupuncture (n=57) | 17.28 (10.0 to 24.6) | — |
| Acupuncture v massage | 16.32 (4.4 to 28.3) | 0.0052 |
| Acupuncture v sham laser | 6.93 (−5.0 to 18.9) | 0.327 |
| Patients with the myofascial pain syndrome | ||
| Acupuncture (n=34) | 30.05 (20.4 to 39.7) | — |
| Massage (n=43) | 7.23 (−1.3 to 15.8) | — |
| Sham acupuncture (n=45) | 19.02 (10.8 to 28.2) | — |
| Acupuncture v massage | 22.8 (8.3 to 37.3) | 0.0012 |
| Acupuncture v sham laser | 11.0 (−3.2 to 25.2) | 0.1480 |
| Patients with pain >5 years | ||
| Acupuncture (n=23) | 31.87 (21.9 to 41.8) | — |
| Massage (n=23) | 13.52 (3.6 to 23.5) | — |
| Sham acupuncture (n=27) | 17.15 (7.9 to 26.3) | — |
| Acupuncture v massage | 18.35 (2.4 to 34.3) | 0.0216 |
| Acupuncture v sham laser | 14.7 (0.6 to 30.6) | 0.0617 |
VAS=visual analogue scale. *Dunnetts's test.
Pain related to motion improved by more than 50% compared with baseline in 29/51 (57%) patients who received acupuncture compared with 18/57 (32%) patients who received sham laser and 14/57 (25%) patients who received massage (χ2 test P=0.008).
Secondary outcome measures
Table 4 shows mean changes in secondary outcome measures and comparisons between treatment groups. The results for secondary outcome measures were similar to those for the primary outcome measure. The acupuncture group achieved the best results in most of the secondary outcome measures, including significant differences compared with massage in pain related to motion and direction immediately and one week after treatment. Three months after treatment these differences were comparatively small and no longer significant. However, significantly more patients in the acupuncture group considered their pain (spontaneous, motion related) and global complaints improved three months after treatment compared with patients in the massage group (χ2 tests). We found no significant differences between groups in pressure pain threshold.
Table 4.
Secondary outcome measures. Improvement in 165 patients with chronic neck pain immediately after (M2) and three days after (M3) first treatment, immediately after (M4) and one week after (M5, primary end point) last treatment, and at three month follow up (M6) compared with baseline measurements and comparison between groups by treatment. Figures are means (SD) unless indicated otherwise
| Acupuncture | Massage | Sham laser | Difference between groups*
|
||
|---|---|---|---|---|---|
| Acupuncture v massage | Acupuncture v sham laser | ||||
| Pain related to motion (improvement on VAS 0-100) | |||||
| M2 | 7.8 (21.1) | 7.2 (21.5) | 7.3 (21.2) | 0.981 | 0.984 |
| M3 | 12.7 (22.2) | 5.4 (24.7) | 11.4 (21.4) | 0.168 | 0.937 |
| M4 | 25.3 (22.6) | 12.7 (29.5) | 19.2 (26.5) | 0.027 | 0.388 |
| M6 | 17.4 (29.7) | 14.4 (31.9) | 17.4 (26.4) | 0.823 | 1.000 |
| Range of motion (degrees)† | |||||
| M4 | 19.6 (36.3) | 6.2 (25.3) | 12.9 (25.1) | 0.034 | 0.384 |
| M5 | 19.8 (37.9) | 5.1 (22.2) | 8.7 (33.0) | 0.031 | 0.125 |
| M6 | 8.9 (30.1) | 5.5 (37.2) | 3.5 (29.8) | 0.815 | 0.609 |
| Pain related to direction (improvement on VAS 0-100)‡ | |||||
| M4 | 16.9 (15.6) | 5.6 (15.3) | 10.2 (18.5) | 0.001 | 0.066 |
| M5 | 17.3 (18.0) | 3.1 (15.0) | 11.4 (18.7) | 0.0001 | 0.138 |
| M6 | 15.0 (14.3) | 8.1 (21.8) | 11.2 (19.3) | 0.113 | 0.486 |
| Pressure pain threshold (kg/cm2)§ | |||||
