Abstract
AIM: To assess the reasons for, and factors associated with, patient-initiated changes in treating specialist in inflammatory bowel diseases (IBD).
METHODS: Prospectively identified IBD patients (n = 256) with ≥ 1 encounter at a metropolitan hospital were surveyed, including whether they had changed treating specialist and why. Negative reasons included loss of confidence, disagreement, and/or personality clash with the specialist.
RESULTS: Of 162 respondents, 70 (43%) had ever changed specialists; 30/70 (43%) for negative reasons, 52/70 (74%) in the preceding year. Patients with negative reasons for changing (n = 30) were younger (median, 35.2 years vs 45.3 years) ,had higher IBD knowledge (median, 5.0 years vs 4.0 years), yet had lower medication adherence and satisfaction scores (median, 19.0 years vs 22.0 years, 14.0 years vs 16.0 years respectively, Mann-Whitney tests, all P < 0.05), compared to all other responders (n = 132). Patients with a recent change (for any reason) were more likely to have Crohn’s disease, currently active disease, previous bowel resection and recent hospitalization [OR 2.6, 95% CI (1.3-5.4), 2.2 (1.0-4.7), 5.56 (1.92-16.67), 2.0 (1.3-3.0), each P < 0.05].
CONCLUSION: Changing specialist appears associated with patient- related (age, nonadherence) and contemporaneous disease-related factors (recent relapse) which, where modifiable, may enhance patient-doctor relationships and therefore quality of care.
Keywords: Inflammatory bowel disease, Patient-doctor relationship, Quality of care, Disease outcomes, Quality of life
INTRODUCTION
In chronic inflammatory bowel diseases (IBD), a positive patient-doctor relationship (PDR) appears integral to optimizing quality of care (QoC). Although specific IBD data are lacking, a positive PDR is associated with improved patient satisfaction and health outcomes in other chronic diseases like diabetes and hypertension[1]. In a consumer-driven society, patient-centered care appears essential for a positive PDR[2], and thus assessing patients’ satisfaction with their specialist is important[3]. A positive PDR should facilitate the development of trust essential to the therapeutic process and ensure continuity of care, thus consolidating high-quality care[4,5].
Conversely therefore, PDR discord may compromise QoC, leading to adverse outcomes[6]. Discord may result from personality clashes, lack of rapport, misunderstandings, patient disenfranchisement over management decisions, or adverse disease outcomes. Yet, quantifying PDRs is difficult. Patient self-report instruments to rate PDRs are emerging, but understanding of their relevance to QoC is limited[7,8].
In Australia, as in many countries worldwide, there is significant variation in care models available to IBD patients; ranging from those managed solely by their primary care practitioner; those seen by a colorectal or general surgeon, general physician/internist, or by a specialist gastroenterologist either in private rooms or within a local hospital clinic setting; to those seen in the secondary/tertiary care setting within a dedicated hospital-based “IBD service” with multiple gastroenterologists and clinicians co-located with specific interests in IBD[9]. Each model has inherent strengths and weaknesses and may be attractive to different patients for various reasons. Moreover, with the multiple options potentially available, patients are theoretically able to select and change treating specialist (either in the government-funded public or private sectors), pending appropriate referral from their primary care practitioner and subject to regional availability. Thus one may theoretically assume the patient, as the consumer, may change their treating IBD specialist if their perceived PDR discord “threshold” was overcome and a suitable alternative existed (i.e., “voting with their feet”).
Hence, we aimed to explore PDRs in an IBD cohort with the simple, tangible measure of whether patients changed treating specialists and whether this had occurred recently and/or for negative reasons, as a marker of patient satisfaction with the PDR and their medical care. We also explored potential factors associated with patients switching specialist for their care. Although patients logically may report changing specialists for innocuous reasons (e.g., relocation), instances where change occurs, especially for negative reasons from the patients’ perspective, represent vulnerable moments in QoC delivery, but also provide an insight into the importance of the PDR, and its continuity[10].
MATERIALS AND METHODS
Subjects and recruitment
All patients with confirmed IBD diagnoses who had an inpatient or outpatient encounter for any reason at the Royal Adelaide hospital (RAH), in a 6-mo period from November 1 2007 to April 30 2008, were prospectively identified as previously described[9].
Subsequently, medical record review was performed to verify diagnoses, and extract further data including demographics, psychological comorbidity, previous surgery and healthcare utilization data. A contemporaneous (± median 14 d), physician global assessment[11] of disease activity (0 = inactive through to 4 = severe) was performed based on all information available, including clinical data (Harvey-Bradshaw criteria)[12], pathology and histological/endoscopic activity grading.
