Introduction
Restoration of shoulder abduction following injury to the brachial plexus is sometimes difficult to achieve in obstetrical brachial plexus palsy and traumatic brachial plexus palsy. Nerve transfers are a recognized treatment option for patients with traumatic brachial plexus injuries [5]. To maximize shoulder function, notably shoulder abduction and external rotation, simultaneous reconstruction of the suprascapular and axillary nerves is often advocated [6, 7].
Nerve transfers permit faster reinnervation of muscle than traditional nerve grafting because the nerve repair can be performed much closer to the neuromuscular junction [9]. Application of nerve transfers in the obstetric brachial plexus palsy-affected population is gaining acceptance and is increasingly practiced along with or in lieu of neuroma resection with autologous nerve grafting [2].
While the triceps branch of the radial nerve to the axillary nerve transfer has been described in the adult patient population, there is a paucity of reports of its effectiveness in restoring shoulder abduction in children. In this report, consecutive cases of triceps to axillary nerve transfer in children performed by a single surgeon are reviewed. These nerve transfers were performed for patients with obstetrical brachial plexus palsy and also for traumatic injuries.
Materials and Methods
In order to evaluate whether the triceps to axillary nerve transfer improved shoulder abduction, all cases of pediatric patients at ages 17 years and younger who had received triceps to axillary nerve transfers by a single surgeon at a single institution from September 2008 to February 2009 were reviewed. Records that did not include a minimum of 1-year postoperative follow-up were excluded. The work was performed in accordance with the standards of our institution's research ethics board and with the Helsinki Declaration of 1975. The following data were obtained from the medical record: patient age at procedure, gender, etiology of brachial plexus injury (traumatic versus obstetric), preoperative active movement scores for shoulder abduction, shoulder external rotation and elbow extension, denervation time (defined as the time elapsed between brachial plexus injury and nerve transfer), the number of motor branches transferred from the triceps nerve, postoperative active movement scores for shoulder abduction, shoulder external rotation and elbow extension, and total follow-up time postprocedure.
The following is a description of the surgical technique. A curvilinear incision is made on the posterior upper arm down to the muscular fascia. The interval between the deltoid and the teres major muscle is dissected in order to locate the axillary nerve. By dissecting distally, inferior to the teres major muscle, branches of the radial nerve are located. With the help of bipolar stimulation, branches to the long, medial, and lateral heads of the triceps are identified. Care is taken to preserve the branches that serve the wrist or digital extension. Under the operating microscope, the axillary nerve is transected proximally and then reflected distally. The sensory branch of the axillary nerve is excluded from the reconstruction in an effort to maximize motor reinnervation. The nerve to the medial or long head of the triceps is transected distally, just prior to branching within the muscle. A tensionless nerve coaptation is performed with 9-0 or 10-0 nylon sutures. The involved upper extremity is immobilized in a Velpeau stockinette dressing for 10 days and then allowed to move freely. For children old enough to comply with physiotherapy, abduction is attempted at 3 months after first practicing maximal elbow extension. For infants and toddlers, therapy is play-based.
All children were followed up for a minimum of 1 year and The Hospital for Sick Children active movement scale (AMS) scores were obtained at every visit. The active movement scale of The Hospital for Sick Children is a well-validated, highly discriminatory 8-point test on a 0–7 scale that can identify subtle changes in upper extremity movement. A score of 4, or full range of movement without gravity, must first be attained before a full score of 7, or full range of motion against gravity is attained (See Table 1). Of great importance for this study, infants and young pediatric patients cannot comply with instructions for voluntary demonstration of full power, as required by the older, more familiar Medical Research Council scale. The active movement scale addresses this issue, and further studies have demonstrated its consistent interrater and intrarater reliability even among inexperienced examiners [1]. Statistical analysis involved an evaluation of patient AMS scores of shoulder abduction and external rotation at 1-year follow-up and compare them with preoperative scores. The threshold AMS score of ≥4 indicates movement against gravity while a score of 7 indicates full range of motion against gravity. AMS scores of triceps extension were also evaluated to determine whether transfer of the triceps nerve branches weakened elbow extension.
