Abstract
Although there is a clear trend toward internal fixation for ankle arthrodesis, there is general consensus that external fixation is required for cases of posttraumatic infection. We retrospectively evaluated the technique and clinical long term results of external fixation in a triangular frame for cases of posttraumatic infection of the ankle. From 1993 to 2006 a consecutive series of 155 patients with an infection of the ankle was included in our study. 133 cases of the advanced "Gächter" stage III and IV were treated with arthrodesis. We treated the patients with a two step treatment plan. After radical debridement and sequestrectomy the malleoli and the joint surfaces were resected. An AO fixator was applied with two Steinmann-nails inserted in the tibia and in the calcaneus and the gap was temporary filled with gentamicin beads as the first step. In the second step we performed an autologous bone graft after a period of four weeks. The case notes were evaluated regarding trauma history, medical complaints, further injuries and illnesses, walking and pain status and occupational issues. Mean age at the index procedure was 49.7 years (18-82), 104 patients were male (67,1%). Follow up examination after mean 4.5 years included a standardised questionnaire and a clinical examination including the criteria of the AO-FAS-Score and radiographs. 92,7% of the cases lead to a stable arthrodesis. In 5 patients the arthrodesis was found partly-stable. In six patients (4,5%) the infection was not controllable during the treatment process. These patients had to be treated with a below knee amputation. The mean AOFAS score at follow up was 63,7 (53-92). Overall there is a high degree of remaining disability. The complication rate and the reduced patient comfort reserve this method mainly for infection. Joint salvage is possible in the majority of cases with an earlier stage I and II infection.
Keywords: Infection ankle joint, posttraumatic, resection arthrodesis, tibial pilon
Introduction
Severe infection is still an important concern in the treatment of ankle and especially tibial plafond fractures [1]. Predisposing factors for joint infection are in particular open fractures, penetrating injuries, necrosis of the skin, soft tissue infection and comorbidity like diabetes, rheumatism and vascular disease [1,2]. Goal of the treatment must primarily be control of the infection. Secondly absence of pain, mobility, joint function and the ability to return to work. The methods for ankle arthrodesis differ significantly, probably a sign that no method is clearly superior to others. In the last ten years there is a clear favour toward internal fixation by screws with or without resection of the joint surfaces for cases of posttraumatic arthritis [3-7]. Surprisingly, there are only very few publications concerning arthrodesis for cases of posttraumatic joint infection, which makes comparison of the results of post-traumatic arthritis and septic cases difficult [8,9]. Methods using internal fixation seem to provide better comfort and compliance of the patients and some authors quote a higher rate of non-union for the use of external fixators [10-15]. On the other hand results of internal fixation are often compared with historical studies or techniques using the Charnley-type external fixation. Compared to modern fixators, the Charnley type is a highly unstable frame fixator construction [10,16,17]. Studies directly comparing the techniques were unable to find a significant difference in non union rates [18-20]. In particular for cases of joint infection there is consensus, that external fixation is first choice treatment [9,13,21-26].
Patients
From 1993 to 2006 a consecutive series of 155 patients with posttraumatic septic arthritis of the ankle joint were included. Retrospectively the medical files were evaluated regarding history of trauma, medical complaints, further injuries and illnesses, walking and pain status, occupational issues and the clinical examination before arthrodesis. Mean age at the index procedure was 49.7 years (18-82), 104 patients were male (67,1%). In all cases the joint infection occurred due to trauma or a posttraumatic condition. Ankle fractures and luxations were the cause of infection in 59 cases (38%), fractures of the tibial pilon in 94 cases (61%) and lesions of the fibular ligaments of the ankle in 2 cases (1%). 12 (20%) of the ankle fractures and 44 (47%) of the tibial pilon fractures were open fractures. Before our treatment started the patients had an average on 3.7 operations (0-24) in pretreating hospitals. The mean body mass index (BMI) was 28,5 kg/m2. More than 50% of all patients were suffering from relevant co-morbidity like obesity, diabetes and alcoholism. The treatment was funded by the workers injury compensation scheme in 87 patients, the remaining 68 were covered by the regular health insurance. Excluded for this study were patients with aseptic arthritis of the ankle joint and patients with non-traumatic infection. Seven patients (4,5%) were lost to follow up and were therefore excluded. The extent of infection was intraoperatively determined using the Gächter classification [27] (Table 1).
