Abstract
Objective
Primary diffuse leptomeningeal gliomatosis (PDLG) is a rare neoplasm with a short survival time of a few months. there is currently no standardized therapeutic approach for PDLG.
Materials and methods
We report on a 53-year-old male patient who presented with epileptic seizures, gait disturbance, paraparesis and sensory deficits in the dermatomes T8-10.
Results
Magnetic resonance imaging (MRI) revealing numerous spinal and cranial gadolinium-enhancing nodules in the meninges and histopathology led us to diagnose primary diffuse leptomeningeal gliomatosis with WHO grade III astrocytic cells. Consecutively, the patient underwent craniospinal radiotherapy (30 Gy) and 11 sequential cycles of temozolomide. This regimen led to partial tumor regression. Thirteen months later, spinal MRI revealed tumor progression. Second-line chemotherapy with 5 cycles of irinotecan and bevacizumab did not prevent further clinical deterioration. The patient died twenty-two months after diagnosis, being the longest survival time described thus far with respect to PDLG consisting of astrocytic tumor cells.
Conclusions
Radiochemotherapy including temozolomide, as established standard therapy for brain malignant astrocytomas, might be valid as a basic therapeutic strategy for this PDLG subtype.
Keywords: primary diffuse leptomeningeal gliomatosis; temozolomide; radio-chemotherapy, malignant astrocytic cells, survival time
Introduction
Primary diffuse leptomeningeal gliomatosis (PDLG) is diagnosed when a glioma is located in the subarachnoid space, while intraparenchymal tumor lesions are absent [1]. PDLG must be distinguished from secondary meningeal gliomatosis resulting from a primary gliomatous CNS tumor. PDLG occurs frequently along the spinal cord [2]. PDLG, especially when caused by malignant astrocytic cells, is associated with very poor survival [3]. A standardized therapy for patients with PDLG is lacking [4].
We describe a patient with PDLG consisting of malignant astrocytic cells who underwent combined radio- and chemotherapy leading to the longest survival time described in the literature thus far.
Case Report
A 53-year-old man was referred to the Dept. of Neurology due to a generalized epileptic seizure and five months later he presented with bilateral sensory deficits at dermatome levels T8-10, paraparesis and gait disturbance. Cerebrospinal fluid (CSF) analysis revealed a high cell count (300/3 cells/μl; reference range: 5/3 cells/μl) with atypical cells that could not be further characterized. T1-weighted images (T1-WI) revealed spinal and cranial Gd-enhancing nodules in the leptomeninges (Figures 1a-e) and on T2-weighted images (T2-WI) an intramedullary edema (Figure 1c).
Figure 1.
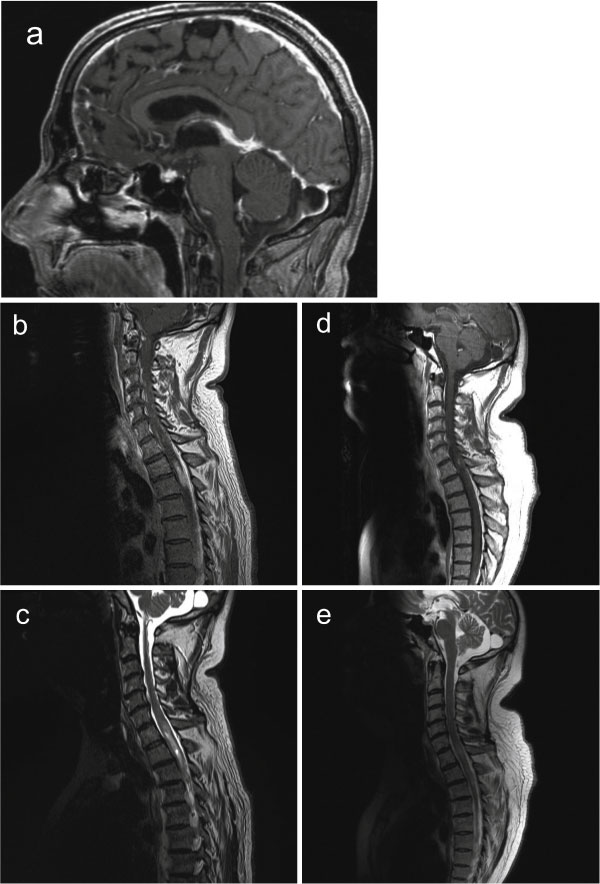
Note Gd-enhanced supra- and in-fratentorial meningeal thickenings of the brain in sagittal T1-W image (a). Prior to ra-diochemotherapy, T1-WI reveals lep-tomeningeal Gd-enhancement (b) and T2-WI shows edema of the myelon on levels C7, T1-2 and T5-6 due to minor tumor extensions in the adjacent spinal cord (c). Following radiochemotherapy, T1-WI displays reduced leptomeningeal Gd-enhancement (d) while T2-WI shows less myelon spinal edema on those levels (e).