Table 1.
Explanation of active movement scale scores (adapted from Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin 1995; 11:563–581)
| Observation | Movement grade |
|---|---|
| Gravity eliminated | |
| No contraction | 0 |
| Contraction, no motion | 1 |
| Motion ≤1/2 range | 2 |
| Motion >1/2 range | 3 |
| Full motion | 4 |
| Against gravity | |
| Motion ≤1/2 range | 5 |
| Motion >1/2 range | 6 |
| Full motion | 7 |
Two-tailed Wilcoxan rank sum test was used for comparing preoperative and postoperative active movement scores. Linear regression analysis was performed to assess the correlation between denervation time and final AMS scores for shoulder abduction and external rotation. All statistical analysis was performed using GraphPad Prism (Version5.0, GraphPad Software Inc., La Jolla, CA). Significant associations were defined as p < 0.05.
Results
Seven patients received triceps to axillary nerve transfers during the study. It was not possible to obtain active movement scores for two of the seven patients at the minimum of 1-year follow-up, and these patients therefore did not meet inclusion criteria and were excluded from the analysis. Five patients fulfilled the criteria for inclusion in this report (Tables 2 and 3). The ages ranged from 212 days to 15 years old (average age, 6.3 years; standard deviation, 7.5 years).
Table 2.
Patient demographic and operative data for the five patients meeting inclusion criteria in the study
| Patient | Sex | Age at surgery | Etiology of injury | Triceps branch radial nerve transferred | Additional transfers / procedures | Denervation time (days) |
|---|---|---|---|---|---|---|
| I | F | 330 days | Trauma | Medial head branch | CNXI to Suprascapular | 132 |
| II | F | 15 years | Trauma | Medial head branch | (1) CNXI to Suprascapular | 128 |
| (2) Median to bicep | ||||||
| (3) Ulnar to brachialis | ||||||
| III | M | 14 years | Trauma | Medial head branch and long head branch | Decompress suprascapular | 172 |
| IV | M | 212 days | OBPP | Medial head branch | (1) CNXI to suprascapular | 212 |
| (2) Median to biceps | ||||||
| (3) Ulnar to brachialis | ||||||
| V | F | 306 days | OBPP | Medial head branch | (1)Decompression of suprascapular | 306 |
| (2) Median to biceps | ||||||
| (3) Ulnar to brachialis |
CNXI spinal accessory nerve
Table 3.
Preoperative vs. postoperative active movement scale (ams) scores
| Patient | Shoulder abduction pre-op | Shoulder abduction post-op | Shoulder external rotation pre-op | Shoulder external rotation post-op | Triceps extension pre-op | Triceps extension post-op |
|---|---|---|---|---|---|---|
| I | 1 | 7 | 3 | 7 | 7 | 7 |
| II | 2 | 7 | 0 | 7 | 7 | 7 |
| III | 2 | 6 | 0 | 6 | 7 | 7 |
| IV | 2 | 5 | 0 | 3 | 7 | 7 |
| V | 3 | 6 | 0 | 2 | 7 | 7 |
Postoperatively, all five patients were able to actively abduct their shoulders against gravity (as indicated by an AMS score of at least 4/7). Two of five patients had full range of motion against gravity (as indicated by an AMS score of 7/7). Improvement of external rotation of the shoulder was also noted with three of five patients scoring AMS of 5 or greater.