Table 1.
Gächter Joint-infection classification
| Gächter Stage | Clinical Aspect |
|---|---|
| I | Hyperaemia of synovia, effusion |
| II | Hypertrophia of synovia/pus |
| III | Beginning cartilage damage, no radiological destruction |
| IV | Radiological visible changes to bony structures, synovia grows over the cartillage |
Methods
Stage adapted treatment algorithm
We did not see any stage I infection in our study population. 22 patients (14%) had a stage II Infection treated with bilateral arthrotomy, synovialectomy, debridement and application of antibiotic beads as the first step. Open wound treatment with daily irrigation in the bath for one week followed. Wound closure was performed as the second step. Systemic antibiotic therapy was applied for at least five days in accordance to the swab results. In 19 of the 22 cases (86%) with a stage II infection the joint could be salvaged. 3 cases showed re-infection. 2 of them were treated with arthrodesis and one below knee amputation was necessary.
133 cases (86%) with advanced stage III and IV-Infections were treated with a two step treatment strategy with distance arthrodesis by wide open resection of joint surfaces and temporary filling with gentamicin beads as the first step (Table 2). Systemic antibiotic therapy was applied for at least five days in accordance to the swab results. As the second step autologous cancellous bone graft was performed after 4 weeks.
Table 2.
Stage adapted treatment of ankle joint infection
| Gächter stage Number of Patients | Treatment |
|---|---|
| I = 0 II = 22 (14%) | Bilateral arthrotomy, open wound treatment for one week before closure. |
| III-IV = 133 (86%) | Distance arthrodesis and temporary filling with gentamicin beads. Autologous bone graft after 4 weeks. |
Operative technique of resection arthrodesis
An AO fixator was applied with 4 Steinmann nails. Two Steinmann-nails were inserted with approximately 8 cm distance in the tibia, and two in the calcaneus. We recommend installing the external fixator before resection of joint surfaces and malleoli to prevent malrotation. Therefore draping should leave the knee blank. Predetermined approaches were used if possible. Metalwork implanted during previous operations was completely removed. After radical debridement and sequestrectomy of the infected areas malleoli and joint surfaces were resected. We aim for a neutral position of the arthrodesis with a maximum of 5° valgus und slight dorsalisation of the talus.
Postoperatively, subcutaneous low molecular weight heparin was prescribed until full weight bearing was achieved. Partial weight bearing with approximately 10 kg for 16 weeks followed (4 weeks from arthrodesis until bone graft and 12 weeks after the bone graft). Patients were discharged after mean 16,4 days (12-34). When bony union was confirmed on radiographs the external fixator was removed in an outpatient setting. All patients were supplied with an orthesis which allowed incremental weight bearing over a period of approximately 6 weeks. Finally an arthrodesis boot was fitted and used for at least one year (Figure 2). Follow up examination at mean 4.5 years (23-110 months) included a standardised questionnaire and a clinical examination including the criteria of the AOFAS-Score as described by Kitaoka et al (1994) and radiographs. The follow up examination was performed by an examiner that was not involved in the operative care of the patients.
Figure 2.

Orthesis allowing partial weight bearing (left) and arthrodesis boot (right).
