Abstract
Papillary thyroid carcinoma frequently metastasises to the regional neck lymph nodes. However, cervical lymph node metastases as sole manifestation of occult papillary thyroid carcinoma are observed rarely. The authors report the case of a 52-year-old man presenting for slowly enlarging neck region and shortness of breath, with an insidious history for 15 years. Thyroid imaging showed a goitre predominantly of the right lobe, but histopathological finding revealed a multi-centric thyroid papillary carcinoma with lymph node metastasis.
Background
The purpose of this manuscript is to present an uncommon type of evolution in a patient with papillary thyroid carcinoma with neck lymph node metastasis and a very long evolution for more than 15 years. This is a rare type of presentation of this pathology and I considered interesting to show the patient’s imaging together with histopathological finding and a very brief review of this infrequent situation.
Case presentation
A 52-year-old man presented for slowly enlarging neck region and progressively growing dyspnoea, with an insidious history for 15 years. The patient had a thyroid hormonal check-up by his general practitioner 2 years after onset of symptoms which seemed to be normal, no treatment being prescribed. However, no radiological examination of the neck was done, the patient being advised to see an ear, nose, throat specialist. The patient did not consult any specialist neither did he return to his general practitioner in the next 13 years until present.
In the last 3 months before consultation, the patient accused serious shortness of breath, especially in supine position and during effort, without any improvement in time. Physical examination revealed several huge cervical and supraclavicular nodes changing the entire neck morphology, with widened mediastinum on chest radiograph; the thyroid’s limits were difficult to appreciate. The serum thyrotropin and free thyroxin levels were normal as well as calcitonin serum value.
Investigations
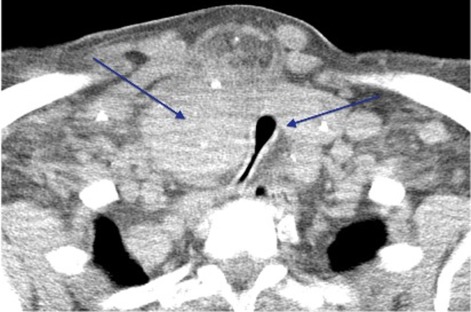
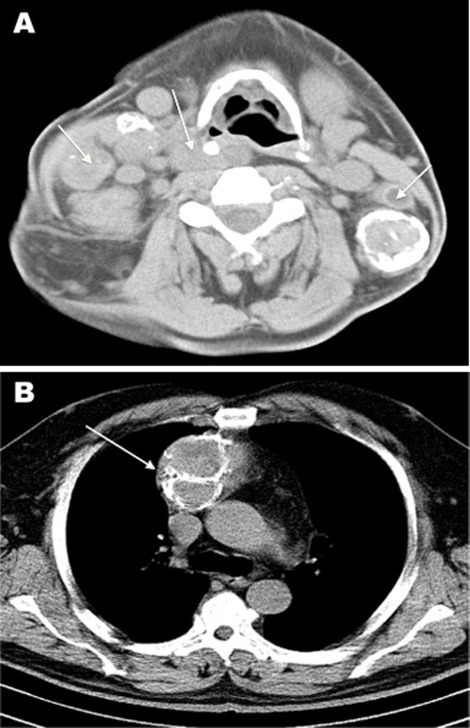
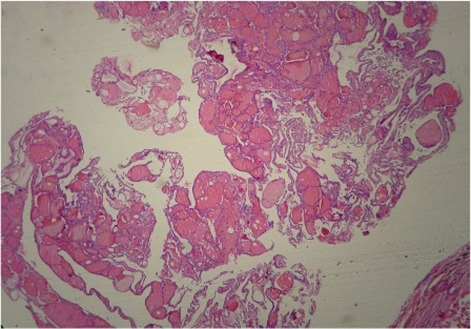
Ultrasonography of the neck revealed a homogenous thyroid gland and multiples cervical lymph nodes inhomogeneous with calcifications. The cervico-thoracic CT showed an enlarged inhomogeneous right thyroid lobe compressing the trachea (figure 1, left arrow), several cervical, supraclavicular and mediastinal adenopathy (figure 2A,B, arrows). A cervical lymph node biopsy revealed a structure compatible with nodular thyroid goiter (figure 3).
Figure 1.
Cervical CT showing enlarged inhomogeneous right thyroid lobe compressing the trachea (left arrow).
Figure 2.
(A, B) Cervical, supraclavicular and mediastinal lymphadenopathy (arrows).
Figure 3.
Cervical lymph node biopsy revealing typical nodular thyroid goiter tissue.
