Abstract
Childhood sexual abuse (CSA) is associated with sexual risk behavior in adulthood, but little research has investigated processes that might mediate this relation. The purpose of this study was to investigate whether constructs suggested by the traumagenic dynamics (TD) model (a theory of the effects of CSA) or constructs suggested by the Information-Motivation-Behavioral skills (IMB) model (a theory of the antecedents of sexual risk behavior) better mediated the relation between CSA and sexual risk behavior in adulthood. Participants were 481 women attending an STI clinic (66% African American) who completed a computerized survey as well as behavioral simulations assessing condom application and sexual assertiveness skills. Forty-five percent of the sample met criteria for CSA and CSA was associated with sexual risk behavior in adulthood. In multiple mediator models, the TD constructs mediated the relation between CSA and the number of sexual partners whereas the IMB constructs mediated the relation between CSA and unprotected sex. In addition, the TD constructs better mediated the relation between CSA and the number of sexual partners; the TD and IMB constructs did not differ in their ability to mediate the relation between CSA and unprotected sex. Sexual risk reduction interventions for women who were sexually abused should target not only the constructs from health behavior models (e.g., motivation and skills to reduce sexual risk), but also constructs that are specific to sexual abuse (e.g., traumatic sexualization and guilt).
Keywords: child sexual abuse, sexual risk behavior, information motivation behavioral skills model, traumagenic dynamics model, mediation
INTRODUCTION
Sexually transmitted infections (STIs) are a major public health problem for women. In 2008, there were more than 890,000 cases of Chlamydia and more than 180,000 cases of gonorrhea reported among women in the U.S. (Centers for Disease Control and Prevention, 2008). For women, the consequences of having an STI include pelvic inflammatory disease, ectopic pregnancy, and infertility (Centers for Disease Control and Prevention, 2008); infection with an STI also increases the risk of being infected with HIV (Fleming & Wasserheit, 1999).
Childhood sexual abuse (CSA) is also a major problem for women, affecting 15% to 32% of women in the U. S. (Briere & Elliott, 2003; Vogeltanz et al., 1999). Women with a history of CSA are especially vulnerable to STIs. CSA has been associated with several risk behaviors among women, including an earlier age of first intercourse, a greater number of sexual partners, and trading sex for money or drugs (Cohen et al., 2000; DiIorio, Hartwell, & Hansen, 2002; NIMH Multisite Prevention Trial Group, 2001; Senn, Carey, Vanable, Coury-Doniger, & Urban, 2006). In addition, CSA has been associated with a greater likelihood of being diagnosed with an STI for women (Brown, Lourie, Zlotnick, & Cohn, 2000; Senn et al., 2006; Upchurch & Kusunoki, 2004). This association between CSA and sexual risk behavior in adulthood has been found in the general population of women as well as specific subgroups (e.g., women attending primary care clinics, ethnic minority women, women infected with or at risk for HIV, etc.) (for review, see Senn, Carey, & Vanable, 2008).
Conceptual Models and Empirical Evidence Linking CSA with Sexual Risk Behavior in Adulthood
Despite the well-established relation between CSA and sexual risk behavior in adulthood, there is little empirical research investigating how CSA may lead to sexual risk behavior. Several researchers have proposed conceptual models of the CSA/sexual risk relation that include mediating variables such as mental health, self-efficacy or assertiveness, substance use, sexual revictimization, and partner violence (Malow, Dévieux, & Lucenko, 2006; Miller, 1999; Purcell, Malow, Dolezal, & Carballo-Dieguez, 2004). Some of these variables, such as substance use and partner violence, have received empirical support as mediators of the CSA/adult sexual risk behavior relation (NIMH Multisite Prevention Trial Group, 2001; Senn et al., 2006). Recent research has also found that being in unstable relationships also mediates the relation between CSA and sexual risk behavior in adulthood (Wilson & Widom, 2011). However, no research has investigated cognitive or appraisal factors that might mediate the relation between CSA and sexual risk behavior in adulthood.
Two conceptual models have been proposed that may help to explain the relationship between CSA and sexual risk behavior in adulthood. One model, the traumagenic dynamics framework, begins with a focus on CSA whereas the second model, information-motivation-behavioral skills model, begins with a focus on sexual risk behavior.
Traumagenic Dynamics
The traumagenic dynamics (TD) framework (Finkelhor & Browne, 1985) suggests one set of psychological variables that may mediate the CSA-adult sexual risk behavior relation. According to the TD framework, CSA may lead to four consequences: (1) traumatic sexualization, in which maladaptive scripts for sexual behavior are developed and reinforced because the child is rewarded for sexual activity; (2) betrayal and lack of trust, in which the child feels betrayed by the abuser, by others’ reactions to abuse disclosure, or by others’ failure to recognize and stop the abuse; (3) stigmatization, in which the child feels stigmatized because of the abuse as sexually different and thus feels shame and guilt; and (4) powerlessness, in which the child feels unable to control the sexual aspects of relationships (Finkelhor & Browne, 1985).
All four traumagenic dynamics may influence later sexual risk behavior. Traumatic sexualization may lead individuals who were sexually abused to have many sexual partners or to agree to risky sexual activity with a sexual partner, to obtain affection or other rewards. Betrayal may lead to difficulty trusting others and forming close relationships or it may lead to impairment in learning how to judge who is trustworthy, both of which could lead to brief, multiple relationships. Stigmatization may lead an individual to feel that they are sexually different from others and perhaps that they are in some way “marked” as someone who is highly sexually active or who enjoys sexual activity. These feelings, if internalized, could lead them to have multiple sexual partners or engage in unsafe sexual behavior. Alternatively, feelings of shame or guilt about sexual behavior could lead to less sexual behavior. Finally, powerlessness could lead to feeling unable to control sexual situations; an individual who feels powerless may be unable to refuse sex or unable to refuse risky sex. Thus, there is reason to believe that traumatic sexualization, betrayal, stigmatization, and powerlessness may mediate the association between CSA and sexual risk behavior in adulthood.
There is evidence that CSA is related to the TD constructs. CSA has been associated with greater traumatic sexualization (Matorin & Lynn, 1998), less partner trust (DiLillo & Long, 1999; Mullen, Martin, Anderson, Romans, & Herbison, 1994), more shame (Feiring, Coates, & Taska, 2001), and greater powerlessness (Bolger & Patterson, 2001; Bolstad & Zinbarg, 1997; Gwandure, 2007). In addition, the TD constructs have been associated with later psychological functioning. Greater traumatic sexualization was associated with more anxiety, sexual avoidance, and less sexual self-esteem (Hazzard, 1993; Matorin & Lynn, 1998). Greater betrayal beliefs were associated with more interpersonal problems (Hazzard, 1993). Greater shame and stigmatization were associated with lower self-esteem, more psychological distress, and depression (Hazzard, 1993; Wenninger & Ehlers, 1998) and greater powerlessness was associated with lower self-esteem and more depression (Hazzard, 1993).
Further, there is some evidence that the traumagenic dynamics constructs mediate the relation between CSA and later psychological outcomes (i.e., outcomes other than sexual risk behavior). Stigmatization mediated the relation between CSA and use of disengagement methods of coping to deal with a recent sexual assault (Gibson & Leitenberg, 2001) and between CSA and adult psychological adjustment (Coffey, Leitenberg, Henning, Turner, & Bennett, 1996; Kallstrom-Fuqua, Weston, & Marshall, 2004). Powerlessness mediated the relation between CSA and maladaptive relationships and between CSA and psychological distress (Kallstrom-Fuqua et al., 2004). However, to our knowledge, no research has investigated whether these TD constructs are associated with sexual risk behavior in adulthood or whether they mediate the relation between CSA and sexual risk behavior in adulthood.
Information-Motivation-Behavioral Skills Model of Sexual Risk Behavior
The IMB model (Fisher & Fisher, 1992), which was developed based on research in sexual health and behavior, suggests a different set of mediating constructs. In this model, information (about transmission, prevention, and consequences of STIs), motivation (e.g., motivation to protect oneself and attitudes towards safer sex), and behavioral skills (e.g., skills for discussing safer sex with a partner and condom use skills) influence sexual risk (and protective) behavior.
Numerous studies support the association between the IMB constructs and sexual risk behavior (Mustanski, Donenberg, & Emerson, 2006; Robertson, Stein, & Baird-Thomas, 2006; Scott-Sheldon et al., 2010). Associations between IMB constructs and sexual risk behavior have been found in a variety of populations, including adolescents (Boyer et al., 2000), adolescents seeking mental health care (Mustanski et al., 2006), incarcerated adolescents (Robertson et al., 2006), and patients attending STI clinics (Walsh, Senn, Scott-Sheldon, Vanable, & Carey, 2011). The relation between motivation, skills, and sexual risk behavior has been consistently established, although the relation between information and sexual risk behavior is less consistent (Fisher, Fisher, & Shuper, 2009). A meta-analysis found that interventions with motivational and skills components increased condom use more than interventions that did not include these components (Johnson, Carey, Chaudoir, & Reid, 2006), further supporting the utility of the IMB model. Thus, the link between the IMB constructs and sexual risk behavior is well-established.