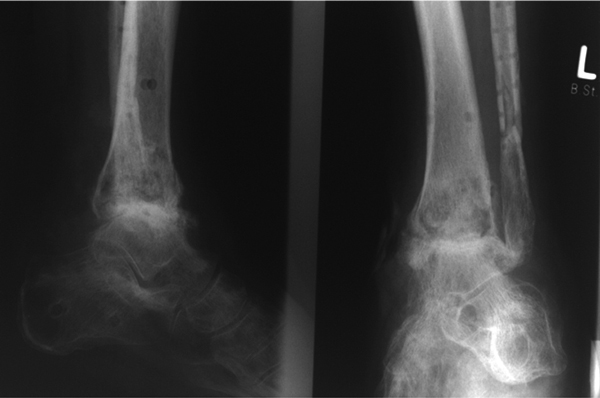
Figure 1.

Resection arthrodesis with AO-external fixator and gentamicin beads applied.
The AOFAS score gives scores from 0 to 100. A score of 90-100 is judged as an excellent result, 75-89 as good, 60-74 as fair and below 60 as poor. Follow-up examination included all 133 patients treated with resection arthrodesis.
Results
Evaluation of the intraoperative swabs showed Staph aureus in the majority of cases. 40 cases did not show a positive swab, reason might be the previous therapy with antibiotics (Table 3).
Table 3.
Results intraoperative Swab
| Staph. aureus | 95 (61%) |
| MRSA | 8 (5%) |
| Mixed | 12 (8%) |
| No pos. swab | 40 (26%) |
After mean 15.3 (10-19) weeks after bone transplantation radiographs confirmed satisfactory consolidation of the arthrodesis and the fixator was removed (Figure 3). There were no cases of deep vein thrombosis or pulmonary embolism detected in the postoperative period. 25 patients (18,8%) developed a pin tract infection which healed under conservative measures. In two cases (1.5%) a bony infection around a pin site developed making surgical procedures with debridement and replacement of the affected pin necessary. 125 (91,7%) of the procedures lead to a stable arthrodesis.
Figure 3.
Stable arthrodesis, external fixator removed.
In 5 patients (3,8%) the arthrodesis had to be stated partly-stable. A negligible amount of remaining, but painfree, mobility occurred in these cases. In six patients (4,5%) the infection was not controllable during the treatment process. These patients had to be treated with a below knee amputation. We did not see any reinfections after a stable arthrodesis was achieved. At the follow up examination a mean leg length discrepancy of -13 mm (-5 to -19 mm) was measured. Lower leg circumference difference was measured on average with -21 mm (-5 to -38 mm). The mean AOFAS score (Diagram 1, Figure 4) at follow up was 63,7 (53-92). 60 Patients (45%) returned to their previous occupation or were stated fit to work by their GP. 12 patients (9%) changed their occupation due to the results of the accident and 61 patients (46%) retired due to the outcome of the accident.
Figure 4.
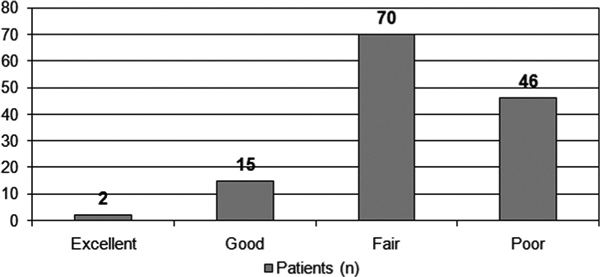
Diagram 1. Grouped results of the AOFAS-score.
