Abstract
Purpose
Both open and arthroscopic Bankart repair are established procedures in the treatment of anterior shoulder instability. While the open procedure is still considered as the "golden standard" functional outcome is supposed to be better in the arthroscopic procedure. The aim of this retrospective study was to compare the functional outcome between open and arthroscopic Bankart repair.
Materials and methods
In 199 patients a Bankart procedure with suture anchors was performed, either arthroscopically in presence of an detached, but not elongated capsulolabral complex (40) or open (159). After a median time of 31 months (12 to 67 months) 174 patients were contacted and agreed to follow-up, 135 after open and 39 after arthroscopic Bankart procedure.
Results
Re-dislocations occurred in 8% after open and 15% after arthroscopic Bankart procedure. After open surgery 4 of the 11 re-dislocations occurred after a new adequate trauma and 1 of the 6 re-dislocations after arthroscopic surgery. Re-dislocations after arthroscopic procedure occured earlier than after open Bankart repair. An external rotation lag of 20° or more was observed more often (16%) after open than after arthroscopic surgery (3%). The Rowe score demonstrated "good" or "excellent" functional results in 87% after open and in 80% patients after arthroscopic treatment.
Conclusion
In this retrospective investigation the open Bankart procedure demonstrated good functional results. The arthroscopic treatment without capsular shift resulted in a better range of motion, but showed a tendency towards more frequently and earlier recurrence of instability. Sensitive patient selection for arthroscopic Bankart repair is recommended especially in patients with more than five dislocations.
Keywords: traumatic shoulder instability, Bankart procedure, open versus arthroscopic procedure
Introduction
In 1938 Bankart [2] reported excellent results of re-attachment of the capsulolabral complex in patients with anterior shoulder instability, a method first described by Perthes [31]. This technique is based on the premis that detachment of the anteroinferior capsulolabral complex is the cause for recurrent dislocations and therefore refixation is the therapy of choice. Since then open "Bankart repair" with minor modifications has been performed with good results and low recurrence rates and therefore was considered as the "golden standard". Rowe [33] reported in 1978 excellent and good functional results in 97% and a recurrence rate of 3.5% with this technique after an average follow-up duration of 6 years. Different studies have proven this technique as a sucessful treatment for traumatic anterior shoulder instability with recurrence rates below 10% [13,15,16,24,29,32,40]. However, long-term follow-up studies and investigations including subluxation as a failure demonstrated a higher recurrence rate than expected [26].
Problems reported to be associated with open Bankart repair include restriction in external rotation [4,6,17,21] and subscapularis muscle insufficiency [35]. Therefore less invasive arthroscopic techniques have been developed and have improved from disappointingly high recurrence rates with staple capsulorrhaphy [7], transglenoid sutures [14,30] and bioabsorbable tacks [8] to promising results with suture anchors equal to open procedures [3,5,9,11,19,23]. Arthroscopic stabilization is considered advantageous in terms of decreased morbidity with reduced pain and shorter hospitalization (if necessary at all), faster rehabilitation, no violation of the subscapularis tendon and no loss in range of motion [1]. Nevertheless, higher recurrence rates compared to the open procedure have been reported [10,20,38].
The intention of this investigation was to compare open and arthroscopic Bankart repair concerning functional outcome and stability at mid-term follow-up.
Materials and methods
In this retrospective cross-sectional study patients were reviewed, who underwent surgical treatment for shoulder instability at the authors' Orthopedic department. In 1995 a modified Bankart procedure without osteotomy of the coracoid process became the standard operation for traumatic anterior shoulder instability at the authors' department. A total of 212 patients were treated between 1995 and June 2004 for traumatic anterior shoulder dislocation (TUBS) according to the criteria of Matsen [41].
Patient samples
Most patients (206, 97%) had recurrent dislocations, 169 (80%) were male and 43 (20%) female. In 109 patients (51%) the dominant side was involved. Age at first dislocation was in median 22 years (range 5 to 67 years), the time from first dislocation to surgery was in median 28 month (ranging from 1 month to 8 years).
