Abstract
The public health threat of orthopoxviruses from bioterrorist attacks has prompted researchers to develop suitable animal models for increasing our understanding of viral pathogenesis and evaluation of medical countermeasures (MCMs) in compliance with the FDA Animal Efficacy Rule. We present an accessible intrabronchial cowpox virus (CPXV) model that can be evaluated under biosafety level-2 laboratory conditions. In this dose-ranging study, utilizing cynomolgus macaques, signs of typical orthopoxvirus disease were observed with the lymphoid organs, liver, skin (generally mild) and respiratory tract as target tissues. Clinical and histopathological evaluation suggests that intrabronchial CPXV recapitulated many of the features of monkeypox and variola virus, the causative agent of smallpox, infections in cynomolgus macaque models. These similarities suggest that CPXV infection in non-human primates should be pursued further as an alternative model of smallpox. Further development of the CPXV primate model, unimpeded by select agent and biocontainment restrictions, should facilitate the development of MCMs for smallpox.
Four factors drive the need for improved non-human primate (NHP) models of orthopoxvirus infection: (i) the increased threat of intentional release of variola virus (VARV), the causative agent of smallpox, as a bioterrorism weapon, (ii) the increased frequency of sporadic cases and spread of zoonotic orthopoxviruses including cowpox (CPXV) (Vorou et al., 2008) and particularly monkeypox virus (MPXV) (Parker et al., 2007; Rimoin et al., 2010) in humans, (iii) the uncertain future of VARV research due to increased interest in eradication of the known VARV stocks (Lane & Poland, 2011; McFadden, 2010; Tucker, 2011), and (iv) the lack of an NHP model that fully mimics the natural route or course of infection as mandated by the FDA ‘Animal Rule’. To fulfil the requirements of the ‘Animal Rule’, a medical countermeasure (MCM) must demonstrate efficacy in at least two animal models in which the route and dose of virus administration, time to onset of disease and time-course/progression of infection optimally reflects human disease (FDA, 2009). To this end, animal model development in multiple species and using natural routes of transmission must be explored to effectively evaluate MCMs. CPXV-induced disease may serve as an ideal model for orthopoxviruses because (i) CPXV is a biosafety level-2 (BSL-2) pathogen, (ii) CPXV shares homology with MPXV and VARV (Lefkowitz et al., 2005; Seet et al., 2003; Xing et al., 2006), and (iii) CPXV produces disease in mice and NHPs (Bray et al., 2000; Martinez et al., 2000).
Recent studies suggest that CPXV inoculation of NHPs may serve as an additional model of VARV infection that would increase our knowledge of orthopoxvirus disease progression in NHPs. We have recently described the disease progression of CPXV Brighton Red strain after intravenous (i.v.) inoculation of cynomolgus macaques (Macaca fascicularis). i.v. inoculation resulted in a rapid, fulminant haemorrhagic disease that shared several characteristics with human haemorrhagic smallpox (Johnson et al., 2011b). Other groups have explored common marmosets as an alternative NHP model of orthopoxvirus disease after an outbreak of CPXV in a German zoo (Martina et al., 2006; Mätz-Rensing et al., 2006). A follow-up study exploring CPXV infection of marmosets revealed that the LD50 via intranasal inoculation in marmosets was <103 p.f.u. and the Calpox variant produced some typical signs of poxvirus disease (Kramski et al., 2010). Establishment of the marmoset cowpox model is significant, but critical reagents are not readily available for marmosets, and i.v. MPXV infection of macaques is the most widely established NHP orthopoxvirus model for testing MCMs (Chen et al., 2005; Earl et al., 2008; Edghill-Smith et al., 2005; Hooper et al., 2004; Huggins et al., 2009; Jahrling et al., 2004; Stittelaar et al., 2001). The investigation of CPXV-induced disease in macaques and exploration of respiratory exposure is desirable to establish a CPXV model as an alternative to MPXV and VARV NHP models of orthopoxvirus infection. Here, we demonstrate that intrabronchial (IB) inoculation of CPXV Brighton Red strain in cynomolgus macaques results in a disease that shares features with MPXV- and VARV-induced disease. Our results suggest that route of inoculation influences disease presentation of CPXV infection, and continued experimentation with inoculation routes will further refine NHP orthopoxvirus models.