Patient survey
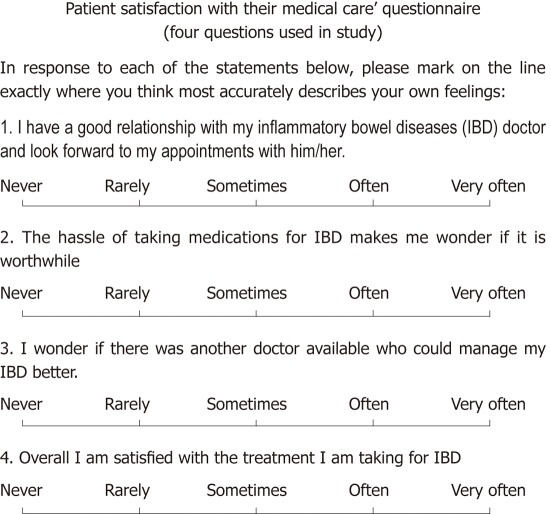
Surveys were distributed to each patient comprising multiple components; IBD patient knowledge was assessed using two validated questionnaires[13,14], health-related quality of life was assessed using the shortened inflammatory bowel disease questionnaire (sIBDQ10)[15], the medication adherence report scale (MARS-5) assessed medication adherence[16], and the hospital anxiety depression scale screened for anxiety and depression[17]. Patient satisfaction with medical care was measured using a novel instrument (Figure 1), yet to be validated but the use of which has previously been reported[9]. This comprises four questions with a total score of 20 indicating 100% patient satisfaction. A score < 16 arbitrarily indicates suboptimal satisfaction.
Figure 1.
Scoring system. Maximum 5 points per question, maximum total of 20 indicates complete, 100% satisfaction with medical care. Score less than 16 indicates “suboptimal” satisfaction. Before scoring, responses to questions 2 and 3 must be inverted (i.e., never = 5, rarely = 4, etc.) prior to calculating absolute scores.
Endpoints relating to change in treating specialist
IBD patients were asked “Have you ever changed your treating specialist,” and “If yes, why?” Reasons for changing were deemed negative if the patients’ response included at least one of: (1) loss of confidence; (2) disagreement/dissatisfaction regarding management; (3) personality clash with specialist; or (4) other (including “specialist too busy”, “waiting time too long”). Alternative reasons including “doctor retired”, “doctor/patient moved” or “financial reasons” were not deemed negative responses. The endpoint “Change within 12 mo of survey completion, for any reason” was used to determine contemporaneous disease- and patient-related associations with changing specialist. At the time of survey, 108 (66.6%) of the cohort saw their current treating specialist at an outpatient clinic at RAH, whereas 54 (33.3%) had a current treating specialist based externally to the hospital (either in public or private sector).
Analysis
Statistical analyses were performed using SPSS 15.0.1.1 (Chicago, IL, United States). Bivariate correlations were conducted between variables and changing endpoints. Subsequently, exploratory logistic regression analyses assessed variables for inclusion in the final multivariable model. Those of definite clinical relevance were retained in the model regardless of statistical significance or fit; continuous variables remained unchanged wherever possible.
Ethics
The study was approved by the RAH Research Ethics Committee. Return of a completed survey was accepted as implied patient consent.
RESULTS
Patient characteristics
Two hundred and fifty-six confirmed IBD patients were prospectively identified over 6 mo, and 162 (63.3%) returned a completed survey. Responders had a median age of 43 years (range, 18-90), median IBD duration of 7 years (range, 0-47) (Table 1). As reported elsewhere, survey responders and non-responders did not differ significantly[9].
Table 1.
Clinical and disease characteristics of inflammatory bowel diseases patients who responded to survey (n = 162)
| Patient variable | n (%) |
| Female sex | 85 (52.5) |
| Crohn’s disease | 95 (58.6) |
| Ulcerative colitis | 65 (40.1) |
| Previous bowel resection surgery (ever) | 50 (30.9) |
| Recent inpatient admission1 | 80 (49.4) |
| Active disease2 | 69 (42.6) |
| Current stoma | 19 (11.7) |
| Current perianal disease | 29 (18.0) |
| Current cigarette smoker | 31 (19.1) |
| Documented history of psychological comorbidity | 41 (25.3) |
| Currently unable to work due to illness | 39 (24.1) |
| Proportion of lowest socioeconomic group3 | 16 (9.9) |
Inpatient admission in period between January 1, 2007-April 31, 2008;
as determined by physician global assessment at time of survey completion;
according to Social Health atlas, Central Northern Adelaide Health Service, Department of Health, SA 2004.
