Abstract
AIM: To study knowledge levels and attitudes of health care providers toward patients with hepatitis C virus infection in Guilan, a northern province of Iran.
METHODS: This cross-sectional study was performed on 239 health care professionals from the Razi Hospital, including doctors, nurses, and operating room technicians. The questionnaires consisted of questions on demographic characteristics, knowledge levels, and attitudes toward hepatitis C patients. The questionnaire was tested in a pilot study and validated by Cronbach’s alpha coefficient. Data were analyzed using SPSS16 software.
RESULTS: The mean ± SD knowledge score was 17.43 ± 2.65 (from a total of 22). 51.9% of the participants achieved scores higher than the mean. There was a significant relationship between knowledge score and age (P = 0.001), gender (P = 0.0001), occupational history (P = 0.0001), and educational history (P = 0.027). There was also a significant relationship between attitude level and age (P = 0.002), gender (P = 0.0001), occupational history (P = 0.0001), and educational history (P = 0.035). Physicians were significantly more knowledgeable and showed more positive attitudes. There was a positive correlation between knowledge and attitude scores (P = 0.02).
CONCLUSION: Discriminatory attitudes are common among health care providers toward hepatitis C patients. It is therefore necessary to improve their knowledge level and attitude toward this disease.
Keywords: Knowledge, Attitude, Hepatitis C, Health professional, Patient care
INTRODUCTION
Hepatitis C is a hepatotropic viral infection caused by hepatitis C virus (HCV), which is a major cause of acute hepatitis and chronic liver disease. It is estimated that 170 million people worldwide (3% of the world population) are chronically infected with HCV and are under the risk of cirrhosis and liver cancer. Chronic HCV infection is usually slowly progressive. HCV infection leads to chronic hepatitis in 50% to 80% of individuals[1-5]. The increasing global prevalence of this disease puts extra demands on health care services and increases the likelihood that health care workers (HCWs) will care for, or have personal contact with, people with hepatitis C[6]. Occupational exposure from percutaneous injuries is a substantial source of infection by blood borne pathogens among HCWs. However, studies of HCWs exposed to HCV by a needle stick injury (NSI), or any other percutaneous injury, have found that the incidence of anti HCV seroconversion is 1.8% (0%-7%) on average[7]. Physicians, laboratory technicians, nurses, and dialysis unit personnel are the main HCWs at risk. Nurses are the most at risk group because they have close contact with patients and are more likely to be exposed to a NSI[8].
NSIs are common in our country. In a study in Qazvin, 52.9% of nurses had a history of NSI[9]. Patients with hepatitis C have met with discrimination and stigmatization in the work place, by family members and by members of their communities. In addition, they may face discrimination from HCWs[10,11]. The discriminatory practices of HCWs may result from a lack of knowledge and negative attitudes toward these kinds of diseases, which could interfere with their willingness to treat these patients because of a fear of contracting hepatitis C. In a study by Richmond et al[6], most health care workers had sufficient knowledge about hepatitis C; however, some of them showed discriminatory attitudes toward patients with hepatitis C. Until now, little research has been conducted on HCW knowledge levels and attitudes toward people with hepatitis C in Iran. We therefore studied HCW knowledge levels and attitudes toward treating people with hepatitis C as a blood borne disease, to investigate how attitudes can be influenced by education and how this can affect their willingness to treat these patients.
MATERIALS AND METHODS
A cross-sectional study was conducted using a questionnaire that was created and standardized by Richmond et al[6] and translated into Persian. The questionnaire was considered by a panel of consulting experts and its validity was documented by a pilot study using a random sample (n = 20) drawn from the subgroups to be surveyed in the main study. The sample was calculated as 345 health care workers, based on the positive attitude proportion among the random subgroup (32%) and considering the precision of 0.06 and the type one error of 0.05. The questionnaire’s validity and reliability were also confirmed by Cronbach’s alpha coefficient (alpha = 0.7). We used this specifically designed questionnaire for the study because no other instrument was identified that explored HCW attitudes toward treating people with hepatitis C in the detail that was required for the current research. The questionnaire consisted of four parts and 49 questions. Seven questions obtained demographic characteristics, 22 questions were used to explore knowledge levels, 10 questions determined attitudes, and 10 questions were designed to determine compassion levels toward hepatitis C patients, willingness to treat hepatitis C patients, their self reported fear of contracting hepatitis C, and their self reported behavior toward injecting drug users. The mean of the total score from a possible score of 22, based on 22 questions, was used as the discriminant level. Scores higher than the mean indicated a good knowledge level and lower than the mean indicated a poor knowledge level[12].