Three weeks later, intradural biopsy from a Gd-enhancing nodule at L2-3 level revealed fibrously-thickened meninges infiltrated by malignant astrocytic tumor cells (Figures 2a-c). the tumor was categorized as primary diffuse leptomeningeal gliomatosis (PDLG) confirmed by the Reference Center for Brain Tumors in Düsseldorf, Germany.
Figure 2.
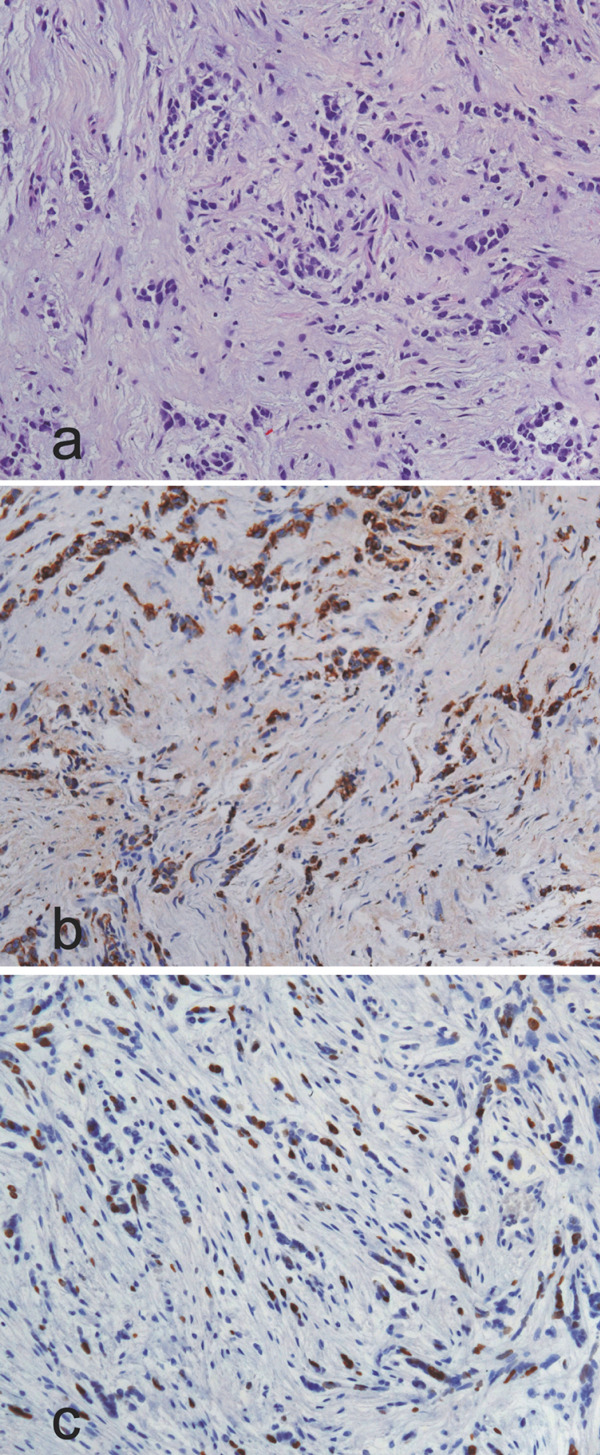
Intradural lumbar biopsy displays fibrously-thickened lep-tomeninges infiltrated by pleomorphic neoplastic astrocytic cells (a). The astrocytic tumor cells reveal intensive intracytoplasmic staining with anti-glial fibrillary astrocytic protein. (b). Ki67 (MIB-1) staining reveals a high proliferation index of up to 20% (c).