Four groups of two cynomolgus macaques were inoculated with serial 10-fold dilutions of CPXV from 5×107 to 5×104 p.f.u. by IB inoculation using a paediatric bronchoscope as described previously (Johnson et al., 2011a). The inoculum was delivered in a volume of 5 ml and deposited in the left tertiary bronchus. NHPs were monitored daily. Blood was drawn for analysis and physical exams were performed periodically throughout the study (days 0, 2, 4, 6, 8, 10, 12, 16, 21 and 28). All animal handling and clinical procedures were performed while NHPs were anaesthetized with Ketamine or Telazol. Complete necropsies were performed when NHPs met established clinical end-point criteria or at study end (day 28). NHPs were deeply anaesthetized with Telazol or Ketamine and humanely euthanized by i.v. pentobarbital overdose. All animal procedures adhered to National Institutes of Health (NIH) policies, including those set forth in the Guide for the Care and Use of Laboratory Animals, and were approved by the National Institute of Allergy and Infectious Diseases Animal Care and Use Committee.
Clinical signs of disease following CPXV IB inoculation included dyspnoea, inappetance and minor cutaneous erythema. Lesion severity was mild compared with MPXV- and VARV-induced disease in humans with seven of eight NHPs developing six or fewer lesions. One NHP receiving 5×106 p.f.u. of CPXV developed 445 lesions (Table 1). All NHPs in the 5×107 p.f.u. and 5×106 p.f.u. groups succumbed on days 7 and 11 post-inoculation (p.i.) and days 11 and 15 p.i., respectively. IB inoculation with 5×105 p.f.u of CPXV resulted in one of two NHPs succumbing on day 14 p.i., and administration of 5×104 p.f.u. of CPXV did not result in lethal disease. Although the group size is small, data obtained in this study suggest that 5×105 p.f.u. of CPXV may be the LD50 following CPXV IB inoculation. By comparison, inoculation of 5×105 p.f.u. of CPXV i.v. was 100 % lethal. The LD50 of CPXV i.v. has yet to be determined (Johnson et al., 2011b), but is likely to be several log10 p.f.u. lower than IB CPXV inoculation.
Table 1. IB CPXV infection of cynomolgus macaques results in severe disease.
na, Not applicable.
| Dose (p.f.u.) | NHP | Day of clinical end-point | Peak no. of skin lesions | Peak viraemia (log10 gene copies ml−1) | Peak viral load in nasal eluates (log10 gene copies ml−1) | Viral load in indicated tissue (log10 p.f.u. g−1)* | ||||||
| Lung | Liver | Lymph nodes† | Spleen | Central nervous system‡ | Trachea | Nares | ||||||
| 5×104 | 8034 | na§ | 6 | 5.1 | 6.3 | <|| | < | < | < | < | < | < |
| 5014 | na | 4 | 6.4 | 3.8 | < | < | < | < | < | < | < | |
| 5×105 | 5094 | na | 2 | 4.9 | 3.1 | < | < | < | < | < | < | < |
| 3606 | 14 | 1 | 6.9 | 7.1 | 7.0 | < | < | < | < | < | < | |
| 5×106 | 8028 | 11 | 4 | 6.9 | 7.2 | 7.3 | 5.9 | 5.1 | < | < | 5.4 | 4.5 |
| 4083 | 15 | 445 | 8.0 | 7.8 | 8.0 | 5.1 | 6.4 | 8.8 | 7.2 | 7.5 | 7.6 | |
| 5×107 | 2023 | 11 | 6 | 8.0 | 7.8 | 8.6 | 7.7 | 6.4 | 7.8 | 5.2 | 9.2 | 6.7 |
| 9051 | 7 | 2 | 5.9 | 6.0 | 7.3 | 6.0 | 5.8 | < | 5.3 | < | 5.4 | |
Tissues were assayed for viral load at time of necropsy on day of clinical end-point (3606, 8028, 4083, 2023 and 9051) or at study end (day 28).