21 patients had an osseus Bankart lesion, in four patients the Bankart fragment could be fixed with screws, nine patients suffering from loss of the anterior glenoid of more than 20% required a reconstruction with iliac crest bone grafting and were excluded from this study. Eight patients with only small osseus fragments were treated with refixation of the capsulolabral complex with suture anchors and were included in this study.
In a total of 199 patients a Bankart procedure with suture anchors was performed (median age at surgery 26 years, 20% females), either arthroscopically in presence of an detached, but not elongated capsulolabral complex (40, 20%) or open (159, 80%). In 56 of these 159 patients (28%) with a wide capsule an additional inferior capsular shift as described by Neer [28] was performed.
Patients who underwent open surgery showed a median age of 27 years (22% females) versus 25 years among the arthroscopically treated patients (13% females). A total of 36% (open) and 40% (arthroscopic) of them reported more than five dislocations before surgery. Three patients treated with open surgery and four patients treated arthroscopically had an additional SLAP lesion. There were 12 partial lesion of the supraspinatus tendon in the open group, the rotator cuff was intakt in all arthroscopic treated patients The demographic data for the patient samples are summarized in Table 1.
Table 1.
Distribution characteristics for demographic data of patients after open and arthroscopic Bankart procedure (absolute and relative frequencies for gender and dislocations before surgery, medians and quartile ranges for age and time from trauma to surgery)
| Open | arthroscopic | |
|---|---|---|
| Total number of patients | 159 | 40 |
| Gender, ratio males: females | 124 (78%): 35 (22%) | 35 (87%): 5 (13%) |
| Age at surgery (y) | 27 (21 - 34) | 25 (19 - 32) |
| Time from trauma to surgery (m) | 32 (15 - 88) | 21 (11 - 52) |
| Number of dislocations before surgery | ||
| up to 5 | 97 (61%) | 24 (60%) |
| more than 5 | 62 (39%) | 16 (40%) |
Surgical procedure
All patients were operated on under general anesthesia and in beach-chair position. After diagnostic arthroscopy through the standard dorsal portal the decision was made whether to continue with arthroscopic or open surgery.
In cases of detached, but intact capsulolabral complex and no visually elongated capsule an arthroscopic fixation using suture anchors was performed. Additional antero-superior and anterior portals were used. In the other cases an open procedure using a deltoideo-pectoral approach with an L-shaped incision of the upper two third of the subscapularis tendon was performed. The capsular incision was done laterally, in cases of elongated capsule a lateral based T-shaped incision was used and an inferior shift was done.
In all cases the anteroinferior capsulolabral complex was separated from the glenoid and anatomical repair was performed with two to three suture anchors (FAS-Tak, Fa.Arthrex; Mini-Revo, Fa.Linvatec; Mitek GII, Fa.Depuy-Mitek). The distal anchor was placed at 5 to 5.30 o'clock in aright shoulder. No capsular shift was done in the arthroscopic cases.
Postoperative rehabilitation
All patients underwent a similar rehabilitation protocol. Instructions were given to the patient by a physiotherapist during hospital stay and in written form for the further therapy. The arm was immobilized in a Gilchrist cast for 6 weeks and only passive motion twice a day (anteversion up to 90°, no abduction, no external rotation) was allowed. During the 7th to the 12th week after surgery active movement was allowed and full range of motion was achieved assisted by physiotherapy. Throwing position was allowed after week 12.
Recall
After a median time of 31 months (12 to 67 months) 174 patients were contacted and agreed to follow-up; a total of 143 of them underwent a clinical examination and a written interview with a questionnaire, further 31 patients only answered the questionaire. Among these recall patients 135 had undergone an open and 39 an arthroscopic Bankart procedure. A total of 24 patients were lost to follow-up.
The questionnaire included information about recurrent instability (dislocation, subluxation or feeling of instability) as well as questions to loss of function and subjective rating. The clinical examination included assessment of range of motion, stability (apprehension and relocation test 36), loss of function and strength in order to obtain the Rowe Score 33 and a modified Rowe Score 34 adapted for subluxations. The lift-off test 12 was applied to determine subscapularis muscle insufficiency.
