Abstract
Invasive fungal infections are on the rise. Echinocandins are a relatively new class of antifungal drugs that act by inhibition of a key enzyme necessary for integrity of the fungal cell wall. Currently there are three available agents: caspofungin, micafungin and anidulafungin.
While the individual echinocandin antifungals have a different spectrum of licensed indications, basically all of them are available for the treatment of candidemia and invasive candidiasis. Antifungal treatment modalities basically include in therapy for suspected or proven infection and prophylaxis. All three drugs are comparatively expensive. Therefore a systematic review of the literature was performed to investigate the following aspects:
• General aspects of cost-effectiveness in the treatment of invasive fungal infections
• Cost-effectiveness of the treatment with the above-mentioned antifungals
• Cost-effectiveness in two settings: therapy and prophylaxis
Early initiation of antifungal therapy, adjustment after availability of microbiological results, duration of therapy, success and occurrence of severe complications (e.g renal failure) are the most important cost drivers in antifungal therapy.
Considering the specific antifungals, for caspofungin the best evidence for cost-effectiveness is found in treatment of invasive candidiasis and in empiric therapy of suspected infections. Favourable economic data are available for micafungin as a cost-effective alternative to LAmB for prophylaxis in patients with hematopoietic stem cell transplantation (HSCT). For anidulafungin, cost-effectiveness was demostrated in a pharmacoeconomic model. Net savings - yet not significant - were observed in a retrospective chart review of 234 patients. Generally, however, most analyses are still based on pharmacoeconomic modelling rather than direct analysis of trial data or real-life clinical populations.
As an overall conclusion, using caspofungin, micafungin, or anidulafungin is not more expensive than using other established therapies. Micafungin has proven to be cost-effective in prophylaxis if the local fungal epidemiology indicates a high level of resistance to fluconazole. Switch strategies involving early initiation of broadly active therapy with switch to cheaper alternatives according to microbiology results and clinical status and early initiation of an appropriate therapy have been proven to be cost-efficient independent of the antifungal agent.
Introduction
Invasive fungal infections are on the rise. Conventional Amphotericin B (c-AmB) and azole antifungals have been the mainstay of antifungal therapy into the last decade. The high incidence of infusion-related toxicity and nephrotoxicity associated with cAmB and the emergence of fluconazole-resistant strains of Candida glabrata prompted a search for alternatives. Echinocandins are a new class of antifungal drugs that act by inhibition of beta-(1,3)-D-glucan synthase, a key enzyme necessary for the integrity of the fungal cell wall. Caspofungin was the first drug licensed drug in this class. It is indicated for esophageal candidiasis, candidemia, invasive candidiasis, empirical therapy in patients with febrile neutropenia and may be used for salvage therapy in patients with invasive aspergillosis. Response rates are generally comparable to those of amphotericin B and fluconazole. Micafungin is presently approved for esophageal candidiasis, invasive candidiasis including candidemia and for prophylaxis of Candida infections in patients undergoing allogeneic HSCT. The currently approved indications for anidulafungin are esophageal candidiasis, candidemia and invasive candidiasis. The incidence of infusion-related adverse effects and nephrotoxicity is much lower with echinocandins than with amphotericin B. And echinocandins show a good safety profile in patients with IRF. Even though they are clearly a better choice than amphotericin B pharmacoeconomically, the higher cost of these drugs in comparison to azole antifungals may attenuate their use as first-line agents in invasive fungal infections [1].
Lookingg at the therapeutic cost of fungal infections, several cost drivers can be identified. The attributable costs for patients suffering from candidemia are significant and range between £8,252 and £16,595 in one analysis [2] and USD34,123 and USD 44,536 in another study [3].
Whether any given antifungal therapy is an economically adequate option depends on its effect on the cost drivers. As echinocandins are relatively costly, DAC is considered an influencing factor on total cost [4]. However some authors find that DAC is not influencing total cost [5] or other factors outweigh DAC [6].
Cost considerations also play an increasingly important role in determining the practical usefulness of medications. A number of studies have shown that the overall expenses associated with the treatment of C/IC are significant and are largely driven by hospitalization costs. Especially LOS is an important cost driver [7-10].
This article provides a review of the current literature on the role of echinocandins in the treatment or prophylaxis of fungal infections from the economical perspective.
