Abstract
Objective:
The objective of this study was to describe a reliable ultrasound based index scoring system based on ultraound characteristics to identify benign thyroid nodules and avoid unnecessary fine needle aspiration cytology.
Materials and Methods:
Patients undergoing ultrasound-guided fine-needle aspiration cytology (FNAC) for thyroid nodules were evaluated prospectively. A total of 284 patients were evaluated from November 2005 to November 2011. There were 284 nodules. Any solid or partly solid focal nodule in the thyroid gland was included in the study. Cysts with no solid component were excluded. We used LOGIQ 9 (GE Healthcare) scanner equipped with a 10--14 MHz linear matrix transducer with color and power Doppler capability. Four US characteristics were evaluated, i.e., nodule margins, echo texture, vascularity, and calcification. Fine needle aspiration (FNA) was performed on all nodules. The nodules were labeled benign or suspicious using an ultrasound index score and the results compared with FNAC. Follicular neoplasms on fine-needle aspiration cytology were further assessed by excision biopsy and histology. Cytology/histology was used as the final diagnosis.
Results:
In total 284 nodules were analyzed. All the 234 nodules in US labeled benign category were proven to be benign on cytology/histology. Therefore the specificity of ultrasound in labeling a nodule benign was 100%. Twenty of the 50 nodules that were suspicious on US were malignant. The most significant US differentiating characteristics were nodule margins, vascularity, and microcalcification.
Conclusion:
Our results show that US can accurately characterize benign thyroid nodules using an index scoring system and therefore preclude FNAC in these patients.
Keywords: Fine needle aspiration cytology, thyroid, ultrasound, benign thyroid nodule
INTRODUCTION

Thyroid nodules in the adult population are common.[1] Although the majority of thyroid nodules are benign, a large number undergo cytology/histology to rule out malignancy.[2] Initially thyroid nodule characteristics were studied individually and their association with malignancy has been reported.[3,4] Subsequently, characteristics were grouped to determine if by having more than one characteristic this association changed.[3,5] Currently most authors divide thyroid nodules into benign, follicular lesions, and malignant nodules based on ultrasound (US)appearance.[6] Recently Horvath et al., created a Thyroid Imaging Reporting and Data System (TIRADS) after evaluating the different characteristics that allow for a better selection of nodules submitted for fine-needle aspiration cytology (FNAC); while Park et al., proposed an equation to predict the probability of malignancy in thyroid nodules based on 12 characteristics.[4,6]
FNAC remains the gold standard in the characterization of thyroid nodules.[7,8] However, different US criteria are now being used to predict the nature of thyroid nodules.[7,8,9–22] This is because performing FNAC of all thyroid nodules is a costly venture with a low yield in identifying the small proportion of nodules that actually represent malignant disease.[15]
There is no universal agreement about the best way to use US in the management of thyroid nodules.[4,6,23,24] This paper evaluated the use of easily adaptable index score based on US characteristics that have a higher correlation with benign nature of a thyroid nodule.
OBJECTIVE
The objective of this study was to describe a reliable ultrasound based index scoring system based on ultraound characteristics to identify benign thyroid nodules and avoid unnecessary fine needle aspiration cytology.
MATERIALS AND METHODS
The study received approval by the Research and Ethics committee of the Aga Khan University Hospital, Nairobi. From November 2005 we started to recruit patients referred for US-guided FNAC of thyroid nodules at the Radiology Department in Aga Khan University Hospital, Nairobi. Written informed consent was acquired from all subjects. All patients underwent ultrasound examination of the thyroid which was performed by one of two radiologists each with greater than 5 years experience in thyroid ultrasound. We used a LOGIQ 9 (GE Healthcare) scanner equipped with a 10--14 MHz linear matrix transducer with color and power Doppler capability.
All solid or partly solid focal nodules in the thyroid gland were included in the study. When a patient had multiple nodules, the most dominant nodule/s were included. This decision to choose the dominant nodule was left to the discretion of the person performing the ultrasound examination. Cysts with no solid component were excluded because they are almost exclusively always benign.[1]
We evaluated four characteristics of each nodule, i.e., border characteristics (margins), echo texture, presence or absence of microcalcification, and vascularity.
Margins
The margin of a thyroid nodule was classified as either regular or irregular. Distinct nodule borders exhibiting a complete halo were called regular whereas indistinct, poorly defined borders with less than 30% circumferential demarcation were defined as irregular [Figures 1 and 2].