There are several mechanisms through which CSA might lead to impairments in safer sex information, motivation, or behavioral skills. CSA may lead to dissociative tendencies, which could interfere with the encoding and processing of sex-related information (Zurbriggen & Freyd, 2004). For example, high scores on a measure of dissociative tendencies were associated both with more past traumatic experiences and with remembering fewer trauma-related words on a divided attention task (Freyd, Martorello, Alvarado, Hayes, & Christman, 1998). Thus, individuals who were sexually abused may have difficulty processing or remembering sex-related information and thus may have deficits in HIV-related knowledge. CSA may also lead to difficulties in distinguishing reality from fantasy because many abusers lie or distort reality (Zurbriggen & Freyd, 2004). Being motivated to engage in safer sexual behaviors may require the understanding that one is at risk for contracting HIV; if individuals are unable to accurately assess the reality of their sexual situations, they may not believe they are at risk for contracting HIV. Perceiving no risk, they may not be motivated to engage in safer sexual behaviors. Finally, individuals who were sexually abused as children may have learned that they have no control over sexual situations; therefore, they may lack the self-efficacy or skills necessary to engage in safer sex.
Although the link between the IMB constructs and CSA is not well-studied, there is some empirical support for the relation between CSA and the IMB constructs. CSA has been associated with less HIV-related knowledge, less favorable safer sex attitudes, less self-efficacy, and fewer skills. Most of this research has been conducted with adolescents (Brown, Kessel, Lourie, Ford, & Lipsitt, 1997; Brown et al., 2000; Hall, Hogben, Carlton, Liddon, & Koumans, 2008; Slonim-Nevo & Mukuka, 2007) and college women (Johnsen & Harlow, 1996). To our knowledge, only one study has investigated the association between CSA and IMB constructs in adult females (Noll, Horowitz, Bonanno, Trickett, & Putnam, 2003). The majority of these studies were cross-sectional, with the exception of the study by Noll et al., in which females who experienced CSA were matched with non-abused females and followed longitudinally. The majority of these studies also relied on self-report data. One study required that a subset of participants complete a role play exercise to assess safer sex communication skills; consistent with self-reported self-efficacy, sexually abused participants received lower scores on the role play exercise than non-abused participants (Brown et al., 1997). Thus, there is both theoretical support and empirical evidence that suggests the IMB constructs are plausible mediators of the CSA-sexual risk behavior relation.
Purpose of the Present Study
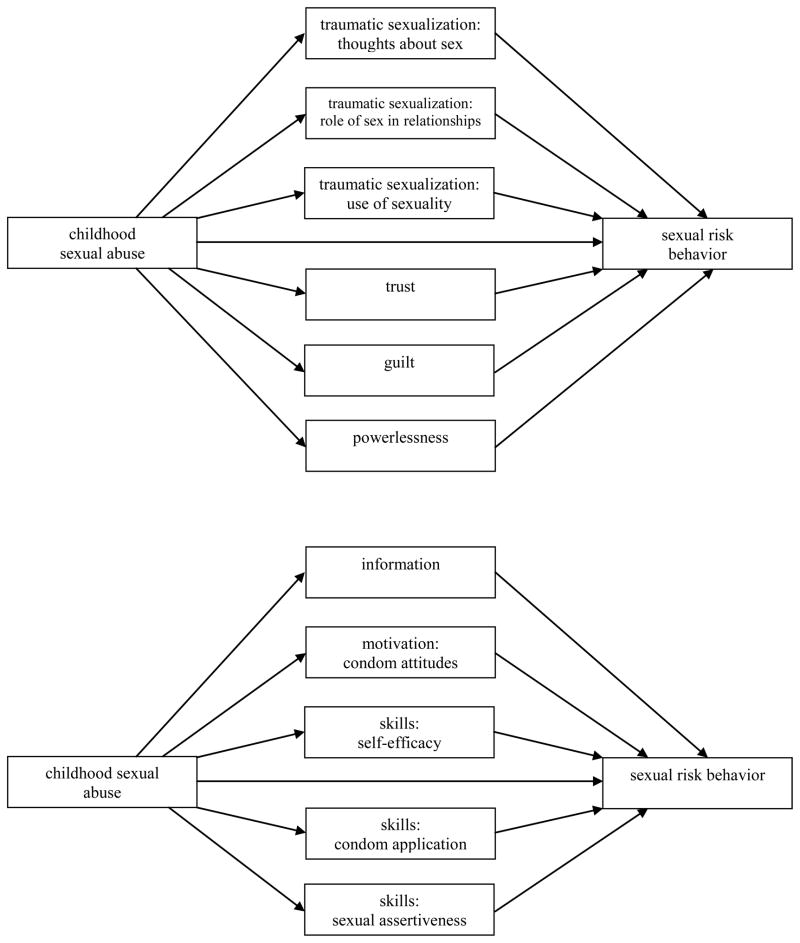
The present research had three main purposes: (1) to determine whether TD constructs mediate the relation between CSA and sexual risk behavior in adulthood; (2) to determine whether IMB constructs mediate the relation between CSA and sexual risk behavior in adulthood; and (3) to determine whether constructs associated with the TD model or constructs associated with the IMB model better mediate the relation between CSA and sexual risk behavior in adulthood (see Fig. 1).
Figure 1.
Mediation models being tested. Top figure shows meditational paths through traumagenic dynamics constructs; bottom figure shows meditational paths through information-motivation-behavioral skills constructs.
METHOD
Participants
Participants were 481 women attending an STI clinic who agreed to participate in a study investigating potential mediators of the relation between childhood sexual experiences and current sexual risk behaviors. The inclusion criterion was: sexually active in the past 3 months. Exclusion criteria were: less than 18 years of age or mental impairment that would prevent someone from participating meaningfully in the study. Of the 1008 women approached about the study, 945 women (94%) agreed to answer the screening questions, 791 women (84% of those screened) were eligible to participate, and 481 (61% of those eligible) agreed to participate.
The sample was 66% African American (n = 317) and 19% Caucasian (n = 90). Approximately half of the sample had a high school or less education (56%; n = 271), was unemployed (49%; n = 235), and had an income <$15,000/year (56%; n = 265). Participants were, on average, 27.5 years of age (SD = 8.8). The majority were single/never married (81%; n = 389).
Procedure
Clinic patients met with a trained research assistant (RA) in a private room where the RA overviewed the study and asked the women if they would be willing to answer a few questions to determine eligibility. The study was explained to eligible women; those who agreed to participate provided written informed consent. Participants completed a calendar of important events in the past 3 months (to orient them to that time frame) and then completed a computerized survey in the private room. The survey assessed childhood sexual experiences, TD and IMB constructs, and sexual behavior. Participants also completed role plays that were presented on a computer and digitally recorded, and completed a condom demonstration exercise which was observed and scored by the RA. Participation took one hour and participants were reimbursed $20 for their time.
At the end of the study tasks, participants were debriefed. As part of this debriefing, they were asked whether they were upset by any of the questions or activities. All participants were provided with a list of local low- and no-cost counseling centers; if participants were interested, we helped them set up an appointment. Participants were also invited to share their thoughts and feelings with the nurse counselor who conducted their HIV pretest counseling (which they received as part of their routine clinic visit after study participation). Finally, participants were given a 24-hour crisis hotline number, in case they ever wanted to talk to someone. Although a few participants reported mild distress, no participants were significantly distressed by their participation. We checked in with participants who reported mild distress; by the time they completed their clinic visit, none remained distressed. All procedures were approved by the Institutional Review Boards of the participating institutions.
Measures
Demographics
Participants reported their race (recoded as Caucasian vs. non-Caucasian for analyses), education (recoded as high school or less vs. some college), employment status (recoded as employed vs. unemployed), income (recoded as < $15,000/year vs. ≥ $15,000/year), marital status (recoded as single vs. ever married), and age.
Childhood sexual abuse
We asked about sexual abuse experience in two ways to be sure that all events were captured. First, participants reported on the different people with whom they had a sexual experience before age 18. The survey allowed participants to report up to 10 different people. These sexual experiences could have been wanted or unwanted and could range from kissing to intercourse. For each person with whom they had a sexual experience, they were asked their age, the other person’s age, their relationship to the other person, the type of act (kissing, fondling, receiving oral sex, giving oral sex, vaginal intercourse, anal intercourse), the duration of the sexual relationship, and whether or not threat or force was used. Questions were adapted from Finkelhor (1979). Second, participants were asked whether or not they were sexually abused as a child. If they answered “yes,” they were asked to provide details about the nature of this experience, including their age, the other person’s age, their relationship to the other person, the type of act, the duration of the sexual relationship, and whether or not threat or force was used. Because either method on its own could be subject to under-reporting (e.g., participants might not include abusive experiences when they think of the people with whom they had a sexual experience before age 18; experiences meeting research criteria for CSA might not be considered abusive by participants), both behavioral questions and self-definition questions were used to reduce the possibility of mis-classifying a participant who was sexually abused.
For this study, participants were considered sexually abused if they experienced oral sex, vaginal sex, or anal sex that occurred: (1) when the participant was age 12 or younger and the other individual was 5 or more years older; (2) when the participant was age 16 or younger and the other person was 10 or more years older; or (3) when the participant was age 16 or younger and the other person threatened or forced her, consistent with previous research that has used both age discrepancy and force as CSA criteria (e.g., Briere, Elliott, Harris, & Cotman, 1995; Wyatt, Lawrence, Vodounon, & Mickey, 1992). Participants who reported that they had been sexually abused as a child were also considered to have been sexually abused.