Materials and Methods
We conducted a literature review to investigate the available evidence on cost-effectiveness of antifungal strategies in proven invasive candidiasis, suspected infection and prophylaxis. Concerning the economical impact of antifungal therapy with echinocandins, several factors were identified as influencing the total cost:
• duration of therapy (DOT) [5]
• adjustment of therapy after availability of microbiological results [4,11]
• drug acquisition cost (DAC) [12,13]
• early initiation of treatment (EI) [14]
• complications, such as renal failure or hepatotoxicity [13,15]
From a healthcare system perspective, there are established methods in CEA to determine whether a new drug should be reimbursed by the public health system or not. One - yet not undisputed - indicator is QALYs [19-22].
With respect to these known major cost drivers, we conducted a literature review focussed on articles dealing with echinocandins in the context of cost issues or cost-impacting factors.
We used the name of the antifungal agent AND 'cost-effectiveness' OR 'economical' as search terms.
Results
The MEDLINE search yielded a total of 17 articles. Three additional analyses were included from poster presentations on international congresses where publication is in progress (Figure 1). The number of publications referring explicitly to cost-effectiveness or economical analyses is the highest for caspofungin.
Figure 1.
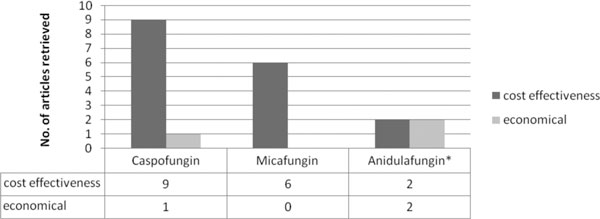
Results or the literature search for cost-effectiveness of echinocandins. * Analyses for anidulafungin as poster presentations, one article in press.
In addition we performed a literature search on general aspects like complications, rationales for empiric therapy and therapy adjustments due to microbiology findings. From this search 7 more relevant articles were retrieved. The following section describes major findings for the three echinocandins and results concerning general economical aspects of C/IC therapy.
Caspofungin
Most CEAs were performed for caspofungin. Two articles were excluded because they involved patients with invasive aspergillosis. Two articles evaluated the cost-effectiveness of caspofungin in candidemia [23,24]. Wingard et al. described favourable effects of using caspofungin instead of LAmB. The authors described cost savings of USD 758.60 per patient when using caspofungin. The effect was mainly caused by the lower incidence of IRF in the caspofungin group. Treatment with caspofungin was found to be a cost-saving strategy for a hospital. Sidhu et al. directly comparied micafungin vs. caspofungin. The CEA was based on data of a clinical trial comparing both agents. The costs for treatment of invasive candidiasis were £29,095 for micafungin vs. £29,953 for caspofungin. There were remarkably lower costs for micafungin in the group of successfully treated patients (£48,771 vs. £52,066). However, the differences were not statistically significant.
Three articles described CEAs in patients with neutropenic fever [5,13,25]. Al-Badriyeh et al. found caspofungin to be a cost-saving alternative compared to LAmB. Savings of AU$ 7,245 per patient were demonstrated. Stam et al. found caspofungin to be cost-effective as treatment costs were € 8,351 for caspofungin vs. € 11,821 for LAmB. The model was based on a clinical trial with a head-to-head comparison of both drugs. Wingard et al. found caspofungin to cause USD 5,326 less costs than LAmB in the treatment of neutropenic fever. This was based on a combined effect of lower DAC and lower IRF-rates when using caspofungin.
Two CEAs evaluated the use of caspofungin in ICU patients with suspected fungal infection [6,26]. Bruynesteyn et al. designed a model that was derived from clinical trial data. It included also costs for IRF. The results showed costs of £ 9,762 for treatment with caspofungin, which was £ 2.033 lower than for the treatment with LAmB. Caspofungin also showed advantages in terms of life years saved (QALY). Golan et al. compared different treatment strategies for ICU patients with suspected Candida infections. The authors compared a caspofungin strategy with a fluconazole strategy. The outcome measures were mortality and cost for discounted life year respectively. As a result, fluconazole turned out to be the more reasonable empiric strategy (USD 12,593 per life year saved and reduction of mortality from 44.0% to 30.4%. Caspofungin is the more effective strategy but causes USD 295,115 of costs per life year saved. However, caspofungin is the more effective strategy if fluconazole resistance among Candida species in a hospital is >25%.