Treatment
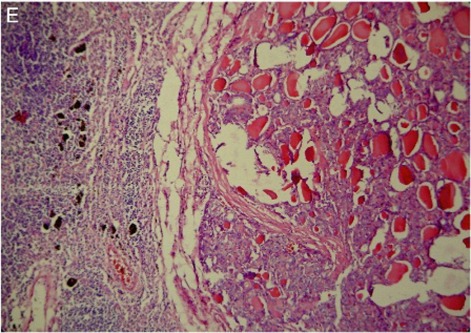
Our patient underwent a total thyroidectomy with neck exploration; cervical and superior mediastinal lymphadenectomy by cervicothoracic aboard was done. Hystopathological finding revealed a multi-centric thyroid papillary carcinoma, with lymph node metastasis (figure 4).
Figure 4.
Histopathological finding showing multicentric thyroid papillary carcinoma.
Outcome and follow-up
The postoperative course was uneventful except for a right recurrent nerve paralysis. The patient was discharged home 16 days after the surgery. Radioiodine therapy was conducted beginning at 4 weeks after surgery. At 6 month and 1 year follow-up the patient had persistent right recurrential paralysis without signs of recurrence.
Discussion
Papillary thyroid carcinoma frequently metastasises to the regional neck. The sites of lymph node metastasis of papillary thyroid carcinomas is typically the paratracheal and jugular lymph nodes.1
Although oronasopharyngeal squamous cell carcinoma has been reported as the main cause of lymph neck node metastasis, cervical lymph node metastases as first and sole manifestation of occult papillary thyroid carcinoma are observed exceptionally rarely. In most of the case, thyroid tumours are not palpable on physical examination and no abnormalities of the thyroid gland are shown by other diagnostic procedures. However, an alternative explanation is the presence of ectopic thyroid tissue associated with a branchial cyst or thyreoglossal duct, especially if no primary tumour is observed in the histological examination of the thyroid gland. For example, one per cent of excised thyreoglossal duct remnants exhibits histologic malignancy, a thyroid papillary carcinoma in 80% of the cases.2–4
Clinically palpable cervical nodes may reveal well-differentiated papillary thyroid cancer, especially in young patients. In contrast to a few follicles arranged in a wedge-shaped segment at the periphery of a lymph node, a significant amount of thyroid tissue in a cervical lymph node is considered evidence of metastatic thyroid carcinoma.5
In conclusion, in patients with lateral cervical tumours, the diagnosis of lymph node metastasis from occult papillary thyroid carcinoma should be considered. Any lateral mass requires tissue diagnosis and fine-needle aspiration is usually adequate for clarification of the histology. Ipsilateral modified neck dissection and total thyroidectomy followed by radioactive iodine therapy offers a favourable prognosis.3
Learning points.
-
▶
Occult papillary thyroid carcinoma metastasises frequently in the cervical lymph nodes.
-
▶
Papillary thyroid carcinoma could present with long history despite the absence of clinically apparent disease.
-
▶
The presence of thyroid tissue in a cervical lymph node is considered evidence of metastatic thyroid carcinoma.
-
▶
All cervical masses require tissue diagnosis and fine-needle aspiration is adequate for clarification of the histology.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Kainuma K, Kitoh R, Yoshimura H, et al. The first report of bilateral retropharyngeal lymph node metastasis from papillary thyroid carcinoma and review of the literature. Acta Otolaryngol 2011;131:1341–8 [DOI] [PubMed] [Google Scholar]
- 2.González-García R, Román-Romero L, Sastre-Pérez J, et al. Solitary cystic lymph neck node metastasis of occult thyroid papillary carcinoma. Med Oral Patol Oral Cir Bucal 2008;13:E796–9 [PubMed] [Google Scholar]
- 3.Verge J, Guixá J, Alejo M, et al. Cervical cystic lymph node metastasis as first manifestation of occult papillary thyroid carcinoma: report of seven cases. Head Neck 1999;21:370–4 [DOI] [PubMed] [Google Scholar]
- 4.Cervera-Paz FJ, Roquette Gaona J, Bartual Pastor J. [Ectopic primitive thyroid papillary carcinoma: report of a fatal case and review of literature]. Acta Otorrinolaringol Esp 1994;45:124–7 [PubMed] [Google Scholar]
- 5.De Jong SA, Demeter JG, Jarosz H, et al. Primary papillary thyroid carcinoma presenting as cervical lymphadenopathy: the operative approach to the “lateral aberrant thyroid”. Am Surg 1993;59:172–6; discussion 176–7. [PubMed] [Google Scholar]