Regarding attitude, participants were asked to what extent they agreed or disagreed (using a five-point Likert scale ranging from “strongly agree” to “strongly disagree”) with each of the statements. For the 10 statements, total scores that could be achieved ranged from 10 to 50. Scores between 10 and 30 were considered as negative attitudes and scores higher than 30 were considered as positive attitudes[13,14]. The knowledge level, attitude questions, and self-behavior statements are shown in Table 1. Demographic data containing participants’ age, sex, working history (years which health care workers had worked for health care service), occupation (doctor, nurse), needle stick injury (NSI) history, education (participation in education classes on NSI), were registered for each participant. Questionnaires were filled by direct interviews, which were performed by a trained general practitioner from the research team.
Table 1.
Hepatitis C knowledge level, attitude and self-reported statement questions in the questionnaire
| Hepatitis C knowledge questions (response options: true, false and uncertain) |
| Hepatitis C is caused by a virus |
| Hepatitis C is caused by bacteria |
| Hepatitis C can be spread through close personal contact such as kissing |
| Hepatitis C can be spread through sharing injecting equipment, such as needles, tourniquets, spoons, filters and swabs |
| Hepatitis C can be spread by mosquitoes |
| Hepatitis C is spread through blood-to-blood contact |
| Having a medical and/or dental procedure performed in the Middle East, South East Asia or the Mediterranean increases a person's chances of contracting hepatitis C |
| Hepatitis C is spread through the air in an enclosed environment (e.g., crowded buses and elevators) |
| Sexual transmission is a common way hepatitis C is spread |
| Some people with hepatitis C were infected through unsterile tattooing |
| Some people with hepatitis C were infected through blood transfusions |
| People with hepatitis C should be restricted from working in the food industry |
| Hepatitis C can lead to cirrhosis |
| Hepatitis C is associated with an increased risk of liver cancer |
| Hepatitis C is a mutation of hepatitis B |
| A person can be infected with hepatitis C and not have any symptoms of the disease |
| There is a pharmaceutical treatment available for hepatitis C |
| There is a vaccine for hepatitis C |
| HIV is easier to catch than hepatitis C |
| An individual can have hepatitis C antibodies without being currently infected with the virus |
| People with hepatitis C should restrict their alcohol intake |
| Once you have had hepatitis C, you cannot catch it again because you are immune |
| Attitudes and self-reported behavior statements according to theme (response options: strongly agree, agree, uncertain, disagree and strongly disagree) |
| Attitudes and self-reported behavior toward the implementation of infection control guidelines |
| When receiving health care, patients with hepatitis C (HCV) should be identified for safety reasons |
| Patients with HCV should be given the last appointment for the day (ICG) |
| Health professionals who are HCV positive should be discouraged from having contact with patients |
| All patients should be tested for HCV before they receive health care |
| I deliver the same standard of care to patients with HCV as I do for other patients |
| I feel that I do not have the skills needed to effectively and safely treat patients with HCV |
| Following infection control guidelines will protect me from being infected with HCV at work |
| I often use additional infection control precautions when treating patients with HCV |
| I would prefer to wear two pairs of gloves when treating a bleeding person with HCV |
| The infection control guidelines necessary to treat patients with hepatitis C would be a financial burden on my practice/ward |
| Attitudes and self-reported compassion toward people with hepatitis C |
| I feel sorry for people who contracted HCV through a blood transfusion |
| I feel sorry for people who contracted HCV through HIV drug use |
| Attitudes and self-reported willingness to treat people with hepatitis C |
| I do not like treating people with HCV |
| I am willing to treat people with HCV |
| I believe my profession should have central role in the treatment of HCV |
HIV: Human immunodeficiency virus; HCV: Hepatitis C virus; ICG: International crisis group.
