Abstract
Merkel cell carcinoma (MCC) is a relatively rare, polyomavirus associated, primary neuroendocrine carcinoma of the skin which is usually arising from dermal skin layers. However, the origin of MCC in the subcutaneous tissue is debatable. We report a 58-yearold female patient with an oedematous mass on her left groin that was firm in consistency and had no discoloration or other visible abnormality of the overlying skin. On histology and immunohistology the tumour was consistent with the diagnosis of MCC showing a predominant subcutanous growth pattern. Pelvic magnetic resonance tomography revealed a tumour conglomerate reaching from the subcutis of the left groin to the left paraaortal and parailiacal region indicating widespread lymphogenic metastisation. Despite complete medical work-up no other MCC primary could be detected. In conclusion, predominant subcutaneous growth pattern as well as tumour localization in the groin are uncommon features of MCC. MCC showing the aforementioned features may be associated with significant delay of diagnosis and therefore represents an unfavourable prognostic factor.
Introduction
Merkel cell carcinoma (MCC) is a relatively rare, polyomavirus associated, primary neuroendocrine carcinoma of the skin usually occurring on sun-exposed areas in elderly patients [1]. The typical clinical manifestation of MCC is that of a firm, nontender, cutaneous nodule with red-, purple-, or violet-coloured skin. It may display aggressive biological behaviour and can grow rapidly, metastasising to the regional lymph nodes and other organs such as liver, bones, lungs and brain [1,2]. In this report, we describe an unusual case of MCC clinically presenting as oedematous mass of the left groin.
Case Report
A 59-year-old woman presented with a painless mass of about 3 months duration in the left inguinal and vulval area. She had a 4-week history for a common iliac vein thrombosis of the left leg. The oedematous mass of the left groin was firm in consistency and had no discoloration or other visible abnormality of the overlying skin, except for a slight 'peau d'orange' appearance (Figure 1a). Pelvic magnetic resonance tomography revealed a tumour conglomerate reaching from the subcutis of the left groin to the left paraaortal and parailiacal region indicating widespread lymphogenic metastisation (Figure 1b). Neoplasms of the uro-genital regions were excluded by urologists and gynaecologists, respectively. A deep incisional skin biopsy was performed. Histological examination revealed a diffuse growth pattern with polygonal-epitheloid tumour cells of "naked" nuclei, coarse chromatin, and frequent mitotic features (Figure 2a). Tumour cells were aggregated in nests and complexes showing trabecular formation in the subcutis, and in part in the deep dermis. Immunohistochemically, the tumour cells were positive for cytokeratin 20 (Figure 2b) in a dot-like and crescentic perinuclear pattern and in a membranous pattern for CD56 along the cell borders. Additional staining for synaptophysin and Ki-67 (40%) was positive. The tumour cells were negative for cytokeratin 7, thyroid transcription factor 1, S100, and CD45. Merkel cell polyomavirus DNA was detected in lesional skin using single round LT3-PCR (309 bp), single round VP1PCR (352 bp) and by nested LT1/M1M2-PCR (179 bp). Computed tomography of the skull, chest and abdomen was unremarkable. Neuron-specific enolase and lactate dehydrogenase were significantly increased in the serum of the patient with 534 μg/l (< 16.3 μg/l) and 753 U/l (135-214 U/l), respectively. These findings were consistent with the diagnosis of metastazised MCC. The patient was treated with combined radiotherapy and chemotherapy (6 cycles eposide and carboplatin). Under this regimen, however, she developed disseminated cutaneous metastases on her left leg. Currently, she is being treated with liposomal doxo rubicine.
Figure 1.
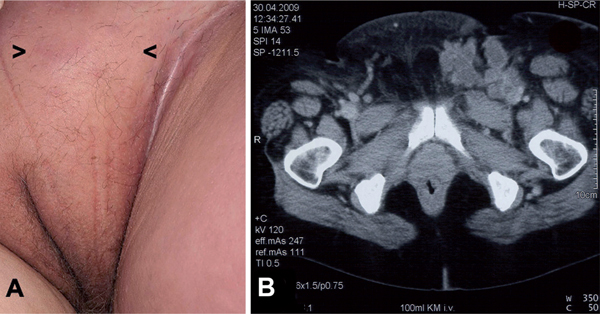
A firm mass in the left groin showing no discoloration or other visible abnormality of the overlying skin (A, arrow heads indicate were biopsy was taken). Pelvic magnetic resonance tomography revealed a widespread tumour conglomerate predominantly reaching from the subcutis of the left groin to the left paraaortal and parailiacal region (B).
Figure 2.