Figure 1.
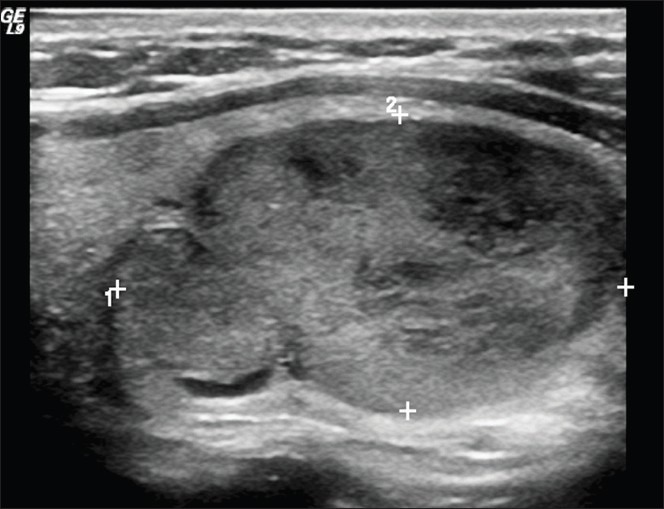
Gray scale image of a benign nodule in a patient with thyrotoxicosis (within calipers). This nodule has a regular margin (0) and is heterogeneous (1) with no calcification (0). Color Doppler revealed normal blood flow. Index score is 1. Final diagnosis was colloid goiter.
Figure 2.
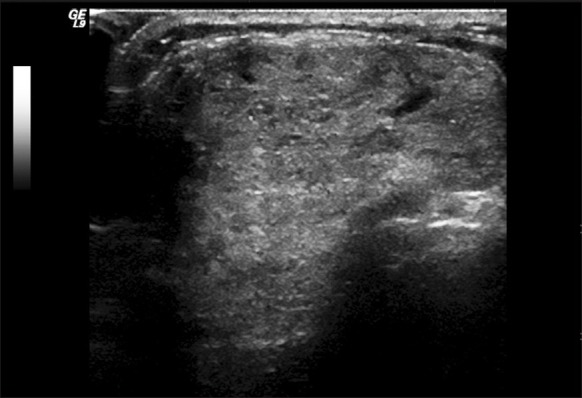
Illustrates a thyroid nodule with an irregular margin.
Echogenicity
This was described as either homogenous or heterogeneous based on comparison to the surrounding thyroid tissue [Figures 1, 3 and 4].
Figure 3.
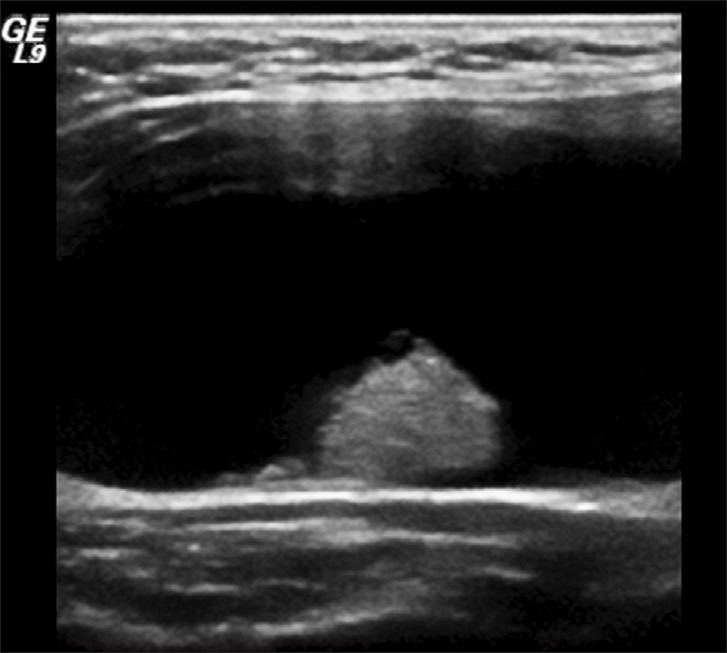
Illustrates cystic lesion with mural nodule. The mural nodule has a homogenous echotexture.
Figure 4.
