Abstract
Malignant lymphomas represent about 9% of cardiac neoplasms. Despite its life-threatening nature, the cardiac manifestations are often subclinical. In about 20% of deaths from lymphoma, cardiac involvement is found only in autopsy. The authors present the case of a 77-year-old female admitted due to intense back pain, vomiting, generalised pruritus, fatigue and weight loss. She had a personal history of hypertension and breast cancer was noted 10 years before admission. The thoracoabdominopelvic CT showed a mass in the left atrium with extension to the right atrium and inferior vena cava, and a paravertebral mass at D10-D11 with invasion of the spinal canal and hepatic hilum. The transthoracic paravertebral mass biopsy was compatible with a diffuse large B cell lymphoma. The patient developed a complete atrioventricular block, with haemodynamic instability, requiring urgent chemoreduction of the paracardiac mass and implantation of an epicardial pacemaker.
Background
Although cardiac involvement is not uncommon in lymphoma, the majority of cases are detected only postmortem. The diagnosis of cardiac involvement is very difficult, because the clinical signs and symptoms of cardiac dysfunction are non-specific and there is often a low index of suspicion.1 A complete heart block, as as a complicating cardiac feature, is extremely rare.
In the clinical case presented, we underline the diagnostic and therapeutic difficulty in management, requiring a multi-disciplinary team involving cardiology and haematology.
Case presentation
A 77-year-old Caucasian female presented in the emergency room with severe back pain radiating to the right hypochondrium, vomiting, generalised pruritus, night sweats and fatigue with 2-weeks evolution and weight loss (8 kilograms) during the previous year.
The patient had a known history of hypertension and breast cancer 10 years before admission (mastectomy and hormone therapy), with evidence of remission. Initial clinical examination was unremarkable (including normal blood pressure and cardiac rhythm), except for a painful palpation of vertebral dorsal spinous processes.
The lab investigation showed a moderate cholestatic pattern and elevated erythrocyte sedimentation rate, lactate dehydrogenase and β-2-microglobulin (table 1).
Table 1.
Relevant laboratory parameters
| Parameter | Value |
|---|---|
| Haemoglobin | 13 (13, 5–18) g/dl |
| Leucocytes/neutrophils | 10200 (4–10) mm3; 77% (37–72) |
| C reactive protein | 4, 32 (<1) mg/dl |
| ESR | 41 (1–20) mm/1st h |
| AST | 167 (14–36) U/l |
| ALT | 363 (9–52) U/l |
| δ-GT | 201 (12–43) U/l |
