Abstract
Background:
Lepra reactions are not always diagnosable under the microscope. We analyzed skin histopathology in 64 cases of lepra reaction.
Aim:
To make detailed observations on histopathologic features of type 1 and type 2 lepra reaction (erythema nodosum leprosum, ENL).
Materials and Methods:
In this retrospective study, we included 64 patients diagnosed during a 3-year period as lepra reaction based on clinico-pathological co-relation.
Results:
Out of the 64 patients, 22 were of type 1 reaction and 42 of ENL. The most consistent finding in type 1 reaction was papillary dermal edema (86%) followed by pyknosis of lymphocytes (77%) and intercellular edema within granuloma (73%). Surprisingly, folliculotropism of lymphocytes was seen in 55% and subcutaneous infiltration in 36%. In ENL, the most common finding was presence of neutrophils within the granuloma (100%), followed by leukocytoclasia (81%), papillary dermal edema (81%), and neutrophilic panniculitis (69%). Fibrin in the vessel wall or/and granulomas was noted in only 38% while fibrin thrombi in the vessel walls were seen in only 12% of cases.
Conclusion:
Infiltration of macrophage granulomas by neutrophils is a reliable sign of ENL. Classical signs of vasculitis are not always present in ENL. Folliculotropism and lymphocytic panniculitis were frequent in type 1 reactions while neutrophilic panniculitis was common with ENL.
Keywords: Erythema nodosum leprosum, lepra reaction, vasculitis
Introduction
Reactions in leprosy are acute inflammatory episodes occurring in an otherwise chronic course of the infection. Histopathology of type 1 lepra reaction shows edema within granuloma separating inflammatory cells with density of lymphocytes in the dermis. To distinguish between upgrading and downgrading reaction histopathologicaly, serial examination of biopsies is required.[1] Histopathology of skin lesions of Type 2 lepra reaction (erythema nodosum leprosum, ENL) shows dermal edema, neutrophilic infiltration and vasculitis on a background of macrophage granuloma.[2]
Wide variations in clinical presentation of leprosy in reaction, make histopathology an important tool for supporting clinical diagnosis. While leprosy is histopathologicaly relatively easy to diagnose, lepra reactions are not always diagnosable under the microscope. Although our study included clinical features, we decided to focus on histopathologic features and their clinicopathologic co-relation.
Materials and Methods
A retrospective clinicopathological analysis of 64 skin biopsies of patients with lepra reaction visiting a tertiary care centre during year 2005–2008 was done. We included skin biopsy specimens of patients of all ages, diagnosed as lepra reaction (type 1 and type 2) after clinico-pathological correlation. Those with doubtful diagnosis were clinically reviewed and if needed, excluded from the study. Histopathological reevaluation of the skin biopsies stained with hematoxylin and eosin stain was done and findings were recorded. AFB staining was not done routinely, as it was not useful for diagnosis of lepra reactions. Clinical review was not possible for 4 patients (1 of type 1 reaction and 3 of type 2 reaction) for logistic reasons.
Results
The age of the patients included in study ranged from 6 years to 68 years (mean age 35.55 years) for type 1 reaction, while it was 11 to 65 years (mean age 40.10 years) for type 2 reaction. Amongst 64 patients, 42 were males and 22 were females.
The leprosy spectrum (based on clinicopathologic co-relation) and type of reaction observed in our patients is mentioned in Table 1, while Table 2 details their clinical features.
Table 1.
Type of lepra reaction and clinical spectrum of Hansen's disease
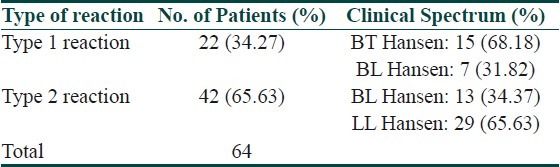
Table 2.