Traumagenic dynamics constructs
The TD constructs were assessed with self-report measures of traumatic sexualization, betrayal/trust, guilt, and powerlessness.
Traumatic sexualization
Traumatic sexualization was assessed with 15 items from the Traumatic Sexualization Survey (Matorin & Lynn, 1998). The original version of the measure included 38 items; for the present study, we retained the items with the highest factor loadings that were not confounded with the sexual behavior outcomes (e.g., “I avoid sexual activity”). Participants indicated on a 5-point scale (0 = never to 4 = almost always) how frequently they feared sex (e.g., “I am afraid of sex”), thought about sex (e.g., “I daydream about sex”), based relationships on sex (e.g., “My relationships with men are based on sex”), and used their sexuality (e.g., “Men want to be with me because I am seductive”). Prior research found that this measure had good internal consistency reliability (all αs ≥ .80) and good test-retest reliability at 3 weeks, with all rs ≥ .82 (Matorin & Lynn, 1998). The subscales were correlated in expected ways with other measures, providing evidence of the measure’s convergent validity.1 In addition, women who were sexually abused scored higher than nonabused women on three of the four subscales, providing further evidence of validity (Matorin & Lynn, 1998).
Because internal consistency reliability on the fear of sex factor was poor in the present sample (α = .51), that scale was not included in the analyses, leaving three factors: (1) thoughts about sex (4 items; α = .89); (2) role of sex in relationships (4 items; α = .80); and (3) use of sexuality (3 items; α = .84). Higher scores on the first factor indicated more frequent sexual thoughts, higher scores on the second factor indicated greater use of sex as the basis for relationships, and higher scores on the third factor indicated greater use of sexuality. Scores on each of the three of the factors ranged from 0 to 4 in the present study.
Betrayal/trust
Trust was assessed with five of eight items from the Dyadic Trust Scale (Larzelere & Huston, 1980). The five items with the highest item-total correlations were included in the present study. Prior research has found this measure has good internal consistency reliability (α = .93). Scores on this measure were positively correlated with scores on measures of love and self-disclosure, and married partners reported greater trust than divorced partners, providing evidence of this measure’s validity (Larzelere & Huston, 1980).
Participants responded on a 7-point scale (1 = strongly disagree to 7 = strongly agree) to items assessing how much they trusted and counted on their partner (e.g., “My partner is perfectly honest and truthful with me”). Women who did not have a main partner were asked to respond to the items based on the sexual partner to whom they felt closest. The five items were averaged, and higher scores indicated greater partner trust (α = .93). Scores ranged from 1 to 7.
Guilt
Participants responded to 8 items from the Revised Mosher Guilt Inventory (Mosher, 1988). This measure was chosen because items assess guilt and shame specifically about sexual behaviors. The revised version of the measure has good internal consistency reliability (α = .95) and is highly correlated (r = .82) with the original version (Janda & Bazemore, 2011). Higher scores on the revised measure were associated with not having had sex, initiating sex at a later age, and having fewer partners, supporting the measure’s validity (Janda & Bazemore, 2011). The revised sex guilt subscale contains 50 items; items for the present study were chosen based on appropriate language (e.g., items referring to “petting” were excluded, because this term is not commonly used) and relevance to the population (e.g., items asking about sexual activity before marriage were excluded, because marriage is not common among the current study population).
Participants indicated on a 7-point scale (0 = not at all true for me; 6 = extremely true for me) how true a series of statements related to sexual desires and practices were (e.g., “Masturbation is not healthy”). Items were averaged, and higher scores indicated greater sexual guilt associated with sexual desires and behaviors (α = .76). Scores in the present study ranged from 0 to 5.6.
Powerlessness
To assess powerlessness, participants responded to 12 items from Levenson’s (1974) Locus of Control Scales (e.g., “My life is chiefly controlled by powerful others”) using a 6-point scale (0 = Strongly Disagree; 5 = Strongly Agree). The original measure included 24 items loading on three scales: powerful others, internal, and chance control. Items with the highest factor loadings were used in the present study. This measure has good internal consistency reliability, with αs ranging from .64 to .78 and one week test-retest reliability, with rs ranging from .64 to .78 (Levenson, 1974). Evidence of validity comes from studies finding that higher scores on the external locus of control scales were associated with depressive symptoms (Wilkinson, 2007) and less involvement in activism-related activities (Levenson, 1974). Further, the scales were positively correlated with the corresponding scales on the Multidimensional Health Locus of Control measure (Wallston, Wallston, & DeVellis, 1978).
In the present study, internal consistency reliability was low for the internal control and chance control scales (α = .34 and .51, respectively); therefore, only the powerful others scale was retained (4 items, α = .75). Items loading on this factor were averaged, and a higher score indicated greater powerlessness. Scores in the present study ranged from 0 to 5.
Information-Motivation-Behavioral Skills constructs
The IMB constructs were assessed with self-report measures of information, motivation, and skills, as well as observational measures of condom application and assertiveness.
Information
Information was assessed with 14 items from the Brief HIV-KQ (Carey, Morrison-Breedy, & Johnson, 1997; Carey & Schroder, 2002) and 5 STI-related items used previously with STI clinic patients (Carey, Senn, Vanable, Coury-Doniger, & Urban, 2010). Prior research has established the internal consistency reliability (αs range from .75 to .89) and 3 month test-retest reliability (rs range from .76 to .88) of the Brief HIV-KQ (Carey & Schroder, 2002). Validity of this measure is evidenced by greater knowledge gains in individuals exposed to a sexual risk reduction intervention, compared to control participants (Carey & Schroder, 2002). The original Brief HIV-KQ includes 18 items; for the present study, items were deleted if more than 90% of participants answered them correctly in a previous study of STI clinic patients (Carey et al., 2010).
Participants were asked to respond “yes,” “no,” or “I don’t know” to a series of HIV and STI questions (e.g., “Does a natural skin condom work better against HIV than a latex condom?”). Correct responses were scored as 1; incorrect or “don’t know” responses were scored as 0. Scores were summed and divided by the total number of items to derive the percentage of correct knowledge items. A higher score indicated more HIV- and STI-related knowledge (α = .66). Scores ranged from 11% to 100% in the present study.
Motivation
Attitudes towards safer sex are one aspect of motivation (Fisher & Fisher, 2000). Motivation to use a condom was assessed with five items adapted from existing scales of condom attitudes (e.g., Brown, 1984; Sacco, Levine, Reed, & Thompson, 1991). Participants rated on a 6-point scale (0 = strongly disagree; 5 = strongly agree) how much they agreed with statements about condom use (e.g., “Sex with a condom can still be pleasurable”). These items have been used previously with STI clinic patients, with adequate internal consistency reliability (α =.70). Participants reported more favorable condom attitudes after participating in a sexual risk reduction intervention, providing evidence of this measure’s validity (Carey et al., 2010). Items were averaged to create a condom attitudes summary score. A higher score indicated more positive condom attitudes (α = .71). Scores ranged from 0.2 to 5.0 in the present study.
Behavioral skills
Behavioral skills were assessed in three ways. First, self-efficacy to engage in safer sex was assessed (Murphy, Stein, Schlenger, Maibach, & National Institute of Mental Health Multisite HIV Prevention Trial Group, 2001). Participants were presented one scenario that involved a steady partner and one scenario that involved a new partner. Participants rated on an 11-point scale (0 = not at all confident; 10 = completely confident) how confident they were that they could engage in a variety of safer sexual behaviors (e.g., convince their partner to use a condom) in response to each scenario. Participants responded to 4 items for each scenario (8 items total). These items were used in prior research with STI clinic patients, with good internal consistency reliability (α = .83) and evidence that participants reported more self-efficacy after participating in a sexual risk reduction intervention (Carey et al., 2010). Scores were averaged across the eight items; higher scores indicated greater safer sex self-efficacy (α = .89). Scores on this measure ranged from 2.1 to 10 in the present study.
Second, condom application skills were assessed with a behavioral simulation (Forsyth, Carey, & Fuqua, 1997). Women were presented with condoms and lubricants and asked to choose what they thought would best protect them from HIV and then to apply their choice to a penis model. The RA observed the participant and scored the participant on 10 condom use skills, which included: opening the package correctly; applying lubricant to the inside tip of the condom; placing the condom on the model right-side up; squeezing the tip of the condom; rolling the condom all the way down to the base of the model; applying lubricant to the outside of the condom; selecting a water-based lubricant; having the condom free of tears or air bubbles; having the condom make contact with the head of the penis model just below the reservoir tip; and selecting a latex condom. In addition, the RA asked the participant six questions about correct condom use (e.g., “When specifically should a condom be applied to the penis?”). All items (the 10 condom application skills items and the 6 correct condom use questions) were scored 0 for an incorrect response and 1 for a correct response. The 16 items were summed to derive a condom application score, with a higher score indicating better skills. Prior research indicates this assessment can be scored reliability (Forsyth et al., 1997). A random sample of 45 participants was double-scored; inter-rater reliability (intraclass correlation) measured .88. In the present study, scores ranged from 1 to 15.