Changing specialist for any reason
Overall, 70/162 (43.2%) respondents had ≥ 1 change in specialist for any reason since IBD diagnosis. Of these, the median number of changes per patient since diagnosis was 2.0 (range: 1-6, Figure 2). Thirty of 70 patients who changed specialists (42.9%) gave a negative reason, and 52/70 patients changing specialist (74.3%) had done so within the prior 12 mo (for any reason). The total number of changes per patient correlated weakly positively with IBD duration (rs = 0.19), and when controlling for disease duration, positively with IBD knowledge (rs = 0.20) and negatively with age (rs = -0.22) (Spearman’s partial correlations, all P < 0.02).
Figure 2.
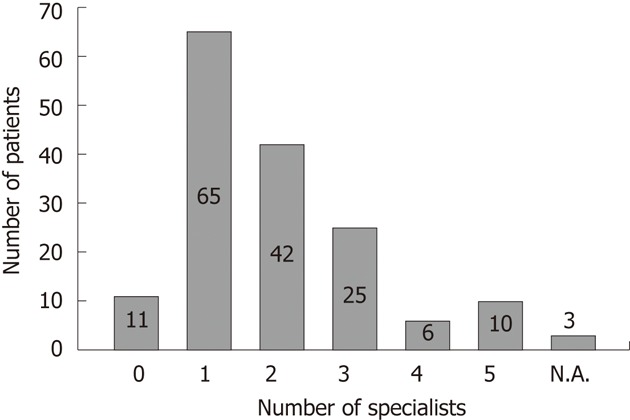
Number of changes in specialist ever by each patient. N.A.: Not available.
IBD patients with four or more changes in specialists had lower median quality of life scores (sIBDQ10, median score 37 vs 48 respectively, P = 0.01) and higher disease activity scores (median score 2.75 vs 2.28 respectively, P = 0.04) than those with a lower number of changes over their total duration of IBD.
Recent change in specialist
In order to identify temporal associations with changing specialist, bivariable (Table 2) then multivariable logistic regression analyses were conducted with the endpoint of specialist change within 12 mo prior to survey completion. The multivariable model (incorporating associations from bivariable analyses where P ≤ 0.05 plus age) showed those with a recent change were more likely to have Crohn’s disease, had recent hospitalization, had a past bowel resection, and trended towards having currently active disease (Table 3).
Table 2.
Bivariable logistic regression analyses of relevant clinical and demographic factors potentially associated with a change in treating specialist
|
Associated with change in treating specialist within 12 mo of survey completion |
Associated with change in specialist for a "negative" reason at any time |
|||
| Variable | OR [95% CI] | P value | OR [95% CI] | P value |
| Age under 30 | 1.13 [0.52, 2.47]5 | 0.015 | 0.60 [0.25, 1.46] | 0.33 |
| Female gender | 1.15 [0.59, 2.24] | 0.73 | 1.57 [0.71, 3.49] | 0.31 |
| Crohn’s as inflammatory bowel diseases diagnosis | 2.03 [1.03, 4.03]5 | 0.045 | 0.79 [0.35, 1.78] | 0.68 |
| Recent inpatient admission3 | 1.70 [0.86, 3.35]5 | 0.135 | 0.82 [0.37, 1.82] | 0.69 |
| Previous bowel resection surgery1 | 3.23 [7.81, 1.41]5 | 0.0055 | 0.61 [0.27, 1.38] | 0.28 |
| Moderate/severe disease activity4 | 2.09 [1.06, 4.12]5 | 0.045 | 0.96 [0.43, 2.15] | 0.93 |
| Polypharmacy2 | 1.09 [0.51, 2.36] | 0.85 | 1.50 [0.57, 3.97] | 0.49 |
| Living alone | 1.06 [0.54, 2.07] | 1.0 | 1.59 [0.71, 3.57] | 0.31 |
| Low socioeconomic status | 1.62 [0.75, 3.48] | 0.26 | 1.33 [0.53, 3.36] | 0.66 |
| Limited employment status | 1.09 [0.52, 2.28] | 0.85 | 0.65 [0.29, 1.49] | 0.37 |
| Poor inflammatory bowel diseases knowledge | 0.39 [0.18, 0.88]5 | 0.035 | 2.04 [0.90, 4.55]5 | 0.125 |
| Poor medication adherence | 1.22 [0.62, 2.40] | 0.60 | 2.22 [0.99, 4.95]5 | 0.065 |
| Poor HRQoL | 1.20 [0.57, 2.49] | 0.71 | 0.91 [0.37, 2.24] | 1.0 |
| Possible psychological disorder (HADS > 7) | 1.13 [0.58, 2.20] | 0.74 | 0.75 [0.34, 1.68] | 0.55 |
| Dissatisfaction with medical care | 0.95 [0.47, 1.90] | 1.0 | 2.39 [1.05, 5.42]5 | 0.045 |
At any time in the past;
taking ≥ 6 prescription medications currently;
in observation period between January 1, 2007-April 31, 2008;
as determined by physician global assessment at time of survey;
Table 3.