Micafungin
We found 6 articles on CEAs investigating the use of micafungin. Two articles evaluated the use of micafungin in candidemia or invasive candidiasis [24,27]. Cornely et al. assessed the economic impact of using micafungin vs. LAmB in candidemia and invasive candidiasis. Micafungin was found to be a cost-effective alternative causing total treatment cost of € 43,243 vs. € 49,216. Moreover the study showed that more patients could be successfully treated with micafungin vs. LAmB (52.9% vs. 49.1%). The study performed by Sidhu et al. [20] was already described in the caspofungin section.
As micafungin is licensed for prophylaxis in patients undergoing allogeneic HSCT we also searched for publications evaluating the use of micafungin in this indication. We found three articles dealing with economic aspects of micafungin in prophylaxis [28-30].
Nomura et al. designed a hypothetical cohort of 40-year old patients with acute myeloic leukemia undergoing chemotherapy. He investigated the economical effects of three different strategies. (1) oral fluconazole, (2) intravenous amphotericin B when fever is detected and (3) no general prophylaxis but use of micafungin if fungal infection occurs. Outcome measures were years of life survived (YLS) and incremental cost per YLS. The fluconazole strategy caused the highest cost per patient but also the highest amount of life years saved. Strategy (1) caused costs of USD 625/YLS vs. strategy' (3) and USD 652/YLS vs. strategy (2). The authors concluded that a prophylaxis strategy using oral fluconazole appeared to ensure clinical benefit with an acceptable cost-effectiveness.
Sohn et al. investigated two different strategies for patients undergoing HSCT. Strategy (1) was micafungin 50 mg/d, strategy (2) was fluconazole 400 mg/d given intravenously. Outcome measures were cost, number of infection-free patients and life years saved. The data were derived from clinical studies. The authors created a hypothetical cohort of 100 patients and tested the strategies. The micafungin strategy saved KW 95,511,000 (1 USD = 925 KW by 2007. Yt resulted in 0.5 more infection-free patients and 4.8 additional life years saved per 100 patients. From these results, the authors concluded that micafungin is a reasonable prophylaxis strategy for patients undergoing HSCT in Korea.
Schonfeld et al. investigated the use of micafungin vs. fluconazole for prophylaxis in patients undergoing HSCT. The data were derived from a phase III clinical trial that included 882 patients. A cost analysis from the hospital perspective was performed. Additional sensitivity analyses were conducted by varying several cost factors. The primary analysis included data from 882 patients (527 males, 355 females; micafungin, 425 patients, mean age, 43.2 years [range, 0.6-73.0 years]; fluconazole, 457 patients, mean age, 41.9 years [range, 0.6-71.0 years]). Total hospital costs per patient were USD 121,098 and USD 124,957 in micafungin and fluconazole recipients, respectively, a difference of USD 3,859. The bootstrapping analysis found that micafungin prophylaxis was cost-saving in 72.4% of the samples versus 9.2% with fluconazole prophylaxis. Sensitivity analyses of estimated hospital costs found that micafungin was a cost-effective therapy.
One article reported on the use of micafungin for suspected ICU-acquired candidemia among patients with sepsis [16]. In this study, a hypothetical cohort of 1,000 patients with suspected ICU-acquired candidemia (ICU-AC) was designed. The strategies were either empirical therapy with micafungin (MIC), empirical therapy with fluconazole (FLU) or no treatment with a watchful waiting strategy. Differences in survivors, drug acquisition cost and cost per QALY were examined and calculated respectively. The data were derived from clinical trials. Cost data were obtained from a clinical centre in the US. The base case analysis assumed an ICU-AC-attributable mortality of 40% and a 52% relative risk reduction in mortality with appropriate timely therapy, compared with FLU (total deaths 31). Treatment with MIC (total deaths 27) then results in 4 fewer deaths at an incremental cost per death avoided of $61,446. Similarly, in a reference case, the incremental cost-effectiveness of MIC over FLU was $34,734 (95% confidence interval $26,312 to $49,209) per QALY. The estimates were most sensitive to the QALY adjustment factor and to the risk of candidemia among septic patients. From these results, the authors concluded that MIC is a reasonable strategy for ICU-AC.
Anidulafungin
Three economic analyses for anidulafungin were presented on different international congresses. One Publication in a peer-reviewed journal is in press [17,18,31,32].