Third, sexual assertiveness was assessed with four role play scenarios that were presented to women on a laptop computer. Women responded to the scenarios and their responses were recorded. The scenarios were based on situations that were commonly reported during formative research and involved: a new partner; a steady partner who was non-monogamous; a child’s father who was not a steady partner; and a resumption of a relationship with a former partner. Each scenario included three prompts to which participants responded. These role play procedures have been used in prior research (Carey et al., 2004; Weinhardt, Carey, Carey, & Verdecias, 1998). Role plays were rated by RAs who were blind to CSA status. Each response was scored 0–2 on five dimensions: refusal of unsafe sex; positive statement about the other person; reason for refusal of unsafe sex; suggestion of an alternative, safer behavior; and assertiveness of the request. A score of 0 indicated low sexual assertiveness, and a score of 2 indicated high sexual assertiveness. Ratings were averaged to derive a total score. Prior research indicates this assessment can be scored reliably (Forsyth et al., 1997). A random sample of 105 role plays was double-scored; inter-rater reliability was adequate (intraclass correlation = .90). In the present study, scores on this measure ranged from 2.2 to 6.2. The three skills measures were uncorrelated (rs ranged from .03 to .07).
Sexual risk behavior
Participants reported the number of male and female sexual partners in their lifetime and in the past 3 months. Participants were asked whether they had a steady partner in the past 3 months, defined as the sexual partner to whom they were closest. Participants were then asked to report the number of condom-protected and the number of unprotected vaginal and anal sex episodes in the past 3 months with a steady partner and with non-steady partner(s). The total number of unprotected sex episodes (vaginal + anal) and the percentage of unprotected sex episodes were calculated based on these responses. These items have been used in previous research with women (e.g., Carey et al., 1997, 2000, 2004,2010). Participants were also asked whether they had ever been treated for an STI.
Data Analysis
We trimmed outliers (observations > 3 × the interquartile range (IQR) from the 75th percentile were trimmed to 3 × IQR from the 75th percentile + 1). Non-normally distributed outcome variables (i.e., number of 3 month partners and number of episodes of unprotected sex) were transformed using a log10 transformation. Linear regression analyses were conducted to determine whether CSA was associated with the recent risk behavior outcomes.
Next, we conducted a series of analyses to test possible mediators of the CSA/sexual risk behavior relation. Mplus (Muthen & Muthen, 1998–2007) was used to conduct bootstrapped mediation analyses with 5000 resamples. Consistent with recommendations in Preacher and Hayes (2008), we first tested each of the IMB and TD variables separately, to determine whether they independently mediated the CSA/sexual risk behavior relation. Second, we conducted analyses with: (1) all of the IMB variables as mediators and (2) all of the TD variables as mediators, to determine whether the total indirect effect through the multiple mediators in each model was significant. Finally, we conducted analyses with the IMB and TD variables included as mediators in the same model to compare the combined indirect effect through the IMB constructs and the TD constructs. The meditational paths associated with each set of constructs were summed and compared (Preacher & Hayes, 2008).
RESULTS
Rates of Adult Sexual Risk Behavior and CSA
Participants reported an average of 22.4 (SD = 23.2; median = 13) lifetime sexual partners and 2.1 (SD = 1.8; median = 1) sexual partners in the past 3 months. They also reported an average of 17.6 (SD = 22.1; median = 9) episodes of unprotected sex in the past 3 months. On average, 66% (SD = 34%) of the reported episodes of vaginal and anal sex were unprotected. The majority of participants (84%; n = 397) reported ever being treated for an STI.
Forty-five percent of the sample (n = 214) reported CSA. The 214 participants who were sexually abused reported 417 CSA experiences with different individuals; 50% of those who were abused reported a CSA experience with more than one person. Among those meeting criteria for CSA, 110 (51%) met the research criteria and self-defined as sexually abused, 58 (27%) met the research criteria but did not self-define as sexually abused, and 46 (21%) self-defined as abused but did not meet research criteria.
Among those who were sexually abused, 335 (81%) of experiences involved fondling, 182 (44%) involved oral sex, and 302 (73%) involved vaginal or anal sex. The majority of experiences (n = 295; 71%) involved threat or force. Slightly more than one-quarter of experiences (n = 117) consisted of a single event; 13% of experiences (n = 53) lasted less than one month; 31% of experiences (n = 128) lasted more than one month but less than one year; and 28% of experiences (n = 116) lasted for one year or longer. The median participant age at the time of the experience was 12.0 years; the median age of the other person was 24.0 years. Most experiences were with a non-relative, including 53 (13%) who reported the experience involved a stranger, 49 (12%) who reported the experience involved a boyfriend or girlfriend, and 196 (47%) who reported the experience involved a person they knew, a friend, or an authority figure. Eleven percent (n = 46) of experiences involved a parent or stepparent, and 17% (n = 70) of experiences involved another relative such as a niece or nephew, cousin, brother or sister, aunt or uncle, or grandparent.
Preliminary Analyses
Compared to women without a history of CSA, women who experienced CSA were more likely to be unemployed, χ2(1, N = 478) = 6.34, p < .05 (55% vs. 44%), to have an income less than $15,000/year, χ2(1, N = 469) = 5.24, p < .05 (62% vs. 51%), and to be older, t(1, 476) = −2.86, p < .01 (28.7 vs. 26.4 years). These variables were controlled for in mediation analyses (i.e., paths from each of the covariates to the dependent variable and from each of the covariates to each of the mediators were included).
We also conducted analyses to determine which demographic variables were related to the sexual risk variables (past 3 months). A greater number of partners was associated with being Caucasian, t(471) = 2.37, p < .05, being unemployed, t(473) = −2.36, p < .05, and earning <$15,000/year, t(465) = −3.85, p < .001. Having fewer episodes of unprotected sex was associated with having an outside (i.e., non-steady) partner, t(470) = 4.22, p < .0001. A greater proportion of episodes of unprotected sex was associated with being older, F(1, 465) = 7.00, p < .01; a smaller proportion of episodes of unprotected sex was associated with having an outside (i.e., non-steady) partner, t(465) = 4.84, p < .0001. These variables were controlled for in subsequent relevant analyses.
Relation between CSA and Adult Sexual Risk Behavior
After controlling for covariates, CSA was associated with more episodes of unprotected sex in the past 3 months, F(1, 458) = 17.48, p < .0001, and a greater proportion of episodes of unprotected sex in the past 3 months, F(1, 453) = 8.64, p < .01. CSA was unrelated to the number of partners in the past 3 months.2 Sexual behavior averages for CSA and non-CSA participants are reported in Table 1.
Table 1.
Sexual Risk Behavior, TD Constructs, IMB Constructs, and Substance Use by Childhood Sexual Abuse Group
| Variable | Childhood Sexual Abuse | No Childhood Sexual Abuse | p | η2 |
|---|---|---|---|---|
| M (SD) | M (SD) | |||
| Partners, 3 months (number) a | 2.2 (1.9) | 2.0 (1.7) | ns | |
| Unprotected Sex (number) b | 21.5 (24.6) | 14.3 (19.1) | <.0001 | .04 |
| Unprotected Sex (%) b | 71% (32%) | 61% (36%) | <.01 | .02 |
| Traumatic sexualization: thoughts about sex | 1.6 (1.0) | 1.4 (0.9) | <.01 | .02 |
| Traumatic sexualization: role of sex in relationships | 1.2 (1.0) | 0.8 (0.8) | <.001 | .93 |
| Traumatic sexualization: use of sexuality | 1.4 (1.1) | 1.1 (1.0) | < .05 | .01 |
| Trust | 3.8 (1.8) | 3.3 (1.6) | <.01 | .01 |
| Sex guilt | 2.1 (1.2) | 2.6 (1.3) | <.001 | .03 |
| Powerlessness | 1.4 (1.2) | 1.2 (1.0) | <.05 | .01 |
| Knowledge (percent correct) | 76.3 (15.4) | 73.2 (15.7) | <.01 | .01 |
| Condom attitudes | 3.7 (1.0) | 3.9 (0.9) | <.05 | .01 |
| Self-efficacy | 8.6 (1.7) | 8.9 (1.6) | ns | |
| Condom application skills | 9.5 (1.9) | 9.1 (1.8) | <.05 | .01 |
| Sexual assertiveness skills | 4.4 (0.6) | 4.4 (0.6) | ns |
Note: TD = traumagenic dynamics; IMB = information-motivation-behavioral skills. All analyses controlled for employment, income, and age.
Analyses also controlled for race.
Analyses also controlled for whether or not participant had a non-steady partner.
Relation between CSA and Proposed Mediators
After controlling for covariates, CSA was associated with all of the traumagenic dynamics constructs. CSA was associated with greater traumatic sexualization on the thoughts about sex subscale, F(1, 455) = 7.40, p < .01, the role of sex in relationships subscale, F(1, 455) = 16.59, p < .0001, and the use of sexuality subscale, F(1,455) = 5.44, p < .05. CSA was also associated with greater trust of a partner, F(1, 455) = 7.06, p < .01 and greater powerlessness, F(1,454) = 4.61, p < .05. CSA was associated with less sexual guilt, F(1, 455) = 15.19, p < .001.