Lymph node was average of inguinal bronchial and submandibular lymph node tissues.
Central nervous system was average of thoracic and lumbar spinal cord.
Indicated NHPs survived to study end (day 28).
No virus detected.
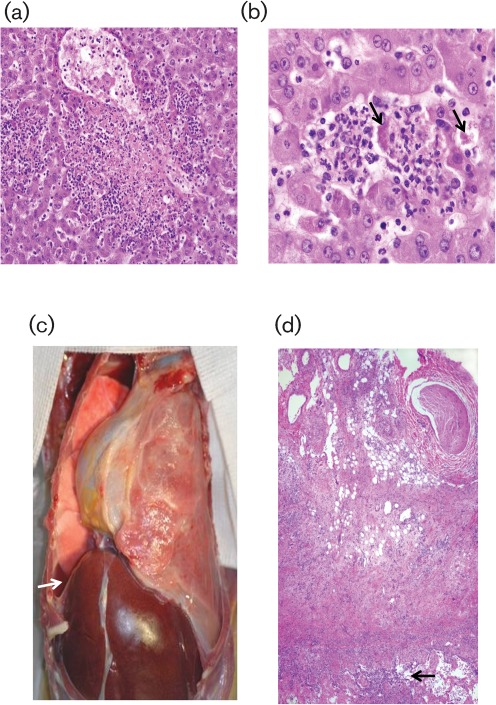
Histopathological changes in lymph nodes or liver following CPXV IB inoculation were similar to those observed following lethal i.v., IB, intratracheal or aerosol challenge of MPXV in NHPs (Goff et al., 2011; Johnson et al., 2011a; Zaucha et al., 2001), i.v. inoculation of CPXV in NHPs (Johnson et al., 2011b), naturally occurring MPXV in a prairie dog (Langohr et al., 2004) and patients with smallpox (Bras, 1952; Lillie, 1930; Martin, 2002). Analysis of haematoxylin and eosin (H&E) stained tissue sections revealed the following morphological changes: lymph nodes indicated oedema and histiocytosis in non-survivors independent of dose and lymphoid hyperplasia in surviving NHPs. There were multifocal neutrophilic infiltrates within the liver (Fig. 1a) at all doses, and some liver sections displayed hepatocellular degeneration. Intrahepatocyte, intracytoplamsic inclusion bodies were also detected in one NHP in the 5×106 p.f.u. dose group (Fig. 1b).
Fig. 1.
Gross necropsy and histopathology of H&E stained tissue sections of intrabronchially cowpox inoculated NHPs. (a) Hepatic centrilobular necrosis with monocytic infiltrates (×10). (b) Intracytoplasmic inclusion bodies within hepatocytes (arrows) and neutrophilic infiltrates (×40). (c) Lung consolidation and oedema (arrow) observed at gross necropsy of a 5×106 p.f.u. NHP (NHP 8028). (d) H&E lung tissue section demonstrating severe pleuritis and alveolar infiltrates (arrow) (×5).
IB CPXV infection shares many similarities with other orthopoxvirus airway inoculation models; however, comparison of the IB CPXV infection with human VARV disease suggests that lung disease is exaggerated in CPXV IB-inoculated NHPs. IB CPXV inoculation resulted in consolidated lungs with oedema and atelectasis in non-surviving NHPs (Fig. 1c). H&E staining of lung tissue from non-surviving NHPs from the 5×107, 5×106 and 5×105 p.f.u. dose groups revealed severe necrotizing pleuritis, alveolar oedema, necrotic bronchiolar epithelium and diffuse vascular congestion (Fig. 1d). CPXV IB inoculated NHPs shared similarities with aerosolized MPXV-infected animals; both displayed fibrinous pleuritis with pleural adhesions and multifocal, white, plaque-like thickenings of the visceral pleura (Zaucha et al., 2001). Similar to MPXV IB inoculation, CPXV IB inoculation resulted in pneumonia, congestion and pleural adhesions (Johnson et al., 2011a). Bronchopneumonia, bronchitis, bronchiolitis, oedema and, rarely, atelectasis was observed in 25 of 177 fatal VARV human cases reviewed by Bras (1952) and 17 of 54 cases reviewed by Councilman (Bras, 1952; Councilman et al., 1904). During the USA 2003 MPXV outbreak, coughing was a common symptom and dyspnoea was observed less frequently (Chapman et al., 2010; Reynolds et al., 2006).