Statistical analysis
Data were entered into SPSS 16 software and analyzed by descriptive statistics (i.e., mean, SD, frequency) and comparison means (i.e., one way ANOVA, χ2 test). A P value less than 0.05 was considered statistically significant.
RESULTS
Response rate and demographic data
The mean age of the participants was 33.06 ± 7.72 years and the mean working history was 7.51 ± 6.49 years. The overall response rate was 69% (239 of 345 HCWs). There was no significant difference between the age, sex, occupation, and working history of responders and non-responders. Table 2 presents the demographic data. Overall, 52.3% of the participants reported having a history of NSI with hepatitis C patients.
Table 2.
Health care workers’ demographic data
| Variable | n (%) | |
| Age (yr) | ≤ 30 | 108 (45.2) |
| 31-40 | 88 (36.8) | |
| ≥ 41 | 43 (18.0) | |
| Sex | Male | 47 (19.7) |
| Female | 192 (80.3) | |
| Working history (yr) | ≤ 5 | 117 (49) |
| 6-10 | 60 (25.1) | |
| ≥ 11 | 62 (25.9) | |
| Health care group | Physicians | 79 (33.1) |
| Nurses | 150 (62.8) | |
| Technicians | 10 (4.2) | |
| NSI history | Yes | 125 (52.3) |
| No | 114 (47.7) | |
| Education | Yes | 189 (79.1) |
| No | 50 (20.9) |
NSI: Needle stick injury.
Nurses (54%) were most likely to have a history of NSI. Most of the HCWs (79.1%) reported that they had received information on hepatitis C patients and NSI (although they did not refer to the type of education they had received). Nurses (85.3%) were significantly more likely to have received training on hepatitis C, while 72.2% of the physicians had received training and operating room technicians (40%) were the least likely to have received training (P = 0.001).
Hepatitis C knowledge level and education
Overall, HCW level of knowledge was satisfactory and the mean knowledge score was 17.43 ± 2.65 from a total score of 22. Scores higher than 17.43 indicated a good knowledge level and lower than 17.43 indicated a poor knowledge level. For example, 95.4% of the participants answered the questions about cirrhosis correctly, 97.5% knew that hepatitis C is contracted through blood contact, 95% knew that non-sterile tattoos are also a method of transmission, and 98.3% of HCWs knew that HCV can be spread through sharing injection equipment, such as needles, tourniquets, spoons, filters, and swabs. However, some deficits were identified in their knowledge level. For example, only 37.7% of HCWs answered correctly to the statement: Sexual contact is a common mode of transmission.
Only 54.8% knew that there are effective treatments for hepatitis C, 35.1% did not know, and 10% were not sure about it.
The mean knowledge score of males was 18.78 ± 2.12 and the mean knowledge score of physicians was 19.26 ± 1.97. Physicians were the most knowledgeable, while technicians were the least knowledgeable group (P = 0.0001). Those who were more than 30 years old were the least knowledgeable group among different professional groups (P = 0.0001) (Table 3). In this study, 55.6% of the HCWs who had received training had a good knowledge score, but only 38% of those who had not received training showed good scores (P = 0.027).
Table 3.
Health care workers’ hepatitis C knowledge scores in association with different variables (mean ± SD)
| Variables | n | Mean knowledge score (SD) | P value | |
| Sex | Male | 47 | 18.78 (2.12) | 0.0001 |
| Female | 192 | 17.1 (2.66) | ||
| Age | ≤ 30 | 108 | 16.75 (2.9) | 0.001 |
| 31-40 | 88 | 17.93 (2.22) | ||
| ≥ 41 | 43 | 18.13 (2.41) | ||
| Working history | ≤ 5 | 117 | 17.05 (2.97) | 0.073 |
| 6-10 | 60 | 17.6 (2.91) | ||
| ≥ 11 | 62 | 17.98 (2.54) | ||
| Professional group | Physicians | 79 | 19.26 (1.97) | 0.0001 |
| Nurses | 150 | 16.61 (2.51) | ||
| Technicians | 10 | 15.3 (1.25) | ||
| NSI history | Yes | 125 | 17.28 (2.81) | NS |
| No | 114 | 17.59 (2.45) |
NSI: Needle stick injury; NS: Not significant.