Earnshaw et al. developed a pharmacoeconomic model with a decision tree structure and assessed cost from a US third party payer's perspective. A cohort of patients was generated with 58 years of mean age and proven candidemia or other evidence of invasive candidiasis. Input parameters including success rate, DOT, LOS and others were taken from a randomized controlled trial [33]. Cost data were derived from publications and a large US-hospital database.
As a result, anidulafungin turned out to be a cost-effective therapy alternative compared to standard-of-care (USD 73,000 vs. USD 81,000). The main drivers for the favourable result with anidulafungin - despite higher DAC - were higher success rate, lower mortality, shorter LOS. One-way sensitivity analysis was performed to test the robustness of the model. No data on the number of iterations and the included variables are published so far.
Reboli et al. performed an economic evaluation of their own data from the randomized controlled trial of anidulafungin versus fluconazole [33], that showed a significantly higher overall success rate for anidulafungin in the protocol-defined primary endpoint [33]. Resource consumption data were collected by medical chart reviews. In cases without available charts (75 of 234 patients), two alternative methods were used for cost estimation: expert assessment or regression analysis comparing the patients with available medical records versus the patients without records. Results showed that anidulafungin was a cost-effective therapy alternative to intravenous fluconazole. Both approximation methods revealed cost savings of USD 2,223 (expert assessment) and USD 2,681 (regression), respectively, for anidulafungin. Interestingly, this is one of the rare studies in which real cases were analyzed retrospectively and no modelling approach was chosen. However, data from one third of the patients were not complete and the cost difference failed to show significance (p = 0.70 in both approaches).
Garcia et.al.[31] presented a pharmaco-economical evaluation of the three currently available echinocandins in a Spanish hospital setting. Anidulafungin therapy was found to have a lower drug acquisition cost per episode (€6000) than other echinocandins, for which costs are influenced by the potential requirement for dose adjustments.
Treatment costs with caspofungin were reported to range from €4281 to €7991, depending on the specific dose requirements based on patient weight and hepatic function. Drug acquisition costs with micafungin were estimated at either €6000 (using a dose of 100 mg/day) or €10 741 (in cases where inadequate response requires a dose increase to 200 mg/day).
The authors concluded that treating C/IC in adult, non-neutropenic patients with anidulafungin was a cost-saving option, and also allowed better budget control.
An analysis regarding the special cohort of critically ill ICU-patients was performed by Reboli et.al.[32]. For patients in the ICU at treatment initiation, anidulafungin exhibited a definite but non-significant trend towards lower costs, which was driven by reductions in ICU and hospital lengths of stay. After adjustment for baseline covariates, those ICU patients who received anidulafungin as first-line therapy for C/IC gained a significant advantage in the number of hospital-free days (18.2 vs. 4.3 days; p 0.04).
Other potential economical benefits can be derived from the overall profile of this echinocandin [34,35]. Particularly, the reportedly low toxicity leads to the assumption that it can be cost-effective in the treatment of invasive candidiasis. As the authors recommend anidulafungin particularly if a very low drug-interaction potential is needed, this could be another factor which leads to economically favourable results.
General Findings on Economical Effects of Antifungal Therapy
Besides articles investigating one of the echinocandins directly we searched for strategies or influencing factors that generally affect treatment cost of antifungal therapy. We retrieved five articles that revealed effects possibly influencing cost [4,11,36-38]. Empirical therapy with a potent antifungal agent in patients with suscepted invasive candidiasis is an established strategy and echinocandins are useful and cost-effective in this setting. However, since methods for rapid species differentiations are available and save early detection of the fungus strain and its resistance patterns is enormously important. Fluorescent in situ hybridisation (FISH) assay is a proven method for the differentiation Candida strains [39]. Forrest et al. and Alexander et al. investigated the potential economical benefit of early detection of the causative Candida strain. If a susceptible species is detected, therapy may be deescalated from an expensive echinocandin to fluconazole after clinical improvement. Alexander et al. found that the use of FISH would save USD 1,837 per patient treated while Forrest et al. calculated savings of USD 1,729 per patient. In these investigations, the savings resulted from a reduction in cost for caspofungin. Of course, the results would be similar with other echinocandins.