Factors associated with change of treating specialist within 12 mo of survey completion - multivariable logistic regression analysis results
| Variable | OR [95% CI] | P value |
| Crohn’s disease as IBD diagnosis | 2.60 [1.25, 5.41] | 0.01 |
| Age1 | 0.98 [0.97, 0.99] | 0.01 |
| Previous bowel resection surgery2 | 5.56 [1.92, 16.67] | 0.002 |
| Recent inpatient admission3 | 1.97 [1.29, 3.01] | 0.002 |
| Moderate/severe disease activity4 | 2.16 [0.99, 4.71] | 0.05 |
For every one year increase in age;
at any time in the past;
within observation period between 2007-April 31, 2008;
as determined by physician global assessment at time of survey. OR: Odd ratio; 95% CI: 95% confidence interval; IBD: Inflammatory bowel diseases.
Patients reporting negative reasons for changing specialist
Thirty patients gave 34 negative reasons for changing specialist, including dissatisfaction with management (n = 23), lost confidence (n = 10) and personality clash (n = 1) (Figure 3). These 30 patients were generally younger (median, 35.2 years vs 45.3 years), had higher IBD knowledge (median, 5.0 score vs 4.0 score respectively), yet had lower medication adherence and satisfaction scores (median, 19.0 score vs 22.0, respectively, 14.0 score vs 16.0, respectively, Mann-Whitney, all P < 0.05) compared to all other responders (n = 132). There were no other statistically significant differences including no difference in disease duration, IBD-related characteristics, hospitalization outcomes, or QoL scores between patients changing for negative reasons and other responders (data not shown). However, the frequency of changing specialist [i.e. the duration (years) since IBD diagnosis divided by the total number of changes in specialist over the same period] trended towards being higher in those with one or more negative reasons for changing specialist, compared to other responders (median, 2.8 vs 4.0 years between each change, P = 0.06, Mann-Whitney).
Figure 3.
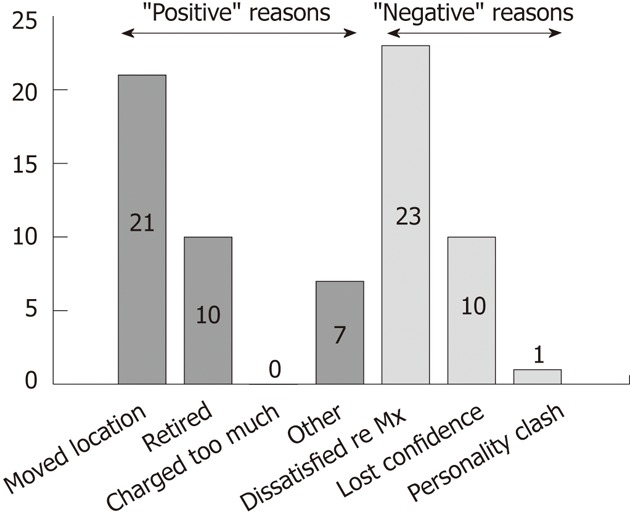
Reasons stated for patient change of treating specialist (72 reasons from 70 patients).
Finally, in order to identify factors associated with changing specialist for a negative reason, bivariable (Table 2) then multivariable logistic regression analyses were conducted where a negative reason for change in specialist was the dependent variable. The multivariable model (incorporating associations from bivariable analyses with P ≤ 0.05, plus sex) showed those with a negative reason had poorer medication adherence and trended towards being of male sex (Table 4).
Table 4.
Factors associated with change in specialist for a negative reason - multivariable logistic regression analysis results
| Variable | OR [95% CI] | P value |
| Female gender1 | 0.36 [0.13, 1.01] | 0.053 |
| Suboptimal satisfaction with medical care | 1.22 [0.40, 3.75] | 0.73 |
| Poor disease knowledge | 0.54 [0.20, 1.50] | 0.24 |
| Poor medication adherence1 | 3.49 [1.12, 10.89] | 0.03 |
Variables indicate those statistically, significantly associated with a negative reason for change in specialist. OR: Odd ratio; 95% CI: 95% confidence interval.