Attitudes and self-reported behaviors
In this sample, 159 HCWs (66.5%) showed negative attitudes (score = 10-30) and 80 HCWs (33.5%) showed positive attitudes (score = 31-50). Males who were over 40 years old and had a working history of more than 10 years were more likely to show positive attitudes toward patients with hepatitis C (P = 0.002 for both) (Table 4). In the physicians group, 55.7% showed positive attitudes and, in the nurses group, 24% showed positive attitudes. Physicians were significantly more positive (P = 0.0001). All of the technicians showed negative attitudes. Those who received training also showed significantly more positive attitudes (P = 0.035).
Table 4.
Association of health care workers’ attitudes with different variables
| Variables | P value |
| Sex | 0.0001 |
| Age | 0.002 |
| Working history | 0.002 |
| Professional group | 0.0001 |
| NSI history | NS |
| Education | 0.035 |
| Knowledge score | 0.0001 |
NSI: Needle stick injury; NS: Not significant.
HCWs who were weak in knowledge were more likely to show negative attitudes and those who were knowledgeable were more likely to show positive attitudes (P = 0.02. There was a positive correlation between knowledge score and attitude (r = 0.227, Figure 1).
Figure 1.
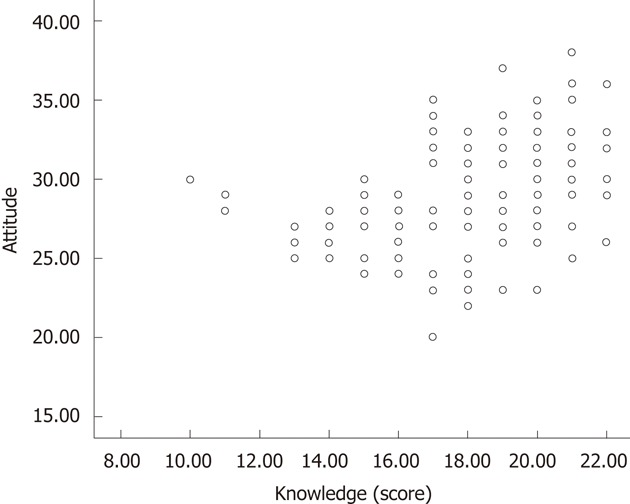
Pearson correlation between health care workers knowledge levels and attitudes.
Regarding attitude statements, 95.8% of the HCWs believed that hepatitis C patients should be identified for infection control purposes, 82.8% of the participants indicated that they used additional infection control precautions when they knew patients had hepatitis C; 74.4% were double-gloved when they treated a bleeding person with hepatitis C. 48.5% of the participants indicated that patients with hepatitis C should be given the last appointment of the day.
Compassion toward people with hepatitis C was measured in two statements (Table 1). Among the HCWs, 92.1% felt compassion when hepatitis C was acquired through a blood transfusion, compared with 55.6% when it was contracted through injection drug use. Participants’ willingness to care for people with hepatitis C was identified by responses to three questions (Table 1). Among HCWs, 82.8% believed that they liked to treat these patients and 15.5% said that they did not like treating these patients. Regarding attitudes toward intravenous (IV)-drug users, 78.7% showed fear toward IV-drug users, while 77% said that they were worried they might contract a disease from them. 35.6% believed that IV-drug users deserved the disease and 40.2% indicated that they did not want to treat IV-drug users. 26.8% believed that opiates should not be used for pain relief in patients with a history of injection drug use. There was an association between HCW knowledge level and fear of contracting a disease (P = 0.0001) and attitudes toward IV-drug users (P = 0.0001); however, there was no association between knowledge level and willingness to treat these patients. In addition, HCW attitudes toward IV-drug users emerged as a significant issue that affected willingness to treat people with hepatitis C (P = 0.035).