| Alkaline phosphatase | 166 (38–126) U/l |
| LDH | 5828 (313–618) U/l |
| β-2-microglobulin | 3, 6 (<2) mg/l |
| Electrophoresis of proteins/serum immunofixation | No monoclonal peak |
| Troponin | 0, 1 (<0,05) ng/ml |
| HIV ½ (ELISA) | Negative |
| HBsAg/anti-HBs/anti-HBc | Negative |
| Anti-HCV | Negative |
ALT, alanine transaminase; AST, aspartate aminotransferase; ESR, erythrocyte sedimentation rate; GT, glutamyl transpeptidase; LDH, lactate dehydrogenase
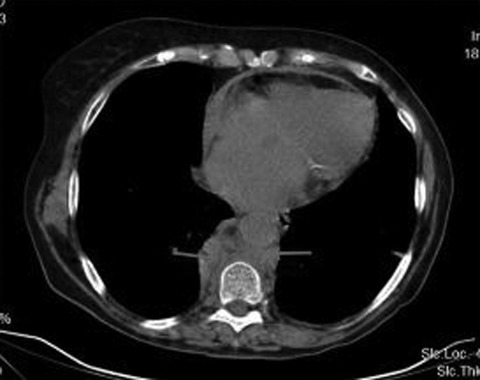
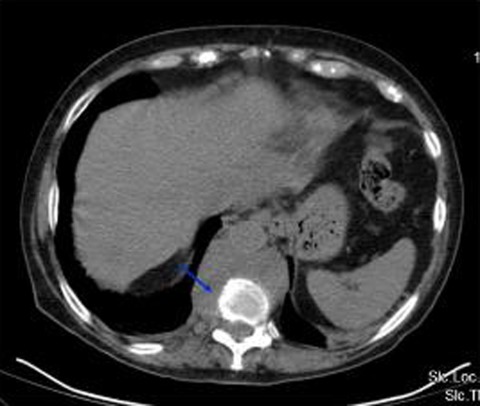
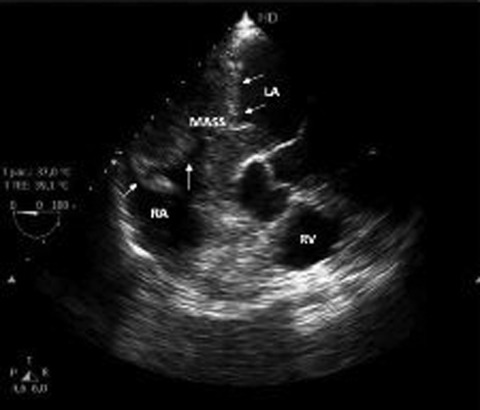
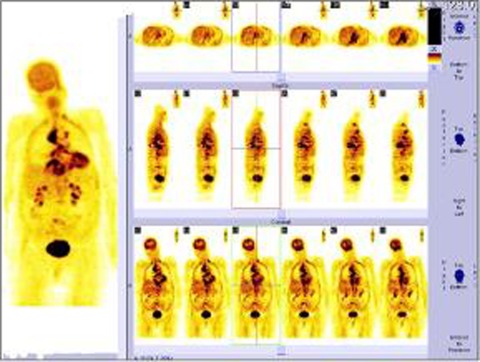
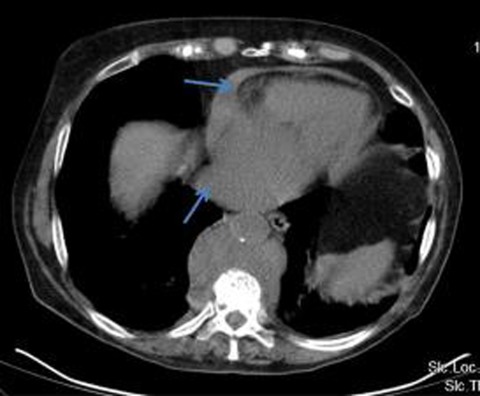
The thoracoabdominopelvic CT showed mediastinal, retro-crural and aortocava enlarged lymph nodes; a paravertebral mass at D10-D11 (6 5 centimetres) with invasion of the spinal canal and hepatic hilum; main bile duct and intrahepatic dilation; a mass in the left atrium (LA) with intraluminal and parietal component, with extension to the right atrium (RA) and inferior vena cava (IVC) (figures 1–3). The transthoracic and transoesophageal echocardiography confirmed a large mass in the RA (4 4×4 7 centimetres), involving the interatrial septum, LA and IVC, causing flow obstruction and dilation of the vein (figure 4). The positron emission tomography (PET)-CT confirmed the abnormalities found in the CT, showing extensive F18-fluorodeoxyglucose (18F-FDG) uptake in the right mediastinum; In the lower back revealed an hypocaptive area surrounded by an uptake halo, corresponding to the paravertebral mass (figure 5). The transthoracic CT-guided paravertebral mass biopsy was compatible with a diffuse large B cell lymphoma (non-Hodgkin): large cell size, κ monoclonality, CD5−/CD20+ (low intensity)/CD19+.
Figure 1.
Thoracoabdominopelvic CT showed a paravertebral mass at D10-D11.
Figure 3.
Thoracoabdominopelvic CT showed a paravertebral with invasion of the spinal canal.
Figure 4.
The transoesophageal echocardiography revealed a large mass in the right atrium, involving the septum and inferior vena cava. The arrows show the limits of the mass. LA, left atrium; RA, right atrium; RV, right ventricle.
Figure 5.
Positron emission tomography with extensive F18-fluorodeoxyglucose uptake in the right mediastinum; In the lower back revealed a hypocaptive area surrounded by an uptake halo, corresponding to the paravertebral mass.
Figure 2.
Thoracoabdominopelvic CT showed a mass in the left atrium with extension to the right atrium and inferior vena cava.
A bone marrow biopsy revealed normocellular bone marrow without infiltration of lymphomatous cells.