| M4 | 0.06 (0.58) | 0.04 (0.50) | −0.03 (0.51) | 0.971 | 0.558 |
| M5 | −0.02 (0.54) | −0.09 (0.62) | −0.07 (0.52) | 0.696 | 0.864 |
| M6 | 0.19 (0.77) | 0.05 (0.59) | 0.03 (0.62) | 0.447 | 0.368 |
| Spontaneous pain (rating scale)¶ | |||||
| M5 | 35/51 (69%) | 28/56 (50%) | 30/56 (54%) | 0.150 | 0.242 |
| M6 | 33/47 (70%) | 25/57 (44%) | 28/56 (50%) | 0.015 | 0.056 |
| Pain related to motion (rating scale)¶ | |||||
| M5 | 44/52 (85%) | 33/58 (57%) | 34/57 (60%) | 0.002 | 0.012 |
| M6 | 38/48 (79%) | 29/57 (51%) | 34/57 (60%) | 0.007 | 0.089 |
| Global complaints (rating scale)¶ | |||||
| M5 | 46/52 (88%) | 32/58 (55%) | 39/57 (68%) | 0.001 | 0.040 |
| M6 | 39/48 (81%) | 32/57 (56%) | 38/57 (67%) | 0.022 | 0.225 |
| Role physical** | |||||
| M5 | 8.06 (31.9) | 12.37 (34.4) | 0.00 (23.6) | 0.797 | 0.498 |
| M6 | 0.83 (41.3) | 4.95 (37.3) | 5.83 (34.5) | 0.865 | 0.825 |
| Pain index** | |||||
| M5 | 8.41 (20.2) | 10.15 (17.3) | 8.85 (16.9) | 0.843 | 0.989 |
| M6 | 13.76 (22.4) | 14.64 (22.1) | 15.67 (21.5) | 0.971 | 0.870 |
VAS=visual analogue scale.
P values. Parametric variance analytic models used for comparison of improvements of all quantitative variables with adjustment according to Dunnett. For comparison of qualitative variables (rating scale) χ2 tests were used without adjustment for multiple comparisons. Repeated measurements at different time points were performed without further adjustment.
Data from six movement directions added for each patient. To analyse changes of range, differences calculated by subtracting results for each patient after treatment from those before treatment.
Ratings of six movement directions averaged for each patient; less painful movement directions included in score. To analyse changes of direction related pain, differences were calculated by subtracting results for each patient after treatment from those before treatment.
Measurements on individual maximum point. Results for three other sites were similar.
No of patients improved v treated (percentage); 7 point rating scale reduced to 3 point scale (improvement, no change, worsening).
Only two of eight scales showed limitations in SF-36 before treatment.
Baseline evaluation of quality of life related to health showed limitations in only two of eight scales (role physical, pain index). After treatment these two scales were improved in all groups, without significant differences between groups. A total of 119 patients (67%) were referred to physiotherapy during follow up. There were no differences between groups.
Side effects
Seventeen (33%) participants reported mild reactions after needle insertion during acupuncture, mainly slight pain or vegetative reactions (sweating, low blood pressure). After a short rest they agreed to continue the treatment. Similar mild reactions were seen in four (7%) in the massage group and 12 (21%) in the sham laser group. No serious adverse reactions were observed.
Discussion
Our results show that acupuncture is a safe form of treatment for people with chronic neck pain and offers clear clinical advantages over conventional massage in the reduction of pain and improvement of mobility. Acupuncture was most effective in people who had had pain for over five years and in those with the myofascial pain syndrome. Such patients can be identified from their case histories and a detailed physical examination.