Bates et al. designed a study based on real-life hospital cases and investigated the occurrence and cost of renal failure in 707 patients treated with amphotericin B: 212 (30%) of 707 adult patients receiving amphotericin B developed renal failure. Overall mortality increased from 16% to 54% in patients with renal fail are. LOS in the hospital was prolonged by 8.2 days and additional costs of USD 29,823 occurred. If patients already suffer from IRF, echinocandins are definitely the recommended alternative as they show a better safety profile for these patients compared to polyene antifungals [40].
Moreover, as the antifungal therapy is costly and clinician's knowledge of therapeutic strategies is variable, regular audits have been found to be effective in optimizing antifungal therapy and saving costs. Raymond et al. [37] set up an audit for the use of expensive systemic antifungals in a French university hospital. They investigated the prescription patterns in 81 patients receiving 118 antifungal prescriptions. Although the initiation of therapy itself was justified in 92% of the prescriptions, the chosen regimen was appropriate in only 54% according to local guidelines. The authors found an overuse of caspofungin and dosing errors of voriconazole in paediatric patients. They concluded that the audit results stress the need to update local recommendations.
Finally Arnold et.al.[38] showed that appropriate treatment is an important independent cost driver in the therapy of C/IC. The population of patients was derived from a single-center retrospective chart review analysis. Appropriate therapy was defined as prescription and delivery of an antifungal agent to which the isolated pathogen was sensitive within 24 h of positive culture. In addition the dosage ought to be adequate. Data were analysed for 167 patients (22 in the appropriate therapy group and 145 in the inappropriate therapy group). Postculture LOS was shorter in the appropriate therapy group (mean 7 vs 10.4 days, p = 0.037). This correlated with total hospital costs that were lower in the appropriate therapy group (mean $15,832 vs $33,021, p<0.001.) A graded increase in costs was noted with increasing number of modifiable risk factors (p = 0.001). The authors concluded that inappropriate therapy for C/IC occurring within 14 days of hospitalization was associated with prolonged LOS and increased costs. A rise in costs, but not LOS, was noted with increasing modifiable risk factors.
Table 1 summarizes the data indicating a positive influence of echinocandins on cost drivers and influencing factors.
Table 1.
Summary of potential economic effects of the echinocandins.
| Parameter/agent | Caspofungin | Micafungin | Anidulafungin |
|---|---|---|---|
| cost-effectiveness in invasive candidiasis/candidemia | X | X | X |
| cost-effectiveness in suspected infections | X | X | X |
| Lowering the incidence of IRF | X | X | X |
| cost-effectiveness in prophylaxis | X |
X = potential reduction of total treatment cost vs. more traditional antifungals.
Table 2 shows general strategies that showed to be cost-saving in the setting of C/lC-therapy.
Table 2.
General aspects of C/IC-therapy.
| De-escalation of initial therapy after micribiological differentiation |
| Regular clinical audits of antifungals utilization and regular updates of treatment algorithms |
| Appropriate (early and right-dosed) effective antifungal therapy |
Proven cost-effective strategies in the Management of C/IC.
Discussion
Caspofungin and micafungin are well investigated in terms of pharmacoeconomical aspects. However, most analyses still are models using data derived from clinical trials. Takingg this into account [20,41], these two antifungals can be considered cost-effective in their respective indications. Most authors admit that the results of their models are highly sensitive to changes in some cost-associated factors. Usually, sensitivity analyses or Monte Carlo simulations are used to assess the robustness of the assumptions in a pharmacoeconomic model. As these analyses were performed in all studies cited above, the results can be considered quite reliable.
When usingg models and scenario-apporaches, significant savings were found. Retrospective case analysis did show for anidulafungin better response with slightly higher cost, yet results were not significant.
However, a subgroup of ICU patients (retrospective analysis) is clearly showing favourable results for anidulafungin. Thus it can be concluded that especially critically ill patients benefit clinically and economically when treated with anidulafungin.
The positive trend towards cost-effectiveness of anidulafungin should be verified via further research and analyses.
Considering the treatment of suspected infections, adaptation of strategies to local epidemiology and resistance patterns appears crucial. Once the rate of a fluconazole-resistant Candida strains in a clinical center exceeds 25%, echinocandins should be considered a cost-effective empiric treatment choice.