The patient was at stage III-B (involvement of lymph node regions on both sides of the diaphragm, which may be accompanied by localised involvement of an extranodal organ; presence of B symptoms) of Ann Arbor Classification.
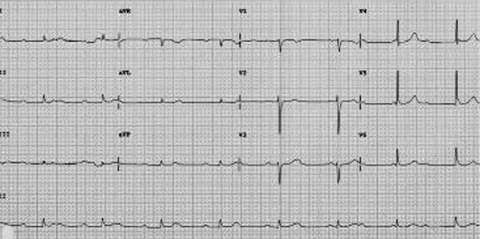
On the 9th day as an inpatient, evidence of bradycardia (40 to 50 beats per min) with haemodynamic instability was noted. EKG was compatible with an atrioventricular (AV) complete block (figure 6). The case was discussed in a multi-disciplinary meeting with cardiologist and haematologist.
Figure 6.
EKG with an atrioventricular complete block.
Treatment
Technical difficulty in implantion of a pacemaker via the transvenous approach was noted due to to the location and dimension of the paracardiac mass; it was decided to perform urgent chemoreduction in a haemato-oncology centre with R-CHOP (rituximab, cyclophosphamide, doxorrubicine, vincristine and prednisolone), maintenance therapy with an isoprenaline perfusion and methylprednisolone and, later on, surgical implantation of an epicardial pacemaker with a good primary cardiac outcome.
Outcome and follow-up
In the haemato-oncology centre, the patient completed four chemotherapy cycles but unfortunately succumbed, 5 months later, due to sepsis secondary to pneumonia and had already evidence of lymphomatous leptomeningeal involvement.
Discussion
The patient had the diagnosis of a diffuse large B cell non-Hodgkin lymphoma (NHL), with lymph node, cardiac, paravertebral, spinal cord, hepatic hilum and later on, leptomenigeal involvement. At the time of death, the patient was at stage IV-B (disseminated, with distant extranodal organs and lymph node involvement; presence of B symptoms) of Ann Arbor Classification.
The term lymphoma describes a heterogeneous group of malignancies with different biology and prognosis. About 85% of all malignant lymphomas are NHLs and almost 85% of NHLs are of B cell origin.2
Diffuse large cell lymphoma is the most common type, representing 31% of NHLs, and it is rapidly fatal if untreated. In general, it occurs in middle-aged and older people.3
Cardiac masses arising from the heart or the pericardium are potentially lethal whether defined as benign or malignant. Almost 75% of primary cardiac masses are benign. The most common primary malignant tumours are sarcomas and lymphomas. Metastatic deposits represent the vast majority of cardiac malignancies; the common primary sources include lung, oesophagus and breast cancers as well as lymphoma, leukaemia and melanoma.4
Primary cardiac lymphoma is rare (1%), but secondary involvement of the heart by lymphoma is not uncommon (20%).5 6 Primary cardiac lymphoma has been linked to imunossupressive states, including that of HIV, being extremely rare in immunocompetent subjects, and most frequently involves the RA.6 Recently, the close relation between Epstein–Barr virus and malignant lymphoma occurring in immunodeficient patients has been established.7
Cardiac involvement as an initial presentation of malignant lymphoma is a rare occurrence. At autopsy, cardiac involvement is evident in about 1% of patients with advanced cancer. Secondary involvement of the heart is seen in 8 7–27 2% of documented clinical cases of lymphoma: 16% of patients with Hodgkin’s disease and 18% of patients with NHLs.4 8
T cell lymphomas invade the heart more frequently and present with a greater variety of cardiac manifestations than B cell lymphomas.9
Despite its life-threatening nature, the cardiac manifestations of lymphomatous involvement of the heart are often subclinical. Signs and symptoms of cardiac dysfunction such as chest pain, dyspnoea and arrhythmia, may be clinically undetectable, and cardiac involvement is often undermined before death.8 The disease may involve all cardiac structures, but lesions of the right heart and particularly the RA are predominant.10
Clinical presentation of cardiac metastases is determined by numerous factors such as tumour location, size, growth rate, degree of invasion and friability.4
In spite of no signs of conduction disturbance, sudden death occurs in many cases. This suggests the lymphoma infiltrates the cardiac conduction system silently and causes a sudden fatal arrhythmia.11
EKG findings include atrial flutter, atrial fibrillation, varied degree of AV block, bundle branch block and low voltage, but these findings are non-specific for malignant lymphoma.12