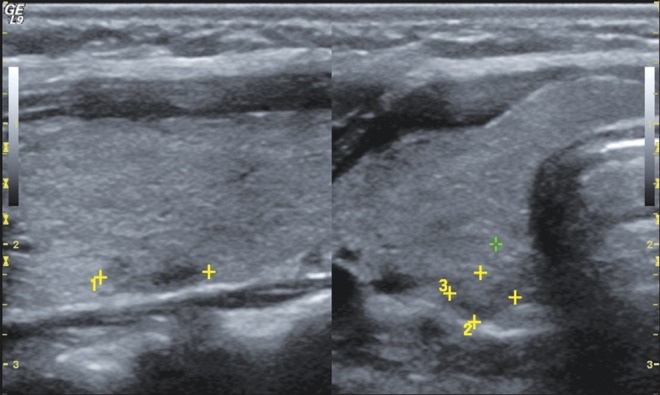
Illustrates a thyroid nodule in longitudinal and transverse planes within calipers that has a homogeneous echogenicity is also isoechoic to the surrounding thyroid gland parenchyma.
Vascularity
This was assessed by color Doppler and vascularity was compared with the surrounding thyroid gland. It was classified as centrally increased, peripherally increased or normal [Figures 5 and 6].
Figure 5.
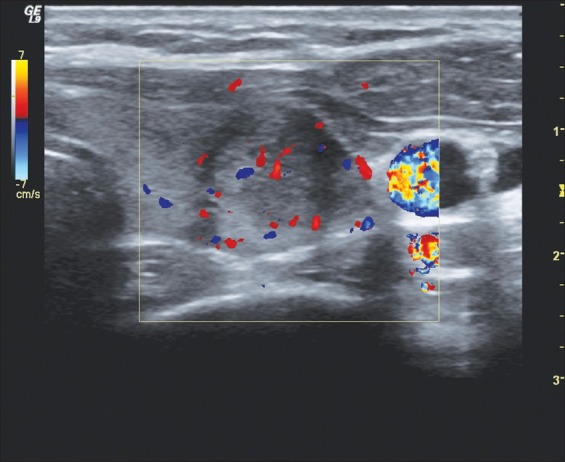
Illustrates a thyroid nodule with central increased blood flow.
Figure 6.
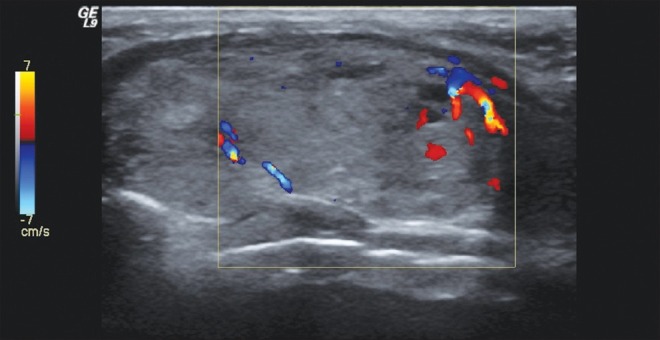
Illustrates a thyroid nodule with peripheral increased blood flow.
The presence of calcification was classified as macrocalcifications/microcalcifications/none. If a nodule had both microcalcification and macrocalcification it was classified under microcalcification [Figures 7 and 8].
Figure 7.
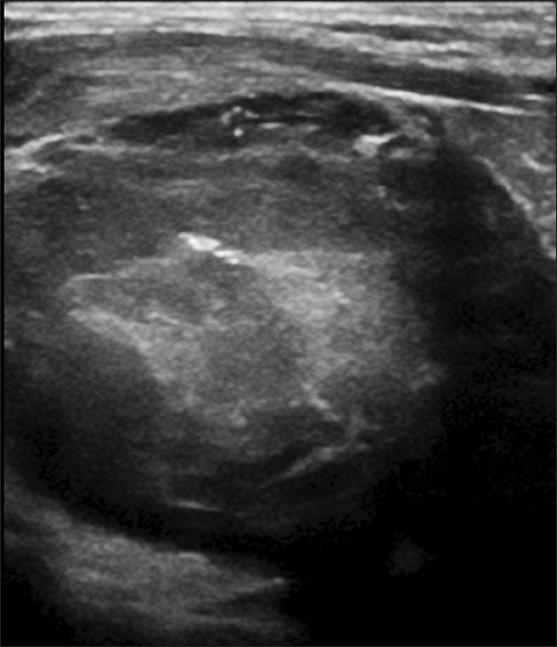
Illustrates a thyroid nodule with macrocalcifications.