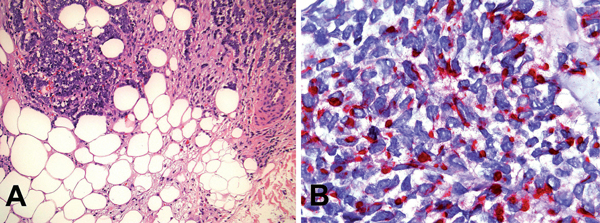
Haematoxylin and eosin staining (magnification, × 200) showing subcutaneous infiltrates consisting of small round tumour cells (A). A characteristic expression of cytokeratin 20 in a dot-like pattern is evident (B, magnification, × 200).
Discussion
MCC is mainly a dermal tumour consisting of cells that likely originate from immature totipotent stem cells and acquire neuroendocrine characteristics upon malignant transformation. The origin of MCC in the subcutaneous tissue is debatable. For example, Balaton et al. [3] previously reported the clinical and pathological features of three unusual soft tissue tumours which primarily affected the subcutaneous tissue in the groin of elderly patients. In case 1, the inguino-crural tumour coexisted with a second mass in the pelvis. The tumours had a tendency to relapse locally and to invade the regional lymph nodes. Metastatic dissemination of the disease resulted in death of one patient (case 3). Interestingly, routine histology and immunostainings were consistent with MCC. Primarily subcutaneous growth of MCC has also recently reported by Huang et al. [4] who reported a 63-year old woman with primary lesion of MCC that arose from the subcutaneous fat layer of the left arm. Moreover, there are reports on MCC of the inguinal lymph nodes with no identifiable primary site [5]. Likely these cases may however represent lymph node metastases from a regressed skin primary - a phenomenon which has sporadically been observed in patients with MCC [6]. In the present case of a primary MCC, a predominant subcutaneous growth pattern was observed. Lymphatic invasion of MCC is known to occur very early from nearly 40% of cases at the initial presentation to up to 90% in the post-excision phase [1,2]. Invasion of paraortal and parailiacal region in the present case could have contributed to common iliac vein thrombosis and hence oedema of the affected area, groin and subcutaneous tissue. Indeed, the clinical picture and anatomic location of the here presented MCC did not favour a diagnosis of MCC. However, the presence of the Merkel cell polyomavirus in lesional skin as well as the histological and immunohistological findings were consistent with MCC.
In conclusion, predominant deep dermal and subcutaneous growth pattern as well as tumour localization in the groin are uncommon features of MCC. MCC showing the aforementioned features may be associated with significant delay of diagnosis and therefore represents an unfavourable prognostic factor.
Conflict of interests
The authors declare that they have no competing interests.
Funding sources
None.
References
- Güler-Nizam E, Leiter U, Metzler G, Breuninger H, Garbe C, Eigentler TK. Clinical course and prognostic factors of Merkel cell carcinoma of the skin. Br J Dermatol. 2009. in press . [DOI] [PubMed]
- Pectasides D, Pectasides M, Economopoulos T. Merkel cell cancer of the skin. Ann Oncol. 2006;17:1489–95. doi: 10.1093/annonc/mdl050. [DOI] [PubMed] [Google Scholar]
- Balaton AJ, Capron F, Baviéra EE, Meyrignac P, Vaury P, Vuong PN. Neuroendocrine carcinoma (Merkel cell tumor?) presenting as a subcutaneous tumor. An ultrastructural and immunohistochemical study of three cases. Pathol Res Pract. 1989;184(2):211–6. doi: 10.1016/S0344-0338(89)80122-0. [DOI] [PubMed] [Google Scholar]
- Huang GS, Chang WC, Lee HS, Taylor JA, Cheng TY, Chen CY. Merkel cell carcinoma arising from the subcutaneous fat of the arm with intact skin. Dermatol Surg. 2005;31(6):717–9. doi: 10.1111/j.1524-4725.2005.31622. [DOI] [PubMed] [Google Scholar]
- Boghossian V, Owen ID, Nuli B, Xiao PQ. Neuroendocrine (Merkel cell) carcinoma of the retroperitoneum with no identifiable primary site. World J Surg Oncol. 2007;5:117. doi: 10.1186/1477-7819-5-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richetta AG, Mancini M, Torroni A, Lorè B, Iannetti G, Sardella B, Calvieri S. Total spontaneous regression of advanced merkel cell carcinoma after biopsy: review and a new case. Dermatol Surg. 2008;34(6):815–22. doi: 10.1111/j.1524-4725.2008.34153.x. Epub 2008 Mar 24. [DOI] [PubMed] [Google Scholar]