Clinical profile of patients
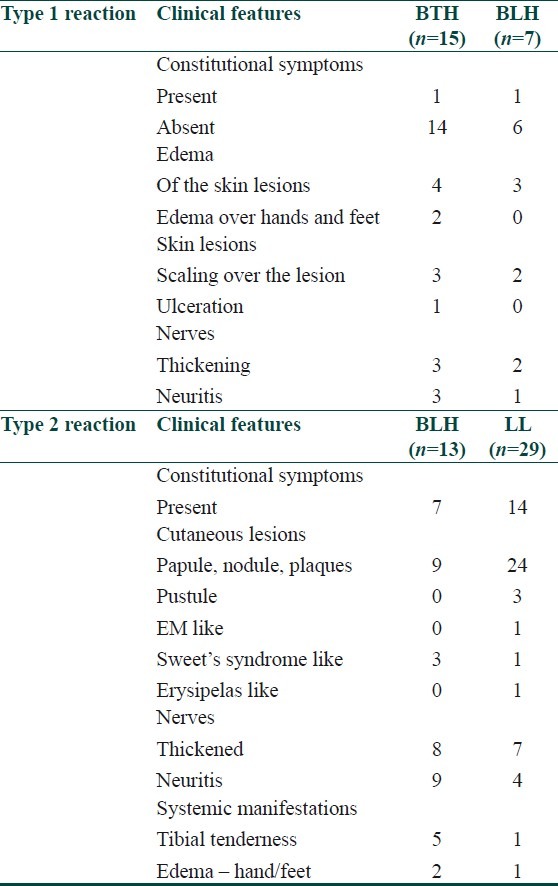
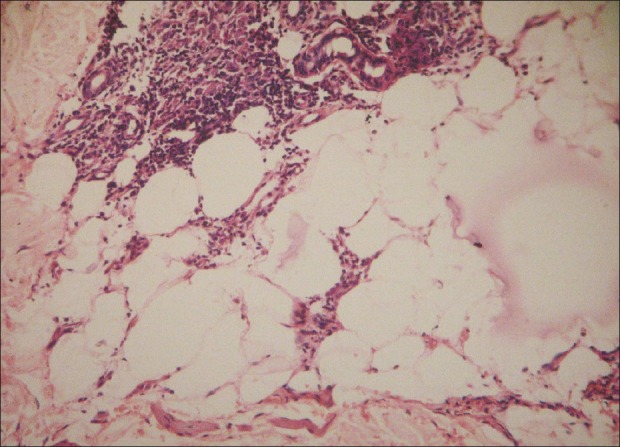
Histopathological observations in type 1 reaction are illustrated in Table 3. The most consistent finding in type 1 reaction was higher than expected accumulation of lymphocytes within granuloma which was seen in all specimens, followed by occurrence of edema in papillary dermis, pyknosis of lymphocytes, and edema in the granuloma followed by folliculotropism [Figure 1] and lymphocytic panniculitis [Figure 2].
Table 3.
Histopathological observations in type 1 reaction
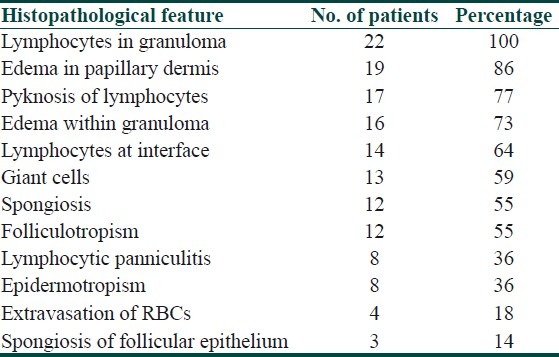
Figure 1.