After controlling for covariates, CSA was also associated with several of the IMB constructs. CSA was associated with more HIV-related knowledge, F(1, 458) = 6.77, p < .01, less positive condom attitudes, F(1, 455) = 6.28, p < .05, and greater condom application skills, F(1, 456) = 4.63, p < .05. CSA was not associated with self-efficacy or with sexual assertiveness skills. Average scores on each of the constructs, by CSA group, are presented in Table 1.
Mediators of the CSA and Adult Sexual Risk Behavior Relation
As displayed in Table 2, we initially conducted single mediation models for each of the three dependent variables. The relation between CSA and the number of partners (past 3 months) was mediated by traumatic sexualization (sexual thoughts, role of sex in relationships, and use of sexuality) and sex guilt. Individuals who were sexually abused reported more traumatic sexualization (sexual thoughts, role of sex in relationships, and use of sexuality) and less sexual guilt. Each of these variables was, in turn, associated with a greater number of partners in the past 3 months.
Table 2.
Significant Mediators of the CSA/Sexual Risk Behavior Relation
| Mediator | Standardized Parameter Estimate, CSA to mediator | Standardized Parameter Estimate, mediator to outcome | Bootstrapped 95% CI for the Indirect Effect |
|---|---|---|---|
| Outcome = Number of Partners | |||
| Traumatic sexualization: thoughts about sex | 0.13 | 0.19 | .002, .019 |
| Traumatic sexualization: role of sex in relationships | 0.20 | 0.35 | .013, .042 |
| Traumatic sexualization: use of sexuality | 0.11 | 0.33 | .002, .027 |
| Guilt | −0.18 | −0.15 | .003, .020 |
| Outcome = Number of Episodes of Unprotected Sex | |||
| Motivation | −0.12 | −0.18 | .003, .044 |
| Guilt | −0.18 | −0.11 | .002, .043 |
| Outcome = Proportion of Episodes of Unprotected Sex | |||
| Motivation | −0.12 | −0.17 | .002, .029 |
Note: CI = confidence interval. Results reported are from individual mediator models.
Table 2 (panel b) shows that motivation and sex guilt mediated the relation between CSA and the number of episodes of unprotected sex (3 months). Individuals who were sexually abused had less positive condom attitudes and less sexual guilt; less positive attitudes and less sexual guilt were, in turn, both associated with more episodes of unprotected sex.
Motivation mediated the relation between CSA and the proportion of episodes of unprotected sex in the past 3 months. Individuals who were sexually abused had less positive condom attitudes; less positive condom attitudes were, in turn, associated with a greater proportion of episodes of unprotected sex (Table 2, panel c).
Multiple Mediators of the Relation Between CSA and Adult Sexual Risk Behavior
We conducted multiple mediator analyses to determine whether the IMB constructs combined and the TD constructs combined mediated the relation between CSA and sexual risk behavior in adulthood. The TD constructs mediated the relation between CSA and the number of sexual partners in the past 3 months (see Table 3). The IMB constructs combined did not mediate the relation between CSA and the number of partners.
Table 3.
Sum of the Indirect Effects through the Information-Motivation-Behavioral Skills Model Constructs, the Traumagenic Dynamics Constructs, and Substance Use Constructs
| Mediator | Standardized Estimate | SE | Bootstrapped 95% CI for the Indirect Effect |
|---|---|---|---|
| Outcome = Number of Partners | |||
| Sum of IMB Constructs | .006 | .012 | −.007, .011 |
| Sum of TD Constructs | .072 | .022 | .011, .044 |
| Outcome = Number of Episodes of Unprotected Sex | |||
| Sum of IMB Constructs | .043 | .016 | .015, .080 |
| Sum of TD Constructs | .019 | .014 | −.008, .052 |
| Outcome = Proportion of Episodes Unprotected Sex | |||
| Sum of IMB Constructs | .034 | .015 | .005, .045 |
| Sum of TD Constructs | .012 | .014 | −.011, .028 |
Note: CI = confidence interval; IMB = information, motivation, behavioral skills; TD = traumagenic dynamics.
In contrast, the IMB constructs mediated the relation between CSA and the number of episodes of unprotected sex, as well as the relation between CSA and the proportion of episodes of unprotected sex. The TD constructs did not mediate these relations.
Comparing the Strength of the Indirect Effects through the IMB Constructs and the TD Constructs
We conducted analyses including all hypothesized mediators in a single model, to compare the relative strength of the indirect effects through each set of constructs (i.e., IMB and TD). That is, for each of the three outcomes, we conducted one contrast that evaluated the indirect effects through IMB constructs–indirect effects through TD constructs.
For the number of partners (past 3 months), the contrast was significant and negative, CI.95 = [−.058, −.018], indicating that the indirect effects through the TD constructs were greater than the indirect effects through the IMB constructs. For the number of episodes of unprotected sex (past 3 months), the contrast was nonsignificant, CI.95 = [−.003, .101], indicating that the indirect effects through the IMB constructs did not differ from the indirect effects through the TD constructs. For the proportion of episodes of unprotected sex (past 3 months), the contrast was again nonsignificant, CI.95 = [.000, .071], indicating that the indirect effects through the IMB constructs did not differ from the indirect effects through the TD constructs.
DISCUSSION
The women recruited for this study–mostly urban, socially- and economically-disadvantaged, young adult women–reported high rates of both CSA and sexual risk behavior. The high levels of sexual risk behavior reflect, in part, the fact that women were recruited from an STI clinic; patients attending STI clinics report higher than average rates of sexual risk behavior (Satterwhite et al., 2007). The rate of CSA reported by women in this study (45%) is considerably higher than rates of CSA reported by women in national samples, which range from 15% to 32% (Briere & Elliott, 2003; Vogeltanz et al., 1999). However, these high rates of CSA are consistent with rates reported in other studies of women attending STI clinics, which range from 38% to 53% (NIMH Multisite Prevention Trial Group, 2001; Senn et al., 2006).
Corroborating findings from previous studies, we found that women who reported sexual abuse in childhood or adolescence reported more sexual risk behavior in adulthood (Senn et al., 2008). Uniquely, however, we investigated mediators of this relation using two prominent theories, one of health behavior (i.e., the IMB model) and one of CSA effects (i.e., traumagenic dynamics). We also directly compared the indirect effects suggested by the competing models.
Our results show that the mediators of the CSA/sexual behavior relation differed depending on the risk behavior being investigated. TD constructs (traumatic sexualization and guilt) mediated the relation between CSA and the number of sexual partners. As suggested by the TD model, CSA was associated with greater traumatic sexualization, which, in turn, was associated with more partners. The concept of traumatic sexualization suggests that individuals who are sexually abused may be reinforced with attention, affection, and possibly material gifts for their sexual behavior; thus, they may learn to use sex to obtain affection or other needs, which may lead them to have more partners.
Contrary to what was predicted based on the TD model, CSA was associated with less sexual guilt. Perhaps CSA experiences are perceived as non-normative and stigmatizing whereas adult sexual experiences are seen as normative. Therefore, women who experienced CSA may have reported less sexual guilt than women who were not sexually abused. Individuals who experienced less sexual guilt, in turn, reported more partners in the past 3 months. Alternatively, it is possible that having more sexual partners leads to less sexual guilt, a hypothesis that merits further investigation in a longitudinal study.
Contrary to our hypotheses, CSA was associated with more, rather than less, trust of a sexual partner. This finding is in contrast to results from previous research, which has found CSA is associated with less partner trust (DiLillo & Long, 1999; Mullen et al., 1994). One possible explanation for these contradictory findings is that sexual abuse by a caregiver may lead to insecure attachment (Briere, 2002; Cicchetti & Toth, 2005), resulting in difficulty trusting others (Fraley & Shaver, 2000). However, if someone other than a caregiver is the abuser, there may be less disruption in attachment, and these individuals may have less trouble trusting others. In this study, only 11% of participants reported abuse by a parent or stepparent. In addition, because abusers often lie or distort reality (Zurbriggen & Freyd, 2004), women who were sexually abused as children may have difficulty judging who is trustworthy, or may have a low threshold for deciding someone is trustworthy and can be counted on. Further research is needed to better understand these inconsistent findings.
In contrast to the importance of most of the TD constructs in mediating the relation between CSA and the number of recent sexual partners, few of the TD constructs mediated the relation between CSA and unprotected sex. The exception was sex guilt, which mediated the relation between CSA and the number of episodes of unprotected sex. As mentioned earlier, CSA was associated with less sexual guilt. It is possible that many individuals feel guilt after engaging in unprotected sex because they realize the possibility of disease or unintended pregnancy; this guilt may make them less likely to engage in unprotected sex. Individuals who feel less of this guilt after unprotected sex may engage in more episodes of unprotected sex.