Statistical analysis
The primary analysis was performed via Kaplan/Meier estimation of the dislocation-free time after initial surgery; the description of the survival estimates was based on the mean dislocation-free times after the respective surgical treatment and the corresponding 95% confidence intervals. The Kaplan/Meier estimates for the time to dislocation after open versus arthroscopic treatment were then compared by means of a univariate Logrank test and by means of a multivariate Cox regression analysis based on Likelihood Ratio tests. The latter adjusted the dislocation patterns of the samples for putative prognostically relevant cofactors such as age and gender. Results of both the univariate and multivariate analysis were summarized in terms of p-values. Due to the exploratory character of the multivariate analysis p-values derived from the latter were not formally adjusted for multiplicity; a p-value < 0.05 therefore indicates a locally significant difference between samples.
In general the data were analysed according to the respective endpoints' scale level: the description of continuous endpoints was based on medians and quartiles, the description of categorical endpoints of appropriate absolute and relative frequencies. The significance comparison of sub samples was based on pairwise two sample Wilcoxon and Fisher tests, accordingly.
All numeric and graphic analyses were performed with SPSS software (release 12.0 for Windows; SPSS Inc, Chicago, IL).
Results
Re-dislocations occurred in 11 (8%) of 135 patients after open and in 6 (15%) of 39 patients after arthroscopic Bankart procedure. After open surgery 4 of these 11 re-dislocations occurred after a new adequate trauma and 1 of the 6 re-dislocations after arthroscopic surgery. This corresponds to an adjusted re-dislocation rate without new adequate trauma of 5% (7 of 135 patients) after open versus 13% (5 of 39 patients) after arthroscopic treatment (Table 2).
Table 2.
Absolute and relative rates for recurrence of instability in patients after open and arthroscopic Bankart procedure
| Open | arthroscopic | |
|---|---|---|
| Total number at Recall | 135 | 39 |
| Redislocation | 11 (8%) | 6 (15%) |
| without trauma | 7 (5%) | 5 (13%) |
| with new trauma | 4 | 1 |
| Redislocation and subluxation | 15 (11%) | 9 (23%) |
Furthermore 4 patients after open and 3 patients after arthroscopic surgery reported subluxations. If both "dislocation for any cause" and "subluxation" are considered as recurrence of instability, the open treatment failed in 15 patients (11%) versus 9 patients after arthroscopic treatment (23%).
After arthroscopic surgery there was an increased rate of failure (re-dislocation and subluxation) observed among patients, who had reported more than 5 dislocations before initial surgery (6 of 16 patients [38%]) versus patients with fewer previous dislocations (3 of 23 patients [13%]). There was no such difference in patients after open surgery.
The mean time interval between surgery and dislocation for any cause was 64 month after open and 41 month after arthroscopic procedure (95% confidence intervals 62 - 67 versus 37 - 45 months, respectively). The underlying dislocation-free time distributions differed statistically significantly (p = 0.0268). Figure 1 displays the corresponding Kaplan/Meier survival estimates.
Figure 1.
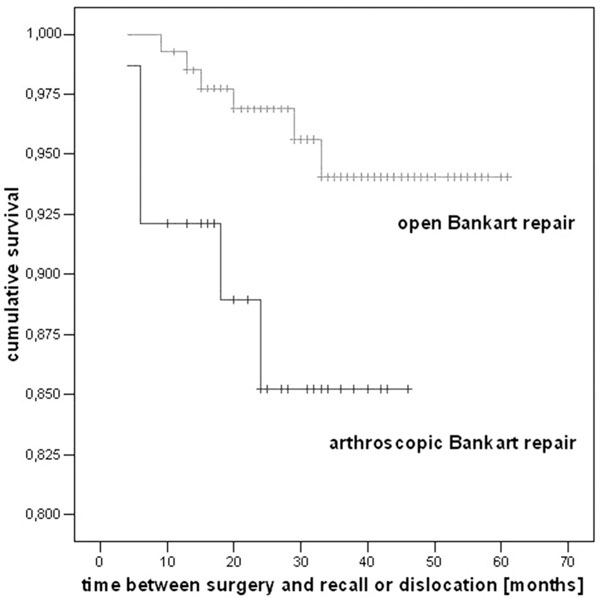
Kaplan/Meier survival estimate for the dislocation-free time [months] after initial surgery of patients after open and arthroscopic Bankart procedure (crosses indicate censoring of patients).