A complete heart block caused by tumour destruction of the conduction system is extremely rare.1
In the English literature about 20 cases presenting with AV block have been described. Among those cases, a pacemaker was inserted in patients with high degree AV block.13
More common presenting symptoms associated with malignant tumours of the heart are congestive heart failure, pericardial effusion and superior vena cava obstruction.7
Troponin elevations as result of cardiac ischaemia from lymphomatous deposits are a more unusual presentation.4
Three mechanisms can be suggested to explain heart tissue involvement: direct neighbouring extension of the tumour from a primitive mediastinal site, retrograde flow through the cardiac lymphatics and haematogenous spread.10 Most authors believe that direct extension and/or retrograde lymphatic spread are the most common means by which carcinomas involve the heart. In contrast, the haematogeneous route, has been proposed as the most common mechanism by which lymphomas, leukemias, sarcomas and malignant melanomas metastasise to the heart.14
The direct extension, as in our clinical case, has been found most destructive with the highest frequency of cardiac dysfunction.15
A diagnosis of cardiac lymphoma is difficult because of limitations in the imaging resolution of available techniques.11
Echocardiography was the first non-invasive mechanism for examining the chambers of the heart and pericardium, but the restricted acoustic window of the transthoracic approach remains a significant limitation. The larger imaging field afforded by transesophageal echocardiography makes this a more sensitive technique for these patients. CT adequately demonstrates morphology, location and extent of cardiac neoplasms, while MRI signal intensity with contrast enhancement results in superior images identifying anatomy, blood flow and cardiac function.4 CT and MRI have better contrast resolution than echocardiography and may suggest the tumour type.16 17 Although the different imaging tests (ultrasound, CT, MRI) should be considered complementary than competitive, if a cardiac involvement is suspected, MRI should be the preferred tool.18
FDG PET imaging has recently been reported to reveal previously unsuspected cardiac involvement.4 Cytology is diagnostic in two-thirds of cases.11
The prognosis of cardiac involvement lymphoma remains poor due to diagnostic delay and advanced stage of organ infiltration.10 The available literature suggests systemic chemotherapy is the only effective therapy. There is a theoretical risk of cardiac wall perforation in response to chemotherapy. The majority of cases are treated with combination chemotherapy with varying results.4
The cyclophosphamide, adriamycin (doxorubicin), vincristine, prednisone (CHOP) regimen was among the first combinations to produce complete response rates and long-term survivors.3
However, nowadays, the addition of rituximab to the CHOP protocol increases the overall survival rate.10 Rituximab is a monoclonal antibody directed against CD20 and frequently induces regression in a variety of B cell NHLs. Its mechanism of action seems to involve induction of antibody-dependent, cell-mediated cytotoxicity, complement-mediated lysis, phagocytosis of antibody-coupled tumour cells and induction of apoptosis.19
Whenever a complete AV block caused by an infiltration of lymphoma cells occurs, chemotherapy is thus considered to be the treatment of choice, as well as the implant of a pacemaker to control the arrhythmia.7
A brief review was performed based on a MEDLINE search using the Pubmed database. The search of ‘secondary cardiac lymphoma with complete AV block’ revealed no references. The search of ‘cardiac lymphoma (primary) with complete AV block’ revealed 14 references (25 cases): nine were written in English, two in French, one in Spanish, one in Japanese and one in Danish.
Learning points.
-
▶
Metastatic cardiac involvement is not uncommon in lymphoma, but carries a high mortality due to the absence of symptoms, stressing the importance of maintaining a high suspicion index.
-
▶
Use of several imaging modalities, including echocardiography, cardiac CT, MRI and FDG PET may allow an early diagnosis and can suggest the tumour type.