DISCUSSION
The total response rate in the present study was rather high compared to other studies on this issue[6,11,15]. In the present study, the reasons for not responding included not having enough time and not having enough interest. Some part of not having enough interest may have been because of incomplete knowledge on the issue.
In the current study, 49.4% of physicians and 54% of nurses had a history of NSI and the difference, unlike in Zafar’s study[16], was not significant. Vitale et al[17] and Wicker et al[18] reported a lower rate of NSI history. Perhaps the reason for the high rate of NSI among HCWs was not receiving enough practical education, HCW stress, or carelessness because of an increased workload.
HCWs are currently receiving training about blood borne diseases. In the present study, however, we did not refer to the contents and efficacy of training. Nurses in the current study were most likely to have received training, possibly because of their close contact with these patients and their greater interest in having a correct approach toward them.
In the current study, the mean knowledge level score was acceptable. Physicians were more knowledgeable than other groups. Richmond showed a significant relationship between medical groups and mean knowledge scores: doctors were the most knowledgeable group[6]. In the study by Shehab et al[19], the knowledge level of internal medicine residents on hepatitis was suboptimal. The higher knowledge level of physicians was likely because of more advanced and professional education on gastrointestinal and liver diseases.
In the present study, males and HCWs who were more than 40 years old were more knowledgeable. In Richmond’s study[6], HCWs who were 30-49 years old were the most knowledgeable and those above 40 were the least knowledgeable. This finding shows that older age and greater experience can be associated with greater knowledge. However, in elders, the efficacy of initial education decreases.
In the present survey, HCWs were insufficiently knowledgeable about the complications of hepatitis C. Sood et al[20] showed that more than half of the participants answered correctly to the questions about hepatitis C complications. In a study by Nicklin et al[21], half of the personnel indicated cirrhosis was caused by hepatitis C and 37% thought it caused liver cancer. In the present study, the knowledge about modes of transmission was also acceptable. In the studies of D’Souza et al[11] and van de Mortel et al[22], most of the participants indicated that blood transfusion is a major mode of transmission. However, some deficits were seen in HCW knowledge on sexual contact as a mode of transmission for hepatitis C.
In some prospective studies, in which the effect of HCW training on HCV knowledge was investigated, participants who received training showed significant advances in their knowledge levels[23-25]. Zdanuk et al[25] showed the same advances after receiving training. However, D’Souza et al[11] and Shehab et al[19] indicated that education did not produce any advance in knowledge levels. In the current study, education was introduced as an effective agent for developing HCW knowledge. However, we should not ignore the role of clinical practice as a form of education. For example, in Richmond’s survey, while complementary therapists were the group most likely to have been educated about hepatitis C, they were not the most knowledgeable[6]. In addition, in the current study, nurses were the most likely group to have been educated, but were not the most knowledgeable. Therefore, other factors must influence the knowledge level of HCWs. However, we should not deny the fact that the information presented cannot be effective if it has not been repeated and recorded in the mind. In some studies, it has been suggested that one method for getting better results is active and problem-based learning[6,20].
In the present study, attitude scores were significantly different among different groups (P = 0.0001). Physicians were the most positive group towards people with hepatitis C and technicians showed negative attitudes. This may be related to the fact that physicians were the most knowledgeable group and the better attitudes of males and elders reflect this, as these groups are mainly composed of physicians. Perhaps the positive attitudes are not related to age or experience.
Education had a significant influence on developing positive attitudes, which was also noted by van de Mortel[22] and Richmond et al[6]. However, it should be considered that HCW attitudes on hepatitis C patients might be influenced by the attitudes of colleagues. A problem associated with consulting colleagues is that the information provided could be inaccurate, outdated, or reflect just subjective clinical experiences about people with hepatitis C.