Our study population generally had “non-specific neck pain,” which includes most patients suffering from chronic neck pain.23,24 Between 55% and 90% of patients with chronic neck pain have the myofascial pain syndrome4,14 and 20% to 50% have suffered a whiplash injury.5 There were no significant differences between groups in the primary outcome measure (pain related to motion) and most of the secondary outcome measures three months after treatment. This is consistent with the results of recent systematic reviews that show that a single treatment approach in chronic pain does not result in long term effects.7,8 However, results of the qualitative verbal rating scales, which express a more subjective change of pain and global complaints, might indicate longer lasting benefits of acupuncture. Conventional massage had only a weak effect on chronic neck pain. This is in agreement with recent reviews indicating a lack of evidence for the efficacy of massage, although it is one of the most common forms of treatment.2,18
Previous trials of acupuncture for neck pain have had contradictory results. In a systematic review of 14 acupuncture trials, White and Ernst found no evidence for efficacy, with outcomes equally balanced between positive and negative.10 The authors judged methodological quality of the studies as disappointing. In a more recent review, Smith et al assessed the analgesic efficacy of acupuncture for neck and back pain. Using a newly developed tool to measure validity of findings of randomised clinical trials, they found no convincing evidence for the analgesic efficacy of acupuncture, and, again, the quality of most trials was poor.12 In contrast with previous studies our trial had a large sample size, adequate measures evaluated by blinded observers, blinded patients for placebo control, individual acupuncture treatment by more than one licensed acupuncturist, data analyses by an independent institution, follow up assessments, and documentation of drop outs and adverse events.
We chose sham laser acupuncture because it does not activate somatosensory receptors and laser acupuncture is a well known method. We were surprised by the results of sham laser acupuncture compared with massage. They could be explained by an enhanced placebo effect, but the assessment of credibility showed no differences between therapies before treatment. Sham laser acupuncture, however, does not really resemble needle acupuncture. Consequently, non-specific acupuncture effects can only be estimated. Also, sham laser was probably not an inert control because participants might have benefited from palpation of acupuncture points, performed before treatment to select acupuncture points.
Participants received only five treatments because we did not want to treat patients with chronic pain with placebo for longer for ethical reasons. According to traditional Chinese medicine about 10 sessions would be more appropriate.15 Future research is necessary to evaluate the optimum number of treatments.
It has become clear from our results that placebo controlled studies should include a third group with alternative treatment or without treatment for improved classification of the effects of acupuncture because a true placebo procedure, including blinding of acupuncturists, does not exist for needle acupuncture studies.11,25 The results do not elicit the specificity of acupuncture points or physiological mechanisms.
Conclusion
We conclude that acupuncture can be a safe form of treatment for patients with chronic neck pain if the objective is to obtain relief from pain related to motion and to improve cervical mobility. As neck pain may be a chronic condition with considerable socioeconomic impact single forms of treatment may be inadequate, and acupuncture merits consideration.
Figure.
Participants' progress through trial and withdrawals
Acknowledgments
We thank K Gleditsch, Dr R Pfeiffer, Dr M Haase, H Arndt, C Müller, D Drexler, and P Köllges for their work in data collection, and all participating colleagues and physiotherapists in the department of physical medicine and rehabilitation, University of Munich, the pain unit, University of Munich, and the department of orthopaedics, University of Würzburg. We also thank the patients who made the project possible.
Footnotes
Funding: German Ministry for Education and Research (BMBF, formerly BMFT) (Project 01 KT 9406/1). Preparation of the manuscript was supported by the German Medical Acupuncture Association (DÄGfA).
Competing interests: None declared.