Conclusion
The economic impact of antifungal therapy with echinocandins is an increasingly important issue, as the number of fungal infections in critically ill patients and immunocompromised patients is constantly growing [42,43] and these infections are asscociated with extremely high total cost of treatment [2,3]. The analysis of the current literature shows that therapy with echinocandins is generally cost-effective and may even be associated with net savings although drug acquisition cost are higher than with conventional therapy regimens. Currently, favourable cost effects are best documented for caspofungin. A number of pharmacoeconomic analyses are available for micafungin. Some poster presentations are available for anidulafungin and one study is in press. Moreover there are general clinical strategies to be further investigated and discussed [44]. Particularly early specific determination of the causative strain, therapies that consider renal function, regular audits and early appropriate therapy were also proven to be cost-effective strategies in antifungal therapy. In prophylaxis, the optimal strategies depend on local epidemiology and resistance patterns. Future clinical studies should incorporate economical aspects in the initial design.
List of abbreviations
HSCT: hematopoietic stem cell transplantation; FNP: febrile neutropenia; LAmB: liposomal amphotericin B; ICU days: treatment days on an intensive care unit; LOS: lenggth of stay in hospital; DAC: drug acquisition cost; Ei: early initiation of therapy; DOT: duration of therapy; CEA: cost-effectiveness analysis; QALY: quality adjusted life-year; IRF: impaired renal function; C/IC: Candidemia/invasive candidiasis.
References
- Grover ND. Echinocandins: A ray of hope in antifungal drug therapy. Indian journal of pharmacology. pp. 9–11. [DOI] [PMC free article] [PubMed]
- Hasssan I, Powell G, Sidhu M, Hart WM, Denning DW. Excess mortality, length of stay and cost attributable to candidaemia. J Infect. 2009;59:360–5. doi: 10.1016/j.jinf.2009.08.020. [DOI] [PubMed] [Google Scholar]
- Hennen CR. Pharmacoeconomic evaluations of antifungal therapies. Curr Med Res Opin. 2009;25:1751–8. [PubMed] [Google Scholar]
- Alexander BD, Ashley ED, Reller LB, Reed SD. Cost savings with implementation of PNA FISH testing for identification of Candida albicans in blood cultures. Diagn Microbiol Infect Dis. 2006;54:277–82. doi: 10.1016/j.diagmicrobio.2005.10.011. [DOI] [PubMed] [Google Scholar]
- Al-Badriyeh D, Liew D, Stewart K, Kong DC. Economic impact of caspofungin as compared with liposomal amphotericin B for empirical therapy in febrile neutropenia in Australia. The Journal of antimicrobial chemotherapy. pp. 1276–85. [DOI] [PubMed]
- Golan Y, Wolf MP, Pauker SG, Wong JB, Hadley S. Empirical anti-Candida therapy among selected patients in the intensive care unit: a cost-effectiveness analysis. Annals of internal medicine. pp. 857–69. [DOI] [PubMed]
- Gagne JJ, Breitbart RE, Maio V. et al. Costs associated with candidemia in a hospital setting. Pharmacol Ther. 2006;31:586–619. [Google Scholar]
- Zaoutis TE, Argon J, Chu J, Berlin JA, Walsh TJ, Feudtner C. The epidemiology and attributable outcomes of candidemia in adults and children hospitalized in the United States: a propensity analysis. Clin Infect Dis. 2005;41:1232–9. doi: 10.1086/496922. [DOI] [PubMed] [Google Scholar]
- Gagne JJ, Goldfarb NI. Candidemia in the in-patient setting: treatment options and economics. Expert Opin Pharmacother. 2007;8:1643–50. doi: 10.1517/14656566.8.11.1643. [DOI] [PubMed] [Google Scholar]
- Rentz AM, Halpern MT, Bowden R. The impact of candidemia on length of hospital stay, outcome, and overall cost of illness. Clin Infect Dis. 1998;27:781–8. doi: 10.1086/514955. [DOI] [PubMed] [Google Scholar]
- Forrest GN, Mankes K, Jabra-Rizk MA, Peptide nucleic acid fluorescence in situ hybridization-based identification of Candida albicans and its impact on mortality and antifungal therapy costs. Journal of clinical microbiology. pp. 3381–3. [DOI] [PMC free article] [PubMed]
