Introduction
Arthroplasty of the metacarpophalangeal (MCP) joints for inflammatory arthritis can be performed using silicone implants with or without metal grommets. Titanium metal grommets were introduced in 1987 for MCP joint arthroplasty and theoretically protect the silicone implant from fracture and fragmentation [15, 16, 18, 20–22]. We found two reports of particulate metal debris associated with silicone implants with grommets leading to a robust tissue reaction [9, 25]. In contrast, metallosis from hip and knee arthroplasty has been frequently reported [7, 8, 11, 24, 26]. Herein we present a patient with rheumatoid arthritis who developed metallosis following MCP arthroplasties with grommets.
Case Report
A 70-year-old right-handed female with longstanding rheumatoid arthritis was referred for increasing difficulty extending the fingers of her left hand at the MCP joints. Ten years earlier she underwent silicone MCP joint implants (Wright Medical Technology Inc. Tennessee, USA) with grommets in her index, middle, and ring fingers. She did well initially but over time she noticed deterioration in function. She also complained of increasing pain and progressive deformity at the MCP joints. Examination revealed swelling over the MCP joints. At rest the MCP joints of all fingers were fixed in 90° of flexion, ulnarly deviated, and dislocated. Although, she was unable to actively extend her fingers at the MCP joint, the extensor tendons appeared to be intact and were visible through her thin dorsal skin. Radiographic examination confirmed failure of MCP joint arthroplasties with radial deviation of the metacarpals (Fig. 1). Notable osteolysis was absent.
Fig. 1.
Anteroposterior radiographs demonstrating dislocated MCP joint silicone arthroplasties with grommets
We elected to perform revision MCP joint silicone arthroplasties. Radial deviation of the metacarpals was not addressed surgically due to the frail nature of the patient. Abundant metallic gray tissue surrounding the implants was observed, debrided, and sent for histological evaluation (Fig. 2). The extensor tendons of all four fingers were ulnarly dislocated with mild fraying but were otherwise intact. All of the silicone implants were fractured. New silicone implants without grommets were inserted. Postoperatively, the fingers were splinted in extension for 3 weeks followed by initiation of active range of motion and night splinting for 8 weeks. Follow-up 3 months later revealed ulnar drift of 10° and range of motion from 20° of extension to 70° of flexion.
Fig. 2.
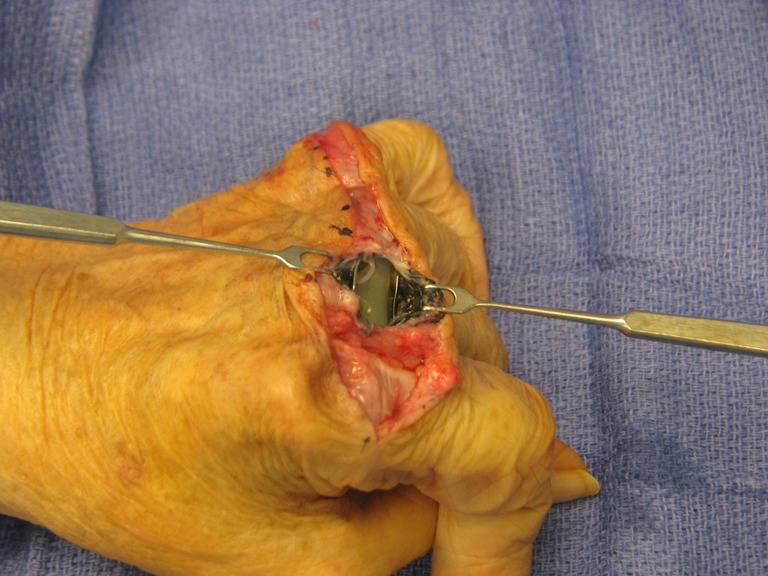
Clinical intraoperative photo demonstrating the silicone implants with grommets. Note the metallic gray pseudosynovium
Histology showed prominent reactive fibrosis with numerous subsynovial black, irregular metallic particles associated with giant cell reaction (Fig. 3). Silicone particles were not present. Numerous refractile particles were seen in the tissue under examination of polarized light (Fig. 4).
Fig. 3.
