Abstract
Background
Intestinal malrotation in the newborn is usually diagnosed after signs of intestinal obstruction, such as bilious emesis, and corrected with the Ladd procedure.
Objectives
The objective of this report is to describe the presentation of severe cases of midgut volvulus presenting in infancy, and to discuss the characteristics of these cases.
Case Report
We performed a seven year review at our institution and present two cases of catastrophic midgut volvulus presenting in the post-neonatal period, ending in death soon after the onset of symptoms. These two patients also had significant laboratory abnormalities compared to patients with more typical presentations resulting in favorable outcomes.
Conclusions
While most cases of intestinal malrotation in infancy can be treated successfully, in some circumstances, patients’ symptoms may not be detected early enough for effective treatment, and therefore may result in catastrophic midgut volvulus and death.
Keywords: Malrotation, midgut volvulus, neonatal intensive care
INTRODUCTION
Intestinal malrotation may go unrecognized in the perinatal period. However, if cecal (Ladd's) bands are present or midgut volvulus ensues, the neonate may present with symptoms of intestinal obstruction such as bilious emesis, or signs of ischemic bowel such as bleeding per rectum.[1] If not treated expeditiously, volvulus can progress to ischemic gut necrosis, sepsis, and death.
CASE REPORTS
Case 1
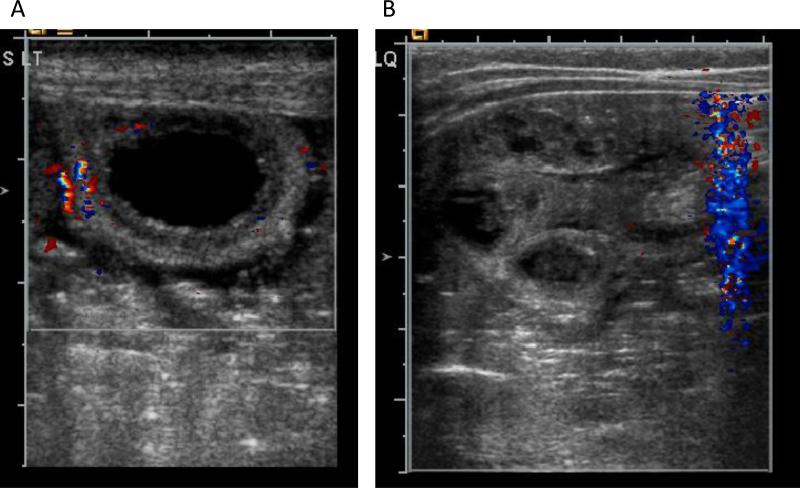
A male infant was born at 36 weeks gestation with a birth weight of 2.4 kg. He was in good health until 37 days old when, 8 hours prior to admission, he was fussy but consolable. Two hours prior to admission, he appeared pale and listless, had one non-bilious emesis, and developed difficulty breathing. He was brought to the emergency department (ED) with the following vital signs: heart rate 140 beats/min, respiratory rate 28 breaths/min, blood pressure 90/50 mm Hg, temperature 94.10 F (34.5° C), with a weight of 4.6 kg. He then developed bradycardia and his blood pressure decreased to 50/27 mm Hg. Soon thereafter, no heartbeat was detectable and cardiopulmonary resuscitation (CPR) was started. After three doses of epinephrine, his heart rhythm recovered after 20 minutes. Arterial blood gas revealed pH 6.5, pCO2 > 100, and base deficit 25. The patient had been resuscitated in the ED and then transferred to the neonatal intensive care unit without a clear diagnosis. Due to a distended abdomen, an abdominal ultrasound was performed by a pediatric radiologist, which showed fixed, dilated, fluid-filled loops with a thick bowel wall, no peristalsis, and decreased blood flow to the bowel wall (Figure 1A). The patient was taken to the operating room where exploratory laparotomy revealed distended bowel loops with bloody fluid in the abdominal cavity, along with midgut volvulus. Approximately 200 cm of necrotic bowel was removed, with much of the remaining bowel also suspicious for injury. Therefore, a plan was made to perform a “second look” procedure within 24 hours. He progressed to multi-organ failure with hypoglycemia, hyperkalemia, and anuria. He required 100% oxygen with sub-optimal oxygenation on high frequency oscillatory ventilation. There was an attempt to return to the operating room, but he was too unstable for that transition. After discussion with the family, the patient was transitioned to comfort care, and he expired soon thereafter, 30 hours after the initial presentation.