The IMB construct of motivation (to use a condom) mediated the relation between CSA and both the number and proportion of episodes of unprotected sex. Women who were sexually abused had less positive condom attitudes. As predicted by the IMB model, less positive condom attitudes were, in turn, associated with less condom use. There are several possible explanations for the association between CSA and less positive condom attitudes. Women who were sexually abused may be unable to accurately assess the reality of their risk in sexual situations because reality was distorted by their abuser (Zurbriggen & Freyd, 2004); if they do not believe they are at risk, they may not see a need to use a condom and thus have less positive condom attitudes. Alternatively, perhaps women who were sexually abused and who as adults base their relationships on sex and use sex to obtain affection (Matorin & Lynn, 1998) are more likely to internalize a partner’s negative attitudes towards condoms (Maxwell & Boyle, 1995), or to view condoms as a barrier to their primary method of obtaining intimacy (Corbett, Dickson-Gómez, Hilario, & Weeks, 2009). Qualitative research is needed to better understand why women who were sexually abused have more negative condom attitudes than women who were not abused.
HIV-related knowledge did not mediate the association between CSA and sexual risk behavior; however, an unexpected finding was that, CSA was associated with greater HIV knowledge. It may be that because women who were sexually abused as children generally had quite early initial sexual experiences, they also began learning sexual and HIV-related information at an earlier age. Alternatively, women who were sexually abused are more likely to have ever been diagnosed with an STI (Senn et al., 2006); contact with healthcare providers that occurs during STI testing and treatment may have provided these women with additional HIV-related knowledge.
Consistent with the results from the individual mediator models, the TD constructs as a whole were better mediators of the relation between CSA and the number of partners; however, the IMB constructs as a whole did not differ from the TD constructs as a whole as mediators of the relation between CSA and the number and proportion of episodes of unprotected sex. Other studies have found different mediators of the CSA/adult sexual risk behavior relation, depending on the sexual risk behavior outcome being studied (e.g., Senn et al., 2006). These results suggest that different sexual risk behaviors may have different underlying causes and that it is important to study sexual risk behaviors separately rather than creating composite indicators of sexual risk behavior (c.f. Susser, Desvarieux, & Wittkowski, 1998).
Study strengths include a large and diverse sample of women who reported CSA, use of ACASI to obtain more valid self-reports about sensitive topics and behaviors (Des Jarlais et al., 1999; Metzger et al., 2000), use of both behaviorally specific questions as well as a question allowing participants to self-define as sexually abused to reduce under-reporting, role playing testing of behavioral skills, use of theory to determine constructs for model testing, and direct comparison of competing theories (Fisher & Fisher, 2000; Noar & Zimmerman, 2005).
Study limitations should also be acknowledged. First, there is no consensus on the definition of CSA (Haugaard, 2000); the definition we used (i.e., childhood and adolescent sexual experiences that were age-discrepant or involved force, as well as individuals who self-defined as sexually abused) is consistent with previous research (see Hulme, 2004 for a review of CSA definitions). There were some differences between (1) participants who self-defined as sexually abused but did not meet research criteria for CSA and (2) participants who met research criteria and self-defined; these differences emerged on traumatic sexualization scores and number of lifetime partners, with those who only self-defined having lower scores on these measures. A trade-off of the decision to be maximally inclusive (i.e., including all types of CSA, including less severe experiences) is likely an attenuation of the strength of the meditational associations we investigated. In addition, we limited the number of people with whom participants could report a childhood sexual experience to 10 in order to reduce response burden; however, participants who had childhood sexual experiences with more than 10 people may have been mis-classified as non-abused.
Second, there are no reliability or validity data on the measure of CSA used in the present study. As with any self-report of behavior, responses to both CSA and sexual risk behavior questions may have been biased, due to self-presentation or recall error (c.f. Schroder, Carey, & Vanable, 2003). Given the sensitive nature of both of these topics, participants may have under-reported these behaviors, although use of ACASI has been shown to minimize this under-reporting (Des Jarlais et al., 1999; Metzger et al., 2000). In addition, participants may have had difficulty remembering their childhood sexual experiences, because of the amount of time that elapsed between those experiences and the survey, and may also have had difficulty remembering their sexual behavior in the past 3 months. However, a 3-month recall period has been recommended for sexual behavior surveys, because it allows sufficient time for variability in sexual behavior and results in the most reliable sexual behavior data (Napper, Fisher, Reynolds, & Johnson, 2010).
Third, our design was cross-sectional; although use of a longitudinal design would help to better assess the temporal relations among CSA, mediators, and sexual risk behavior, such a design presents many logistical challenges and is probably infeasible. Fourth, the research was conducted with a low-income sample of women recruited from an STI clinic who reported high rates of sexual risk behavior. This is an important group to study because they are at high risk for HIV and other STIs. However, because of the at-risk nature of the sample, the results may not generalize to all women who have experienced CSA. Research is also needed to study mediators of the CSA/sexual risk behavior relation with men. Fifth, several of the measures had low internal consistency reliability in this sample, which could have reduced the power to detect effects. Sixth, we did not ask whether women were sexually assaulted in adulthood. Sexual victimization in adulthood is associated with being sexually abused as a child (Classen, Palesh, & Aggarwal, 2005; Roodman & Clum, 2001), and individuals who report both CSA and later sexual revictimization report higher rates of sexual risk behavior than those who report only one of these risk factors (Arata, 2000; Miner, Flitter, & Robinson, 2006). Thus, by not investigating or controlling for adult sexual assault, we may have over-estimated the impact of CSA on sexual risk behavior in adulthood. Seventh, we did not include a measure of CSA severity. Additional research is needed to investigate how the severity of the CSA impacts the meditational relationships found in this study. Finally, the effect sizes we found in this study were small.
Our findings have important clinical implications for the design of sexual risk reduction interventions. It is important to recognize that, depending on the clinical setting, a significant percentage of individuals may have been sexually abused as children and that this experience may have long-lasting effects on sexual behavior. Because individuals who were sexually abused report high rates of sexual risk behavior in comparison to non-abused individuals, it is important to develop targeted sexual risk reduction interventions for these individuals.
Unfortunately, few sexual risk reduction interventions have been developed to address the unique needs and sexual risk determinants of women who were sexually abused, with the exception of a few interventions focused on women who are HIV positive (Sikkema et al., 2008; Wyatt et al., 2004). Our findings provide guidance for those who wish to develop sexual risk reduction interventions for women who were sexually abused as children. For these women, it is important to address the usual determinants of risk targeted in sexual risk reduction interventions, such as motivation and behavioral skills; however, it also appears important to address determinants that are specific to sexual abuse, such as traumatic sexualization and guilt. Indeed, given the central role that partner concurrency may play in STI/HIV transmission (Mah & Halperin, 2010; Morris, Kurth, Hamilton, Moody, & Wakefield, 2009), our findings that the TD constructs mediated the relation between CSA and the number of recent sexual partners suggests that targeting these constructs may be particularly important in reducing STI and HIV rates. Further research is critically needed to develop and evaluate sexual risk reduction interventions for women with a history of CSA.
Acknowledgments
This research was supported by grant R21MH083502 from the National Institute of Mental Health.
Footnotes
For example, the fear of sex subscale was negatively correlated with a measure of dysfunctional sexual behavior; the thoughts about sex subscale was negatively correlated with measures of sexual self-esteem and sex guilt; the basing relationships on sex subscale was positively correlated with dysfunctional sexual behavior; and the subscale assessing use of sexuality was negatively correlated with sexual guilt and positively correlated with dysfunctional sexual behavior (Matorin & Lynn, 1998).
Although Baron and Kenny (1986) initially proposed that a significant relation between the independent and dependent variables was a necessary prerequisite for testing mediation, more recent writings suggest that this criterion be relaxed because this requirement greatly reduces the power to detect a mediated effect (MacKinnon, Fairchild, & Fritz, 2007). Therefore, we included number of partners in the past 3 months as an outcome in the mediation analyses.