Discussion
Although two staged treatment protocols for the treatment of fractures of the tibial plafond have been established, posttraumatic infection is still an important concern when dealing with these injuries [2,28]. The external compression arthrodesis as described by Charnley (1951) was the standard method for aseptic arthrodesis of the ankle joint for a long while. High rates of non union [10,14,15,29] led to biomechanical [5,30-33] and clinical comparison with internal fixation methods [10]. Biomechanical studies showed the Charnley type external fixator to have inferior stability especially regarding rotational forces [34,35]. Hagen (1986) and Berman (1989) achieved a significant improvement in stability via a three point fixation using 2 more Steinmann-nails and thereby improved union rates. There are only few publications concerning arthrodesis for cases of posttraumatic joint infection, what makes comparison of the results of posttraumatic arthritis and septic cases difficult [8,9] but for cases of joint infection there is consensus, that external fixation is the first choice treatment [9,13,21-26]. With this technique we saw a non-union and failure rate of 8.5% in our series. The pinsite infection rate of 19% is in accordance with other studies. In series treated with internal fixation there are complication rates of up to 10% reported due to the osteosynthesis material [5,16,36], the rate of necessary further procedures including the removal of metalwork is reported between 11 to 22% [37]. The loss of alignment was a known problem of the Charnley type external fixation [15,17], with our frame setup of the fixator, no secondary loss of correction occurred in our study. The surgical techniques for ankle arthrodesis differ. In the case of infection it is required to radically remove all the infected parts of cartilage and bone. Some authors recommend to salvage the medial malleolus [16,38] others always perform arthrodesis under usage of the osteomised distal fibula [15,38-40]. Again our results suggest that this is not necessary, the correction of a deformity might actually be hindered by remaining malleoli [31,41]. The perfusion of the talus is sometimes quoted as a rationale for salvage of the medial malleolus [16,38]. We saw no cases of osteonecrosis of the talus in our series. For the AOFAS-Score after internal osteosynthesis results between 67 to 76 points are reported [16,37,42], which is compared to the slightly worse 63,7 points we found in our series treating only septic cases of the advanced Gächter stage III and IV.
Conclusion
Clinical outcome of ankle arthrodesis with a frame-pattern external fixator due to advanced infection showed slightly worse results compared to arthrodesis following posttraumatic arthritis. In advanced cases the two staged treatment with arthrodesis gives satisfactory healing rates, pain control and mobility. Overall there is a high degree of remaining disability. The complication rate and the reduced patient comfort reserves this method mainly for cases of infection and for complicated soft tissue situations. Joint salvage is possible in the majority of cases with an earlier stage I and II infection. Because infection of the ankle joint is often diagnosed in an advanced stage, when arthrodesis cannot be avoided and after several pervious operations, suspicious cases should be referred to a specialised center as early as possible.
Conflict of interests statement
The authors declare that they have no competing interests.
References
- SooHoo NF. et al. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am. 2009;91(5):1042–1049. doi: 10.2106/JBJS.H.00653. [DOI] [PubMed] [Google Scholar]