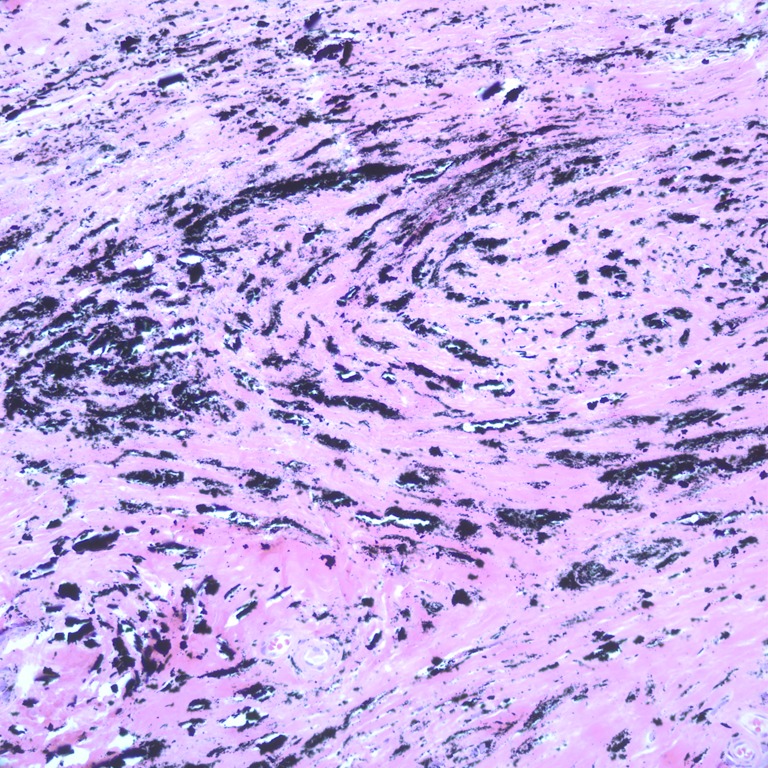
Extensive metallic particle deposition in the pseudosynovial tissue. H&E × 200
Fig. 4.
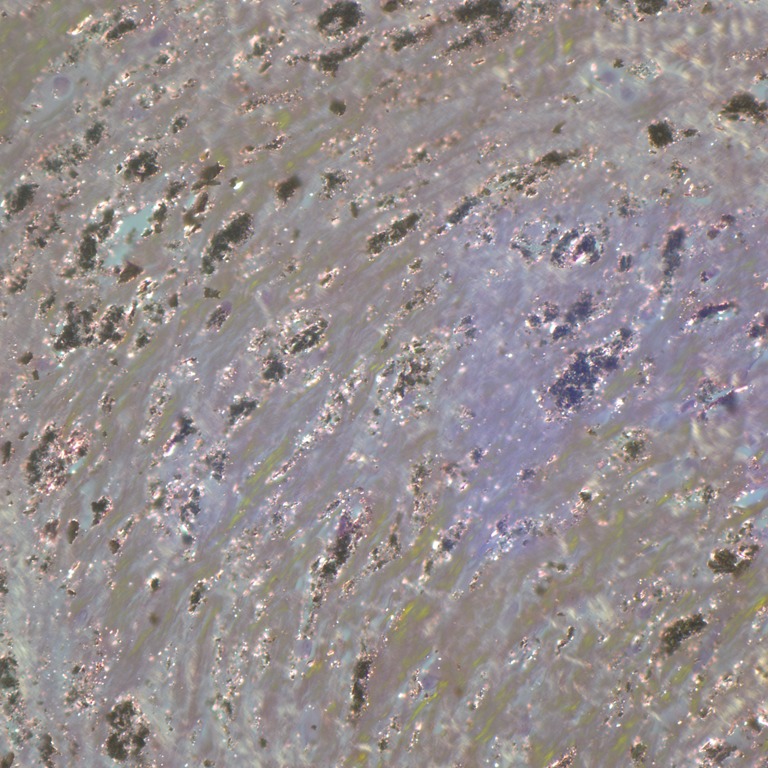
Many refractile particles noted under polarized light evaluation. ×400
Discussion
Titanium grommets used in association with MCP joint arthroplasty have been available since 1987 [21]. It has been postulated that grommet use in silicone arthroplasty protects the implants from breakage and fragmentation [18]. Swanson et al. reported on silicone implants with grommets for MCP and first metatarsophalangeal joint arthroplasty [18, 21]. They compared differences between arthroplasties performed with and without grommets and found a higher incidence of bone resorption, implant breakage, and reactive synovitis in the group without grommets. They concluded that grommets protect the implant from breakage and provide a better implant–bone interface leading to enhanced bone preservation [21].
The use of grommets has also been attempted on other joints such as the wrist [3, 13, 17, 19]. Swanson et al. reported favorable results in flexible radiocarpal arthroplasties noting no breakage [19]. Although they report a few cases of synovitis, they do not elaborate on its nature. Similarly, Rossello et al. reported their results of 32 silicone total wrist implant with grommets [13]. One grommet dislocated and there were no cases of particulate synovitis.
