Abstract
Background
Brief and low-burden HIV risk reduction counseling interventions are needed for populations at greatest risk for HIV infection.
Purpose
This randomized controlled trial tested a brief theory-based counseling intervention delivered entirely over the telephone for men who engage in unprotected intercourse with men.
Methods
Participants received either risk reduction counseling that included information, motivational enhancement and behavior skills building, or brief HIV education counseling. A total of 319 participants completed follow-up assessments over a 10-month period. Descriptive and random effects mixed models are used to evaluate findings.
Results
Results demonstrate that a brief telephone intervention can reach and engage high-risk men in risk reduction counseling. Nearly one third of participants identified as men of color; the median age was 33 years. Participants in both counseling conditions increased their motivation and behavioral skills to practice safer sex and reduced their number of sex partners and frequencies of engaging in unprotected anal sex over the study observation period. However, there were few differences between intervention conditions.
Conclusions
The effects of repeated measurement reactivity and brief interpersonal consciousness raising may account for the lack of differences between counseling conditions and the decrease in risk for all participants over time.
INTRODUCTION
Efforts to control the spread of HIV continue to emphasize behavior change strategies to reduce sexual risk practices and promote safer sex. Prevention programs and research efforts for men who have sex with men (MSM) most often target high-risk individuals who are seeking prevention services. However, MSM represent a highly diverse population with respect to their readiness to change sexual risk behaviors, and engaging high-risk men who are not yet ready to change their behaviors in prevention programs presents considerable challenges. In addition, there are now a wide variety of harm reduction strategies that MSM are enacting on their own, including selecting partners assumed or known to be of the same HIV status (1), negotiating sexual positions such as insertive or receptive positions during anal intercourse as well as penile withdrawal prior to ejaculation (2), and “safer” relationship contexts (negotiated safety relationships (3,4). These behavioral contexts underlie varying degrees of HIV transmission risks among sexually active MSM.
Individual and idiosyncratic patterns of readiness to change and harm reduction strategies suggest the need for client-centered approaches that meet individuals “where they are” in terms of their readiness to change as well as their skills and abilities to enact behavior change. Research has shown substantial differences in behavior are often related to contextual factors such as the HIV status of the person and their partner as well as the type of relationship an individual has with their partner (e.g., primary partnerships, occasional partnerships, one-time partnerships). Sexual relationships between persons who know each other’s HIV status are substantially safer in terms of HIV transmission risks than are sexual relationships where the HIV status of partners is unknown (5). In addition, studies show that condoms are more likely used in occasional sexual relationships compared to long-term primary partnerships (6). Thus, at least two interrelated dimensions, HIV status knowledge and relationship type (7), are related to sexual risks, pointing toward the use of individualized interventions that can tailor intervention content to prevention needs and behavioral contexts.
Interventions that successfully engage high-risk populations that may be reluctant to seek prevention services therefore must be sensitive to the unique circumstances of the individual. Brief risk reduction counseling interventions offer several advantages to achieving these goals. Brief client-centered prevention counseling has been demonstrated effective in reducing HIV risks in the context of HIV antibody testing. The Center for Disease Control and Prevention’s Project RESPECT, for example, showed that two 20-min HIV risk reduction counseling sessions conducted in conjunction with HIV antibody testing demonstrated the same efficacy in reducing HIV risk behavior and recurrent sexually transmitted infections (STI) as did a four-session enhanced counseling intervention (8). Project RESPECT showed that participants in the two-session risk reduction counseling intervention had a 30% reduction in new STI over 6 months follow-up and a 20% reduction over 12 months follow-up.
Risk reduction counseling has also demonstrated promising outcomes when delivered outside of HIV testing. Belcher and colleagues (9) tested a 120-min HIV prevention counseling intervention for women also grounded in the Information, Motivation, and Behavioral Skills (IMB) model. Similarly, Kalichman and colleagues (10) demonstrated the efficacy of a 90-min IMB model-based risk reduction counseling intervention for men and women receiving STI clinic services. These studies have shown promise for brief client-centered HIV prevention counseling interventions, but these models still require facility attendance and engage persons who are seeking services.