Figure 1.
(A) Case 1 – a fixed, dilated, aperistaltic, and hypoperfused bowel wall; (B) Case 2 – dilated bowel loops with thickened bowel wall
Case 2
A male infant was born at term with a birth weight 2.8 kg. The patient was well until 44 days old when he had symptoms of diaphoresis, fussiness, and poor feeding seven hours prior to admission. He fed three hours later without difficulty. Two hours later, he was fussy and his diaper was noted to have blood. He was taken to the ED approximately six hours after the initial symptoms, where he was noted to be lethargic, flaccid, and ashen in color. He was intubated, and an intraosseous line was placed for volume resuscitation. Capillary blood gas revealed pH 6.8, pCO2 31, pO2 163, and base deficit 29. During transport to the children's hospital, he had seizure activity and was given phenobarbital. The diagnosis was not clear at the time of transfer, but acute abdominal event was in the differential, as well as sepsis, congenital heart disease, and metabolic disorder. Admission vital signs were: heart rate 172 beats/min, respiratory rate 50 breaths/min, blood pressure 59/31 mm Hg, with weight 4 kg. His abdomen was distended with no bowel sounds. Abdominal radiograph and bedside ultrasound showed dilated bowel loops and thickened bowel wall (Figure 1B). Exploratory laparotomy revealed pan-necrosis of the entire small bowel and cecum, secondary to malrotation and midgut volvulus. After discussion with the family, the decision was made to close without bowel resection and transition to comfort care. He expired soon thereafter, 13 hours after the initial presentation.
DISCUSSION
Several reports have discussed the impact of delayed diagnosis on outcomes in malrotation and volvulus, with more time elapsed typically leading to increased mortality or more severe outcomes.[2-5] In the two cases presented here, the time between onset of symptoms and diagnosis was very short, but ended in death. Neither infant had any bilious emesis. Mortality has been described as higher in the immediate newborn period compared to the older infant, with one large series reporting the median age of survivors as 30 days compared to 4 days for those who died.[2] Another series of 68 children found that the worst outcomes occurred in patients presenting within the first week.[6] The two patients described in our report are atypical in that they had a normal, uneventful, and healthy first month and presented in the post-neonatal period with sudden, catastrophic volvulus leading to death despite appropriate management.
Although intestinal transplantation in children has greatly advanced, cases of massive intestinal resection remain challenging, as wait times are long and children often have complications associated with prolonged parenteral nutrition.[7] Children undergoing intestinal transplant are likely to have worse outcomes if the intestinal failure is surgical in nature.[8] Those requiring combined liver and intestinal transplant have even worse prognoses.[8] These considerations are noteworthy in the context of counseling parents whose infant has undergone a catastrophic event of bowel ischemia and necrosis.
We performed a seven year (2000-2007) retrospective review of all cases of malrotation with volvulus managed at XXXXXXXX presenting in the first year of life. We excluded patients with other congenital anomalies. Significant laboratory test differences between the two deaths and the 23 other cases are shown in Table 1. The two patients who died were significantly more anemic with hematocrit of 23.5% compared to 44.1% for those who survived. The two dying infants also had elevated liver function enzymes, and were coagulopathic with INR more than double compared to patients who survived (Table 1). Electrolyte abnormalities were also more notable, including disturbances in protein and phosphorus.
Table 1.
Laboratory differences between deaths and survivors in malrotation and volvulus.
| Mean laboratory values | Deaths (n=2) | Survived (n=11-20)* |
|---|---|---|
| Alkaline phosphatase (U/L) | 394 | 216 |
| Potassium (mEq/L) | 6.8 | 4.7 |
| Total protein (g/dL) | 4.2 | 5.6 |
| Alanine aminotransferase (U/L) | 116 | 20.9 |
| Aspartate aminotransferase (U/L) | 198 | 37.7 |
| Phosphorus (mg/dL) | 9.8 | 6.7 |
| Red blood cells (MIL/uL) | 2.3 | 4.3 |
| Hemoglobin (g/dL) | 7.7 | 14.9 |
| Hematocrit | 23.5% | 44.1% |
| International normalized ratio (INR) | 2.6 | 1.2 |
| Fibrinogen (mg/dL) | 116 | 266 |
p < 0.05 for all comparisons using student's t-test.
There were 23 survivors but not all laboratory tests were obtained at admission for each patient, and therefore N varies from 11 to 20.