Prior to radiotherapy of the craniospinal axis (4 × 2.5 Gy/week, total dose: 30 Gy), the patient underwent 3 cycles of temozolomide (TMZ) (cycle 1: 150-200 mg/m2 TZM, d1-5, q28d). On re-staging, spinal T1-weighted images showed tumor-lesion regression on L5 and spinal T2-WI images demonstrated spinal-edema regression (compare Figures 1c-d with Figures 1a-b). Three weeks after the completion of radiotherapy the patient received eight additional cycles of TMZ (200 mg/m2 TZM, d1-5, q28d), during which meningeal thickening of the brain regressed. However, spinal MRI thirteen months after starting TMZ therapy revealed meningeal tumor progression at the lesions on spinal levels C1-2, C7-t2 and T5-8. Five cycles of second-line chemotherapy with irinotecan and bevacizumab failed to halt further clinical deterioration. the patient died twenty-two months after the diagnosis of PDLG and exhibited until dead an encouraging Karnovsky performance status of 60%. an autopsy was declined.
Discussion
The diagnosis of PDLG is usually established by autopsy but rarely diagnosed prior to death [1]. PDLG of the oligodendroglial and that of the well-differentiated astrocytic tumor type are associated with a considerably longer median survival time than that of the malignant astrocytic tumor type [5].
PDLG was diagnosed in the aforementioned case, as we observed on histopathology leptomeningeally-encapsulated malignant astrocytic cells without primary attachment to the spinal cord or brain parenchyma and Gd-enhancing leptomeningeal thickening at the base of the brain and spinal level in MRI [6,7].
Various treatment modalities were used for 14 patients suffering from PDLG with malignant astrocytic cells reported in the literature so far (cf. Table 1), demonstrating the lack of a standardized treatment regimen of PDLG with malignant astrocytic cells. Although the number of cases is small, the data on their survival times (cf. Table 2) might suggest that radiotherapy and temozolomide (TMZ) as established treatment for newly diagnosed recurrent anaplastic astrocytomas [8] also seem to be valid for PDLG with malignant astrocytic cells. This concept is supported by the observation that radiotherapy alone can prolong the median survival time of five months for patients without any specific therapy to a median survival of 12 months and that integration of TMZ in the chemotherapy alone may lead to a prolonged median survival of 15 months. The importance of TMZ in the chemotherapy treatment of PDLG is supported by the observation that the median survival time fell to 3 months when the integration of TMZ was omitted.
Table 1.
Clinico-pathological characteristics and treatment of adult patients suffering from PDLG with malignant astrocytic cells including our case
| Age | Gender | Survival | First Symptoms | Localization | Biopsy | Autopsy | Radiotherapy | Chemotherapy | Reference |
|---|---|---|---|---|---|---|---|---|---|
| 43 | M | < 1 | headache, nausea, facial nerve paresis | Cr, SC | - | + | - | - | [15] |
| 51 | M | 2 | IRP, back pain | Cr, SC | + | - | - | + CYC, ADR, 5FU, MTX it | [10] |
| 47 | M | 2 | headaches, altered consciousness, numbness in both arms | Cr | + | - | - | + MTX it | [16] |
| 23 | F | < 3 | IRP, seizures | Cr | - | + | - | - | [12] |
| 52 | M | 3 | low back pain, numbness of both legs | Cr, SC | + | + | + (craniospinal) | + MCNU, Interferon | [17] |
| 63 | F | 3 | IRP, headache, coma | Cr, BrS | + | + | - | + CYC | [11] |
| 19 | M | 3 | IRP | Cr, SC | - | + | - | - | [18] |
| 25 | M | 5 | IRP | Cr, BrS, SC | + | + | - | - | [19] |
| 71 | M | 7 | back stiffness | SC | - | + | - | - | [2] |
| 50 | M | 7 | IRP, polyneuritis cranialis | Cr, BrS, SC | + | + | - | - | [5] |
| 19 | M | 11 | holocephalic headache, nausea, vomitus, left-sided weakness | Cr, SC | + | - | + (craniospinal) | + TMZ | [13] |
| 60 | M | 12 | blurred vision, back pain | SC | + | - | + (spinal) | - | [20] |
| 24 | M | 13 | holocephalic headache, neck pain, diplopia, confusion | Cr, SC | + | - | - | + 12c × TMZ/BCNU | [13] |
| 40 | F | 17 | ataxia, incontinence, obstipation | Cr | + | - | - | + 7c × TMZ, AUC + ETO, BCNU | [14] |
| 53 | M | 24 | seizures, gait disturbance, paraparesis, sensory disturbance | Cr, SC | + | - | + (craniospinal) | +11c xTMZ, INN, DDP, INT, BVZ | our case |
5-FU = 5-fluouracil, ADR = Adriamycin, AUC 5 = Carboplatine, BCNU = Carmustine, BrS = brainstem, BVZ = Bevacizumab, c = cycle, CA = Cytarabine, CCNU = Lomustine, Cr = Cranial, CYC = Cyclophosphamide, DDP = Cisplatin, ETO = Etoposide, INN = topotecan, INT = Irinotecan, IRP = raised intracranial pressure, it = intrathecally, MCNU = Ramustine, MTX = Methotrexate, SC = spinal cord, TMZ = Temozolomide, TOP = Thiotepa, Vincristine, Prednison
Table 2.