References
- 1.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine. 1994;19:1307–1309. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Andersson GBJ. The epidemiology of spinal disorders. In: Frymoyer JW, editor. The adult spine: principles and practice. Philadelphia, PA: Lippincott-Raven; 1997. pp. 130–141. [Google Scholar]
- 3.Hagen KB, Harms-Ringdahl K, Enger NO, Hedenstad R, Morten H. Relationship between subjective neck disorders and cervical spine mobility and motion-related pain in male machine operators. Spine. 1997;22:1501–1507. doi: 10.1097/00007632-199707010-00015. [DOI] [PubMed] [Google Scholar]
- 4.Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985;60:615–623. doi: 10.1016/0030-4220(85)90364-0. [DOI] [PubMed] [Google Scholar]
- 5.Stovner LJ. The nosological status of the whiplash syndrome: a critical review based on a methodological approach. Spine. 1996;23:2735–2746. doi: 10.1097/00007632-199612010-00006. [DOI] [PubMed] [Google Scholar]
- 6.Bland J, editor. Disorders of the cervical spine. Philadelphia, PA: WB Saunders; 1987. [Google Scholar]
- 7.Aker PD, Gross RA, Goldsmith CH, Peloso P. Conservative management of mechanical neck pain: a systematic overview and meta-analysis. BMJ. 1996;313:1291–1296. [PMC free article] [PubMed] [Google Scholar]
- 8.Gross AR, Aker PD, Goldsmith CH, Peloso P. Physical medicine modalities of mechanical neck disorders. Cochrane Database Syst Rev 2000;(2):CD000961. [DOI] [PubMed]
- 9.Fisher P, Ward A. Medicine in Europe: complementary medicine in Europe. BMJ. 1994;309:107–111. doi: 10.1136/bmj.309.6947.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White AR, Ernst E. A systematic review of randomized controlled trials of acupuncture for neck pain. Rheumatology (Oxford) 1999;38:143–147. doi: 10.1093/rheumatology/38.2.143. [DOI] [PubMed] [Google Scholar]
- 11.NIH consensus conference. Acupuncture. JAMA. 1998;280:1518–1524. [PubMed] [Google Scholar]
- 12.Smith LA, Oldman AD, McQuay HJ, Moore RA. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain. 2000;86:119–132. doi: 10.1016/s0304-3959(00)00234-7. [DOI] [PubMed] [Google Scholar]
- 13.Schops P, Siebert U, Azad SC, Friedle AM, Beyer A. Diagnostic criteria and new classification of the cervical spine syndrome [Diagnostische Kriterien und neue Klassifikation des Halswirbelsäulensyndroms] Schmerz. 2000;3:160–174. doi: 10.1007/s004820000002. [DOI] [PubMed] [Google Scholar]
- 14.Travell JG, Simons DG. Myofascial pain and dysfunction. The trigger point manual. Baltimore, MD: Lippincott Williams and Wilkins; 1992. [Google Scholar]
- 15.Cheng Xinnong., editor. Chinese acupuncture and moxibustion. Beiijing: Foreign Languages Press; 1987. [Google Scholar]
- 16.Baldry PE. Acupuncture, trigger points and musculoskeletal pain. Edinburgh: Churchill Livingstone; 1993. [Google Scholar]
- 17.Irnich D. Acupuncture in complaints of the locomotor system, especially of the cervical syndrome [Akupunktur bei Beschwerden des Bewegungssystems am Beispiel des HWS-Syndrom] Deutsch Z Akupunkt. 1999;2:81–90. [Google Scholar]
- 18.Braverman DL, Schulman RA. Massage techniques in rehabilitation medicine. Phys Med Rehabil Clin N Am. 1999;3:631–649. [PubMed] [Google Scholar]
- 19.Vincent CA. Credibility assessment in trials of acupuncture. Complement Med Res. 1990;1:8–11. [Google Scholar]
- 20.Natalis M, König A. Noninvasive, accurate and reliable measurement of cervical spine motion with a 3D real-time ultrasound motion analyzer [Nichtinvasive, akkurate und reliable Messung der Halswirbelsäulenbeweglichkeit mittels ultraschallgestützter 3D-Echtzeitanalyse] Ultraschall Med. 1999;20:70–73. doi: 10.1055/s-1999-14237. [DOI] [PubMed] [Google Scholar]
- 21.Atkins CJ, Zielinski A, Klinkhoff AV, Chalmers A, Wade J, Williams D, et al. An electronic method for measuring joint tenderness in rheumatoid arthritis. Arthritis Rheum. 1992;35:407–410. doi: 10.1002/art.1780350408. [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey. Med Care. 1992;6:473–481. [PubMed] [Google Scholar]
- 23.Bourghouts JAJ, Koes BW, Bouter LM. The clinical course and prognostic factors of non-specific neck pain: a systematic review. Pain. 1998;77:1–13. doi: 10.1016/S0304-3959(98)00058-X. [DOI] [PubMed] [Google Scholar]
- 24.Bogduk N. Neck pain. Aust Fam Physician. 1984;13:26–30. [PubMed] [Google Scholar]
- 25.Vincent CA, Lewith G. Placebo controls for acupuncture studies. J R Soc Med. 1995;88:199–202. [PMC free article] [PubMed] [Google Scholar]