Silicone debris from small joint implants incites a symptomatic inflammatory reaction [2, 6, 12]. Debris from metal on metal arthroplasty can also cause an intense particulate tissue reaction termed metallosis and has been reported primarily following knee and metal on metal hip arthroplasty [7, 8, 11, 24, 26]. Symptomatic titanium debris and metallosis from elbow and other hand arthroplasty procedures has been reported sporadically in the literature [1, 4, 9, 14, 25]. Pathologic evaluation typically reveals metal debris with an intense tissue reaction characterized by giant cells and fibrosis. Associated silicone synovitis may also be present. Khoo et al. reported two cases of metallosis related to silicone MCP joint implants with grommets [9]. Both patients required revision surgery secondary to pain and inflammation. Comparison of their pathology with ours bares striking resemblance except that our case lacked particulate synovitis from the silicone.
Trail et al. retrospectively reviewed the 17-year survivorship of over 1,000 silicone MCP joint arthroplasties [23]. They statistically analyzed differences between revision rates of implants with and without grommets and concluded that grommets did not protect the implant from fracture. In our patient, all silicone implants had fractured. Our report illustrates a case of metallosis from grommets in the setting of painful MCP joint arthroplasty failure in three of four affected fingers that ultimately required revision surgery. The metallosis would be classified as grade 3+ (jet-black histiocytes/>100 visible metal particles/histiocytes) according to the modified Mirra classification [5, 10]. A causal relationship between metallosis and implant failure cannot be made based on this case report. Radial deviation of the metacarpals may have been a contributing factor to implant failure as well.
Nevertheless, this case highlights an unusual complication associated with grommets and adds to the growing literature that grommets do not necessarily protect the silicone from fracturing. Metallosis is a potential long-term complication of grommets, and given the lack of documented benefit from grommets we recommend against their use.
Acknowledgments
The authors would like to thank Dr. Jiang Wang for assisting in the pathologic evaluation and imaging for this publication.
Conflicts of Interest
The authors have no conflicts of interest, commercial associations, or intent of financial gain regarding this research.
Contributor Information
Imran K. Choudhry, Phone: +1-513-5584592, FAX: +1-513-5582220, Email: imranchoudhry2003@yahoo.com
Joyce M. Wilson, Phone: +1-573-6358000, FAX: +1-573-5561710, Email: jpingsterhaus@gmail.com
Peter J. Stern, Phone: +1-513-5584516, FAX: +1-513-5582220, Email: pstern@handsurg.com
References
- 1.Asahina A, Fujita H, Fukuda S, Kai H. Extensive skin pigmentation caused by deposits of metallic particles following total elbow arthroplasty: metallosis or not? Br J Dermatol. 2007;157(5):1074–1076. doi: 10.1111/j.1365-2133.2007.08161.x. [DOI] [PubMed] [Google Scholar]
- 2.Atkinson RE, Smith RJ. Silicone synovitis following silicone implant arthroplasty. Hand Clin. 1986;2(2):291–299. [PubMed] [Google Scholar]
- 3.Capone RA., Jr The titanium grommet in flexible implant arthroplasty of the radiocarpal joint: a long-term review of 44 cases. Plast Reconstr Surg. 1995;96(3):667–672. doi: 10.1097/00006534-199509000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Degreef I, Sciot R, Smet L. Metallosis in revision total elbow arthroplasty. Complications and staging method. Acta Orthop Belg. 2008;74(6):753–760. [PubMed] [Google Scholar]
- 5.Doorn PF, Mirra JM, Campbell PA. Tissue reaction to metal on metal total hip prostheses. Clin Orthop Relat Res. 1996;329:S187–205. doi: 10.1097/00003086-199608001-00017. [DOI] [PubMed] [Google Scholar]
- 6.Foliart D. Swanson silicone finger joint implants: a review of the literature regarding long-term complications. J Hand Surg Am. 1995;20(3):445–449. doi: 10.1016/S0363-5023(05)80104-2. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs JJ, Hallab NJ. Loosening and osteolysis associated with metal-on-metal bearings: a local effect of metal hypersensitivity? J Bone Joint Surg Am. 2006;88(6):1171–1172. doi: 10.2106/JBJS.F.00453. [DOI] [PubMed] [Google Scholar]