- Kilian O. et al. Long-term results in the surgical treatment of pilon tibial fractures. A retrospective study. Chirurg. 2002;73(1):65–72. doi: 10.1007/s104-002-8031-1. [DOI] [PubMed] [Google Scholar]
- Maurer RC, Transarticular cross-screw fixation. A technique of ankle arthrodesis. Clin Orthop Relat Res. 1991. pp. 56–64. [PubMed]
- Monroe MT, Beals TC, Manoli A. Clinical outcome of arthrodesis of the ankle using rigid internal fixation with cancellous screws. Foot Ankle Int. 1999;20(4):227–231. doi: 10.1177/107110079902000404. [DOI] [PubMed] [Google Scholar]
- Rockett MS, Zygmunt KH, Brage ME. The use of the Synthes 7.3-mm. cannulated screw in rearfoot and ankle surgery: a preliminary prospective study. J Foot Ankle Surg. 1997;36(2):87–94. doi: 10.1016/S1067-2516(97)80051-8. [DOI] [PubMed] [Google Scholar]
- Stranks GJ, Cecil T, Jeffery IT. Anterior ankle arthrodesis with cross-screw fixation. A dowel graft method used in 20 cases. J Bone Joint Surg Br. 1994;76(6):943–946. [PubMed] [Google Scholar]
- Wagner H, Pock HG. Screw-fixation in arthrodesis of the ankle-joint. Unfallheilkunde. 1982;85(7):280–300. [PubMed] [Google Scholar]
- Schmidt HG. et al. Principles of OSG arthrodesis in cases of joint infection. Orthopade. 2005;34(12):1216–1228. doi: 10.1007/s00132-005-0870-1. [DOI] [PubMed] [Google Scholar]
- Cierny G, Cook WG, Mader JT. Ankle arthrodesis in the presence of ongoing sepsis. Indications, methods, and results. Orthop Clin North Am. 1989;20(4):709–721. [PubMed] [Google Scholar]
- Moeckel BH, Ankle arthrodesis. A comparison of internal and external fixation. Clin Orthop Relat Res. 1991. pp. 78–83. [PubMed]
- Johnson EE. et al. Ilizarov ankle arthrodesis. Clin Orthop Relat Res. 1992;280:160–169. [PubMed] [Google Scholar]
- Boobbyer GN. The long-term results of ankle arthrodesis. Acta Orthop Scand. 1981;52(1):107–110. doi: 10.3109/17453678108991769. [DOI] [PubMed] [Google Scholar]
- Charnley J. Compression arthrodesis of the ankle and shoulder. J Bone Joint Surg Br. 1951;33B(2):180–191. [PubMed] [Google Scholar]
- Helm R. The results of ankle arthrodesis. J Bone Joint Surg Br. 1990;72(1):141–143. doi: 10.1302/0301-620X.72B1.2298774. [DOI] [PubMed] [Google Scholar]
- Schnettler R. et al. Arthrodesis of the upper ankle joint. Indications, technique, results. Aktuelle Traumatol. 1992;22(6):251–258. [PubMed] [Google Scholar]
- Thermann H. et al. Screw arthrodesis of the ankle joint. Technique and outcome. Orthopade. 1996;25(2):166–176. [PubMed] [Google Scholar]
- Breitfuss H, Muhr G, Monnig B. Fixation or screws in arthrodeses of the upper ankle joint. A retrospective comparison of 76 patients. Unfallchirurg. 1989;92(5):245–253. [PubMed] [Google Scholar]
- Frey C. et al. A review of ankle arthrodesis: predisposing factors to nonunion. Foot Ankle Int. 1994;15(11):581–584. doi: 10.1177/107110079401501102. [DOI] [PubMed] [Google Scholar]
- Cracchiolo A, Cimino WR, Lian G. Arthrodesis of the ankle in patients who have rheumatoid arthritis. J Bone Joint Surg Am. 1992;74(6):903–909. [PubMed] [Google Scholar]
- Thordarson DB, Markolf K, Cracchiolo A. Stability of an ankle arthrodesis fixed by cancellous-bone screws compared with that fixed by an external fixator. A biomechanical study. J Bone Joint Surg Am. 1992;74(7):1050–1055. [PubMed] [Google Scholar]
- Berman AT. et al. Compression arthrodesis of the ankle by triangular external fixation: an improved technique. Orthopedics. 1989;12(10):1327–1330. doi: 10.3928/0147-7447-19891001-08. [DOI] [PubMed] [Google Scholar]