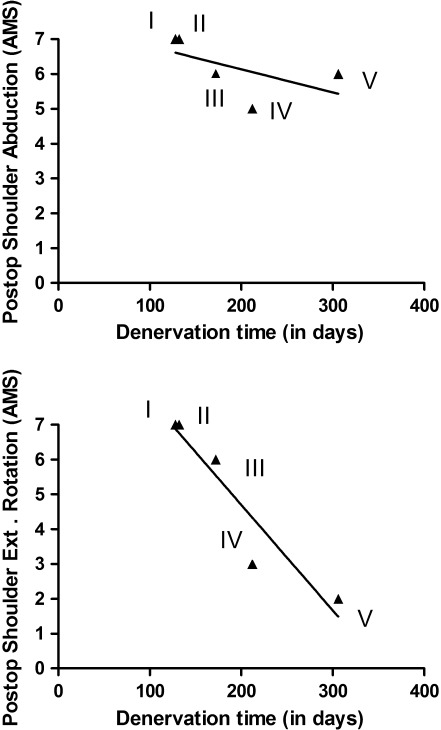
In all patients, AMS scores for triceps extension did not change postoperatively. All patients had elbow extension scores of 7/7 pretransfer and posttransfer, indicating that the use of one or two triceps branches did not produce a measureable decrement in elbow extension. Shorter denervation times correlated with better recovery for both shoulder abduction active movement scale scores and also for shoulder external rotation AMS scores (Fig. 1).
Fig. 1.
Linear regression demonstrated that postoperative active movement scale shoulder abduction (upper panel) and external rotation scores (lower panel) correlated with denervation time. Correlation for shoulder abduction was R2 = 0.35 (for a p value of 0.30) and correlation for shoulder external rotation was R2 = 0.89 (for a p value of 0.01), indicating that denervation time appeared to play a more significant role in the final outcome of shoulder external rotation than of shoulder abduction. Roman numerals indicate individual patients from Tables 1 and 2
Patient Summaries
Patient I
This patient suffered brachial plexus injury in a motor vehicle accident at 7 months of age. Active movement scores for shoulder abduction and shoulder external rotation were 1 and 3, respectively. Transfer of the left distal spinal accessory nerve to the suprascapular nerve and transfer of the nerve to the medial head of triceps to the axillary nerve were undertaken. Denervation time prior to surgery was 4 months. At postoperative follow-up of 390 days, AMS scores of 7 for both abduction and external rotation demonstrated recovery of shoulder function.
Patient II
Brachial plexus injury resulted from multiple stab wounds to the right shoulder at 15 years of age. Denervation time prior to surgery was 128 days. Preoperative AMS scores for shoulder abduction and external rotation were 2 and 0, respectively. Nerve transfers included the nerve from the long head of triceps to the axillary nerve, a median to bicep nerve transfer, an ulnar to brachialis nerve transfer, and transfer of the spinal accessory nerve to the suprascapular nerve. At 367 days postoperative follow-up, AMS score for shoulder abduction and external rotation were 7/7, indicating recovery of full range of active movement against gravity.
Patient III
This patient suffered brachial plexus injury due to a dirt-biking accident at age 14. On preoperative evaluation, his AMS score for shoulder abduction was 2 and AMS score for shoulder external rotation was 0. Denervation time prior to surgery was 172 days. He underwent transfer of the nerves to both the medial and long heads of triceps muscle to the axillary nerve. He also underwent decompression of the suprascapular nerve. At 699 days postoperatively, his shoulder abduction and external rotation scores had both improved to AMS 6/7.
Patient IV
This patient suffered obstetrical brachial plexus palsy. His preoperative AMS score for shoulder abduction and external rotation were 2 and 0, respectively. He underwent right distal spinal accessory to suprascapular nerve transfer and right medial head of triceps to posterior axillary nerve transfer at 212 days of age. He simultaneously underwent transfer of a fascicle of the median nerve to the biceps branch of the musculocutaneous nerve and transfer of a fascicle of the ulnar nerve to the brachialis branch of the musculocutaneous nerve. At 398 days postoperatively, shoulder abduction had improved to an AMS score of 6 while external rotation had improved to 3/7.
Patient V
Left shoulder function was compromised due to obstetrical brachial plexus palsy. On preoperative evaluation, shoulder abduction had an AMS score of 2 and shoulder external rotation was measured as 0. At 306 days old, the nerve to the medial head of triceps was transferred to the axillary nerve, and the suprascapular nerve was decompressed by dividing the suprascapular ligament from a posterior approach. In addition, median nerve to biceps branch of the musculocutaneous nerve and ulnar nerve to brachialis branch of the musculocutaneous nerve transfers were used. At 398 days postoperatively, shoulder abduction had improved to an AMS score of 6 and external rotation had improved to an AMS score of 2.