The Cox regression analysis of the above re-dislocation rates confirmed the surgical procedure as the dominating and statistically significant determinant (Likelihood Ratio p = 0.039): Neither age at first dislocation (p = 0.441) or at recall (p = 0.219), the patient's gender (p = 0.984), the duration between first luxation and initial surgery (p = 0.297) or the self-reported number of dislocations before surgery (p = 0.088) showed a statistically significant association with the time to re-dislocation after surgery.
Functional and subjective outcome
A total of 125 patients (93%) after open surgery versus 30 patients (77%) after arthroscopic treatment were satisfied with the operation (Fisher p = 0.016). Only 2 patients (2%) after open surgery and 2 patients (5%) after arthroscopic treatment would not agree to undergo the same type of surgery again.
Among the 143 patients who underwent clinical examination (108 after open and 35 after arthroscopic treatment) a total of 6 patients (6%) after open and 5 patients (14%) after arthroscopic treatment showed a positive apprehension and relocation test during clinical examination (Fisher p = 0.144).
Concerning range of motion compared to the contralateral side no significant difference between open and arthroscopic Bankart procedure were observed for abduction. An external rotation lag of 20° or more was observed more often (16%) after open than after arthroscopic surgery (3%, Fisher p = 0.073). Using the Lift-off test 12 to determine the subscapularis function there were no clinical signs for subscapularis muscle insufficiency.
The Rowe score [33] demonstrated "good" or "excellent" functional results in 94 of 108 (87%) patients after open and in 28 of 35 (80%) patients after arthroscopic treatment (Fisher p = 0.409). The modified Rowe 34 score demonstrated "good" or "excellent" functional results in 91 of 108 (84%) patients after open and in 26 of 35 (74%) patients after arthroscopic treatment (Fisher p = 0.210; Table 3). These differences are mainly caused by the number of re-dislocations. Taking only the patients without re-dislocations there are similar results in both groups.
Table 3.
Functional outcome of patients after open and arthroscopic Bankart procedure assessed and classified by means of the Rowe and the modified Rowe score
| open | arthroscopic | ||
|---|---|---|---|
| Rowe score33 | "excellent" | 91 (84%) | 27 (77%) |
| "good" | 3 (3%) | 1 (3%) | |
| "fair" | 9 (8%) | 3 (9%) | |
| "poor" | 5 (5%) | 4 (11%) | |
| Modified Rowe score34 | "excellent" | 68 (63%) | 19 (54%) |
| "good" | 23 21%) | 7 (20%) | |
| "fair" | 15 (14%) | 7 (20%) | |
| "poor" | 2 (2%) | 2 (6%) |
Discussion
This retrospective investigation demonstrated an numerically increased recurrence rate after arthroscopic compared to open Bankart repair as already reported in previous studies (Table 4) and a recent Meta-Analysis 25, but the observed difference did not reach statistically significance. However, the recurrences of instability after artroscopically treated patients were observed earlier than after open treatment (Figure 1).
Table 4.