DISCUSSION
Accepted IBD dogma dictates that expert specialist care is vital in optimizing outcomes, as per recent IBD consensus guidelines[18,19]. However, these guidelines do not specifically address continuity of care or patient satisfaction with their PDR. Moreover, the United Kingdom IBD Standards Group emphasizes the importance of maintaining patient-centered care (Standard C), “offering personalized and responsive healthcare so that any patient can migrate between models of care according to activity and complexity of disease, local facilities and personal preference[20]. In this prospectively encountered IBD cohort, we showed that patients frequently changed treating specialist (43.2% of responders) and of these, many changed (42.9%) for negative reasons, which appears to represent a high prevalence of discordant/poor PDR, which has not previously been documented. Suboptimal PDRs and/or discontinuity of care appear to impair QoC[18], therefore, clinicians (for both the sake of the patient and retaining their own practice) should be cognizant of and, wherever possible, endeavor to address when and why this discord exists[21].
Quantifying PDRs is inherently difficult, however assessing past and hence, risk of future changes in treating specialist via patient self-report is a novel, tangible method of surrogately measuring patient satisfaction with the PDR and their medical care. Increasingly, health providers are utilizing patient feedback via satisfaction questionnaires as a means to establish a patient-centered approach and for evaluating and improving quality performance[22,23]. In IBD, this has led to development of a limited number of disease-specific satisfaction questionnaires such as the comprehensive QUOTE-IBD survey[24] and others such as the Treatment Satisfaction Questionnaire for Crohn’s disease[25]. Given the lack of brief but validated surveys focusing on specialist care in IBD, an unvalidated four-item survey was used in this study[9]. Further refinement and validation of this and similar surveys are needed, whereupon specialists may utilize these in routine practice as a means to identify and address problems with patient dissatisfaction and thus potentially enhance the PDR, and hence quality of care[26].
We thus examined the data to identify characteristics of patients likely to opt for change. Patient factors temporally associated with a recent change, accepting these associations may not be causal, although nevertheless potentially modifiable, include higher disease activity, diagnosis of Crohn’s disease, and previous surgery. We believe that these adverse disease factors may jeopardize patient satisfaction and the PDR. In this context, subsequent hospitalization may be the “final straw” in an already vulnerable PDR, prompting a patient-initiated change[10]. Additionally, given all patients were identified via a recent hospital encounter at the study centre (RAH), this encounter may have resulted in a sample biased towards those provided with an opportunity to change IBD specialist, given that their inpatient care may have been conducted by a different treating specialist than their usual doctor. However as mentioned, one-third of the cohort continued seeing a treating specialist external/unaffiliated to the study hospital at the time of survey.
Indeed, the data may also reflect societal changes. First, patient care is increasingly often disjointedly administered across multiple primary care, hyper-specialized and provider-specific boundaries[5]. This frequently tests the ability of health systems to ensure a seamless flow of clinical information and correspondence responsive to patient transitions between health providers, especially where larger institutions are involved[27,28]. For instance, a gastroenterologist with a solely community-based practice caring for a patient who suffers an IBD flare may remain unaware when their patient is admitted to a tertiary hospital, and conversely the hospital staff may not be aware of the treating specialist’s long-term relationship with the patient. Post-discharge follow-up may then be routinely arranged in the hospital-based IBD clinic instead of the private gastroenterologist’s rooms. Hence, depending on the patient’s own initiative, a “system-induced change” in specialist may occur, resulting in a loss of continuity of care and potentially, reduced patient satisfaction and jeopardized QoC. Second, consumer expectations of doctors and health outcomes, congruent with medical technological advances, continue to escalate, thus conceivably, patients do (and will) change specialists more readily than ever before[5,29]. Finally, there is a consumer perception that larger entities (e.g., large department stores analogous to large hospitals) offer better products, more conveniently at a lower cost which may also drive patient-initiated changes[30].
Interestingly, we also found that patients with superior IBD knowledge appeared more likely to change specialists. Potentially, knowledgeable IBD patients who expect to participate in management decisions, desire a patient-centered emphasis within the PDR, otherwise this unmet need may drive patients to change specialist[10,31]. Moreover, given those with negative reasons generally exhibited lower adherence again underlines potential disadvantages of a discordant PDR, although these data cannot ascertain whether this discord elicits nonadherence or vice versa. Hence, these patients may be deemed at risk of future adverse disease outcomes in the context of nonadherence, which is unlikely to be salved by changing specialist[21,32].