- 8.Jacobs JJ, Urban RM, Hallab NJ. Metal-on-metal bearing surfaces. J Am Acad Orthop Surg. 2009;17(2):69–76. doi: 10.5435/00124635-200902000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Khoo CT, Davison JA, Ali M. Tissue reaction to titanium debris following Swanson arthroplasty in the hand: a report of two cases. J Hand Surg Br. 2004;29(2):152–154. doi: 10.1016/j.jhsb.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Korovessis P, Petsinis G, Repanti M, et al. Metallosis after contemporary metal-on-metal total hip arthroplasty: five to nine-year follow-up. J Bone Joint Surg Am. 2006;88(6):1183–91. doi: 10.2106/JBJS.D.02916. [DOI] [PubMed] [Google Scholar]
- 11.Ollivere B, Darrah C, Barker T. Early clinical failure of the Birmingham metal-on-metal hip resurfacing is associated with metallosis and soft-tissue necrosis. J Bone Joint Surg Br. 2009;91(8):1025–1030. doi: 10.1302/0301-620X.91B8.21701. [DOI] [PubMed] [Google Scholar]
- 12.Peimer CA, Medige J, Eckert BS. Reactive synovitis after silicone arthroplasty. J Hand Surg Am. 1986;11(5):624–638. doi: 10.1016/s0363-5023(86)80002-8. [DOI] [PubMed] [Google Scholar]
- 13.Rossello MI, Costa M, Pizzorno V. Experience of total wrist arthroplasty with silastic implants plus grommets. Clin Orthop Relat Res. 1997;342:64–70. doi: 10.1097/00003086-199709000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Sayed-Noor AS, Sjödén GO. Severe metallosis after total elbow arthroplasty—a case report. Hand. 2010;5:86–89. doi: 10.1007/s11552-009-9201-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt K, Willburger R, Ossowski A. The effect of the additional use of grommets in silicone implant arthroplasty of the metacarpophalangeal joints. J Hand Surg Br. 1999;24(5):561–564. doi: 10.1054/jhsb.1999.0240. [DOI] [PubMed] [Google Scholar]
- 16.Sebold EJ, Cracchiolo A., 3rd Use of titanium grommets in silicone implant arthroplasty of the hallux metatarsophalangeal joint. Foot Ankle Int. 1996;17(3):145–151. doi: 10.1177/107110079601700305. [DOI] [PubMed] [Google Scholar]
- 17.Swanson AB, Swanson G. Flexible implant arthroplasty of the radiocarpal joint. Semin Arthroplasty. 1991;2(2):78–84. [PubMed] [Google Scholar]
- 18.Swanson AB, Swanson G, Ishikawa H. Use of grommets for flexible implant resection arthroplasty of the metacarpophalangeal joint. Clin Orthop Relat Res. 1997;342:22–33. [PubMed] [Google Scholar]
- 19.Swanson AB, Swanson G, Maupin BK. Flexible implant arthroplasty of the radiocarpal joint. Surgical technique and long-term study. Clin Orthop Relat Res. 1984;187:94–106. [PubMed] [Google Scholar]
- 20.Swanson AB, Swanson G, Maupin BK. The use of a grommet bone liner for flexible hinge implant arthroplasty of the great toe. Foot Ankle. 1991;12(3):149–155. doi: 10.1177/107110079101200304. [DOI] [PubMed] [Google Scholar]
- 21.Swanson AB. de Groot Swanson G. Use of grommets for flexible hinge implant arthroplasty of the great toe. Clin Orthop Relat Res. 1997;340:87–94. doi: 10.1097/00003086-199707000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Takatori R, Tokunaga D, Hojo T. Utility of grommets for implant arthroplasty of the great toe in a patient with rheumatoid arthritis: a case report. Mod Rheumatol. 2005;15(5):364–366. doi: 10.1007/s10165-005-0413-y. [DOI] [PubMed] [Google Scholar]
- 23.Trail IA, Martin JA, Nuttall D, et al. Seventeen-year survivorship analysis of silastic metacarphalangeal joint replacement. J Bone Joint Surg Br. 2004;86B:1002–1006. doi: 10.1302/0301-620X.86B7.15061. [DOI] [PubMed] [Google Scholar]
- 24.Urban RM, Jacobs JJ, Tomlinson MJ. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82(4):457–476. doi: 10.2106/00004623-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Voellmicke KV, Bansal M, O'Malley MJ. Failed first metatarsophalangeal arthroplasty salvaged by hamstring interposition arthroplasty: metallic debris from grommets. Am J Orthop. 2008;37(2):E42–45. [PubMed] [Google Scholar]
- 26.Willis-Owen CA, Keene GC, Oakeshott RD. Early metallosis-related failure after total knee replacement: a report of 15 cases. J Bone Joint Surg Br. 2011;93(2):205–209. doi: 10.1302/0301-620X.93B2.25150. [DOI] [PubMed] [Google Scholar]