- Fdci DR, Dos SRP, Wirth F, Goldani LZ. Continuous infusion of amphotericin B deoxycholate: an innovative, low-cost strategy in antifungal treatment. Mycoses. [DOI] [PubMed]
- Wingard JR, Leather HL, Wood CA, Pharmacoeconomic analysis of caspofungin versus liposomal amphotericin B as empirical antifungal therapy for neutropenic fever. American journal of health-system pharmacy : AJHP: official journal of the American Society of Health-System Pharmacists. pp. 637–43. [DOI] [PubMed]
- Hsu DI, Nguyen M, Nguyen L, Law A, Wong-Beringer A. A multicentre study to evaluate the impact of timing of caspofungin administration on outcomes of invasive candidiasis in non-immunocompromised adult patients. The Journal of antimicrobial chemotherapy. pp. 1765–70. [DOI] [PubMed]
- Kaskel P, Tuschy S, Wagner A, Economic evaluation of caspofungin vs liposomal amphotericin B for empirical therapy of suspected systemic fungal infection in the German hospital setting. Annals of hematology. pp. 311–9. [DOI] [PMC free article] [PubMed]
- Zilberberg MD, Kothari S, Shorr AF. Cost-effectiveness of micafungin as an alternative to fluconazole empiric treatment of suspected ICU-acquired candidemia among patients with sepsis: a model simulation. Critical care (London, England) 2009;13:R94. doi: 10.1186/cc7924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw SR GC, Gasper S. In 47th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC) Chicago, Ill.; 2007. Cost-effectiveness of Anidulafungin in confirmed candidemia and other forms of invasive candidiasis. [Google Scholar]
- Reboli AC RC, Kett DH, Schorr A, Hux M, Maschio M, Chambers R, Tarallo M. Economic Evaluation of anidulafungin (Eraxis(R)/ECALTA(R)) versus intravenous fluconazole in the treatment of hospital inpatients diagnosed with candidemia an other forms of invasive candidiasis (C/IC). In: 19th ECCMID. Helsinki, Finland; 2009. [Google Scholar]
- Williams A. The role of health economics in clinical decision-making: is it ethical? Respiratory medicine. pp. 3–5. [DOI] [PubMed]
- Brouwer WB, Koopmanschap MA. On the economic foundations of CEA. Ladies and gentlemen, take your positions! Journal of health economics. pp. 439–59. [DOI] [PubMed]
- Schwalm A, Danner M, Seidl A, Volz F, Dintsios CM, Gerber A. Wo steht die Kosten-Nutzen-Bewertung des IQWiG : Abgleich mit einem internationalen Referenzszenario? IQWiG's methods for the cost-benefit assessment : Comparison with an international reference scenario] Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz. pp. 615–22. [DOI] [PubMed]
- Brazier JE, Dixon S, Ratcliffe J. The role of patient preferences in cost-effectiveness analysis: a conflict of values? PharmacoEconomics. 2009;27:705–12. doi: 10.2165/11314840-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Wingard JR, Wood CA, Sullivan E, Berger ML, Gerth WC, Mansley EC. Caspofungin versus amphotericin B for candidemia: a pharmacoeconomic analysis. Clin Ther. 2005;27:960–9. doi: 10.1016/j.clinthera.2005.06.023. [DOI] [PubMed] [Google Scholar]
- Sidhu MK, van EAK, Kleintjens J, Schoeman O, Palazzo M. Cost-effectiveness analysis of micafungin versus caspofungin for treatment of systemic Candida infections in the UK. Current medical research and opinion. pp. 2049–59. [DOI] [PubMed]
- Stam WB, Aversa F, Kumar RN, Jansen JP. Economic evaluation of caspofungin versus liposomal amphotericin B for empiric antifungal treatment in patients with neutropenic fever in Italy. Value in health : the journal of the International Society for Pharmacoeconomics and Outcomes Research. 2008;11:830–41. doi: 10.1111/j.1524-4733.2008.00324.x. [DOI] [PubMed] [Google Scholar]
- Bruynesteyn K, Gant V, McKenzie C, A cost-effectiveness analysis of caspofungin vs. liposomal amphotericin B for treatment of suspected fungal infections in the UK. European journal of haematology. pp. 532–9. [DOI] [PMC free article] [PubMed]