Regardless in many ways, the patient’s self-reported reasons for changing specialist may over-simplify the complex interplay of patient beliefs and expectations, their underlying illness and the PDR, resulting in the change. Hence the fact that the change occurred, rather than the stated reason may be more relevant to consider. For instance, we showed that patients with four or more changes for any reason had lower QoL scores, yet there was no statistically significant difference between patients stating a negative reason for changing specialist and other responders. Thus, the prevalence and frequency of changes (regardless of reason or timing) warrant attention so as to determine whether these lead to increased risk of adverse outcomes via disjointed care and underlying dissatisfaction, and whether these outcomes are potentially preventable. Possible avenues begin with the specialist, including engendering patient involvement in clinical decision making and self-empowerment[33], patient-friendly doctor-patient communication, and regular opportunities for patients to provide feedback on their care received[34,35]. Furthermore, patients suspected of medication nonadherence must be sensitively confronted and efforts made to rectify this as previously documented elsewhere[36,37]. Also, fail-safe systems of timely referral and correspondence between health providers must be instituted in order to prevent loss to treating specialist follow-up and discontinuity of care, which often may occur during times of disease deterioration where continuity and high QoC may in fact be most needed[20,38]. Indeed, in occasional scenarios where a discordant PDR is irreconcilable, and upon mutual agreement between doctor and patient, patients may ultimately benefit from referral on to alternative colleagues or services for ongoing care[39].
In conclusion, in this novel study, we demonstrated that a patient-initiated change in treating specialist in IBD occurs frequently and appears temporally associated with adverse disease traits. Continuity of care, within a positive PDR, is an important element of high-quality care, thus, we recommend that treating specialists should monitor their patients for history and future risk of changing specialists. In view of the recent genesis of national standards in the United Kingdom and United States[20,40], we recommend that continuity of care and institution of efficient, fail-safe referral mechanisms are included as markers of quality in IBD. Adopting a patient-centered approach to IBD management, regularly surveying patient satisfaction and maintaining best practice therapeutic strategies, may result in durable benefits to both patients and doctors alike, although proven formulae to minimize avoidable change in specialist and maintain positive PDRs require further evaluation.
COMMENTS
Background
Inflammatory bowel diseases (IBD) is typically an unpredictable, relapsing- remitting condition and thus patient satisfaction and a robust patient-doctor relationship (PDR) are fundamental to high quality care. Conversely however, relational discord between patient and doctor may compromise quality of care (QoC), leading to adverse outcomes. Thus, in this study, we aimed to explore whether patients changed treating specialists as a tangible marker of patient satisfaction with the PDR and their medical care.
Research frontiers
In the 21st century, patient-centered care is integral in chronic disease management. Measuring patient satisfaction is an important component of ensuring a high standard of care delivery. A compromised PDR, and therefore, QoC, may result in inferior disease outcomes.
Innovations and breakthroughs
A patient-initiated change in treating specialist represents a vulnerable moment in delivery of care but also is a surrogate, tangible measure of patient satisfaction. By establishing factors associated with a change in specialist, one may better understand to what extent these are preventable, and/or how these are best identified so as to minimize disruptions to QoC, thus avoiding adverse outcomes.
Applications
Monitoring patient satisfaction is important to maintain continuity of care and therefore quality. Ensuring failsafe referral and follow-up mechanisms, especially in times of IBD relapse may reduce contemporaneous changes in specialists, thus ultimately improving outcomes for patients.
Peer review
This is an interesting study that sheds some light on the nature and complexity of the PDR in IBD patients. Given the importance of a positive PDR in IBD, such a study is necessary to understand the full dynamics of that relationship. The manuscript should be a good addition to the existing literature on the subject.