Viral load in the blood and nasal swabs were measured by qPCR and viral load in 72 tissues collected at necropsy were determined by plaque assay of tissue homogenates on Vero cells as described previously (Johnson et al., 2011a). Viral load data are summarized in Table 1. Viral load in whole blood and nasal swabs was initially detected between days2 and 6 for all groups, and peak viral load in blood as measured by qPCR ranged from 4.9 to 8.0 log10 gene copies ml−1 with surviving NHPs generally developing lower peak viral load than non-survivors (Table 1). The four NHPs that succumbed at higher doses (5×106 or 5×107 p.f.u.) of CPXV had high viral titres in several tissues, indicating a systemic infection. Each of the NHPs in the 5×106 and 5×107 p.f.u. dose groups had virus concentrations ranging from 4.5 to 9.2 log10 p.f.u. g−1 in tissue samples from the lymph nodes, lungs, liver and nares at moribund end-point. Three of four NHPs in these groups also had detectable virus in the skin (data not shown), central nervous system and spleen. Similar to human patients with MPXV (Müller et al., 1988), CPXV was isolated from livers of four of five moribund animals.
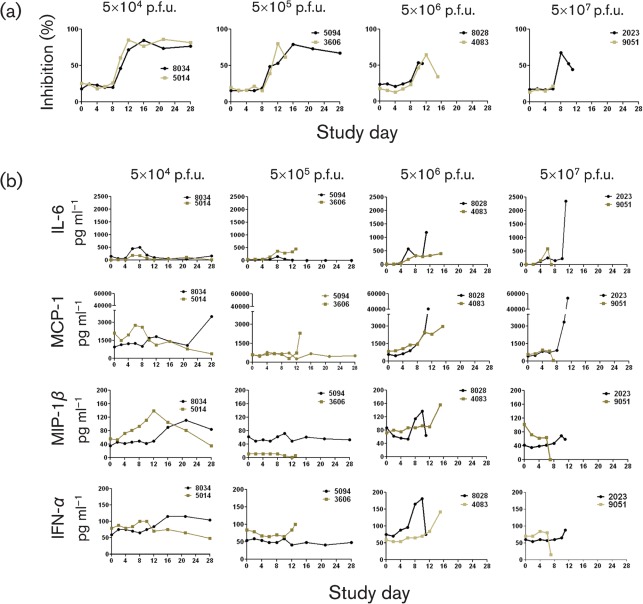
The immune response to CPXV infection was evaluated by measuring the neutralizing antibody activity and cytokine concentrations in serum. Neutralizing antibody activity was detected using a flow cytometry-based assay modified from Earl et al. (2003) and serum cytokine concentrations were measured using the Biosource human cytokine multiplex-25 bead array assay kit (Invitrogen). Seven of eight infected NHPs developed detectable neutralizing antibody against CPXV, and the neutralizing antibody activity rapidly increased between days 8 and 10 p.i. and plateaued in surviving NHPs by day 16 (Fig. 2a). The NHP that received 5×107 p.f.u and succumbed on day 7 did not develop any detectable neutralizing antibody. However, the remaining NHPs that succumbed did develop neutralizing antibody by day 10 p.i. The peak neutralizing antibody titre was not maintained and declined by moribund end-point. The data suggest that the neutralizing antibody response alone was probably not sufficient to resolve CPXV infection. The serum concentrations of 25 cytokines and chemokines were analysed over the course of the study and increases in interleukin (IL)-6 and monocyte chemoattractant protein-1 (MCP-1) serum concentrations were observed in NHPs infected with 5×106 and 5×107 p.f.u. of CPXV, although the peak concentrations varied widely (Fig. 2b). In addition, concentrations of macrophage inflammatory protein-1β (MIP-1β) and alpha interferon (IFN-α) were elevated in NHPs inoculated with 5×106 p.f.u. of CPXV. The increases in MIP-1β, IL-6 and MCP-1 demonstrated similar trends when compared to VARV infection in NHPs (Jahrling et al., 2004).
