Abstract
A 34-year-old Caucasian female with advanced primary angle closure glaucoma developed acute angle closure following administration of g.pilocarpine 2% given as preparation for laser peripheral iridotomies. Subsequent investigations supported an underlying diagnosis of spherophakia with no systemic associations. She required peripheral iridotomies, bilateral clear lens extractions and left cyclodiode laser to control her intraocular pressures. This case highlights the situations when pilocarpine should be given with caution and also the increasing role of phacoemulsification as an alternative to filtration surgery in primary angle closure glaucoma management.
Background
Our case highlights the situations when pilocarpine should be given with caution and also the increasing role of phacoemulsification as an alternative to filtration surgery in primary angle closure glaucoma management.
Case presentation
A 34-year-old Caucasian with advanced primary angle closure glaucoma was referred for peripheral iridotomies (PI). She had best-corrected visual acuities of 6/9 right (−14.50 DS) and 1/60 left (–15.00/−3.00×60). Intraocular pressure (IOPs) were 25 mm Hg right and 32 mm Hg left eye despite topical bimatoprost. Gonioscopy showed 360° appositional closure either eye.
Topical pilocarpine 2% and apraclonidine were administered in preparation for laser PI. Within 45 min she had severe headache with nausea and vomiting. IOPs were 18 mm Hg right and 68 mm Hg left. She was treated with intravenous acetazolamide and topical hypotensive medications and underwent uncomplicated PI. This resolved the left acute IOP rise, however it remained high at 32 mm Hg following PI and was 40 mm Hg 1 week later despite maximum medical IOP treatment. Repeat gonioscopy showed 180° appositional closure right eye, and 360° angle closure left eye of which 90° was peripheral anterior synechae (PAS). She underwent left cyclodiode laser and uncomplicated bilateral clear lens extractions.
Investigations
PCI biometry showed axial lengths of 28.44 mm right and 29.23 mm left with anterior chamber depths of 2.69 mm right and 2.24 mm left. Left lens thickness was 5.41 mm.
Outcome and follow-up
Four months later her IOPs are now well controlled on combination topical treatment.
Discussion
In eyes with narrow angles, pilocarpine increases the angle width as the effect of reduced iris thickness and iris root pull is greater than the forward movement of the iris-lens diaphragm due to ciliary muscle contraction.1 There are however exceptions. Acute angle closure (AAC) following pilocarpine administration has been reported in patients with spherophakia2 (as in Weill–Marchesani syndrome, WMS) but can also occur in patients with no known systemic abnormalities.3 In spherophakia, the highly convex lens is supported by long weak zonules that allow greater anterior movement of the iris-lens diaphragm. AAC in this situation can be relieved by PI. Other conditions associated with a paradoxical reaction to pilocarpine include exfoliation syndrome (zonular weakness), phacomophic glaucoma and malignant glaucoma.4 Our patient had no systemic features of WMS, however she was highly myopic with a left lens thickness of 5.41 mm with steep anterior lens curvature (figure 1) consistent with spherophakia.
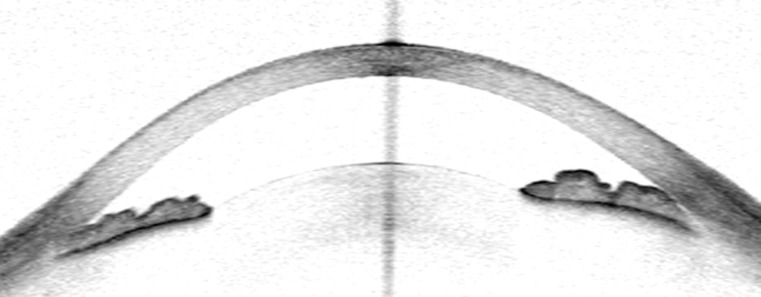
Figure 1.
Anterior segment optical coherence tomography image of left eye following PI showing closed anterior chamber angles.
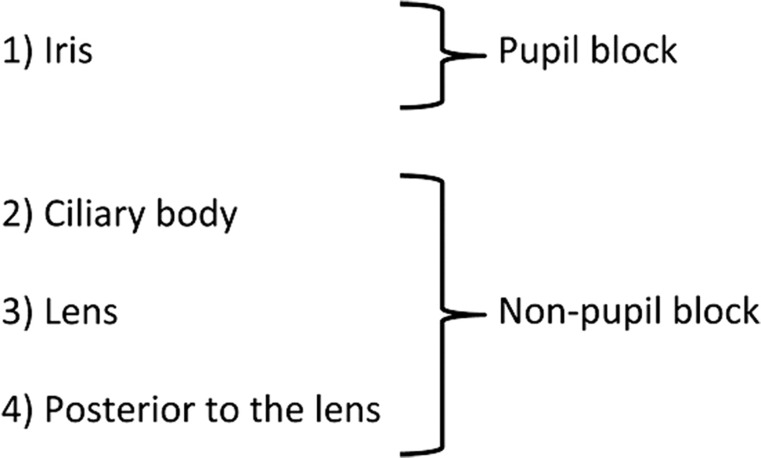
Ritch classified the anatomical basis of angle closure by four levels of block5 (figure 2). Angle closure resulting from level 3 or 4 (lenticular or retro-lenticular) block responds paradoxically to pilocarpine.5 As supported by the biometric and refractive data in our case, angle-closure was initially due to atypical non-pupil block mechanisms, with pilocarpine paradoxically precipitating AAC due to pupil block. The involvement of lower level block was only confirmed following exclusion of pupil block by PI. As PI does not treat non-pupil block causes of angle closure, lens exchanges were performed with cyclodiode laser to additionally help control the left IOP. Laser peripheral iridoplasty was contraindicated due to the presence of PAS.
Figure 2.
Anatomical levels of angle closure.
Learning points.
-
▶
Pilocarpine can paradoxically induce acute angle closure.
-
▶
Non-pupil block mechanisms of angle closure should be suspected in all young patients with angle closure.
-
▶
Laser peripheral iridotomy does not treat non-pupil block causes of angle closure.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Kobayashi H, Kobayashi K, Kiryu J, et al. Pilocarpine induces an increase in the anterior chamber angular width in eyes with narrow angles. Br J Ophthalmol 1999;83:553–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Willi M, Kut L, Cotlier E. Pupillary-block glaucoma in the Marchesani syndrome. Arch Ophthalmol 1973;90:504–8 [DOI] [PubMed] [Google Scholar]
- 3.Mohamed Q, Fahey DK, Manners RM. Angle closure in fellow eye with prophylactic pilocarpine treatment. Br J Ophthalmol 2001;85:1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ritch R. The pilocarpine paradox. J Glaucoma 1996;5:225–7 [PubMed] [Google Scholar]
- 5.Ritch R, Liebmann JM. Argon laser peripheral iridoplasty. Ophthalmic Surg Lasers 1996;27:289–300 [PubMed] [Google Scholar]