References
- Arata CM. From child victim to adult victim: A model for predicting sexual revictimization. Child Maltreatment. 2000;5:28–38. doi: 10.1177/1077559500005001004. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological reserach: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bolger KE, Patterson CJ. Pathways from child maltreatment to internalizing problems: Perceptions of control as mediators and moderators. Development and Psychopathology. 2001;13:913–940. [PubMed] [Google Scholar]
- Bolstad BR, Zinbarg RE. Sexual victimization, generalized perception of control, and posttraumatic stress disorder symptom severity. Journal of Anxiety Disorders. 1997;11:523–540. doi: 10.1016/s0887-6185(97)00028-5. [DOI] [PubMed] [Google Scholar]
- Boyer CB, Shafer M, Wibbelsman CJ, Seeberg D, Teitle E, Lovell N. Associations of sociodemographic, psychosocial, and behavioral factors with sexual risk and sexually transmitted diseases in teen clinic patients. Journal of Adolescent Health. 2000;27:102–111. doi: 10.1016/s1054-139x(99)00113-5. [DOI] [PubMed] [Google Scholar]
- Briere J. Treating adult survivors of severe childhood abuse and neglect: Further development of an integrative model. In: Myers JEB, Berliner L, Briere J, Hendrix CT, Jenny C, Reid TA, editors. The APSAC handbook on child maltreatment. 2. Thousand Oaks, CA: Sage Publications; 2002. pp. 175–203. [Google Scholar]
- Briere J, Elliott DM. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse and Neglect. 2003;27:1205–1222. doi: 10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Briere J, Elliott DM, Harris K, Cotman A. Tr ma Symptom Inventory: Psychometrics and association with childhood and adult victimization in clinical samples. Journal of Interpersonal Violence. 1995;10:387–401. [Google Scholar]
- Brown IS. Development of a scale to measure attitude toward the condom as a method of birth control. The Journal of Sex Research. 1984;20:255–263. [Google Scholar]
- Brown LK, Kessel SM, Lourie KJ, Ford HH, Lipsitt LP. Influence of sexual abuse on HIV-related attitudes and behaviors in adolescent psychiatric inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:316–322. doi: 10.1097/00004583-199703000-00009. [DOI] [PubMed] [Google Scholar]
- Brown LK, Lourie KJ, Zlotnick C, Cohn J. Impact of sexual abuse on the HIV-risk-related behavior of adolescents in intensive psychiatric treatment. American Journal of Psychiatry. 2000;157:1413–1415. doi: 10.1176/appi.ajp.157.9.1413. [DOI] [PubMed] [Google Scholar]
- Carey MP, Braaten LS, Maisto SA, Gleason JR, Forsyth AD, Durant LE, Jaworski BC. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: A second randomized clinical trial. Health Psychology. 2000;19:3–11. doi: 10.1037//0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, Schroder KEE, Vanable PA. Reducing HIV-risk behavior among adults receiving outpatient psychiatric treatment: Results from a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2004;72:252–268. doi: 10.1037/0022-006X.72.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Morrison-Breedy D, Johnson BT. The HIV-knowledge questionnaire: Development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS and Behavior. 1997;1:61–74. [Google Scholar]
- Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Education and Prevention. 2002;14:172–182. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Senn TE, Vanable PA, Coury-Doniger P, Urban MA. Brief and intensive behavioral interventions to promote sexual risk reduction among STD clinic patients: Results from a randomized controlled trial. AIDS and Behavior. 2010;14:504–517. doi: 10.1007/s10461-009-9587-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance. Atlanta, GA: Author; 2008. [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Classen CC, Palesh OG, Aggarwal R. Sexual revictimization: A review of the empirical literature. Trauma, Violence, and Abuse. 2005;6:103–129. doi: 10.1177/1524838005275087. [DOI] [PubMed] [Google Scholar]
- Coffey P, Leitenberg H, Henning K, Turner T, Bennett RT. Mediators of the long-term impact of child sexual abuse: perceived stigma, betrayal, powerlessness, and self-blame. Child Abuse and Neglect. 1996;20:447–455. doi: 10.1016/0145-2134(96)00019-1. [DOI] [PubMed] [Google Scholar]
- Cohen M, Deamant C, Barkan S, Richardson J, Young M, Holman S, Melnick S. Domestic violence and childhood sexual abuse in HIV-infected women and women at risk for HIV. American Journal of Public Health. 2000;90:560–565. doi: 10.2105/ajph.90.4.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett AM, Dickson-Gómez J, Hilario H, Weeks MR. A little thing called love: Condom use in high-risk primary heterosexual relationships. Perspectives on Sexual and Reproductive Health. 2009;41:218–224. doi: 10.1363/4121809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Paone D, Milliken J, Turner CF, Miller H, Gribble J, Friedman SR. Audio-computer interviewing to measure risk behavior for HIV among injecting drug users: A quasi-randomized trial. Lancet. 1999;353:1657–1671. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- DiIorio C, Hartwell T, Hansen N. Childhood sexual abuse and risk behaviors among men at high risk for HIV infection. American Journal of Public Health. 2002;92:214–219. doi: 10.2105/ajph.92.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiLillo D, Long PJ. Perceptions of couple functioning among female survivors of child sexual abuse. Journal of Child Sexual Abuse. 1999;7:59–76. [Google Scholar]
- Feiring C, Coates DL, Taska LS. Ethnic status, stigmatization, support, and symptoms development following sexual abuse. Journal of Interpersonal Violence. 2001;16:1307–1329. [Google Scholar]
- Finkelhor D. Sexually victimized children. New York: The Free Press; 1979. [Google Scholar]
- Finkelhor D, Browne A. The traumatic impact of child sexual abuse: A conceptualization. American Journal of Orthopsychiatry. 1985;55:530–541. doi: 10.1111/j.1939-0025.1985.tb02703.x. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. New York: Kluwer Academic/Plenum Publishers; 2000. pp. XXX–XXX. [Google Scholar]
- Fisher JD, Fisher WA, Shuper PA. The Information-Motivation-Behavioral Skills model of HIV preventive behavior. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research. San Francisco: Jossey-Bass; 2009. pp. XXX–XXX. [Google Scholar]
- Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: The contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sexually Trasmitted Infections. 1999;75:3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsyth AD, Carey MP, Fuqua RW. Evaluation of the validity of the condom use self-efficacy scale (CUSES) in young men using two behavioral simulations. Health Psychology. 1997;16:175–178. doi: 10.1037//0278-6133.16.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley RC, Shaver PR. Adult romantic attachment: Theoretical developments, emerging controversies, and unanswered questions. Review of General Psychology. 2000;4:132–154. [Google Scholar]
- Freyd JJ, Martorello SR, Alvarado JS, Hayes AF, Christman JC. Cognitive environments and dissociative tendencies: Performance on the standard Stroop task for high versus low dissociators. Applied Cognitive Psychology. 1998;12:S91–S103. [Google Scholar]
- Gibson LE, Leitenberg H. The impact of child sexual abuse and stigma on methods of coping with sexual assault among undergraduate women. Child Abuse and Neglect. 2001;25:1343–1361. doi: 10.1016/s0145-2134(01)00279-4. [DOI] [PubMed] [Google Scholar]
- Gwandure C. Sexual assault in childhood: Risk HIV and AIDS behaviours in adulthood. AIDS Care. 2007;19:1313–1315. doi: 10.1080/09540120701426508. [DOI] [PubMed] [Google Scholar]
- Hall T, Hogben M, Carlton AL, Liddon N, Koumans EH. Attitudes towards using condoms and condom use: Differences between sexually abused and nonabused African American female adolescents. Behavioral Medicine. 2008;34:45–52. doi: 10.3200/BMED.34.2.45-54. [DOI] [PubMed] [Google Scholar]
- Haugaard JJ. The challenge of defining child sexual abuse. American Psychologist. 2000;55:1036–1039. [PubMed] [Google Scholar]
- Hazzard A. Trauma-related beliefs as mediators of sexual abuse impact in adult women survivors: A pilot study. Journal of Child Sexual Abuse. 1993;2:55–69. [Google Scholar]
- Hulme PA. Retrospective measurement of childhood sexual abuse: A review of instruments. Child Maltreatment. 2004;9:201–217. doi: 10.1177/1077559504264264. [DOI] [PubMed] [Google Scholar]
- Janda LH, Bazemore SD. The Revised Mosher Sex-Guilt Scale: Its psychometric properties and a proposed ten-item version. Journal of Sex Research. 2011;48:392–396. doi: 10.1080/00224499.2010.482216. [DOI] [PubMed] [Google Scholar]
- Johnsen LW, Harlow LL. Childhood sexual abuse linked with adult substance use, victimization, and AIDS-risk. AIDS Education and Prevention. 1996;8:44–57. [PubMed] [Google Scholar]
- Johnson BT, Carey MP, Chaudoir SR, Reid AE. Sexual risk reduction for persons living with HIV: Research synthesis of randomized controlled trials, 1993 to 2004. Journal of Acquired Immune Deficiency Syndromes. 2006;41:642–650. doi: 10.1097/01.qai.0000194495.15309.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallstrom-Fuqua AC, Weston R, Marshall LL. Childhood and adolescent sexual abuse of community women: Mediated effects on psychological distress and social relationships. Journal of Consulting and Clinical Psychology. 2004;72:980–992. doi: 10.1037/0022-006X.72.6.980. [DOI] [PubMed] [Google Scholar]
- Larzelere RE, Huston TL. The dyadic trust scale: Toward understanding interpersonal trust in close relationships. Journal of Marriage and the Family. 1980;42:595–604. [Google Scholar]
- Levenson H. Activism and powerful others: Distinctions within the concept of internal-external control. Journal of Personality Assessment. 1974;38:377–383. [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mah TL, Halperin DT. Concurrent sexual partnerships and the HIV epidemics in Africa: Evidence to move forward. AIDS and Behavior. 2010;14:11–16. doi: 10.1007/s10461-008-9433-x. [DOI] [PubMed] [Google Scholar]