- Carrier DA, Harris CM. Ankle arthrodesis with vertical Steinmann's pins in rheumatoid arthritis. Clin Orthop Relat Res. 1991;268:10–14. [PubMed] [Google Scholar]
- Dehoust W, Schmidt HG. Late results of arthrodeses of the upper ankle joint. Aktuelle Traumatol. 1989;19(4):156–161. [PubMed] [Google Scholar]
- Greifensteiner H. Eine neue Methode zur Behandlung von eiternden Pseudarthrosen und Schlottergelenken. Z Orthop Ihre Grenzgeb. 1947;77(2):144–153. [PubMed] [Google Scholar]
- Hawkins BJ. et al. The Ilizarov technique in ankle fusion. Clin Orthop Relat Res. 1994;303:217–225. [PubMed] [Google Scholar]
- Willms R, Gotzen L. Monolateral external compression arthrodesis of the upper ankle joint. Unfallchirurg. 1990;93(3):115–119. [PubMed] [Google Scholar]
- Gaechter A. Gelenkinfekt-Arthoskopische Spülungsbehandlung - Hints and Tricks. Arthroskopie. 1994;7:98–101. [Google Scholar]
- Koulouvaris P. et al. Long-term results of various therapy concepts in severe pilon fractures. Arch Orthop Trauma Surg. 2007;127(5):313–320. doi: 10.1007/s00402-007-0306-y. [DOI] [PubMed] [Google Scholar]
- Eingartner C. et al. Bone repair in pseudarthrosis after arthrodesis of the upper ankle joint. Aktuelle Traumatol. 1994;24(4):155–160. [PubMed] [Google Scholar]
- Morrey BF, Wiedeman GP Jr. Complications and long-term results of ankle arthrodeses following trauma. J Bone Joint Surg Am. 1980;62(5):777–784. [PubMed] [Google Scholar]
- Myerson MS, Miller SD. Salvage after complications of total ankle arthroplasty. Foot Ankle Clin. 2002;7(1):191–206. doi: 10.1016/S1083-7515(02)00020-7. [DOI] [PubMed] [Google Scholar]
- Myerson MS, Quill G. Ankle arthrodesis. A comparison of an arthroscopic and an open method of treatment. Clin Orthop Relat Res. 1991;268:84–95. [PubMed] [Google Scholar]
- Pommer A. et al. Biomechanical study of the initial stability of various arthrodesis methods for the upper ankle joint. Unfallchirurg. 1995;98(10):535–539. [PubMed] [Google Scholar]
- Pilette S. et al. Comparative biomechanical evaluation of the immediate stability of three fixators in arthrodesis of the ankle. Ann Chir. 1993;47(9):905–911. [PubMed] [Google Scholar]
- Scranton PE, Fu FH, Brown TD. Ankle arthrodesis: a comparative clinical and biomechanical evaluation. Clin Orthop Relat Res. 1980;151:234–243. [PubMed] [Google Scholar]
- Turan I, Wredmark T, Fellander-Tsai L. Arthroscopic ankle arthrodesis in rheumatoid arthritis. Clin Orthop Relat Res. 1995;320:110–114. [PubMed] [Google Scholar]
- Buchner M, Sabo D. External or internal fixation for arthrodesis of the ankle -- a comparative study of perioperative and long-term results. Unfallchirurg. 2003;106(6):472–477. doi: 10.1007/s00113-003-0595-8. [DOI] [PubMed] [Google Scholar]
- Holt ES. et al. Ankle arthrodesis using internal screw fixation. Clin Orthop Relat Res. 1991;268:21–28. [PubMed] [Google Scholar]
- Lance EM. et al. Arthrodesis of the ankle joint. A follow-up study. Clin Orthop Relat Res. 1979;142:146–158. [PubMed] [Google Scholar]
- Lynch AF, Bourne RB, Rorabeck CH. The long-term results of ankle arthrodesis. J Bone Joint Surg Br. 1988;70(1):113–116. doi: 10.1302/0301-620X.70B1.3339041. [DOI] [PubMed] [Google Scholar]
- Strohecker T, David A. Prosthesis implantation in the proximal ankle joint--a real therapeutic alternative in post-traumatic arthrosis? Unfallchirurg. 2002;105(7):619–623. doi: 10.1007/s00113-001-0390-3. [DOI] [PubMed] [Google Scholar]
- Kiene J. et al. Clinical results of resection arthrodesis by triangular external fixation for posttraumatic arthrosis of the ankle joint in 89 cases. Eur J Med Res. 2009;14(1):25–29. doi: 10.1186/2047-783X-14-1-25. [DOI] [PMC free article] [PubMed] [Google Scholar]