Footnotes
Peer reviewer: Tedros Bezabeh, PhD, Senior Research Officer, Institute for Biodiagnostics, National Research Council, 435 Ellice Avenue, Winnipeg, Manitoba R3B 1Y6, Canada
S- Editor Gou SX L- Editor Kerr C E- Editor Xiong L
References
- 1.Kaplan SH, Greenfield S, Ware JE. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 2.Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20:953–957. doi: 10.1111/j.1525-1497.2005.0178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gray JR, Leung E, Scales J. Treatment of ulcerative colitis from the patient’s perspective: a survey of preferences and satisfaction with therapy. Aliment Pharmacol Ther. 2009;29:1114–1120. doi: 10.1111/j.1365-2036.2009.03972.x. [DOI] [PubMed] [Google Scholar]
- 4.Pereira AG, Kleinman KP, Pearson SD. Leaving the practice: effects of primary care physician departure on patient care. Arch Intern Med. 2003;163:2733–2736. doi: 10.1001/archinte.163.22.2733. [DOI] [PubMed] [Google Scholar]
- 5.Alexander GC, Lantos JD. The doctor-patient relationship in the post-managed care era. Am J Bioeth. 2006;6:29–32. doi: 10.1080/15265160500394556. [DOI] [PubMed] [Google Scholar]
- 6.Murphy J, Chang H, Montgomery JE, Rogers WH, Safran DG. The quality of physician-patient relationships. Patients’ experiences 1996-1999. J Fam Pract. 2001;50:123–129. [PubMed] [Google Scholar]
- 7.Meredith LS, Orlando M, Humphrey N, Camp P, Sherbourne CD. Are better ratings of the patient-provider relationship associated with higher quality care for depression? Med Care. 2001;39:349–360. doi: 10.1097/00005650-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Richardson WCB, Bisgard DM, Bristow JC, Buck LR, Cassel CR, Chassin CK, Chassin MR. Crossing the Quality Chasm: A New Health System for the 21st Century. In: Committee on Quality Health Care in America IoM., editor. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 9.van Langenberg DR, Lange K, Hetzel DJ, Holtmann GJ, Andrews JM. Adverse clinical phenotype in inflammatory bowel disease: a cross sectional study identifying factors potentially amenable to change. J Gastroenterol Hepatol. 2010;25:1250–1258. doi: 10.1111/j.1440-1746.2010.06302.x. [DOI] [PubMed] [Google Scholar]
- 10.Safran DG, Montgomery JE, Chang H, Murphy J, Rogers WH. Switching doctors: predictors of voluntary disenrollment from a primary physician’s practice. J Fam Pract. 2001;50:130–136. [PubMed] [Google Scholar]
- 11.Sostegni R, Daperno M, Scaglione N, Lavagna A, Rocca R, Pera A. Review article: Crohn’s disease: monitoring disease activity. Aliment Pharmacol Ther. 2003;17 Suppl 2:11–17. doi: 10.1046/j.1365-2036.17.s2.17.x. [DOI] [PubMed] [Google Scholar]
- 12.Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1:514. doi: 10.1016/s0140-6736(80)92767-1. [DOI] [PubMed] [Google Scholar]
- 13.Leong RW, Lawrance IC, Ching JY, Cheung CM, Fung SS, Ho JN, Philpott J, Wallace AR, Sung JJ. Knowledge, quality of life, and use of complementary and alternative medicine and therapies in inflammatory bowel disease: a comparison of Chinese and Caucasian patients. Dig Dis Sci. 2004;49:1672–1676. doi: 10.1023/b:ddas.0000043384.26092.f4. [DOI] [PubMed] [Google Scholar]
- 14.Eaden JA, Abrams K, Mayberry JF. The Crohn’s and Colitis Knowledge Score: a test for measuring patient knowledge in inflammatory bowel disease. Am J Gastroenterol. 1999;94:3560–3566. doi: 10.1111/j.1572-0241.1999.01536.x. [DOI] [PubMed] [Google Scholar]
- 15.Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996;91:1571–1578. [PubMed] [Google Scholar]
- 16.Ediger JP, Walker JR, Graff L, Lix L, Clara I, Rawsthorne P, Rogala L, Miller N, McPhail C, Deering K, et al. Predictors of medication adherence in inflammatory bowel disease. Am J Gastroenterol. 2007;102:1417–1426. doi: 10.1111/j.1572-0241.2007.01212.x. [DOI] [PubMed] [Google Scholar]
- 17.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 18.Elkjaer M, Moser G, Reinisch W, Durovicova D, Lukas M, Vucelic B, Wewer V, Frederic Colombel J, Shuhaibar M, O’Morain C, et al. IBD patients need in health quality of care ECCO consensus. J Crohns Colitis. 2008;2:181–188. doi: 10.1016/j.crohns.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Carter MJ, Lobo AJ, Travis SP. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53 Suppl 5:V1–16. doi: 10.1136/gut.2004.043372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arnott I, Bloom S, Edwards C, Hawkey C, Leiper K, Shaw I, Travis S. Nicholls J, Northover J, Shorthouse A, Rubin G, Croft N, Mitton S, Lomer M, Nightingale A, Mason I, Younge L, Driscoll R. IBD Standards Working Group. Quality care: service standards for the healthcare of people who have Inflammatory Bowel Disease (IBD); 2009. [Google Scholar]