Figure 8.
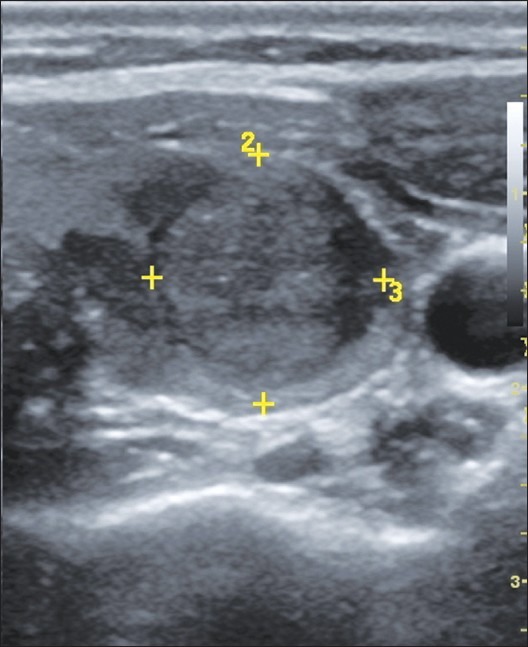
Illustrates a thyroid nodule (within calipers) with microcalcifications.
We then graded the nodules by giving them an index score of one to four using the four major US characteristics in Table 1.
Table 1.
US index scoring
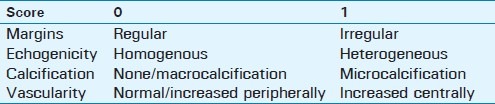
Each nodule had a minimum score of 0 and a maximum of 4. Those with scores of 0 and 1 were labeled as benign [Figure 1]. Scores of 2, 3, or 4 were labeled “suspicious” [Figure 9a and b]. In the interpretation of the US features both radiologists arrived at a consensus diagnosis, i.e., benign or suspicious.
Figure 9.

Illustrates a suspicious thyroid nodule. (a) Gray scale image of a malignant nodule with heterogeneous echogenicity and microcalcifications. (b) Color Doppler image of the same nodule demonstrates increased central blood flow. This nodule has a regular margin (0), is heterogeneous (1) with microcalcification (1), and has increased central blood flow (1). Index score is 3. Final diagnosis was papillary carcinoma.
US-guided FNAC procedure
Superficial nodules: Multiple passes were made using a 25 gauge needle (without any suction).
Deeper nodules: Multiple passes through the nodule with a 21/23 gauge needle and suction with a syringe.
A cytologist then analyzed them at the same sitting to reduce the number of inadequate samples. Two pathologists in consensus classified the cytological diagnosis as benign, malignant or follicular nodule.
Some authors have used a vacuum gun to aid suction of small nodules that are located deep within the thyroid gland.[17] The nature of a follicular nodule cannot be determined by FNAC; hence histology is imperative for a final diagnosis to be arrived at.[26,27] In our study all follicular nodules underwent an incisional or excisional biopsy for histological diagnosis.
Specificity of US in the characterization of benign thyroid nodules using the major characteristics was then calculated. All the nodules included were analyzed and the gold standard was cytology or histology. All characteristics were tabulated to calculate their level of association with malignancy by determining the percentage of each in the benign and suspicious categories respectively. A P-value was assigned to each to determine the level of significance. A value less than 0.5 was considered significant.
RESULTS
A total of 284 nodules were analyzed. The patient selection was from a pool of consecutive referrals to Aga Khan University Hospital's radiology department in Nairobi. The nodule size ranged from 3 mm to 28 mm (anteroposterior), 10 mm to 20 mm (transverse), and 3 mm to 12 mm (length).
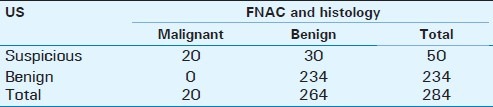
A total of 234 nodules were characterized as benign on US, all of which were benign on FNAC. Therefore the specificity of US labeling a nodule benign was 100%. There were 50 suspicious nodules on US of which 20 turned out to be malignant [Table 2].
Table 2.