Discussion
In this pediatric case series, we have demonstrated the improvement in shoulder abduction by reinnervating the axillary nerve using transfers from the triceps motor branches. Leechavengvongs et al. [3] and Witoonchart et al. [10] first assessed the transfer of the long head of triceps branch of the radial nerve to the anterior branch of the axillary nerve by a posterior approach in an anatomic study followed by a clinical study in 2003. They demonstrated that the nerve to the long head of triceps could reliably be used for nerve transfer as it was of sufficient length to not require grafting, and of sufficient fascicular caliber (quantity of motor fibers) to provide for sufficient motor axons to reinnervate the deltoid via the anterior axillary nerve. They reported that the nerve to the long head of triceps has 45% of the fascicular volume of the anterior axillary nerve.
Lurje [4] is credited with the first use of the triceps branches to reinnervate the axillary nerve, reporting a transfer of two branches of the triceps nerve to the axillary nerve in a single case reported in 1948. His preferred technique for neurotization of the axillary nerve involved the use of two branches “rami tricipitis” as he felt that the triceps remained functional. He also felt that on cross section, two triceps nerve branches provided enough axons to reinnervate the large-caliber axillary nerve. Our patient with a double nerve transfer from both nerves to the medial and long heads of the triceps muscle had both a good functional recovery and minimal dysfunction noted on elbow extension.
The functional loss to the triceps with a single nerve transferred is negligible because of compensation by the remaining head(s). Travill [8] showed that among the three heads of the triceps, the long head is the least important for elbow extension. This is consistent with the data of our case series. In addition, the triceps action is synergistic with shoulder abduction, and therefore this represents an excellent choice for functional rehabilitation.
Considering this type of nerve transfer in children, one must be very careful in recognizing and distinguishing between obstetrical brachial plexus palsy (OBPP) and traumatic lesions. The majority of obstetrical lesions likely would not benefit from this strategy because, often, many different movements are impaired and nerve transfers address a smaller number of deficits, than do neuroma excision and nerve grafting. Only highly selected patients, therefore, would be served equally by this strategy compared with neuroma excision and sural nerve grafting. However, nerve transfer in OBPP cases should be considered if the child presents late (i.e., first seen by the surgical team at 6 months–1 year). Additionally, if previous sural nerve grafting or other supraclavicular reconstruction has been performed with no postoperative benefit at 1 year, then nerve transfer may be an additional option. Further, C5/C6 root avulsion with intact C7/C8/T1 roots present an anatomically favorable situation for use of this nerve transfer in combination with others mentioned in this series. Finally, those children who have been observed nonoperatively for many months, who have regained some essential functions (such as elbow flexion) but lack a small number of important movements, such as shoulder abduction, may benefit from isolated nerve transfers.
One major difference between OBPP and traumatic cases is that in OBPP most lesions are partial, thus leaving some fascicles intact, whereas many traumatic lesions are complete transections. Because partial lesions present incomplete recovery, additional time may elapse before the window of possibility for nerve transfers to permit recovery narrows, compared to traumatic cases. Again, OBPP lesions and traumatic lesions must be considered entirely different since their pathophysiology and anticipated outcomes are very different.
The preoperative status of the axillary nerve was determined using the active movement scale, a sensitive, validated instrument that has been previously demonstrated to be effective in determining the preoperative and postoperative function in infants and small children (Tables 1, 2 and 3). For the two OBPP cases, shoulder abduction was preoperatively rated at 2 and 3 out of a possible score of 7. Following transfer, the scores were 5 and 6, respectively (which indicates that the two patients were able to achieve antigravity shoulder abduction). For a full list of the ratings of the active movement scale, please see Table 1. Our interpretation of these preoperative AMS scores is that the axillary nerve was partially injured, and given that useful recovery had not occurred by age 6–9 months, it was unlikely that these two children would gain meaningful function without surgery. Again, these two cases are highly selected among many children with OBPP, the majority of which are observed nonoperatively, and those that undergo surgery are primarily treated with sural nerve grafting.
