Abstract
A 59-year-old woman presented with a history of rapidly progressive recurrent tumor of 6.5 cm diameter of the scalp. Histopathological examination revealed a case of malignant cylindroma. There has been no recurrence or metastases and the patient is disease free at the end of 15 months postoperatively. Malignant transformation occurs less often in solitary form of cylindroma, but once transformed, tumors behave aggressively with extensive local infiltrative growth or metastases. The case is reported to document a rare case of malignant cylindroma arising in a patient with solitary cylindroma on the parieto-temporal region.
Keywords: Cylindroma, malignant cylindroma, recurrent, scalp, solitary
Introduction
Cylindromas are benign skin appendageal tumors. The site of origin is still controversial. Cylindromas are most likely very primitive sweat gland tumors differentiating toward either the eccrine or apocrine line.[1,2] They most commonly occur on the head and neck as solitary or multiple tumors. Solitary cylindromas occur sporadically and typically are not inherited. Multiple tumors are inherited in an autosomal dominant manner. Multiple lesions can cover the entire scalp giving an appearance of disfiguring turban, and hence, the eponym “turban tumor”. Malignant cylindromas are very rare with only few single reports described in literature. Malignant transformation occur more commonly in the multiple variant than the solitary cylindromas.[3,4] We report a rare case of malignant cylindroma arising in a patient with a solitary lesion on the parieto-temporal region.
Case Report
A 59-year-old female presented with chief complaint of a rapidly growing painful mass over right parieto-temporal region. She had a history of excision of similar kind of tumor at the same site twelve years back. Histopathological report of excision biopsy at that time was benign cylindroma. The lesion was exophytic, well circumscribed of 7 × 5 × 3.5 cm size. On palpation, it was firm and tender. There were no lymph nodes palpable in the neck or in other regions. Radiographic examination of the skull did not show any abnormality and magnetic resonance imaging of the brain revealed no intracranial pathology. The patient's family and medical history was non-contributory. All the laboratory investigations were within normal range. Under general anesthesia, wide surgical excision of the lesion with 1.5 cm intact skin margins was done after carefully separation of the facial planes. Skin grafting was performed.
Specimen was submitted in the histopathology section. On gross examination, the lesion was exophytic with irregular nodular surface [Figure 1]. Cut surface was solid and homogenously grey white. Multiple sections were taken. Microscopically, majority of the histological sections revealed malignant component with irregular asymmetrical nodules and large solid sheets of tumor cells [Figure 2]. Marked cellular pleomorphism with prominent nucleoli and mitosis up to 10-12/ high power field was noted [Figure 3]. Surgical margins were free of tumor, and there was no aponeurotic invasion in any of the sections. There were sections with the typical histopathological pattern of cylindroma. This consisted of aggregated, multiple circumscribed islands of epithelial cells surrounded by hyaline sheaths arranged in jigsaw pattern [Figure 4].
Figure 1.

Gross photograph showing exophytic growth with ulcerated and irregular nodular surface
Figure 2.
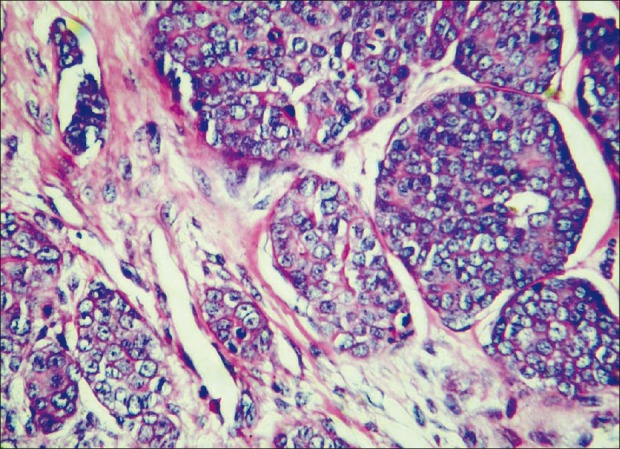
Photomicrograph showing malignant component with irregular asymmetrical nodules. (H and E stain, 400×)
Figure 3.