Fig. 2.
(a) The level of neutralizing antibodies in CPXV-infected NHPs was measured by a flow cytometric assay using a VACV expressing GFP (VACV–GFP) as the target virus. CV-1 cells (5×104) were incubated with VACV–GFP at an m.o.i. of 2.5 in the presence of 44 µg cytosine arabinoside and sera (diluted 1 : 1000) from infected NHPs for 18–24 h. Prior to addition to the cells, the sera and virus were allowed to complex for 1 h at 37 °C. Following incubation, cells were trypsinized (Trypsin+2.5 % EDTA), washed twice in PBS+2 % FBS, and analysed by flow cytometry for GFP expression. (b) The concentration of selected cytokines and chemokines in serum samples from CPXV-infected NHPs indicate a strong, but variable pro-inflammatory response. Serum cytokine concentrations were measured using the Biosource human cytokine multiplex-25 bead array assay kit (Invitrogen) from serum samples drawn throughout the study.
Similarities between VARV-, MPXV- and CPXV-induced disease include target organs, viraemia, upregulation of MCP-1, IL-6 and MIP-1β, similar histopathology findings and development of neutralizing antibody. The small sample size evaluated limited the utility of statistical analysis of this dataset, but the observed disease and similarity in disease presentation when compared to VARV infection of humans suggests that CPXV infection of cynomolgus macaques by airway exposure may provide an effective model of human VARV infection. By further developing CPXV airway models in parallel with recognized poxvirus models, we hope to establish CPXV infection as a suitable BSL-2 NHP model that would provide greater access of orthopoxvirus models to the research community, thus facilitating the development of improved vaccines and anti-orthopoxvirus therapeutics.
Acknowledgements
This work was supported in part by the NIAID Division of Intramural Research. We wish to thank Catherine Jett, Leslie Wachter, Sarah Rovezzi, Lily Cheng and the Division of Intramural Research Comparative Medicine Branch staff for contribution to these studies. We also thank Grant McFadden Ph.D., University of Florida for cowpox Brighton Red.
References
- Bras G. (1952). The morbid anatomy of smallpox. Doc Med Geogr Trop 4, 303–351 [PubMed] [Google Scholar]
- Bray M., Martinez M., Smee D. F., Kefauver D., Thompson E., Huggins J. W. (2000). Cidofovir protects mice against lethal aerosol or intranasal cowpox virus challenge. J Infect Dis 181, 10–19 10.1086/315190 [DOI] [PubMed] [Google Scholar]
- Chapman J. L., Nichols D. K., Martinez M. J., Raymond J. W. (2010). Animal models of orthopoxvirus infection. Vet Pathol 47, 852–870 10.1177/0300985810378649 [DOI] [PubMed] [Google Scholar]
- Chen N., Li G., Liszewski M. K., Atkinson J. P., Jahrling P. B., Feng Z., Schriewer J., Buck C., Wang C., Lefkowitz E. (2005). Virulence differences between monkeypox virus isolates from West Africa and the Congo basin. Virology 340, 46–63 10.1016/j.virol.2005.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Councilman W. T., Magrath G. B., Brinckerhoff W. R. (1904). The pathological anatomy and histology of variola. J Med Res 11, 12–135 [PMC free article] [PubMed] [Google Scholar]