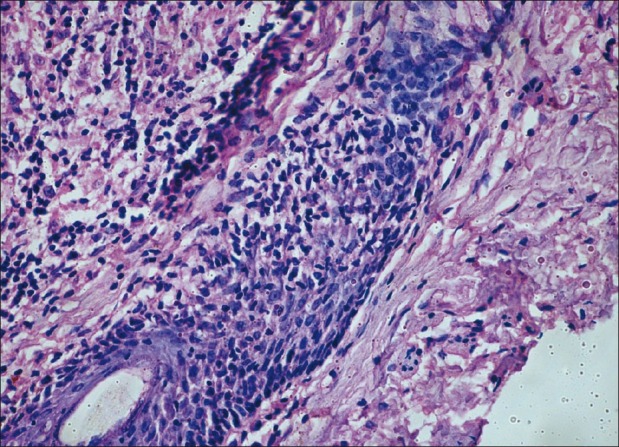
Lymphocytic infiltratation of follicle (folliculotropism)
Figure 2.
Lymphocytic panniculitis
Histopathological observations in type 2 reaction have been depicted in Table 4. We observed that, the presence of neutrophils in the granuloma was a uniform feature seen in all lesions of ENL [Figure 3]. Other common findings were leukocytoclasia and papillary dermal edema (81% each) and lobular [Figure 4] and septal neutrophilic panniculitis (66%).
Table 4.
Histopathological observations in type 2 reaction
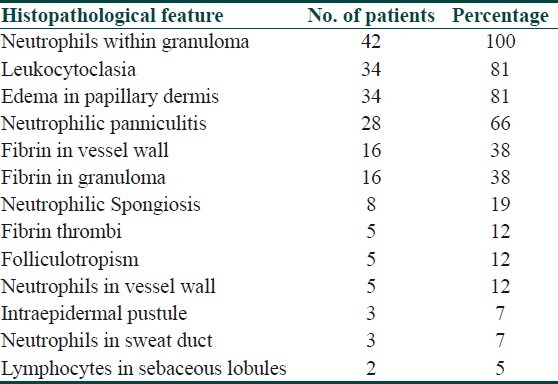
Figure 3.
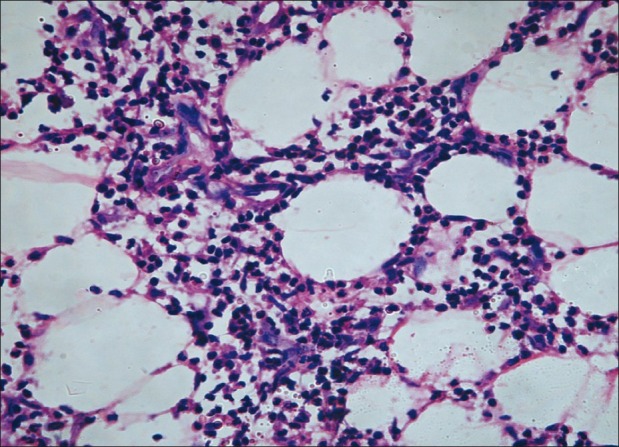
Neutrophils in panniculus
Figure 4.
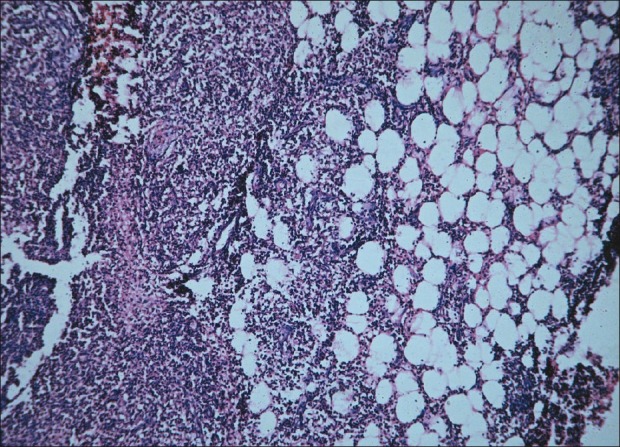
Lobular panniculitis
Discussion
Prior studies on histopathologic features of lepra reactions are prospective clinicopathological evaluations.[3] Due to the sheer amount of data such a study must process, most do not describe details of histopathologic findings. e.g., vasculitis is mentioned as a finding but individual histopathologic features of vasculitis like fibrin in vessel wall or fibrin thrombi or leukocytoclasia are not described.