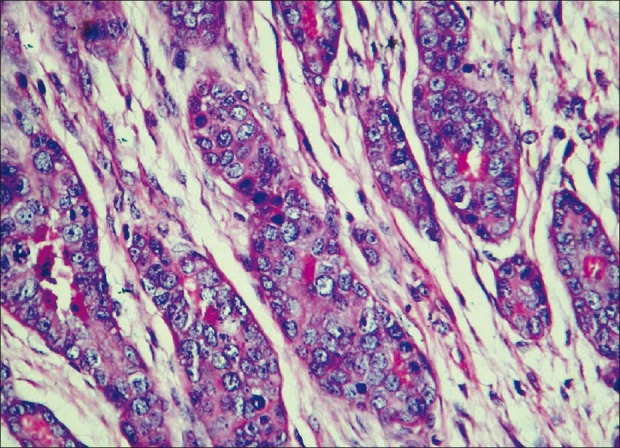
Photomicrograph showing pleomorphism with prominent nucleoli and mitosis (H and E stain, 400×)
Figure 4.
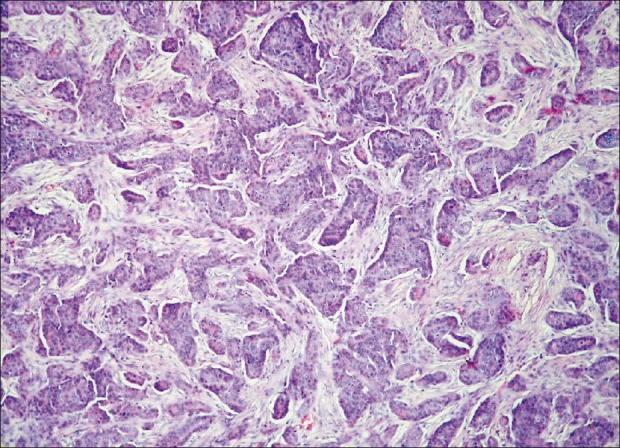
Photomicrograph showing histopathological pattern of cylindroma consisting of aggregated, multiple islands of epithelial cells surrounded by hyaline sheaths arranged in jigsaw pattern. (H and E stain, 40×)
The patient had been on follow-up and at the end of 15 months postoperatively there were no local or distant metastases. All the laboratory investigations, radiological examination of chest and computerized tomography of cranium and bones are normal.
Discussion
Ancell[5] first described the cylindroma in 1842 and malignant change was described in 1929 by Weidman.[6] The clinical features of cutaneous cylindroma are pink, skin colored, nodular growth; it may be solitary or multiple and vary in size from a few millimeters to centimeters. The ratio of women to men is between 2.1 and 3.1. The lesions usually first appear in second decade of life and growth is gradual. The lesions are usually painless but 35% patients reported the same to be painful.[7,8]
Clinically, cylindroma has two types of presentations: i) a solitary form, occurring in patients without a family history of cutaneous cylindromas and; ii) a variant with multiple cutaneous cylindromas, which is supposed to be inherited in an autosomal dominant manner. Cylindromas are also a component of the Brooke-Spiegler tumor; this is a dominantly inherited form associated with multiple facial trichoepitheliomas. The solitary form occurs as frequently as the multiple form or even more frequently. Malignant transformation of cutaneous cylindromas is very rare and is usually seen in multiple types.[3,9,10]
The prevalence of malignant cylindroma is not well-established since the literature largely consists of case reports and not all the cases are documented properly. Using a Pubmed database search, we found a total of 36 well-documented cases of malignant cylindroma in the literature. Out of these 36 cases, only 9 transformed from the solitary type. Studies have reported external factors like incomplete surgical excision, radiation therapy, frequent trauma and chronic irritation to play role in histogenesis of malignancy. In the present case, history of previous surgical excision was present. Clinically, malignant transformation is suggested by ulceration, rapid growth, bleeding, color change, pain and fixation of the lesion. In our patient, there was recurrence of tumor with rapid progressive enlargement.