-
▶
The cardiac lymphomas can lead to a complex and difficult management, with a need of a prompt multi-disciplinary approach.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Schifter DR, Hussain KM, Saul BI, et al. A case report of complete heart block caused by non-Hodgkin’s lymphoma: the diagnostic role of transesophageal echocardiography. J Am Soc Echocardiogr 1995;8:331–3 [DOI] [PubMed] [Google Scholar]
- 2.Vinjamaram S, Estrada-Garcia DA, Hernandez-Ilizaliturri FJ, Sparano JA. Non-Hodgkin lymphoma. Emedicine (WebMD). 2011. Available from: URL: http://emedicine.medscape.com/article/203399-overview (accessed 15 August 2011).
- 3.Kallab AM. Diffuse Large Cell Lymphoma. Emedicine (WebMD). 2011. Available from: URL: http://emedicine.medscape.com/article/202969-overview (accessed 15 August 2011).
- 4.O’Mahony D, Piekarz RL, Bandettini WP, et al. Cardiac involvement with Lymphoma: a review of the literature. Clin Lymphoma Myeloma 2008;8:249–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liang R, Yu CM, Au WY, et al. Non-Hodgkin’s lymphoma involving the heart. J Clin Oncol 2000;18:1998–9 [DOI] [PubMed] [Google Scholar]
- 6.Yavari A, El-Mahy H, Mc illiams ET. Right atrial mass in the context of recurrent non-Hodgkin’s lymphoma: atrial myxoma presenting with atrial flutter. BMJ Case Reports 2009;doi: 10.1136/bcr.10.2008.1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagano M, Uike N, Suzumiya J, et al. Successful treatment of a patient with cardiac lymphoma who presented with a complete atrioventricular block. Am J Hematol 1998;59:171–4 [DOI] [PubMed] [Google Scholar]
- 8.Ban-Hoefen, Zeglin MA, Bisognano JD. Difuse large B cell lymphoma presenting as a cardiac mass and odynophagia. Cardiol J 2008;15:471–4 [PubMed] [Google Scholar]
- 9.Chinen K, Izumo T. Cardiac involvement by malignant lymphoma: a clinicopathologic study of 25 autopsy cases based on the WHO classification. Ann Hematol 2005;84:498–505 [DOI] [PubMed] [Google Scholar]
- 10.Errihani H, Belbaraka R, Ismaili N, et al. An unusual presentation of non-Hodgkin lymphoma: cardiac involvement. J Cancer Res Ther 2010;6:401–2 [DOI] [PubMed] [Google Scholar]
- 11.Takenaka S, Mitsudo K, Inoue K, et al. Successful treatment of primary cardiac lymphoma with atrioventricular nodal block. Int Heart J 2005;46:927–31 [DOI] [PubMed] [Google Scholar]
- 12.Huang HL, Hung CY, Chin CH, et al. Primary cardiac lymphoma with complete atrioventricular block. Acta Cardiol Sin 2011;27:56–9 [Google Scholar]
- 13.Cho SW, Kang YJ, Kim TH, et al. Primary cardiac lymphoma presenting with atrioventricular block. Korean Circ J 2011;40:94–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McDonnell PJ, Mann RB, Bulkley BH. Involvement of the heart by malignant lymphoma: a clinicopathologic study. Cancer 1982;49:944–51 [DOI] [PubMed] [Google Scholar]
- 15.Gouldesbrough DR, Carder PJ. Rapidly progressive cardiac failure due to lymphomatous infiltration of the myocardium. Postgrad Med J 1989;65:668–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ryu SJ, Choi BW, Choe KO. CT and MR findings of primary cardiac lymphoma: report upon 2 cases and review. Yonsei Med J 2001;42:451–6 [DOI] [PubMed] [Google Scholar]
- 17.Araoz PA, Eklund HE, Welch TJ, et al. CT and MR imaging of primary cardiac malignancies. Radiographics 1999;19:1421–34 [DOI] [PubMed] [Google Scholar]
- 18.Tesoro-Tess JD, Biasi S, Balzarini L, et al. Heart involvement in lymphomas. The value of magnetic resonance imaging and two-dimensional echocardiography at disease presentation. Cancer 1993;72:2484–90 [DOI] [PubMed] [Google Scholar]
- 19.Nakagawa Y, Ikeda U, Hirose M, et al. Successful treatment of primary cardiac lymphoma with monoclonal CD20 antibody (rituximab). Circ J 2004;68:172–3 [DOI] [PubMed] [Google Scholar]