US and FNAC Correlation
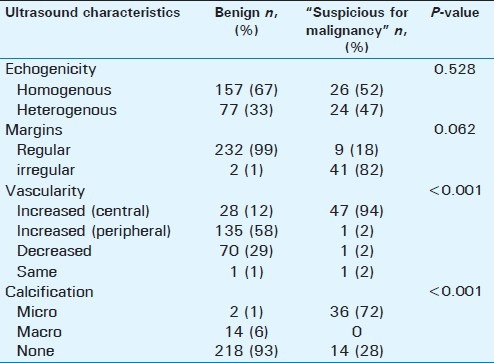
Of the ultrasound characteristics analyzed margins, vascularity, and calcification were found to have significant P-values [Table 3]. Echogenicity was not significant in identifying benign or malignant nature of the nodule.
Table 3.
Statistical measure of US features used in the study
DISCUSSION
The widespread use of US in the evaluation of thyroid nodules has created an overwhelming need to establish scientifically sound, straight-forward, and easily adaptable protocols that minimize costs related to nodule management and maximize the benefits of US. Our aim was to suggest an US index score that has the characteristics of such a protocol. We assessed the reliability of our US criteria in labeling a thyroid nodule as benign. Ninety-three percent of the thyroid nodules referred for US-guided FNAC were benign and 7% were malignant. A similar incidence has been published by Lannuccilli et al.[15] All of the 234 nodules that were characterized as benign on US (0-1 category) were confirmed to be benign on cytology/histology. Based on these findings, if US classifies a nodule as benign FNAC can be deferred. This is reiterated by studies such as Stacul and Kwak et al., which have shown that most malignant nodules have more than two malignant US characteristics.[28,29]
Several US characteristics have been studied previously. These include border characteristics (margins), echogenicity, calcifications, vascularity, size, shape, orientation, and acoustic transmission. We only evaluated four of these characteristics in each nodule, i.e., border characteristics (margins), echogenicity, presence or absence of microcalcification, and vascularity. These features were selected because they have been shown to be the most widely looked for, as they have the highest correlation with malignancy when studied in combination.[3,4,5,6,23] They are also similar to those used in a study by Kovacevic et al.[18] In two studies on the same patient population, Koike et al., demonstrated how combining highly sensitive US characteristics of malignancy with more specific FNA cytology can yield a accuracy similar to that using a set of more specific US characteristics to diagnose malignancy.[1,25] We did not assess size and shape in order to determine to what extent they may be linked to the benign nature of a thyroid nodule. Size and shape of the nodule have been shown to be less sensitive and specific indicators of thyroid malignancy.[5] We did not assess nodule orientation or acoustic transmission because they have not been used as frequently as the characteristics we chose to analyze. Other sonographic variables not measured in the study that could have incremental predictive value, include ultrasound-directed qualitative intranodular vascular distribution and quantitative analysis of tumor vascularity (tumor vascular resistive index).[8] These are complex and not easily adaptable in routine US imaging of the thyroid gland.
We have described a method in which one can use US to predict benignity. Table 4 summarizes already published operating characteristics of described methods for using US features of thyroid nodules as predictors of malignancy.
Table 4.
Summary of previously published studies for predicting thyroid nodule malignancy
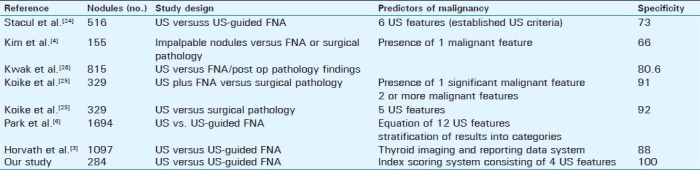
With an index scoring system using the US features it has been shown to have the highest association with malignancy. Based on our scoring system we had a very high specificity to diagnose a benign nodule [Table 4]. Our high pick up rate of benign nodules may be partly due to the specific characteristics we used, but we must acknowledge the high prevalence of benign nodules regardless of the effectiveness of our index score. Our specificity is high compared with Kwak, Stacul, Koike etal., and more recently Horvath et al., [Table 4]. This may be because we were targeting benign nodules. Kim et al., had the lowest specificity which may be because they adapted the older method of using just one US feature to assess malignancy, rather than using a combination of US features [Table 4].