Studies comparing open and arthroscopic Bankart procedure
| Study | Year | Design | Artroscopic technique |
Total number open/arthroscopic |
Follow-up open/arthroscopic |
Recurrence open/arthroscopic |
|---|---|---|---|---|---|---|
| Steinbeck et al. | 1998 [40] |
prospective | transglenoid suture | 32/30 | 40/36 months | 6%/17% |
| Sisto et al. | 1998 [37] |
retrospective | Suretac | 7/23 | 47/47 months | 0%/13% |
| Kartus et al. | 1998 [21] |
retrospective | Suretac | 18/18 | 31/28 months | 0%/0% |
| Jorgensen et al. | 1999 [17] |
prospective | transglenoid suture | 20/21 | 36/36 months | 0%/5% |
| Kim et al. | 2002 [22] |
retrospective | suture anchors | 30/59 | 39/39 months | 6.7%/3.4% |
| Fabbriciani et al. | 2004 [9] |
prospective randomized | suture anchors | 30/30 | 24/24 months | 0%/0% |
| Tjoumakaris et al. | 2006 [42] |
retrospective | suture anchors | 24/69 | 42/42 months | 4%/1% |
| Bottoni et al. | 2006 [4] |
prospective randomized |
suture anchors | 29/32 | 32/32 months | 7%/3% |
|
Including subluxations |
||||||
| Jorgensen et al. | 1998 [17] |
prospective | transglenoid suture | 20/21 | 36/36 months | 10%/10% |
| Cole et al. | 2000 [6] |
prospective | Suretac | 20/37 | 54/54 months | 9%/16% 18%/24% (incl. positive apprehension test) |
| Sperber et al. | 2001 [38] |
prospective randomized |
Suretac | 26/30 | 24/24 months | 12%/23% |
| Karlsson et al. | 2001 [20] |
prospective | Suretac | 40/60 | 36/28 months | 10%/15% |
These findings may be due to methodological limitation of the study with its retrospective cross-sectional implementation. The treatment samples differed, for example, in the number of dislocations before surgery, in the duration from first dislocation to surgery and in the degree of Bankart lesion and capsular elongation. Another reason for this difference might be the different surgical treatment of the capsule. Although decision for arthroscopic treatment was done after arthroscopic assesment and only patients with considered not elongated capsule were treated arthroscopically the higher recurrence rate in the arthroscopic group may be caused by patient selection. 40% of arthroscopic repairs were performed in patients with more than 5 dislocations before surgery and showed a higher failure rate as has been reported before [19]. The assessment of capsular elongation and quality can be difficult during arthroscopy. We did no capsulorraphy during arthroscopic procedure but an additional capsular shift was performed in 28% of the open Bankart repairs.
Although operated on by a single surgeon (MB) experienced in arthroscopic surgery the number of arthroscopic procedures is quite low and the individual learning curve is included which can lead to a greater recurrence rate [10,27]. However, there was no increased failure rate in the earlier compared to the later treated patients.
Despite its limitations, this investigation indicates, that the clinical outcome after arthroscopic Bankart procedure with no capsular shift seems to be inferior to the results after open surgery and corresponds to previous studies [6,10,17,20,21,37-39] (Table 4). In these studies arthroscopic repair has been performed with different techniques (transglenoid sutures, tacks) and mostly no capsular tightening has been done. Recent studies [4,9,22,42] with suture anchor fixation demonstrate, that equally good results can be achieved for selected patients and in specialized institutions [18] after arthroscopic Bankart repair.
Main disadvantage of open Bankart procedure is the violation of of the subscapularis tendon and therefore the possibility of subscapularis muscle insufficiency [35]. In our patients with open procedures we did not observe any case of clinical subscapularis muscle insufficiency and therefore we consider this not to be a problem as long as thorough dissection and reattachment of the tendon is done.
Another frequently reported disadvantage is loss of range of motion [4,6,17,21]. We observed an external rotation lag of 20° or more in 16% after open and only 3% after artroscopic treatment. This may be an effect of the capsular shift in the open procedures. This external rotation lag was tolerated by most patients as the better rating after open procedure suggests. Nonetheless this can be a problem for some patients who require full range of motion.
Various scoring systems are established but most studies used the Rowe score [33] for assessment of functional results after operative shoulder stabilization [3,9,20,23,32,38]. We found similar good results as reported by these studies in both groups regarding the Rowe score as well as the modified Rowe score [34].