Summary of the literature: PDLG with malignant astrocytic cells
| Number of cases (including our patient) | 15 |
| M: F ratio | 12:3 |
| Median age (in years); age range (in years) | 43; 19-71 |
| Secondary brain involvement | 87% (13/15) |
| Secondary spinal cord involvement | 74% (11/15) |
| Median survival (in months) | 8 (1-24) |
| Median survival without therapy (in months) | 5 (1-7) |
| Median survival with radiotherapy only | 12 |
| (in months) | |
| Median survival with chemotherapy only | 3 |
| (in months) | |
| - without temozolomide | < 3 |
| - including temozolomide | 15 |
| Median survival with radio- und chemotherapy (in months) | 11 |
| - without temozolomide | 3 |
| - including temozolomide (our patient) | 18 |
The prolonged survival of our patient may be due to the addition of TMZ to radiation therapy as it resulted in an extent of the median survival time for high grade glioma patients [9]. In addition, the hypofractionated radiotherapy regimen used is supposed to be more effective than conventional fractionated irradiation. Additionally, the patient's good Karnofsky performance status may have contributed to our patient's prolonged survival.
In conclusion, we report on partial regression and long survival in a patient with PDLG of the malignant astrocytic type following hypofractionated radiotherapy and TMZ. An immediate radiochemotherapy seems crucial for a prolonged survival of PDLG patients in good general condition.
Conflict of interests
The authors disclose no or potential conflict of interest including any financial, personal or other relationships with other people or organizations within the three years of beginning the submitted work that could inappropriately influence or be perceived to influence their work.
References
- Bhatia R, Roncaroli F, Thomas P, Cheah SL, Mehta A, Glaser M, Ulbricht C. A case of primary leptomeningeal gliomatosis confined to the spinal cord. J Neurooncol. 2010;98(1):125–9. doi: 10.1007/s11060-009-0050-y. [DOI] [PubMed] [Google Scholar]
- Barborie A, Dunn EM, Bridges LR, Bamford JM. Primary diffuse leptomeningeal gliomatosis predominantly affecting the spinal cord: case report and review of the literature. J Neurol Neurosurg Psychiatry. 2001;70(2):256–258. doi: 10.1136/jnnp.70.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva M, Bacigaluppi S, Galli C, Citterio A, Collice M. Primary leptomeningeal gliomatosis: case report and review of the literature. Neurol Sci. 2005;26(2):129–134. doi: 10.1007/s10072-005-0446-1. [DOI] [PubMed] [Google Scholar]
- Davila G, Duyckaerts C, Lazareth JP. Diffuse primary leptomeningeal gliomatosis. J neurooncol. 1993;15(1):45–9. doi: 10.1007/BF01050262. [DOI] [PubMed] [Google Scholar]
- Debono B, Derrey S, Rabehenoina C, Proust F, Freger P, Laquerriere A. Primary diffuse multinodar leptomeningeal gliomatosis. Case report and review of the literature. Surg neurol. 2006;65(3):273–282. doi: 10.1016/j.surneu.2005.06.038. [DOI] [PubMed] [Google Scholar]
- Davis PC, Friedman NC, Fry SM, Malko JA, Hoffmann JC Jr, Braun IF. Leptomeningeal metastasis: MR imaging. Radiology. 1987;163(2):449–454. doi: 10.1148/radiology.163.2.3562825. [DOI] [PubMed] [Google Scholar]
- Vertosick FT, Selker RG. Brain stem and spinal metastases of supratentorial glioblastoma multiforme- a clinical series. Neurosurgery. 1990;27(4):516–522. doi: 10.1227/00006123-199010000-00002. [DOI] [PubMed] [Google Scholar]