The histological features of malignant cylindroma are prominent large cells, pleomorphic nuclei, increased abnormal mitoses, loss of jigsaw pattern, loss of hyaline sheaths and loss of peripheral palisading at the tumor island periphery. Malignant cylindroma is a locally aggressive tumor and can spread along draining lymphatic vessels. There may be metastases to regional lymph nodes, stomach, thyroid, liver, lung and bones. Transcranial invasion and erosion have also been reported.[8,11,12]
Immunohistochemically, cylindromas express markers indicating derivation from both eccrine and apocrine glands. Immunohistochemical expression of S-100, alpha-smooth muscle actin, EMA, CEA, laminin, collagen IV, fibronectin and CD-34 are seen. Immunohistochemistry is not helpful in distinguishing benign from malignant cylindroma. We did not perform immunohistochemistry in the present case.[13,14]
The preferred mode of treatment for solitary lesions is wide local excision because of undesirable recurrence rates and the risk of malignant transformation of these tumors. The reported treatment modalities are simple excision, scalping, Mohs’ micrographic surgery and laser ablation. Multiple cylindromas usually require extensive plastic surgery that may be obviated by progressively excising a group of nodules in multiple sittings.[4,15]
Malignant cylindroma arising in solitary lesion is very rare, but should be considered among clinically altered tumors. Once transformation takes place, the tendency for aggressive local destruction and potential to metastasize is high. Therefore, early diagnosis and management offers the patient the best possibility of cure.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Weedon D. 2nd ed. Edinburgh: Churchill Livingstone; 2003. Skin pathology; pp. 890–1. [Google Scholar]
- 2.Massoumi R, Podda M, Fassler R, Paus R. Cylindroma as tumor of hair follicle origin. J Invest Dermatol. 2006;126:1182–4. doi: 10.1038/sj.jid.5700218. [DOI] [PubMed] [Google Scholar]
- 3.Durani BK, Kurzen H, Jaeckel A, Kuner N, Naeher H, Hartschuh W. Malignant transformation of multiple dermal cylindromas. Br J Dermatol. 2001;145:653–6. doi: 10.1046/j.1365-2133.2001.04460.x. [DOI] [PubMed] [Google Scholar]
- 4.Lo JS, Peschen M, Snow SN, Oriba HA, Mohs FE. Malignant cylindroma of the scalp. J Dermatol Surg Oncol. 1991;17:897–901. doi: 10.1111/j.1524-4725.1991.tb03281.x. [DOI] [PubMed] [Google Scholar]
- 5.Ancell H. History of a remarkable case of tumors, developed on the head and face, accompanied with similar disease on the abdomen. Med Chir Trans. 1842;25:227. doi: 10.1177/095952874202500116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiedemann A. Further contributions to the knowledge of the so-called cylindroma of the scalp. Arch Dermatol. 1929;159:180–7. [Google Scholar]
- 7.Hammond DC, Grant KF, Simpson WD. Malignant degeneration of dermal cylindroma. Ann Plast Surg. 1990;24:176–8. doi: 10.1097/00000637-199002000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Lotem M, Trattner A, Kahanovich S, Rotem A, Sandbank M. Multiple dermal cylindroma undergoing a malignant transformation. Int J Dermatol. 1992;31:642–4. doi: 10.1111/j.1365-4362.1992.tb03985.x. [DOI] [PubMed] [Google Scholar]
- 9.Gerretsen AL, van der Putte SC, Deenstra W, van Vloten WA. Cutaneous cylindroma with malignant transformation. Cancer. 1993;72:1618–23. doi: 10.1002/1097-0142(19930901)72:5<1618::aid-cncr2820720521>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 10.Kim C, Kovich OI, Dosik J. Brooke - Spiegler syndrome. Dermatol Online J. 2007;13:10. [PubMed] [Google Scholar]
- 11.De Francesco V, Frattasio A, Pillon B, Stinco G, Scott CA, Trotter D, et al. Carcinosarcoma arising in a patient with multiple cylindromas. Am J Dermatopathol. 2005;27:21–6. doi: 10.1097/01.dad.0000141548.69423.c7. [DOI] [PubMed] [Google Scholar]
- 12.Wyld L, Bullen S, Browning FS. Transcranial erosion of a benign dermal cylindroma. Ann Plast Surg. 1996;36:194–6. doi: 10.1097/00000637-199602000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Tellechea O, Reis JP, Ilheu O, Baptista AP. Dermal cylindroma.An immunohistochemical study of thirteen cases. Am J Dermatopathol. 1995;17:260–5. [PubMed] [Google Scholar]
- 14.Meybehm M, Fischer HP. Spiradenoma and dermal cylindroma: Comparative immunohistochemical analysis and histogenetic considerations. Am J Dermatopathol. 1997;19:154–61. doi: 10.1097/00000372-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Retamar RA, Stengel F, Saadi ME, Kien MC, Della Giovana P, Cabrera H, et al. Brooke-Spiegler syndrome-report of four families: Treatment with CO2 laser. Int J Dermatol. 2007;46:583–6. doi: 10.1111/j.1365-4632.2007.01689.x. [DOI] [PubMed] [Google Scholar]