Conclusion
In this retrospective investigation the open Bankart procedure demonstrated good functional results, a gradual loss of external rotation which was tolerated by most patients and no clinical signs of subcapularis muscle insufficiency. The arthroscopic treatment without capsular shift resulted in a better range of motion, but showed a tendency towards more frequently and earlier recurrence of instability. The authors recommend sensitive patient selection for arthroscopic Bankart repair especially in patients with more than five dislocations. An additional capsular shift should be performed in these patients.
The data of this paper has been presented at the 8th EFORT Congress, 11-15 May 2007 in Firenze, Italy, at the 24. AGA Congress, 27-29 September 2007 in Köln, Germany and at the Congress of the German Orthopedic Society, 24-27 October 2007, Berlin. Parts of this presentation are contained in the Doctoral Thesis of Ms Juliane Lübke (Dresden University of Technology, Medical Faculty).
Conflict of interests
The authors have no commercial or political interests in the methodological or medical aspects presented in this paper. There are no financial or other relationships that might lead to a conflict of interest. The manuscript has been read and approved by all authors. Each author believes that the manuscript represents innovative and original work.
References
- Angelo RL. Controversies in arthroscopic shoulder surgery: arthroscopic versus open bankart repair, thermal treatment of capsular tissue, acromioplasties--are they necessary? Arthroscopy. 2003;19(Suppl 1):224–228. doi: 10.1016/j.arthro.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Bankart ASB. The pathology and treatment of recurrent dislocation of the shoulder joint. Br J Surg. 1938;26:23–29. doi: 10.1002/bjs.18002610104. [DOI] [Google Scholar]
- Barber FA, Snyder SJ, Abrams JS, Fanelli GC, Savoie FH. Arthroscopic Bankart reconstruction with a bioabsorbable anchor. J Shoulder Elbow Surg. 2003;12(6):535–538. doi: 10.1016/S1058-2746(03)00175-7. [DOI] [PubMed] [Google Scholar]
- Bottoni PC, Smith EL, Berkowitz MJ, Towle RB, Moore JH. Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med. 2006;34(11):1730–1737. doi: 10.1177/0363546506288239. [DOI] [PubMed] [Google Scholar]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- Cole BJ, L'Insalata J, Irrgang J, Warner JJ. Comparison of arthroscopic and open anterior shoulder stabilization. A two to six-year follow-up study. J Bone Joint Surg Am. 2000;82-A(8):1108–11014. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- Coughlin L, Rubinovich M, Johansson J, White B, Green-spoon J. Arthroscopic staple capsulorrhaphy for anterior shoulder instability. Am J Sports Med. 1992;20(3):253–256. doi: 10.1177/036354659202000303. [DOI] [PubMed] [Google Scholar]
- Dora C, Gerber C. Shoulder function after arthroscopic anterior stabilization of the glenohumeral joint using an absorbable tac. J Shoulder Elbow Surg. 2000;9(4):294–298. doi: 10.1067/mse.2000.106745. [DOI] [PubMed] [Google Scholar]
- Fabbriciani C, Milano G, Demontis A, Fadda S, Ziranu F, Mulas PD. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy. 2004;20(5):456–462. doi: 10.1016/j.arthro.2004.03.001. [DOI] [PubMed] [Google Scholar]
- Freedman KB, Smith AP, Romeo AA, Cole BJ, Bach BR Jr. Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for Recurrent Anterior instability of the shoulder: a meta-analysis. Am J Sports Med. 2004;32(6):1520–1527. doi: 10.1177/0363546504265188. [DOI] [PubMed] [Google Scholar]