In another brief intervention trial, Patterson and colleagues (11) tested an intervention designed to reduce the sexual risk behaviors among people living with HIV infection. Men (91% of the sample) and women who reported engaging in unprotected sex with HIV-negative or unknown HIV status partners were randomly assigned to one of four study conditions: (a) a single counseling session targeting problem areas identified by the participant in three possible intervention domains (i.e., condom use, negotiation, disclosure); (b) a single-session comprehensive intervention that covered all three intervention domains; (c) the same comprehensive intervention, plus two monthly booster sessions; or (d) a three-session diet and exercise attention-control condition. The median number of unprotected sex acts decreased across groups. Because the diet and exercise control group changed a comparable magnitude as the risk reduction conditions, the results suggest that the intensive repeated assessments raised consciousness and affected behavior across groups. This speculative conclusion seems plausible because the data were collected in interviews and “no attempt was made to separate data collection from the intervention counseling” (p. 140.)
In a previous study, we tested the feasibility of delivering a brief telephone-based, low-burden risk reduction counseling intervention for high-risk MSM. The intervention model was based on the “Drinker’s Check Up,” a brief intervention that has been demonstrated effective in engaging problem drinkers who are behavior change resistant and ambivalent to seek services (12,13). We conducted a randomized controlled pilot intervention to evaluate the efficacy of the telephone-based brief counseling intervention based on Motivational Enhancement Therapy (MET) to reduce sexual risk taking among MSM in Seattle, Washington (14). The study specifically targeted men who were currently engaging in unsafe sex but were not committed to making changes toward safer behaviors. Counselors used motivational interviewing strategies in a single 90-min session to enhance readiness for change, promote greater intentions to use condoms, and support safer sex practices. Men were randomized to receive the experimental “sex check-up” intervention or to a delayed counseling control condition. Minority participants who received the sex check-up intervention were significantly less likely to have engaged in unprotected anal intercourse at follow-up compared to those in the delay condition. These findings were encouraging and support the potential efficacy of a brief intervention based on motivational enhancement principles for promoting safer sex practices among at-risk MSM. The study presented here was therefore conducted to fully test the efficacy of the brief sex check-up risk reduction counseling model for high-risk MSM.
We focused our intervention trial on overcoming barriers to attracting and engaging men at high risk for HIV transmission. We used tailored marketing strategies to attract men who may be ambivalent about engaging in prevention services (15) and implemented procedures to lower barriers to participation through several mechanisms including using a telephone modality, brief counseling protocol, and an option to remain anonymous. Guided by the IMB model of risk behavior change (16), we examined a variety of risk factors in relation to high-risk sexual behavior that incorporates partner serostatus and type of relationship, with particular emphasis on participants’ motivations and ambivalence toward adopting safer sex practices. We hypothesized that a brief theory-based low-burden risk reduction counseling intervention would result in lower sexual risk behavior over time compared to an information and education session control condition. We also predicted that risk reduction outcomes would vary depending on contextual factors, particularly the HIV status of study participants and their partners and the type of relationships in which risk behavior occurred.
METHODS
Participants
Participants were recruited in Seattle, Washington, and Portland, Oregon, between November 2002 and June 2004, primarily through the efforts of outreach workers in gay-identified bars and paid print advertisement in the local alternative and gay press. Based on power calculations from behavioral findings in our pilot trial, we targeted a sample size of 356 participants. Eligibility criteria required that the individual be 16 years of age or older, report at least one episode of unprotected anal intercourse (UA) with a male partner in the prior 90 days, and not be receiving counseling services to become sexually safer elsewhere. Individuals were also excluded if they were in either a “mutually monogamous” or “negotiated safety” relationship that included requirements that the caller and his main partner had been tested for HIV twice, at least 3 months apart, while maintaining their agreement.