In the current study, most of the participants indicated willingness to treat patients with hepatitis C, as in the studies by Hu et al[26] in dentistry students and a study by van de Mortel[22].
The HCWs’ approach toward giving opiates to the IV-drug users for pain relief reflects deficits in their understanding of pain management and drug dependence. This also demonstrates the powerful influence of attitude on their clinical behavior. In the present study, some HCWs said that IV-drug users deserved to contract hepatitis C and this attitude was affected by their knowledge level and influenced their willingness to treat patients with hepatitis C. In addition, Richmond et al[6] showed that HCW willingness to treat patients with hepatitis C was significantly under the influence of their belief on injection drug users, rather than their knowledge of hepatitis C. This shows the role of social prejudice on self-reported behavior. Access to health services could be difficult for people with hepatitis C because HCWs believe that they are injection drug users[27].
Finally, as we expected, there was a significant correlation between HCW knowledge levels and attitudes (P = 0.0001). This finding was also reported in the studies of Richmond[6], Vitale et al[17] and van de Mortel[22]. We suggest that occupational experience and fear of contracting hepatitis C can also influence the willingness to treat people with hepatitis C.
This study had the advantage of direct interviews with the responders, and not just distributing the questionnaires among them. The response rate in the present study (69%) was higher than some other similar surveys[6,11,15]. However, some limitations should be noted. For example, like other similar studies, self-reported behavior was not validated against actual clinical behavior. Self-reported responses may not reflect responders’ actual attitudes[6].
In conclusion, we showed that discriminatory behaviors are common among HCWs towards patients with hepatitis C. Attitudes are directly under the influence of knowledge levels; therefore, it is necessary to increase the level and quality of training among HCWs to prevent discrimination and prejudice towards patients with hepatitis C.
ACKNOWLEDGMENTS
We would like to thank all the hospital staff that assisted us in this study.
COMMENTS
Background
Hepatitis C is a chronic prevalent liver infection worldwide which is caused by a blood borne pathogen (hepatitis C virus, HCV). Occupational exposure due to percutaneous injuries is a source of infection with this pathogen among health care workers. Because this group are in close contact with the patients with hepatitis C their knowledge and attitude toward the disease and the patients is so critical and can influence on their own health and their behavior toward the patients. This issue has not evaluated enough until now.
Research frontiers
In contacting with hepatitis C patients, prejudice and discrimination is so prevalent. The research hotspot is to evaluate health care workers' knowledge toward hepatitis C and its effect on their attitude toward the patients and this way lowering discrimination against the patients through improving the knowledge level among this critical group.
Innovations and breakthroughs
Until now no survey has investigated the association of knowledge and attitude of health care workers toward patients with hepatitis C in Iran, a country with high prevalence of the disease. In most of the previous surveys, the questionnaires were passively distributed among the participants. But the present study has the advantage of direct interviewing with the responders. Also the response rate in this study was much higher than some other similar investigations.
Applications
The present study showed that health care professionals’ attitude and behavior toward hepatitis C patients is directly under the influence of their knowledge and education on hepatitis C. So by increasing education on this issue maybe we can do something on the care given to the patients with hepatitis C.
Terminology
Hepatitis C: A viral liver infection caused by hepatitis C virus which can be transmitted by blood. This kind of hepatitis will usually end to chronic liver disease and cause cirrhosis; Knowledge: Mental perception and clearly realizing the information and learning; Attitude: Mental backgrounds which are achieved by experiences and can influence person's reactions and behaviors toward others and have close association with the personality.
Peer review
This is a good study which gives important information which could be used in improvement of the treatment of the hepatitis C patients. The survey reports the knowledge and attitudes of health care worker (HCW) impacting on the care given to patients with HCV. Their findings reflect on the significant relationship between attitude level and knowledge score, and various demographic factors of HCW. The study is well reported and holds significant value (on a regional level) towards the care of HCV patients.