- Gartsman GM, Roddey TS, Hammerman SM. Arthroscopic treatment of anterior-inferior glenohumeral instability. Two to five-year follow-up. J Bone Joint Surg Am. 2000;82-A(7):991–1003. doi: 10.2106/00004623-200007000-00011. [DOI] [PubMed] [Google Scholar]
- Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br. 1991;73(3):389–394. doi: 10.1302/0301-620X.73B3.1670434. [DOI] [PubMed] [Google Scholar]
- Gill TJ, Zarins B. Open repairs for the treatment of anterior shoulder instability. Am J Sports Med. 2003;31(1):142–153. doi: 10.1177/03635465030310011001. [DOI] [PubMed] [Google Scholar]
- Green MR, Christensen KP. Arthroscopic Bankart procedure: two-to five-year followup with clinical correlation to severity of glenoid labral lesion. Am J Sports Med. 1995;23(3):276–281. doi: 10.1177/036354659502300304. [DOI] [PubMed] [Google Scholar]
- Jaeger A, Braune C, Welsch F, Sarikaya Y, Graichen H. Postoperative functional outcome and stability in recurrent traumatic anteroinferior glenohumeral instability: comparison of two different surgical capsular reconstruction techniques. Arch Orthop Trauma Surg. 2004;124(4):226–231. doi: 10.1007/s00402-003-0601-1. [DOI] [PubMed] [Google Scholar]
- Jolles BM, Pelet S, Farron A. Traumatic recurrent anterior dislocation of the shoulder: two-to four-year follow-up of an anatomic open procedure. J Shoulder Elbow Surg. 2004;13(1):30–34. doi: 10.1016/j.jse.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Jorgensen U, Svend-Hansen H, Bak K, Pedersen I. Recurrent post-traumatic anterior shoulder dislocation-open versus arthroscopic repair. Knee Surg Sports Traumatol Arthrosc. 1999;7(2):118–124. doi: 10.1007/s001670050133. [DOI] [PubMed] [Google Scholar]
- Kailes SB, Richmond JC. Arthroscopic vs. open Bankart reconstruction: a comparison using expected value decision analysis. Knee Surg Sports Traumatol Arthrosc. 2001;9(6):379–385. doi: 10.1007/s001670100210. [DOI] [PubMed] [Google Scholar]
- Kandziora F, Jager A, Bischof F, Herresthal J, Starker M, Mittlmeier T. Arthroscopic labrum refixation for post-traumatic anterior shoulder instability: suture anchor versus transglenoid fixation technique. Arthroscopy. 2000;16(4):359–366. doi: 10.1016/S0749-8063(00)90079-3. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Magnusson L, Ejerhed L, Hultenheim I, Lundin O, Kartus J. Comparison of open and arthroscopic stabilization for recurrent shoulder dislocation in patients with a Bankart lesion. Am J Sports Med. 2001;29(5):538–542. doi: 10.1177/03635465010290050201. [DOI] [PubMed] [Google Scholar]
- Kartus J, Ejerhed L, Funck E, Kohler K, Sernert N, Karlsson J. Arthroscopic and open shoulder stabilization using absorbable implants. A clinical and radiographic comparison of two methods. Knee Surg Sports Traumatol Arthrosc. 1998;6(3):181–188. doi: 10.1007/s001670050096. [DOI] [PubMed] [Google Scholar]
- Kim SH, Ha KI. Bankart repair in traumatic anterior shoulder instability: open versus arthroscopic technique. Arthroscopy. 2002;18(7):755–763. doi: 10.1053/jars.2002.31701. [DOI] [PubMed] [Google Scholar]
- Kim SH, Ha KI, Cho YB, Ryu BD, Oh I. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am. 2003;85-A(8):1511–1518. [PubMed] [Google Scholar]
- Langford J, Bishop J, Lee E, Flatow E. Outcomes following open repair of Bankart lesions for recurrent, traumatic anterior glenohumeral dislocations. Orthopedics. 2006;29(11):1008–1013. doi: 10.3928/01477447-20061101-06. [DOI] [PubMed] [Google Scholar]
- Lenters TR, Franta AK, Wolf FM, Leopold SS, Matsen FA. Arthroscopic compared with open repairs for recurrent anterior shoulder instability. A systematic review and meta-analysis of the literature. J Bone Joint Surg Am. 2007;89(2):244–254. doi: 10.2106/JBJS.E.01139. [DOI] [PubMed] [Google Scholar]