- Cornely OA, Sidhu M, Odeyemi I, van E'AK, van dWJM, Schoeman O. Economic analysis of micafungin versus liposomal amphotericin B for treatment of candidaemia and invasive candidiasis in Germany. Current medical research and opinion. pp. 1743–53. [DOI] [PubMed]
- Nomura K, Kawasugi K, Morimoto T. Cost-effectiveness analysis of antifungal treatment for patients on chemotherapy. European journal of cancer care. pp. 44–50. [DOI] [PubMed]
- Sohn HS, Lee TJ, Kim J, Kim D. Cost-effectiveness analysis of micafungin versus fluconazole for prophylaxis of invasive fungal infections in patients undergoing hematopoietic stem cell transplantation in Korea. Clinical therapeutics. pp. 1105–15. discussion 066-8. [DOI] [PubMed]
- Schonfeld W, Wang CJ, Tong KB, Seifeldin R. Cost-effectiveness analysis of antifungal prophylaxis in patients undergoing hematopoietic stem cell transplantation. Clinical therapeutics. pp. 964–73. [DOI] [PubMed]
- Garcia. 12th Annual European Congress of the International Society for Pharmacoeconomics and Outcomes Research. Paris; 2009. Pharmaco-economic evaluation of currently available echinocandins in a spanish hospital setting. [Google Scholar]
- Reboli AC, Rotstein C, Kett DH, Resource utilisation and cost of treatment with anidulafungin or fluconazole for candidaemia and other forms of invasive candidiasis: focus on critically ill patients. Pharmacoeconomics [in press] 2011. [DOI] [PubMed]
- Reboli AC, Rotstein C, Pappas PG, Anidulafungin versus fluconazole for invasive candidiasis. The New England journal of medicine. pp. 2472–82. [DOI] [PubMed]
- Vehreschild JJ, Kummerle T, Karthaus M, Cornely OA. Anidulafungin-state of affairs from a clinical perspective. Mycoses. 2007;50(Suppl 1):38–43. doi: 10.1111/j.1439-0507.2007.01378.x. [DOI] [PubMed] [Google Scholar]
- Estes KE, Penzak SR, Calis KA, Walsh TJ. Pharmacology and antifungal properties of anidulafungin, a new echinocandin. Pharmacotherapy. 2009;29:17–30. doi: 10.1592/phco.29.1.17. [DOI] [PubMed] [Google Scholar]
- Bates DW, Su L, Yu Dt. et al. Mortality and costs of acute renal failure associated with amphotericin B therapy. Clin Infect Dis. 2001;32:686–93. doi: 10.1086/319211. [DOI] [PubMed] [Google Scholar]
- Raymond S, Henon T, Grenouillet F. et al. [Clinical audit on the use of expensive systemic antifungals in the Besancon University Hospital] Med Mal Infect. 2009;39:125–32. doi: 10.1016/j.medmal.2008.09.028. [DOI] [PubMed] [Google Scholar]
- Arnold HM, Micek ST, Shorr AF. et al. Hospital resource utilization and costs of inappropriate treatment of candidemia. Pharmacotherapy. 2010;30:361–8. doi: 10.1592/phco.30.4.361. [DOI] [PubMed] [Google Scholar]
- Wang P. Rapid differentiation of Candida albicans from non-C. albicans directly in a variety of clinical specimens using fluorescent in situ hybridisation. Mycoses. [DOI] [PubMed]
- Wang JL, Chang CH, Young-Xu Y, Chan KA. Systematic review and meta-analysis of the tolerability and hepatotoxicity of antifungals in empirical and definitive therapy for invasive fungal infection. Antimicrobial agents and chemotherapy. pp. 2409–19. [DOI] [PMC free article] [PubMed]
- Wilke MH. Multiresistant bacteria and current therapy -the economical side of the story. European Journal of Medical Research. 2010;15:571–6. doi: 10.1186/2047-783X-15-12-571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erjavec Z, Kluin-Nelemans H, Verweij PE. Trends in invasive fungal infections, with emphasis on invasive aspergillosis. Clin Microbiol Infect. 2009;15:625–33. doi: 10.1111/j.1469-0691.2009.02929.x. [DOI] [PubMed] [Google Scholar]
- Hosseini-Moghaddam SM, Husain S. Fungi and molds following lung transplantation. Semin Respir Crit Care Med. 2010;31:222–33. doi: 10.1055/s-0030-1249118. [DOI] [PubMed] [Google Scholar]
- Playford EG, Lipman J, Sorrell TC. Prophylaxis, empirical and preemptive treatment of invasive candidiasis. Curr Opin Crit Care. 2010;16:470–4. doi: 10.1097/MCC.0b013e32833e10e8. [DOI] [PubMed] [Google Scholar]