- Earl P. L., Americo J. L., Moss B. (2003). Development and use of a vaccinia virus neutralization assay based on flow cytometric detection of green fluorescent protein. J Virol 77, 10684–10688 10.1128/JVI.77.19.10684-10688.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earl P. L., Americo J. L., Wyatt L. S., Espenshade O., Bassler J., Gong K., Lin S., Peters E., Rhodes L., Jr & other authors (2008). Rapid protection in a monkeypox model by a single injection of a replication-deficient vaccinia virus. Proc Natl Acad Sci U S A 105, 10889–10894 10.1073/pnas.0804985105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edghill-Smith Y., Bray M., Whitehouse C. A., Miller D., Mucker E., Manischewitz J., King L. R., Robert-Guroff M., Hryniewicz A. & other authors (2005). Smallpox vaccine does not protect macaques with AIDS from a lethal monkeypox virus challenge. J Infect Dis 191, 372–381 10.1086/427265 [DOI] [PubMed] [Google Scholar]
- FDA (2009). Guidance for Industry: Animal Models – essential elements to address efficacy under the animal rule: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm078923.pdf
- Goff A. J., Chapman J., Foster C., Wlazlowski C., Shamblin J., Lin K., Kreiselmeier N., Mucker E., Paragas J. & other authors (2011). A novel respiratory model of infection with monkeypox virus in cynomolgus macaques. J Virol 85, 4898–4909 10.1128/JVI.02525-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper J. W., Thompson E., Wilhelmsen C., Zimmerman M., Ichou M. A., Steffen S. E., Schmaljohn C. S., Schmaljohn A. L., Jahrling P. B. (2004). Smallpox DNA vaccine protects nonhuman primates against lethal monkeypox. J Virol 78, 4433–4443 10.1128/JVI.78.9.4433-4443.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huggins J., Goff A., Hensley L., Mucker E., Shamblin J., Wlazlowski C., Johnson W., Chapman J., Larsen T. & other authors (2009). Nonhuman primates are protected from smallpox virus or monkeypox virus challenges by the antiviral drug ST-246. Antimicrob Agents Chemother 53, 2620–2625 10.1128/AAC.00021-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrling P. B., Hensley L. E., Martinez M. J., Leduc J. W., Rubins K. H., Relman D. A., Huggins J. W. (2004). Exploring the potential of variola virus infection of cynomolgus macaques as a model for human smallpox. Proc Natl Acad Sci U S A 101, 15196–15200 10.1073/pnas.0405954101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R. F., Dyall J., Ragland D. R., Huzella L., Byrum R., Jett C., St Claire M., Smith A. L., Paragas J. & other authors (2011a). Comparative analysis of monkeypox virus infection of cynomolgus macaques by the intravenous or intrabronchial inoculation route. J Virol 85, 2112–2125 10.1128/JVI.01931-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R. F., Yellayi S., Cann J. A., Johnson A., Smith A. L., Paragas J., Jahrling P. B., Blaney J. E. (2011b). Cowpox virus infection of cynomolgus macaques as a model of hemorrhagic smallpox. Virology 418, 102–112 10.1016/j.virol.2011.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramski M., Mätz-Rensing K., Stahl-Hennig C., Kaup F. J., Nitsche A., Pauli G., Ellerbrok H. (2010). A novel highly reproducible and lethal nonhuman primate model for orthopox virus infection. PLoS ONE 5, e10412 10.1371/journal.pone.0010412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane J. M., Poland G. A. (2011). Why not destroy the remaining smallpox virus stocks? Vaccine 29, 2823–2824 10.1016/j.vaccine.2011.02.081 [DOI] [PubMed] [Google Scholar]
- Langohr I. M., Stevenson G. W., Thacker H. L., Regnery R. L. (2004). Extensive lesions of monkeypox in a prairie dog (Cynomys sp). Vet Pathol 41, 702–707 10.1354/vp.41-6-702 [DOI] [PubMed] [Google Scholar]
- Lefkowitz E. J., Upton C., Changayil S. S., Buck C., Traktman P., Buller R. M. (2005). Poxvirus Bioinformatics Resource Center: a comprehensive Poxviridae informational and analytical resource. Nucleic Acids Res 33 (Database issue), D311–D316 10.1093/nar/gki110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillie R. D. (1930). Smallpox and vaccinia: the pathologic histology. Arch Pathol (Chic) 10, 241–291 [Google Scholar]