- Omar A, Mason WP. Temozolomide: the evidence for its therapeutic efficacy in malignant astrocytomas. Core Evid. 2009;4:93–111. doi: 10.2147/ce.s6010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stupp R, Mason WP, Van de Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisen-hauer E, Mirimanoff RO. European Organisation for Research and Treatment of Cancer Brain tumor and Radio-therapy groups; national Cancer Institute of Canada Clinical trials group. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- Rees JH, Balakas N, Agathonikou A, Hain SF, Giovanni G, Panayiotopolous CP, Luxsuwong M, Revesz T. Primary diffuse leptomeningeal gliomatosis simulating tuberculous meningitis. J Neurol Neurosurg Psychiatry. 2001;70(1):120–122. doi: 10.1136/jnnp.70.1.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietrich PV, Aapro MS, Rieder A, Pizzolato GP. Primary diffuse leptomeningeal gliomatosis (PDLG): a neoplastic cause of chronic meningitis. J Neuroncol. 1993;15(3):275–283. doi: 10.1007/BF01050075. [DOI] [PubMed] [Google Scholar]
- Tsui EY, Loo KT, Mok CK, Yuen MK, Cheung YK. Primary multifocal leptomeningeal gliomatosis. Eur J Radiol. 2001;37(1):5–7. doi: 10.1016/S0720-048X(00)00220-5. [DOI] [PubMed] [Google Scholar]
- Jicha GA, Glantz J, Clarke MJ, Lehwald LM, Russo DP, Giannini C, Wald JT, Uhm J, Kumar N, Aksamit AJ, Wetmore CJ. Primary diffuse leptomeningeal gliomatosis. Eur neurol. 2009;62(1):16–22. doi: 10.1159/000216838. [DOI] [PubMed] [Google Scholar]
- Franceschi E, Cavallo G, Scopece L, Esposti RD, Paioli G, Paioli A, Palmerini E, Foschini MP, Marliani AF, Crino L. Temozolomide-induced partial response in a patient with diffuse leptomeningeal gliomatosis. J Neurooncol. 2005;73(3):261–264. doi: 10.1007/s11060-004-5672-5. [DOI] [PubMed] [Google Scholar]
- Heye N, Iglesias JR, Tönsen K, Graef G, Maier-Hauff K. Primary leptomeningeal gliomatosis with predominant involvement of the spinal cord. Acta Neurochir. 1990;102(34):145–8. doi: 10.1007/BF01405430. [DOI] [PubMed] [Google Scholar]
- Singh M, Corboy JR, Stears JC, Kleinschmidt-DeMasters BK. Diffuse leptomeningeal gliomatosis associated with multifocal CNS infarcts. Surg Neurol. 1998;50(4):356–362. doi: 10.1016/S0090-3019(97)00371-6. [DOI] [PubMed] [Google Scholar]
- Yomo S, Tada T, Hirayama S, Tachibana N, Otani M, Tanaka Y, Hongo K. A case report and review of the literature. J Neurooncol. 2007;81(2):209–216. doi: 10.1007/s11060-006-9219-9. [DOI] [PubMed] [Google Scholar]
- Pingi A, Trasimeni G, Di Basi C, Gualdi G, Piazza G, Corsi F, Chiappetta F. Diffuse leptomeningeal gliomatosis with osteoblastic metastases and no evidence of intraaxial lesions. AJNR. 1995;16(5):1018–1020. [PMC free article] [PubMed] [Google Scholar]
- Kastenbauer S, Danek A, Klein W, Yousry TA, Bise K, Reifenberger G, Pfister HW. Primary diffuse leptomeningeal gliomatosis: unusual MRI with non-enhancing nodular lesions on the cerebellar surface and spinal leptomeningeal enhancement. J Neurol Neurosurg Psychiatry. 2000;69(3):385–8. doi: 10.1136/jnnp.69.3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi M, Hara K, Nakatsukasa M, Murase I, Toya S. Primary spinal leptomeningeal gliomatosis presenting visual disturbance as the initial symptom: case report. Acta Neurochir (Wien) 1996;138(4):480–481. doi: 10.1007/BF01420313. [DOI] [PubMed] [Google Scholar]