- Magnusson L, Kartus J, Ejerhed L, Hultenheim I, Sernert N, Karlsson J. Revisiting the open Bankart experience: a four-to nine-year follow-up. Am J Sports Med. 2002;30(6):778–782. doi: 10.1177/03635465020300060401. [DOI] [PubMed] [Google Scholar]
- Mologne TS, McBride MT, Lapoint JM. Assessment of failed arthroscopic anterior labral repairs. Findings at open surgery. Am J Sports Med. 1997;25(6):813–817. doi: 10.1177/036354659702500614. [DOI] [PubMed] [Google Scholar]
- Neer CS, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980;62(6):897–908. [PubMed] [Google Scholar]
- Pagnani MJ, Dome DC. Surgical treatment of traumatic anterior shoulder instability in American football players. J Bone Joint Surg Am. 2002;84-A(5):711–715. doi: 10.2106/00004623-200205000-00002. [DOI] [PubMed] [Google Scholar]
- Pagnani MJ, Warren RF, Altchek DW, Wickiewicz TL, Anderson AF. Arthroscopic shoulder stabilization using transglenoid sutures. A four-year minimum followup. Am J Sports Med. 1996;24(4):459–467. doi: 10.1177/036354659602400409. [DOI] [PubMed] [Google Scholar]
- Perthes GC. Über Operationen bei habitueller Schulterluxation. Dtsch Z Chir. 1906;85:199. doi: 10.1007/BF02894989. [DOI] [Google Scholar]
- Potzl W, Witt KA, Hackenberg L, Marquardt B, Steinbeck J. Results of suture anchor repair of anteroinferior shoulder instability: a prospective clinical study of 85 shoulders. J Shoulder Elbow Surg. 2003;12(4):322–326. doi: 10.1016/S1058-2746(03)00032-6. [DOI] [PubMed] [Google Scholar]
- Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60(1):1–16. [PubMed] [Google Scholar]
- Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am. 1981;63(6):863–872. [PubMed] [Google Scholar]
- Scheibel M, Tsynman A, Magosch P, Schroeder RJ, Habermeyer P. Postoperative subscapularis muscle insufficiency after primary and revision open shoulder stabilization. Am J Sports Med. 2006;34(10):1586–1593. doi: 10.1177/0363546506288852. [DOI] [PubMed] [Google Scholar]
- Silliman JF, Hawkins RJ. Classification and physical diagnosis of instability of the shoulder. Clin Orthop Relat Res. 1993. pp. 7–19. [PubMed]
- Sisto DJ, Cook DL. Intraoperative decision making in the treatment of shoulder instability. Arthroscopy. 1998;14(4):389–394. doi: 10.1016/S0749-8063(98)70006-4. [DOI] [PubMed] [Google Scholar]
- Sperber A, Hamberg P, Karlsson J, Sward L, Wredmark T. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. J Shoulder Elbow Surg. 2001;10(2):105–108. doi: 10.1067/mse.2001.112019. [DOI] [PubMed] [Google Scholar]
- Steinbeck J, Jerosch J. Arthroscopic transglenoid stabilization versus open anchor suturing in traumatic anterior instability of the shoulder. Am J Sports Med. 1998;26(3):373–378. doi: 10.1177/03635465980260030501. [DOI] [PubMed] [Google Scholar]
- Steinbeck J, Jerosch J. [Open Bankart repair using suture anchors in posttraumatic shoulder instability: 2 to 5-year results] Unfallchirurg. 1997;100(12):938–942. doi: 10.1007/s001130050215. [DOI] [PubMed] [Google Scholar]
- Thomas SC, Matsen FA. An approach to the repair of avulsion of the glenohumeral ligaments in the management of traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 1989;71(4):506–513. [PubMed] [Google Scholar]
- Tjoumakaris FP, Abboud JA, Hasan SA, Ramsey ML, Williams GR. Arthroscopic and open Bankart repairs provide similar outcomes. Clin Orthop Relat Res. 2006;446:227–232. doi: 10.1097/01.blo.0000205883.73705.19. [DOI] [PubMed] [Google Scholar]