- Malow R, Dévieux J, Lucenko BA. History of childhood sexual abuse as a risk factor for HIV risk behavior. Journal of Psychological Trauma. 2006;5:13–32. [Google Scholar]
- Matorin AI, Lynn SJ. The development of a measure of correlates of child sexual abuse: The traumatic sexualization survey. Journal of Traumatic Stress. 1998;11:261–280. doi: 10.1023/A:1024499019860. [DOI] [PubMed] [Google Scholar]
- Maxwell C, Boyle M. Risky heterosexual practices amongst women over 30: Gender, power and long term relationships. AIDS Care. 1995;7:277–293. doi: 10.1080/09540129550126515. [DOI] [PubMed] [Google Scholar]
- Metzger DS, Koblin B, Turner CF, Navaline H, Valenti F, Holte S, Seage GR. Randomized controlled trial of audio computer-assisted self-interviewing: Utility and acceptability in longitudinal studies. American Journal of Epidemiology. 2000;152:99–106. doi: 10.1093/aje/152.2.99. [DOI] [PubMed] [Google Scholar]
- Miller M. A model to explain the relationship between sexual abuse and HIV risk among women. AIDS Care. 1999;11:3–20. doi: 10.1080/09540129948162. [DOI] [PubMed] [Google Scholar]
- Miner MH, Flitter JMK, Robinson BE. Association of sexual revictimization with sexuality and psychological function. Journal of Interpersonal Violence. 2006;21:503–524. doi: 10.1177/0886260505285913. [DOI] [PubMed] [Google Scholar]
- Morris M, Kurth AE, Hamilton DT, Moody J, Wakefield S. Concurrent partnerships and HIV prevalence disparities by race: Linking science and public health practice. American Journal of Public Health. 2009;99:1023–1031. doi: 10.2105/AJPH.2008.147835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher DL. Revised Mosher Guilt Inventory. In: Davis CM, Yarber WL, Davis SL, editors. Sexuality related measures: A compendium. Lake Mills, IA: Graphic Publishing Company; 1988. pp. 152–155. [Google Scholar]
- Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP. The effect of child sexual abuse on social, interpersonal and sexual function in adult life. British Journal of Psychiatry. 1994;165:35–47. doi: 10.1192/bjp.165.1.35. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Stein JA, Schlenger W, Maibach E National Institute of Mental Health Multisite HIV Prevention Trial Group. Conceptualizing the multidimensional nature of self-efficacy: Assessment of situational context and level of behavioral challenge to maintain safer sex. Health Psychology. 2001;20:281–290. [PubMed] [Google Scholar]
- Mustanski B, Donenberg G, Emerson E. I can use a condom, I just don’t: The importance of motivation to prevent HIV in adolescent seeking psychiatric care. AIDS and Behavior. 2006;10:753–762. doi: 10.1007/s10461-006-9098-2. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user’s guide. 5. Los Angeles, CA: Muthen & Muthen; 1998–2007. [Google Scholar]
- Napper LE, Fisher DG, Reynolds GL, Johnson ME. HIV risk behavior self-report reliability at different recall periods. AIDS and Behavior. 2010;14:152–161. doi: 10.1007/s10461-009-9575-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIMH Multisite Prevention Trial Group. A test of factors mediating the relationship between unwanted sexual activity during childhood and risky sexual practices among women enrolled in the NIMH Multisite HIV Prevention Trial. Women’s Work, Health and Quality of Life. 2001;33:163–180. doi: 10.1300/j013v33n01_10. [DOI] [PubMed] [Google Scholar]
- Noar SM, Zimmerman RS. Health Behavior Theory and cumulative knowledge regarding behaviors: Are we moving in the right direction? Health Education Research. 2005;20:275–290. doi: 10.1093/her/cyg113. [DOI] [PubMed] [Google Scholar]
- Noll JG, Horowitz LA, Bonanno GA, Trickett PK, Putnam FW. Revictimization and self-harm in females who experienced childhood sexual abuse: Results from a prospective study. Journal of Interpersonal Violence. 2003;18:1452–1471. doi: 10.1177/0886260503258035. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Malow RM, Dolezal C, Carballo-Dieguez A. Sexual abuse of boys: Short- and long-term associations and implications for HIV prevention. In: Koenig LJ, Doll LS, O’Leary A, Pequegnat W, editors. From child sexual abuse to adult sexual risk: trauma, revictimization, and intervention. Washington, DC: American Psychological Association; 2004. pp. 93–114. [Google Scholar]
- Robertson AA, Stein JA, Baird-Thomas C. Gender differences in the prediction of condom use among incarcerated juvenile offenders: Testing the information-motivation-behavior skills (IMB) model. Journal of Adolescent Health. 2006;38:18–25. doi: 10.1016/j.jadohealth.2004.08.013. [DOI] [PubMed] [Google Scholar]
- Roodman AA, Clum GA. Reictimization rates and method variance: A meta-analysis. Clinical Psychology Review. 2001;21:183–204. doi: 10.1016/s0272-7358(99)00045-8. [DOI] [PubMed] [Google Scholar]
- Sacco WP, Levine B, Reed DL, Thompson K. Attitudes about condom use as an AIDS-relevant behavior: Their factor structure and relation to condom use. Psychological Assessment. 1991;3:265–272. [Google Scholar]
- Satterwhite CL, Kamb ML, Metcalf C, Douglas JM, Malotte CK, Paul S, Peterman TA. Changes in sexual behavior and STD prevalence among heterosexual STD clinic attendees: 1993–1995 versus 1999–2000. Sexually Transmitted Diseases. 2007;34:815–819. doi: 10.1097/OLQ.0b013e31805c751d. [DOI] [PubMed] [Google Scholar]
- Schroder KEE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Annals of Behavioral Medicine. 2003;26:104–123. doi: 10.1207/s15324796abm2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey MP, Vanable PA, Senn TE, Coury-Doniger P, Urban M. Predicting condom use among STD clinic patients using the information-motivation-behavior skills (IMB) model. Journal of Health Psychology. 2010;15:1093–1102. doi: 10.1177/1359105310364174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: Evidence from controlled studies, methodological critique, and suggestions for research. Clinical Psychology Review. 2008;28:711–735. doi: 10.1016/j.cpr.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA, Coury-Doniger P, Urban MA. Childhood sexual abuse and sexual risk behavior among men and women attending a sexually transmitted disease clinic. Journal of Consulting and Clinical Psychology. 2006;74:720–731. doi: 10.1037/0022-006X.74.4.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Wilson PA, Hansen NB, Kochman A, Neufeld S, Ghebremichael MS, Kershaw T. Effects of a coping intervention on transmission risk behavior among people living with HIV/AIDS and a history of childhood sexual abuse. Epidemiology and Social Science. 2008;47:506–513. doi: 10.1097/QAI.0b013e318160d727. [DOI] [PubMed] [Google Scholar]
- Slonim-Nevo V, Mukuka L. Child abuse and AIDS-related knowledge, attitudes, and behavior among adolescents in Zambia. Child Abuse and Neglect. 2007;31:143–159. doi: 10.1016/j.chiabu.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Susser E, Desvarieux M, Wittkowski KM. Reporting sexual risk behavior for HIV: A practical risk index and a method for improving risk indices. American Journal of Public Health. 1998;88:671–674. doi: 10.2105/ajph.88.4.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upchurch DM, Kusunoki Y. Associations between forced sex, sexual and protective practices, and sexually transmitted diseases among a national sample of adolescent girls. Women’s Health Issues. 2004;14:75–84. doi: 10.1016/j.whi.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Vogeltanz ND, Wilsnack SC, Harris TR, Wilsnack RW, Wonderlich SA, Kristjanson AF. Prevalence and risk factors for childhood sexual abuse in women: National survey findings. Child Abuse and Neglect. 1999;23:579–592. doi: 10.1016/s0145-2134(99)00026-5. [DOI] [PubMed] [Google Scholar]
- Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Education and Behavior. 1978;6:160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- Walsh JL, Senn TE, Scott-Sheldon LAJ, Vanable PA, Carey MP. Predicting condom use using the Information-Motivation-Behavioral Skills (IMB) Model: A multivariate latent growth curve analysis. Annals of Behavioral Medicine. 2011;42:235–244. doi: 10.1007/s12160-011-9284-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP, Carey KB, Verdecias RN. Increasing assertiveness skills to reduce HIV risk among women living with a severe and persistent mental illness. Journal of Consulting and Clinical Psychology. 1998;66:680–684. doi: 10.1037//0022-006x.66.4.680. [DOI] [PubMed] [Google Scholar]
- Wenninger K, Ehlers A. Dysfunctional cognitions and adult psychological functioning in child sexual abuse survivors. Journal of Traumatic Stress. 1998;11:281–300. doi: 10.1023/A:1024451103931. [DOI] [PubMed] [Google Scholar]
- Wilkinson WW. The structure of the Levenson locus of control scale in young adults: Comparing item and parcel indicator models. Personality and Individual Differences. 2007;43:1416–1425. [Google Scholar]
- Wilson HW, Widom CS. Pathways from childhood abuse and neglect to HIV-risk sexual behavior in middle adulthood. Journal of Consulting and Clinical Psychology. 2011;79:236–246. doi: 10.1037/a0022915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt GE, Lawrence J, Vodounon A, Mickey MR. The Wyatt Sex History Questionnaire: A structured interview for female sexual history taking. Journal of Child Sexual Abuse. 1992;1:51–68. [Google Scholar]
- Wyatt GE, Longshore D, Chin D, Carmona JV, Loeb TB, Myers HF, Rivkin I. The efficacy of an integrated risk reduction intervention for HIV-positive women with child sexual abuse histories. AIDS and Behavior. 2004;8:453–462. doi: 10.1007/s10461-004-7329-y. [DOI] [PubMed] [Google Scholar]
- Zurbriggen EL, Freyd JJ. The link between child sexual abuse and risky sexual behavior: The role of dissociative tendencies, information-processing effects, and consensual sex decision mechanisms. In: Koenig LJ, Doll LS, O’Leary A, Pequegnat W, editors. From child sexual abuse to adult sexual risk. Washington, DC: American Psychological Association; 2004. pp. XXX–XXX. [Google Scholar]