Doppler ultrasound findings of a “whirlpool” or “swirl” sign of twisting of the superior mesenteric vein and mesentery around the superior mesenteric artery is diagnostic of volvulus.[9, 10] Also, reversal of the superior mesenteric artery and superior mesenteric vein orientations suggest malrotation, though not necessarily volvulus.[10] In the two case reports presented here, ultrasound findings were non-specific, but imaging combined with clinical presentation were highly suspicious of volvulus, and laparotomy confirmed the diagnosis.
CONCLUSION
While most cases of malrotation can be successfully treated with a timely diagnosis, two cases are reported in which there was a sudden, catastrophic event, likely of intense ischemia and intestinal necrosis, close to the initial recognition of symptoms. These patients presented with severe metabolic acidosis and systemic shock, unfortunately leaving little room for therapeutic intervention. Early diagnosis and treatment remains the key to improving survival, including prompt workup of patients presenting with even the slightest hint of bilious (green) emesis, despite otherwise normal physical findings. Bilious emesis in the full term neonate should be considered midgut volvulus until proven otherwise. Urgent laparotomy should be strongly considered in the term infant with bilious emesis accompanied by abdominal distension as this suggests midgut volvulus with compromised intestine. In such a patient, one should forego radiologic investigations in favor of early surgical intervention. However, as seen in this report, warning signs may not present early enough for adequate intervention in some cases.
Acknowledgments
This project was supported by NIH/NCRR/OD UCSF-CTSI Grant Number KL2 RR024130. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure / Conflicts of interest: None
REFERENCES
- 1.Ingoe R, Lange P. The Ladd's procedure for correction of intestinal malrotation with volvulus in children. AORN J. 2007;85:300–8. doi: 10.1016/S0001-2092(07)60040-4. quiz 9-12. [DOI] [PubMed] [Google Scholar]
- 2.Messineo A, MacMillan JH, Palder SB, Filler RM. Clinical factors affecting mortality in children with malrotation of the intestine. J Pediatr Surg. 1992;27:1343–5. doi: 10.1016/0022-3468(92)90293-g. [DOI] [PubMed] [Google Scholar]
- 3.Powell DM, Othersen HB, Smith CD. Malrotation of the intestines in children: the effect of age on presentation and therapy. J Pediatr Surg. 1989;24:777–80. doi: 10.1016/s0022-3468(89)80535-4. [DOI] [PubMed] [Google Scholar]
- 4.Millar AJW, Rode H, Brown RA, Cywes S. The deadly vomit: malrotation and midgut volvulus. Pediatr Surg Int. 1987;2:172–6. [Google Scholar]
- 5.Rasmussen L, Anderson OP, Pedersen SA. Intestinal malrotation and volvulus in infancy. Pediatr Surg Int. 1990;5:27–9. [Google Scholar]
- 6.Seashore JH, Touloukian RJ. Midgut volvulus. An ever-present threat. Arch Pediatr Adolesc Med. 1994;148:43–6. doi: 10.1001/archpedi.1994.02170010045009. [DOI] [PubMed] [Google Scholar]
- 7.Kaufman SS, Atkinson JB, Bianchi A, Goulet OJ, Grant D, Langnas AN, et al. Indications for pediatric intestinal transplantation: a position paper of the American Society of Transplantation. Pediatr Transplant. 2001;5:80–7. doi: 10.1034/j.1399-3046.2001.005002080.x. [DOI] [PubMed] [Google Scholar]
- 8.Bueno J, Ohwada S, Kocoshis S, Mazariegos GV, Dvorchik I, Sigurdsson L, et al. Factors impacting the survival of children with intestinal failure referred for intestinal transplantation. J Pediatr Surg. 1999;34:27–32. doi: 10.1016/s0022-3468(99)90223-3. discussion -3. [DOI] [PubMed] [Google Scholar]
- 9.Pracros JP, Sann L, Genin G, Tran-Minh VA, Morin de Finfe CH, Foray P, et al. Ultrasound diagnosis of midgut volvulus: the “whirlpool” sign. Pediatr Radiol. 1992;22:18–20. doi: 10.1007/BF02011603. [DOI] [PubMed] [Google Scholar]
- 10.Chao HC, Kong MS, Chen JY, Lin SJ, Lin JN. Sonographic features related to volvulus in neonatal intestinal malrotation. J Ultrasound Med. 2000;19:371–6. doi: 10.7863/jum.2000.19.6.371. [DOI] [PubMed] [Google Scholar]