In interpreting this study, one must recognize that the number of patients is small, and therefore conclusions based on the application of this technique in either OBPP or pediatric trauma should be viewed with appropriate caution. Another limitation of the study is that preoperative and postoperative EMG was not available since this is not our typical routine in our institution. Unfortunately, while obtaining that postoperative EMG is possible in the older children, obtaining reliable EMGs in preschool-aged children is not currently feasible at our institution without sedation. For this reason, we are very selective in ordering sedated EMG, and we generally follow clinical examination to assess preoperative status and postoperative recovery.
Postoperative physiotherapy following these nerve transfers presents some special challenges compared with adults. In teens and younger school-aged children, compliance with therapy may be a significant issue. Play- and game-based therapy is often helpful in this age. In preschool-aged children, play-based therapy is necessary.
Summary
Transfer of branches of the triceps motor nerves to the axillary nerves appears to be safe and effective in restoring shoulder abduction in children and adolescents. Use of this technique should be considered in selected individuals with upper brachial plexus injuries.
Acknowledgments
Conflicts of Interest
The authors declare that they have no conflicts of interest, commercial associations, or intent of financial gain regarding this research.
References
- 1.Curtis C, Stephens D, Clarke HM, Andrews D. The active movement scale: an evaluative tool for infants with obstetrical brachial plexus palsy. J Hand Surg Am. 2002;27(3):470–8. doi: 10.1053/jhsu.2002.32965. [DOI] [PubMed] [Google Scholar]
- 2.Hale HB, Bae DS, Waters PM. Current concepts in the management of brachial plexus birth palsy. J Hand Surg Am. Feb;35(2):322–31. [DOI] [PubMed]
- 3.Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part II: a report of 7 cases. J Hand Surg Am. 2003;28(4):633–8. doi: 10.1016/S0363-5023(03)00199-0. [DOI] [PubMed] [Google Scholar]
- 4.Lurje A. Concerning surgical treatment of traumatic injury to the upper division of the brachial plexus (Erb's type) Ann Surg. 1948;127(2):317–26. doi: 10.1097/00000658-194802000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merrell GA, Barrie KA, Katz DL, Wolfe SW. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg Am. 2001;26(2):303–14. doi: 10.1053/jhsu.2001.21518. [DOI] [PubMed] [Google Scholar]
- 6.Terzis JK, Barmpitsioti A. Axillary nerve reconstruction in 176 posttraumatic plexopathy patients. Plast Reconstr Surg. 2010;125(1):233–47. doi: 10.1097/PRS.0b013e3181c496e4. [DOI] [PubMed] [Google Scholar]
- 7.Terzis JK, Kokkalis ZT. Shoulder function following primary axillary nerve reconstruction in obstetrical brachial plexus patients. Plast Reconstr Surg. 2008;122(5):1457–69. doi: 10.1097/PRS.0b013e3181881f70. [DOI] [PubMed] [Google Scholar]
- 8.Travill AA. Electromyographic study of the extensor apparatus of the forearm. Anat Rec. 1962;144:373–6. doi: 10.1002/ar.1091440408. [DOI] [PubMed] [Google Scholar]
- 9.Tung TH, Mackinnon SE. Nerve transfers: indications, techniques, and outcomes. J Hand Surg Am. 2010;35(2):332–41. doi: 10.1016/j.jhsa.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 10.Witoonchart K, Leechavengvongs S, Uerpairojkit C, Thuvasethakul P, Wongnopsuwan V. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part I: an anatomic feasibility study. J Hand Surg Am. 2003;28(4):628–32. doi: 10.1016/S0363-5023(03)00200-4. [DOI] [PubMed] [Google Scholar]