Dermal edema, loosening of granuloma, and predominance or increase in number of lymphocytes are described as a feature of type 1 reaction in prior studies.[3] We observed some additional features [Table 3].
Interpretation of pyknosis of lymphocytes can be difficult at times as it can be influenced by inter-observer variations. Lymphocytes are seen in granuloma of leprosy though the lesion is not in reaction. We observed that, lymphocytes in granuloma associated with dermal edema and/or edema within the granuloma is highly suggestive type 1 reaction.
Epidermotropism is infiltration of epidermis by lymphocytes without much spongiosis. Epidermotropism has classically been described with mycosis fungoides but here we observed it in few lesions of type 1 lepra reaction. The exact significance of epidermotropism in type 1 reaction is not known.
Lazaro-Medina et al. have described some new markers for type 1 reaction which include spongiosis of the epidermal and follicular epithelium with exocytosis of mononuclear cells, parakeratosis, focal interface changes with occasional individual cell necrosis of keratinocytes, and follicular mucinosis.[4] Some of these findings like epidermal and follicular epithelium spongiosis, interface change were also observed by us.
Occurrence of giant cells in the granuloma is one of the finding which helps in classifying histopathologically the features of upgrading and downgrading type1 lepra reactions. Lockwood DN and co-workers in a prospective study compared skin lesions with type 1 reaction with non-reactional controls; in addition to intra dermal and intra granuloma edema they noted increase in giant cell size and giant cell numbers in type 1 reaction.[5] As in our study such comparison with non-reactional control was not done, we are unable to make any comments on the findings they described.
Neutrophils are not seen in ordinary lesions of leprosy. In type 2 lepra reactions, because of the immune complex deposition, neutrophils are attracted in these lesions. Neutrophils were present either within the granulomatous infiltrate or/and in the interstitium with or without leukocytoclasia. In a few sections, they were also seen encroaching the epidermis and the sweat ducts. The density of neutrophilic infiltrate was variable. More severe and recent onset lesions of lepra reactions showed much denser infiltrate as compared less severe and subsiding lesions. We noted neutrophilic spongiosis as more common than intraepidermal pustule formation. The dense collection of neutrophils in the epidermis and dermis is probably responsible for the clinical finding of pustules in ENL lesions.
Infiltration of sweat duct and sweat gland by neutrophils was found in a few cases without any evidence of damage or necrosis of the sweat duct or sweat glands.
The histopathologic spectrum of vasculitis range from endothelial swelling, neutrophilic infiltration of the vessel wall with destruction of the walls and leucocytoclasia.[6] Fibrin deposition in vessel wall and thrombus formation in lumen also occurs.
A variable degree of vascular involvement in type 2 reaction was noted in our study and majority of the lesions with type 2 reaction did not have all classical features of vasculitis. This finding was in slight disagreement with previous literature where vasculitis affecting arterioles and venules was observed in 50% cases of type 2 reaction by Job et al. in 1964 and Mabalay et al. in 1965.[7]
In our study, fibrin in vessel wall was the commonest sign observed followed by fibrin thrombi and neutrophils in vessel wall in few cases. The histological features of vasculitis depend upon the stage at which a lesion has been biopsied. An older lesion will have sparse neutrophilic infiltrate and predominance of mononuclear cells whereas an early lesion show predominantly neutophilic infiltrate with fibrin deposition. Occlusion of the vascular lumina with extensive involvement where vessels in lower part of the dermis and subcutaneous tissue are involved leads to necrosis or ulceration of the lesion. The vascular changes we noted were more prevalent in the upper and mid dermis than subcutaneous tissue.