- Martin D. B. (2002). The cause of death in smallpox: an examination of the pathology record. Mil Med 167, 546–551 [PubMed] [Google Scholar]
- Martina B. E., van Doornum G., Dorrestein G. M., Niesters H. G., Stittelaar K. J., Wolters M. A., van Bolhuis H. G., Osterhaus A. D. (2006). Cowpox virus transmission from rats to monkeys, the Netherlands. Emerg Infect Dis 12, 1005–1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez M. J., Bray M. P., Huggins J. W. (2000). A mouse model of aerosol-transmitted orthopoxviral disease: morphology of experimental aerosol-transmitted orthopoxviral disease in a cowpox virus-BALB/c mouse system. Arch Pathol Lab Med 124, 362–377 [DOI] [PubMed] [Google Scholar]
- Mätz-Rensing K., Ellerbrok H., Ehlers B., Pauli G., Floto A., Alex M., Czerny C. P., Kaup F. J. (2006). Fatal poxvirus outbreak in a colony of New World monkeys. Vet Pathol 43, 212–218 10.1354/vp.43-2-212 [DOI] [PubMed] [Google Scholar]
- McFadden G. (2010). Killing a killer: what next for smallpox? PLoS Pathog 6, e1000727 10.1371/journal.ppat.1000727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller G., Meyer A., Gras F., Emmerich P., Kolakowski T., Esposito J. J. (1988). Monkeypox virus in liver and spleen of child in Gabon. Lancet 1, 769–770 10.1016/S0140-6736(88)91580-2 [DOI] [PubMed] [Google Scholar]
- Parker S., Nuara A., Buller R. M., Schultz D. A. (2007). Human monkeypox: an emerging zoonotic disease. Future Microbiol 2, 17–34 10.2217/17460913.2.1.17 [DOI] [PubMed] [Google Scholar]
- Reynolds M. G., Yorita K. L., Kuehnert M. J., Davidson W. B., Huhn G. D., Holman R. C., Damon I. K. (2006). Clinical manifestations of human monkeypox influenced by route of infection. J Infect Dis 194, 773–780 10.1086/505880 [DOI] [PubMed] [Google Scholar]
- Rimoin A. W., Mulembakani P. M., Johnston S. C., Lloyd Smith J. O., Kisalu N. K., Kinkela T. L., Blumberg S., Thomassen H. A., Pike B. L. & other authors (2010). Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo. Proc Natl Acad Sci U S A 107, 16262–16267 10.1073/pnas.1005769107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seet B. T., Johnston J. B., Brunetti C. R., Barrett J. W., Everett H., Cameron C., Sypula J., Nazarian S. H., Lucas A., McFadden G. (2003). Poxviruses and immune evasion. Annu Rev Immunol 21, 377–423 10.1146/annurev.immunol.21.120601.141049 [DOI] [PubMed] [Google Scholar]
- Stittelaar K. J., Kuiken T., de Swart R. L., van Amerongen G., Vos H. W., Niesters H. G., van Schalkwijk P., van der Kwast T., Wyatt L. S. & other authors (2001). Safety of modified vaccinia virus Ankara (MVA) in immune-suppressed macaques. Vaccine 19, 3700–3709 10.1016/S0264-410X(01)00075-5 [DOI] [PubMed] [Google Scholar]
- Tucker J. B. (2011). Breaking the deadlock over destruction of the smallpox virus stocks. Biosecur Bioterror 9, 55–67 10.1089/bsp.2010.0065 [DOI] [PubMed] [Google Scholar]
- Vorou R. M., Papavassiliou V. G., Pierroutsakos I. N. (2008). Cowpox virus infection: an emerging health threat. Curr Opin Infect Dis 21, 153–156 10.1097/QCO.0b013e3282f44c74 [DOI] [PubMed] [Google Scholar]
- Xing K., Deng R., Wang J., Feng J., Huang M., Wang X. (2006). Genome-based phylogeny of poxvirus. Intervirology 49, 207–214 10.1159/000090790 [DOI] [PubMed] [Google Scholar]
- Zaucha G. M., Jahrling P. B., Geisbert T. W., Swearengen J. R., Hensley L. (2001). The pathology of experimental aerosolized monkeypox virus infection in cynomolgus monkeys (Macaca fascicularis). Lab Invest 81, 1581–1600 [DOI] [PMC free article] [PubMed] [Google Scholar]