Abstract
Statins are widely prescribed medications and very well tolerated. Rosuvastatin is another member of this drug used to treat dyslipidaemia. It is a competitive inhibitor of the enzyme 3-hydroxy-3-methylglutaryl coenzyme A reductase. Immunobullous disease is usually idiopathic but can be drug-induced. Both idiopathic and iatrogenic forms share common clinical and immunohistological features. The authors report a case of pemphigoid induced by rosuvastatin, a commonly prescribed medication. To our knowledge, there is limited report on rosuvastatin associated with pemphigoid in the literature.
Background
Drug-induced pemphigoid is rare and since rosuvastatin is a commonly prescribed medication and its association with pemphigoid has not been reported in the literature, it is worth mentioning that early recognition of this condition is crucial to reduce the risk of disease persistence, ulceration and scarring. With prompt cessation of the offending medication, the need for systemic corticosteroids and potentially exposure to potent immunosuppressives could be limited.
Case presentation
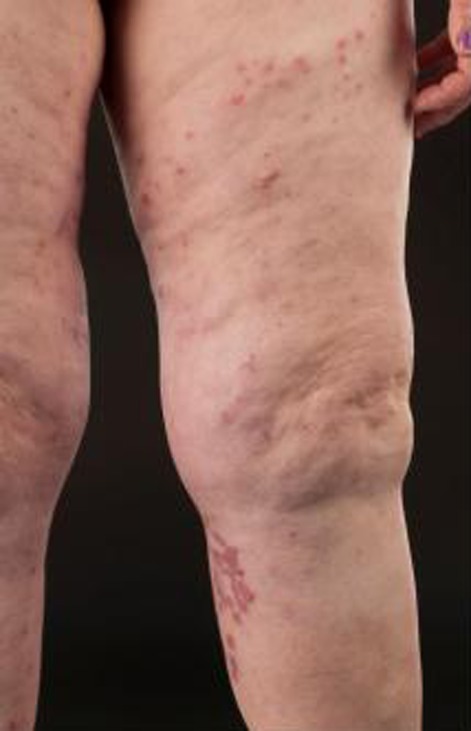
A 58-year-old lady developed an itchy blistering eruption on her legs. She was systemically well and had no other areas involved. She was prescribed rosuvastatin for elevated cholesterol by her general practitioner 2 weeks prior to the eruption. She was not on any other medications. Skin examination revealed clusters of intact blisters with erythematous base on her thighs (figure 1). There was no mucosal involvement and overall, she had a 5% body surface area affected.
Figure 1.
Scattered intact blisters with erythematous base on mid-anterior thighs. Older blisters seen on her upper calf.
Investigations
-
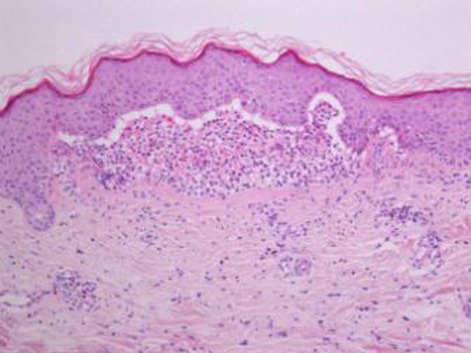
1)
Skin biopsy with H&E staining showed subepidermal blistering with chronic inflammatory cell infiltrate that consist of lymphocytes, eosinophils and histiocytes which were scattered perivascularly and in the interstitial spaces (figure 2).
-
2)
Direct immunofluorescence: no specific staining for IgG, IgA, IgM, C3 and fibrinogen.
-
3)
Indirect immunofluorescence was positive for pemphigoid antibodies.
-
4)
Blood analyses: Normal.
Figure 2.
Skin biopsy with H&E staining showed subepidermal blistering (arrow) with chronic inflammatory cell infiltrate perivascularly and in the interstitial spaces.
Differential diagnosis
-
1)
Idiopathic pemphigoid
-
2)
Lichenoid reaction
-
3)
Linear IgA disease
Treatment
-
1)
Rosuvastatin was discontinued.
-
2)
Topical clobetasol propionate ointment to the affected areas.
Outcome and follow-up
Blisters gradually resolved over 3 weeks with topical treatment and her skin remained clear at 6 months follow-up.
Discussion
Drug-induce pemphigoid was first described in 1970 and since then, several medications have been reported to be associated with this blistering disease. Common medications that are associated with pemphigoid are furosemide, bumetanide, captopril, enalapril, spironolactone, ampicillin and amoxicillin. Treatment of drug-induced pemphigoid consists of discontinuing the offending agent. Systemic steroids may sometimes be necessary depending on the disease severity. Generally, the disease is more severe in patients who are older, immunocompromised and those with mucosal and greater surface area involvement. There are two distinct clinical subtypes.1 ‘Drug-induced pemphigoid proper’ is more acute, but self-limited with rapid resolution after withdrawal of the offending agent. Systemic steroids may not be necessary. The second variant is a more chronic type that seems to be precipitated by a drug and the course is more consistent with spontaneous occurring disease. There are several hypotheses on the mechanisms of drug-induced pemphigoid. The offending drug may bind and modify protein molecules in the lamina lucida, uncovering some hidden antigenic site and potentially changing its antigenic properties.2 3 It may also cause dysregulation of T suppressor cell function which then releases antibodies including those against the antibasement membrane zone which causes pemphigoid.4 Our patient was not on any other medications and had no significant medical history. She improved rapidly when rosuvastatin was discontinued. Diagnosing this condition may not be so straight forward in patients who are on multiple medications. Often, decision on which medication is the cause of the eruption will depend on clinical history, time course from first dose to eruption and rapid resolution of lesions on cessation of the offending drug. Rechallenging with the drug may provide definite diagnosis of the causative agent but is not commonly done due to safety and ethical reasons.
Learning points.
-
▶
Immunobullous disease is usually idiopathic but sometimes can be drug-induced.
-
▶
Focused clinical history and time course from first dose to onset of eruption help differentiates these subtypes.
-
▶
Although clinically distinct, drug-induced pemhigoid share immunohistological features.
-
▶
Immunofluorescence is a good diagnostic adjunct to differentiate the various subtypes of blistering diseases.
-
▶
Drug-induced pemphigoid is self-limited, therefore timely cessation of offending medication reduces the risk of disease persistence, ulceration, scarring and exposure to potent immunosuppressives. They usually have no recurrence.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Hodak E, Ben-Shetrit A, Ingber A, et al. Bullous pemphigoid–an adverse effect of ampicillin. Clin Exp Dermatol 1990;15:50–2 [DOI] [PubMed] [Google Scholar]
- 2.Bean SF, Good RA, Windhorst DB. Bullous pemphigoid in an 11-year-old boy. Arch Dermatol 1970;102:205–8 [PubMed] [Google Scholar]
- 3.Kashihara M, Danno K, Miyachi Y, et al. Bullous pemphigoid-like lesions induced by phenacetin. Report of a case and an immunopathologic study. Arch Dermatol 1984;120:1196–9 [PubMed] [Google Scholar]
- 4.Ruocco V, Sacerdoti G. Pemphigus and bullous pemphigoid due to drugs. Int J Dermatol 1991;30:307–12 [DOI] [PubMed] [Google Scholar]