Necrosis and ulceration is fairly uncommon in ENL in contrast to lucio reaction where ulceration and necrosis is almost always seen. In lucio reaction endothelial proliferation along with thrombosis of dermal and subcutaneous vessels leads to ischemic necrosis and ulceration. As we observed, occlusion of vessel lumen was seen in a few lesions and was limited to upper and mid dermis and that may be the reason why none of the lesion in our study showed ulceration and necrosis.
Similar to the observation of lymphocytic involvement of follicle in type 1 reaction, a few cases (5%) of type 2 reaction showed lymphocytic infiltration of sebaceous lobules.
Involvement of subcutaneous tissue by granulomatous infiltrate can be seen in cases of lepromatous leprosy though the lesion is not in reaction.[8] But the presence of neutrophils in subcutaneous tissue is an important clue to the type 2 reaction. Lobular or septal panniculitis can be seen in lesions of ENL.[9] We noted lobular panniculitis more commonly than a septal or mixed panniculitis.
Conclusion
Papillary dermal edema and lymphocytic infiltration within granulomas were the most consistent signs of type 1 lepra reaction followed by edema in granuloma and pyknosis of lymphocytes. Classical signs of vasculitis were not present in majority of lesions of ENL. Infiltration of granulomas by neutrophils was the most reliable sign in cases of type 2 reaction. A few new findings were folliculotropism, epidermotropism, and lymphocytic panniculitis in type 1 reaction and neutrophils in sweat ducts and lymphocytes in sebaceous lobules in type 2 reaction, which needs validation.
Acknowledgment
We are thankful to Dr. R. Ganpati and Dr.V.V. Pai from Bombay Leprosy Project, Mumbai, for their help in providing required literature for this study.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Lucas S. Bacterial diseases. In: David E, Rosalie E, Bernett J, George M, editors. Lever's histopathology of the skin. 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 575. [Google Scholar]
- 2.Hussain R, Lucas SB, Kifayet A, Jamil S, Raynes J, Uqaili Z, et al. Clinical and histological discrepancies in diagnosis of ENL reactions classified by assessment of acute phase proteins SAA and CRP. Int J Lepr Other Mycobact Dis. 1995;63:222–30. [PubMed] [Google Scholar]
- 3.Sehgal VN, Gautam RK, Koranne RV, Beohar PC. The histopathological study of type 1(Lepra) and type 2 (ENL) reactions in leprosy. Indian J Lepr. 1986;58:240–3. [PubMed] [Google Scholar]
- 4.Lazaro-Medina A, Tianco EA, Avila JM. Additional markers for the type I reactional states of borderline leprosy. Infect Immun. 1983;39:388–93. [PubMed] [Google Scholar]
- 5.Lockwood DN, Lucas SB, Desikan KV, Ebenezer G, Suneetha S, Nicholls P. The histological diagnosis of leprosy type 1 reactions: Identification of key variables and an analysis of the process of histological diagnosis. J Clin Pathol. 2008;61:595–600. doi: 10.1136/jcp.2007.053389. [DOI] [PubMed] [Google Scholar]
- 6.Palit A, Inamadar AC. Vasculitis: Approach to diagnosis and therapy. Indian J Dermatol Venereol Leprol. 2006;72:334–45. doi: 10.4103/0378-6323.27748. [DOI] [PubMed] [Google Scholar]
- 7.Job CK, Gude S, Maladen UP. Erythema nodosum leprosum- A clinicopathologic study. Int J Lepr. 1964;32:177–84. [PubMed] [Google Scholar]
- 8.Lucas S. Bacterial diseases. In: David E, Rosalie E, Bernett J, George M, editors. Lever's histopathology of the skin. 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 572. [Google Scholar]
- 9.Khopkar U, Phadke V, Dongre A. Basic Dermatopathology. In: Valia RG, Valia AR, editors. IADVL Textbook of dermatology. 3rd ed. Mumbai: Bhalani Publishing House; 2009. p. 85. [Google Scholar]