We used an index score consisting of four out of several characteristics that have been shown to be features significantly associated with malignancy.[33] While the most recent publications have moved on to stratify, categorize, and create reporting and data systems,[1,3] we chose to take a simpler and more adaptable yet scientifically sound approach similar to Koike et al.[25]
Of the four major US characteristics that were used, margins, calcification, and vascularity were most significant. A small percentage of benign nodules had an irregular margin but they did not have increased central blood flow and no calcification was seen. These findings are reiterated by Moon and Seya et al.[21,31] If a nodule was classified as malignant it most likely had an irregular margin and increased central vascularity. Echo texture and ancillary characteristics such as size and shape did not have significant P-values. This may be because of the sample size and a larger study for further evaluation of these characteristics would be of value because these features may be used as an additional features to evaluate malignancy. Most patients with malignancies have more than two US features characteristic of malignancy.[1,14,15,31] However certain characteristics are more reliable as shown in Table 2. Presence of microcalcification is most significant in predicting malignancy[1]
The use of US adds the additional advantage of FNA guidance which is particularly beneficial in patients with nonpalpable, multiple, or heterogeneous nodules for preferentially aspirating a specific segment of the nodule (large or partially cystic nodule) or when nodule palpation is difficult (patients with diffuse glandular disease) or obesity.[30]
In the diagnostic management of thyroid nodules, FNAC is still the gold standard despite the growing experience in the use of high resolution US.[8,12,31] FNAC has its limitations. It cannot differentiate a follicular adenoma from a follicular carcinoma.[2,18] Therefore, for these lesions a corresponding histological analysis was taken to be the final diagnosis. FNAC can also be limited by inadequate sampling.[18] In our paper, an attempt to reduce inadequate sampling was made by using US guidance and by having the samples analyzed by a pathologist at the same sitting before the patient left the examination room.[30] The actual effectiveness of different US criteria is still in question and currently being reconsidered and modified.[33] Techniques that combine US features and FNAC are most effective and most accurate for predicting malignancy rather than US alone.[22] Many studies agree that with regard to thyroid nodule management a multidisciplinary approach is best, including clinical examination, laboratory work up, US, FNAC, and surgical excision with biopsy where necessary. A consensus conference statement by the Society of Radiologists in US highlighted six US characteristics that are associated with malignancy.[33], the most specific of which were analyzed in this paper
The authors recognize various limitations of the study. US is a highly operator-dependent examination. As such operator bias could have played a role in the US results. In the interpretation of thyroid nodules, the presence or absence of abnormal neck lymph nodes was not considered. Elastography is a technique that can also help identify thyroid nodules that are likely to be malignant.[32] We did not analyze elastography but focused on an index score that can reliably identify benign nodules. A combination of US features with other investigations such as, serum thyroid stimulating hormone concentration, galectin-3 expression analysis, and FDG/PET scan would be useful in avoiding the higher costs of thyroid surgical procedures.[28] One of the most significant weaknesses of this paper is the small sample size with few malignant nodules compared with recent publications with almost similar objectives but more complex sonographic pattern recognition methods. However we do believe that this is outweighed by the fact that the simple and straight-forward index score used to classify nodules did not need a larger sample size as have recent papers like Horvath et al.[3] In 2002 and later 2007 a paper by Kim and Kovacevic et al. respectively, had even smaller sample sizes and simple classification systems.[4,26]
Finally the purpose of this paper is unique to what has already been done; the structure is sound, methodology is straight-forward (justifying the small sample size), and its findings can be applied during routine imaging without significant cost implications.