Footnotes
Peer reviewers: Vladimir C Serafimoski, Professor, Clinic of Gastroenterohepatology, Medical Faculty, Skopje, Fyrom, Vodnjanska 17, 1000 Skopje, Macedonia; Arturo Panduro, MD, PhD, Head of the Department of Molecular Biology in Medicine, Civil Hospital of Guadalajara Fray Antonio Alcalde/University of Guadalajara, Hospital No. 278 S.H., Guadalajara, Jalisco 44280, Mexico
S- Editor Tian L L- Editor Stewart GJ E- Editor Xiong L
References
- 1.Gurubacharya DL, Mathura KC, Karki DB. Knowledge, attitude and practices among health care workers on needle-stick injuries. Kathmandu Univ Med J (KUMJ) 2003;1:91–94. [PubMed] [Google Scholar]
- 2.Mansour-Ghanaei F, Sadeghi A, Yousefi Mashhour M, Joukar F, Besharati S, Roshan Z, Khosh-Sorur M. Prevalence of hepatitis B and C infection in hemodialysis patients of Rasht (Center of Guilan Province, Northern Part of Iran) Hepatitis Monthly. 2009;9:45–49. [Google Scholar]
- 3.Waheed Y, Shafi T, Safi SZ, Qadri I. Hepatitis C virus in Pakistan: a systematic review of prevalence, genotypes and risk factors. World J Gastroenterol. 2009;15:5647–5653. doi: 10.3748/wjg.15.5647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ŁAbedzka H, Simon K, Gładysz A. Clinical and epidemiological assessment of hepatitis C virus infection among voluntary blood donors. Med Sci Monit. 2002;8:CR591–CR596. [PubMed] [Google Scholar]
- 5.Mastoi AA, Devrajani BR, Shah SZ, Rohopoto Q, Memon SA, Baloch M, Qureshi GA, Sami W. Metabolic investigations in patients with hepatitis B and C. World J Gastroenterol. 2010;16:603–607. doi: 10.3748/wjg.v16.i5.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richmond JA, Dunning TL, Desmond PV. Health professionals’ attitudes toward caring for people with hepatitis C. J Viral Hepat. 2007;14:624–632. doi: 10.1111/j.1365-2893.2007.00849.x. [DOI] [PubMed] [Google Scholar]
- 7.Bryant J. Organized systems of care. Am J Infect Control. 1997;25:363–364. doi: 10.1016/s0196-6553(97)90078-x. [DOI] [PubMed] [Google Scholar]
- 8.Ball J, Pike G. Needlestick injury in 2008 - Result from a survey of RCN members. London: Royal College of Nursing; 2008. [Google Scholar]
- 9.Mohammed N, Allami A, Malek Mohamadi R. Percutaneous exposure incidents in nurses: Knowledge, practice and exposure to hepatitis B infection. Hepat Mon. 2011;11:186–190. [PMC free article] [PubMed] [Google Scholar]
- 10.Reis C, Heisler M, Amowitz LL, Moreland RS, Mafeni JO, Anyamele C, Iacopino V. Discriminatory attitudes and practices by health workers toward patients with HIV/AIDS in Nigeria. PLoS Med. 2005;2:e246. doi: 10.1371/journal.pmed.0020246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D'Souza RF, Glynn MJ, Alstead E, Osonayo C, Foster GR. Knowledge of chronic hepatitis C among East London primary care physicians following the Department of Health’s educational campaign. QJM. 2004;97:331–336. doi: 10.1093/qjmed/hch060. [DOI] [PubMed] [Google Scholar]
- 12.Alemseged F, Tegegn A, Haileamlak A, Kassahun W. Caregivers' knowledge about childhood malaria in Gilgel Gibe field research center, south west Ethiopia. Ethiop J Health Dev. 2008;22:49–54. [PubMed] [Google Scholar]
- 13.Kermode M, Holmes W, Langkham B, Thomas MS, Gifford S. HIV-related knowledge, attitudes and risk perception amongst nurses, doctors and other healthcare workers in rural India. Indian J Med Res. 2005;122:258–264. [PubMed] [Google Scholar]