- 21.Street RL, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6:198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 23.Zemencuk JK, Hayward RA, Skarupski KA, Katz SJ. Patients’ desires and expectations for medical care: a challenge to improving patient satisfaction. Am J Med Qual. 1999;14:21–27. doi: 10.1177/106286069901400104. [DOI] [PubMed] [Google Scholar]
- 24.van der Eijk I, Sixma H, Smeets T, Veloso FT, Odes S, Montague S, Fornaciari G, Moum B, Stockbrügger R, Russel M. Quality of health care in inflammatory bowel disease: development of a reliable questionnaire (QUOTE-IBD) and first results. Am J Gastroenterol. 2001;96:3329–3336. doi: 10.1111/j.1572-0241.2001.05334.x. [DOI] [PubMed] [Google Scholar]
- 25.Coyne K, Joshua-Gotlib S, Kimel M, Thompson C, Lewis A, Danilewitz M. Validation of the treatment satisfaction questionnaire for Crohn’s disease (TSQ-C) Dig Dis Sci. 2005;50:252–258. doi: 10.1007/s10620-005-1591-3. [DOI] [PubMed] [Google Scholar]
- 26.Goldring AB, Taylor SE, Kemeny ME, Anton PA. Impact of health beliefs, quality of life, and the physician-patient relationship on the treatment intentions of inflammatory bowel disease patients. Health Psychol. 2002;21:219–228. doi: 10.1037//0278-6133.21.3.219. [DOI] [PubMed] [Google Scholar]
- 27.Kappelman MD, Palmer L, Boyle BM, Rubin DT. Quality of care in inflammatory bowel disease: a review and discussion. Inflamm Bowel Dis. 2010;16:125–133. doi: 10.1002/ibd.21028. [DOI] [PubMed] [Google Scholar]
- 28.Rittenhouse DR, Shortell SM, Gillies RR, Casalino LP, Robinson JC, McCurdy RK, Siddique J. Improving chronic illness care: findings from a national study of care management processes in large physician practices. Med Care Res Rev. 2010;67:301–320. doi: 10.1177/1077558709353324. [DOI] [PubMed] [Google Scholar]
- 29.Johns Hopkins, American Healthways. Defining the patient-physician relationship for the 21st century. Dis Manag. 2004;7:161–179. doi: 10.1089/dis.2004.7.161. [DOI] [PubMed] [Google Scholar]
- 30.Wachter RM, Shojania KG. The unintended consequences of measuring quality on the quality of medical care. N Engl J Med. 2000;342:520. [PubMed] [Google Scholar]
- 31.Garman AN, Garcia J, Hargreaves M. Patient satisfaction as a predictor of return-to-provider behavior: analysis and assessment of financial implications. Qual Manag Health Care. 2004;13:75–80. doi: 10.1097/00019514-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Nguyen GC, LaVeist TA, Harris ML, Datta LW, Bayless TM, Brant SR. Patient trust-in-physician and race are predictors of adherence to medical management in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1233–1239. doi: 10.1002/ibd.20883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baars JE, Markus T, Kuipers EJ, van der Woude CJ. Patients’ preferences regarding shared decision-making in the treatment of inflammatory bowel disease: results from a patient-empowerment study. Digestion. 2010;81:113–119. doi: 10.1159/000253862. [DOI] [PubMed] [Google Scholar]
- 34.Richards T. Patients’ priorities. BMJ. 1999;318:277. doi: 10.1136/bmj.318.7179.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schattner A, Bronstein A, Jellin N. Information and shared decision-making are top patients’ priorities. BMC Health Serv Res. 2006;6:21. doi: 10.1186/1472-6963-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kane SV. Strategies to improve adherence and outcomes in patients with ulcerative colitis. Drugs. 2008;68:2601–2609. doi: 10.2165/0003495-200868180-00006. [DOI] [PubMed] [Google Scholar]
- 37.Lakatos PL. Prevalence, predictors, and clinical consequences of medical adherence in IBD: how to improve it? World J Gastroenterol. 2009;15:4234–4239. doi: 10.3748/wjg.15.4234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roy MJ, Herbers JE, Seidman A, Kroenke K. Improving patient satisfaction with the transfer of care. A randomized controlled trial. J Gen Intern Med. 2003;18:364–369. doi: 10.1046/j.1525-1497.2003.20747.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pilowsky I. Disagreement between patient and doctor: implications for diagnosis and management. Aust Fam Physician. 1980;9:580–584. [PubMed] [Google Scholar]
- 40.American Gastroenterological Association. Adult inflammatory bowel disease physician performance measures set. 2011. [Google Scholar]