CONCLUSION
Our preliminary results show that US characterization of a thyroid nodule can accurately infer its benign nature. We have suggested the use of an US index score to avoid unnecessary FNAC in patients with thyroid nodules. However as FNAC remains the gold standard in the characterization of a thyroid nodule, both FNAC and US should be used in combination to manage suspicious thyroid nodules. This preliminary work can be used as a guide to the evolving management protocol of thyroid nodules.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/23/95446
REFERENCES
- 1.Morris L, Ragavendra N, Yeh MW. Evidence-based assessment of the role of ultrasonography in the management of benign thyroid nodules. World J Surg. 2008;32:1253–63. doi: 10.1007/s00268-008-9494-z. [DOI] [PubMed] [Google Scholar]
- 2.Monteros Alvi M, Romero NM, Gonorazky S, Galvez V, Galvez M, Virgili E, De Soler GG. Risk markers of follicular neoplasms in thyroid nodules. Medicina. 2009;5:497–501. [PubMed] [Google Scholar]
- 3.Kim EK, Chung WY, Oh KK, Kim DI, Lee JT, Yoo HS. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002;17:687–91. doi: 10.2214/ajr.178.3.1780687. [DOI] [PubMed] [Google Scholar]
- 4.Hoang JK, Lee WK, Lee M, Johnson D, Farrell S. US Features of thyroid malignancy: Pearls and pitfalls. Radiographics. 2007;27:847–60. doi: 10.1148/rg.273065038. discussion 861-5. [DOI] [PubMed] [Google Scholar]
- 5.Park JY, Lee HJ, Jang HW, Kim HK, Yi JH, Lee W. A proposal for a thyroid imaging reporting and data system for ultrasound features of thyroid carcinoma. Thyroid. 2009;19:1257–64. doi: 10.1089/thy.2008.0021. [DOI] [PubMed] [Google Scholar]
- 6.Park JY, Lee HJ, Jang HW, Kim HK, Yi JH, Lee W, et al. An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J Clin Endocrinol Metab. 2009;94:1748–51. doi: 10.1210/jc.2008-1724. [DOI] [PubMed] [Google Scholar]
- 7.Wienke JR, Chong WK, Fielding JR, Zou KH, Mittelstaedt CA. Sonographic features of benign thyroid nodules.Interobserver reliability and overlap with malignancy American Institute of Ultrasound in Medicine. J Ultrasound Med. 2003;22:1027–31. doi: 10.7863/jum.2003.22.10.1027. [DOI] [PubMed] [Google Scholar]
- 8.Stojadinovic A, Peoples GE, Libutti SK, Henry LR, Eberhardt J, Howard RS. Development of a clinical decision model for thyroid nodules. BMC Surg. 2009;9:12. doi: 10.1186/1471-2482-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoang JK, Lee WK, Lee M, Johnson D, Farrell S. US Features of Thyroid Malignancy: Pearls and Pitfalls. RadioGraphics. 2007;27:847–65. doi: 10.1148/rg.273065038. [DOI] [PubMed] [Google Scholar]
- 10.Bonavita JA, Mayo J, Babb J, Bennett G, Oweity T, Macari M, et al. Pattern recognition of benign nodules at ultrasound of the thyroid: Which nodules can be left alone? Am J Roentgenol. 2009;1:207–13. doi: 10.2214/AJR.08.1820. [DOI] [PubMed] [Google Scholar]
- 11.Camargo RY, Tomimori EK, Knobel M, Medeiros-Neto G. Preoperative assessment of thyroid nodules: Role of ultrasonography and fine needle aspiration biopsy followed by cytology. Clinics. 2007;6:411–8. doi: 10.1590/s1807-59322007000400007. [DOI] [PubMed] [Google Scholar]
- 12.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer.Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 13.Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. Am J Roentgenol. 2002;178:687–91. doi: 10.2214/ajr.178.3.1780687. [DOI] [PubMed] [Google Scholar]
- 14.Hoang JK, Lee WK, Lee M, Johnson D, Farrell S. US Features of Thyroid Malignancy: Pearls and Pitfalls. RadioGraphics. 2007;27:847–65. doi: 10.1148/rg.273065038. [DOI] [PubMed] [Google Scholar]
- 15.Iannuccilli JD, Cronan JJ, Monchik JM. Risk for malignancy of thyroid nodules as assessed by sonographic criteria. The need for biopsy. American Institute of Ultrasound in Medicine. J Ultrasound Med. 2004;23:1455–64. doi: 10.7863/jum.2004.23.11.1455. [DOI] [PubMed] [Google Scholar]
- 16.Ito Y, Amino N, Yokozawa T, Ota H, Ohshita M, Murata N. Ultrasonographic evaluation of thyroid nodules in 900 patients: Comparison among ultrasonographic, cytological, and histological findings. Thyroid. 2007;17:1269–76. doi: 10.1089/thy.2007.0014. [DOI] [PubMed] [Google Scholar]