- 14.Sadeghi M, Hakimi H. Iranian dental students’ knowledge of and attitudes towards HIV/AIDS patients. J Dent Educ. 2009;73:740–745. [PubMed] [Google Scholar]
- 15.Jacoby D, St Louis T, Navarro V. Hepatitis C practice routines among Connecticut’s naturopathic physicians. Am J Gastroenterol. 2001;96:2801–2802. doi: 10.1111/j.1572-0241.2001.04148.x. [DOI] [PubMed] [Google Scholar]
- 16.Zafar A, Aslam N, Nasir N, Meraj R, Mehraj V. Knowledge, attitudes and practices of health care workers regarding needle stick injuries at a tertiary care hospital in Pakistan. J Pak Med Assoc. 2008;58:57–60. [PubMed] [Google Scholar]
- 17.Vitale F, Di Benedetto MA, Casuccio A, Firenze A, Calandra G, Ballarò F, Romano N. [The influence of professional degree on the knowledge of HIV, HBV and HCV infections in dentistry practice] Ann Ig. 2005;17:185–196. [PubMed] [Google Scholar]
- 18.Wicker S, Jung J, Allwinn R, Gottschalk R, Rabenau HF. Prevalence and prevention of needlestick injuries among health care workers in a German university hospital. Int Arch Occup Environ Health. 2008;81:347–354. doi: 10.1007/s00420-007-0219-7. [DOI] [PubMed] [Google Scholar]
- 19.Shehab TM, Sonnad S, Gebremariam A, Schoenfeld P. Knowledge of hepatitis C screening and management by internal medicine residents: trends over 2 years. Am J Gastroenterol. 2002;97:1216–1222. doi: 10.1111/j.1572-0241.2002.05708.x. [DOI] [PubMed] [Google Scholar]
- 20.Sood A, Midha V, Awasthi G. Hepatitis C--knowledge & amp; practices among the family physicians. Trop Gastroenterol. 2002;23:198–201. [PubMed] [Google Scholar]
- 21.Nicklin DE, Schultz C, Brensinger CM, Wilson JP. Current care of hepatitis C-positive patients by primary care physicians in an integrated delivery system. J Am Board Fam Pract. 1999;12:427–435. doi: 10.3122/jabfm.12.6.427. [DOI] [PubMed] [Google Scholar]
- 22.van de Mortel TF. Registered and enrolled nurses’ knowledge of hepatitis C and attitudes towards patients with hepatitis C. Contemp Nurse. 2003;16:133–144. doi: 10.5172/conu.16.1-2.133. [DOI] [PubMed] [Google Scholar]
- 23.D'Souza RF, Glynn MJ, Alstead E, Foster GR, Osonayo C. Improving general practitioners’ knowledge of chronic hepatitis C infection. QJM. 2004;97:549–550. doi: 10.1093/qjmed/hch092. [DOI] [PubMed] [Google Scholar]
- 24.Fischer LR, Conboy KS, Tope DH, Shewmake DK. Educating health professionals: a hepatitis C educational program in a health maintenance organization. Am J Manag Care. 2000;6:1029–1036. [PubMed] [Google Scholar]
- 25.Zdanuk S, Gimpel J, Uhanova J, Kaita KD, Minuk GY. The impact of medical informatics on the confidence of rural physicians caring for patients with chronic hepatitis C viral infections. Fam Pract. 2001;18:602–604. doi: 10.1093/fampra/18.6.602. [DOI] [PubMed] [Google Scholar]
- 26.Hu SW, Lai HR, Liao PH. Comparing dental students’ knowledge of and attitudes toward hepatitis B virus-, hepatitis C virus-, and HIV-infected patients in Taiwan. AIDS Patient Care STDS. 2004;18:587–593. doi: 10.1089/apc.2004.18.587. [DOI] [PubMed] [Google Scholar]
- 27.C-change: report of the enquiry into hepatitis C related discrimination. Sydney: Anti-Discrimination Board of New South Wales, 2001. Available from: http://www.lawlink.nsw.gov.au/lawlink/adb/ll_adb.nsf/pages/adb_hepatitis_c_enquiry.