- 17.Kim MJ, Kim EK, Park SI, Kim BM, Kwak JY, Kim SJ. US-guided fine-needle aspiration of thyroid nodules: Indications, techniques, results. Radiographics. 2008;7:1869–86. doi: 10.1148/rg.287085033. [DOI] [PubMed] [Google Scholar]
- 18.Kovacevic O, Skurla MS. Hoboken, New Jersey: Wiley Periodicals, Inc; 2007. Sonographic Diagnosis of Thyroid Nodules: Correlation with the Results of Sonographically Guided Fine-Needle Aspiration Biopsy; pp. 63–7. [DOI] [PubMed] [Google Scholar]
- 19.Yassa L, Cibas ES, Benson CB, Frates MC, Doubilet PM, Gawande AA. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer Cytopathol. 2007;111:508–16. doi: 10.1002/cncr.23116. [DOI] [PubMed] [Google Scholar]
- 20.Lew JI, Rodgers SE, Solorzano CC. Developments in the use of ultrasound for thyroid cancer. Curr Opin Oncol. 2010;22:11–6. doi: 10.1097/CCO.0b013e3283337f16. [DOI] [PubMed] [Google Scholar]
- 21.Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008;247:762–70. doi: 10.1148/radiol.2473070944. [DOI] [PubMed] [Google Scholar]
- 22.Morris LF, Ragavendra N, Yeh MW. Evidence-based assessment of the role of ultrasonography in the management of benign thyroid nodules. World J Surg. 2008;32:1253–63. doi: 10.1007/s00268-008-9494-z. [DOI] [PubMed] [Google Scholar]
- 23.Kim MJ, Kim EK, Park SI, Kim BM, Kwak JY, Kim SJ. US-guided fine-needle aspiration of thyroid nodules: Indications, techniques, results. Radiographics. 2008;28:1869–86. doi: 10.1148/rg.287085033. [DOI] [PubMed] [Google Scholar]
- 24.Stacul F, Bertolotto M, De Gobbis F, Calderan L, Cioffi V, Romano A. US, colour-Doppler US and fine-needle aspiration biopsy in the diagnosis of thyroid nodule. Radiol Med. 2007;112:751–62. doi: 10.1007/s11547-007-0178-9. [DOI] [PubMed] [Google Scholar]
- 25.Koike E, Yamashita H, Noguchi S, Murakami T, Ohshima A, Maruta J. Effect of combining ultrasonography and US-guided fine-needle aspiration biopsy findings for the diagnosis of thyroid nodules. Eur J Surg. 2001;167:656–61. doi: 10.1080/11024150152619273. [DOI] [PubMed] [Google Scholar]
- 26.Kovacevic DO, Skurla MS. Sonographic diagnosis of thyroid nodules: Correlation with the results of sonographically guided fine-needle aspiration biopsy. J Clin Ultrasound. 2007;35:63–7. doi: 10.1002/jcu.20287. [DOI] [PubMed] [Google Scholar]
- 27.Monteros Alvi M, Romero NM, Gonorazky S, Galvez V, Galvez M, Virgili E. Risk markers of follicular neoplasms in thyroid nodules. Medicina (B Aires) 2009;69:497–501. [PubMed] [Google Scholar]
- 28.Stacul F, Bertolotto M, De Gobbis F, Calderan L, Cioffi V, Romano A. US, colour-Doppler US and fine-needle aspiration biopsy in the diagnosis of thyroid nodules. Radiol Med. 2007;112:751–62. doi: 10.1007/s11547-007-0178-9. [DOI] [PubMed] [Google Scholar]
- 29.Kwak JY, Kim EK, Kim MJ, Son EJ. Significance of sonographic characterization for managing subcentimeter thyroid nodules. Acta Radiol. 2009;27:1–7. doi: 10.1080/02841850903062724. [DOI] [PubMed] [Google Scholar]
- 30.Morris LF, Ragavendra N, Yeh MW. Evidence-based assessment of the role of ultrasonography in the management of benign thyroid nodules. World J Surg. 2008;32:1253–63. doi: 10.1007/s00268-008-9494-z. [DOI] [PubMed] [Google Scholar]
- 31.Seya A, Oeda T, Terano T, Omura M, Tahara K, Nishikawa T. Comparative studies on fine-needle aspiration cytology with ultrasound scanning in the assessment. Jpn J Med. 1990;29:478–80. doi: 10.2169/internalmedicine1962.29.478. [DOI] [PubMed] [Google Scholar]
- 32.Asteria C, Giovanardi A, Pizzocaro A, Cozzaglio L, Morabito A, Somalvico F. US-elastography in the differential diagnosis of benign and malignant thyroid nodules. Thyroid. 2008;8:523–31. doi: 10.1089/thy.2007.0323. [DOI] [PubMed] [Google Scholar]
- 33.Frates MC, Benson CB, Charboneau JW. Management of thyroid nodules detected at US.Society of Radiologists in US consensus conference statement. Radiology. 2005;237:794–800. doi: 10.1148/radiol.2373050220. [DOI] [PubMed] [Google Scholar]