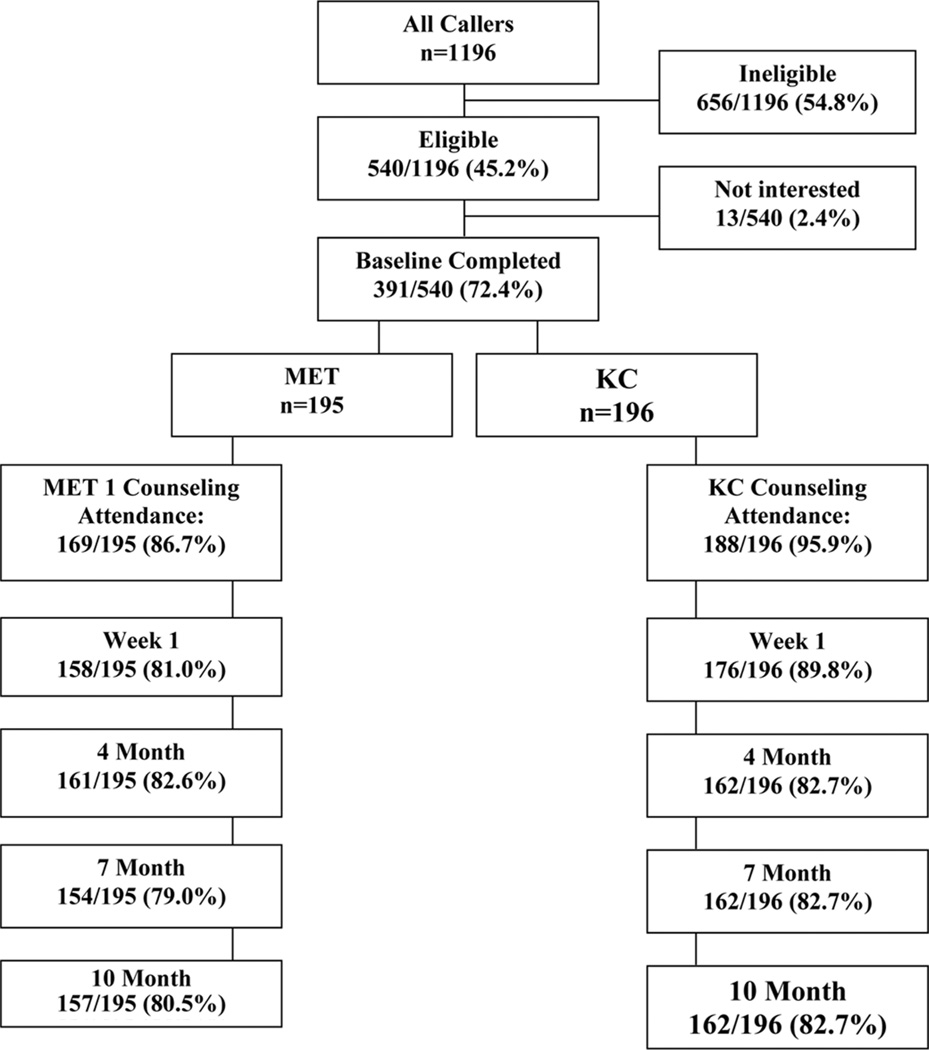
Figure 1 describes participant flow from the initial screening call through the final 10-month assessment. Of 1,196 callers, 45.2% (n = 540) were found eligible for the study. Of the 540 eligible, 527 (98%) expressed interest in participating in the study, and 391 (72%) men completed their baseline interview and enrolled in the study. More than 90% of participants attended counseling. Retention remained at about 80% or slightly higher at each of the scheduled follow-up assessments over 10 months with no difference between conditions.
FIGURE 1.
Participant flow through the Sex Check Study. Note. MET = Motivational Enhancement Therapy; KC = Knowledge Check.
Procedures
All interactions with study participants occurred by telephone. Following a screening interview, interested and eligible callers were mailed a self-assessment questionnaire (SA) and scheduled for a computer-aided telephone interview (CATI) about 7 to 10 days later. All SAs were required to be completed prior to the CATI interview, and baseline CATI interviews were required to be completed within 30 days of the participant’s screening interview. The CATI session lasted an average of 45 min and included a review of the SA prior to conducting the CATI for both completeness and data quality. At the conclusion of the CATI, interviewers conducted a short computerized randomization exercise and informed the participant of their study assignment (MET, or the Knowledge Check [KC]).
Follow-up assessments were scheduled to be completed 1 week following the conclusion of the counseling intervention and at 4, 7, and 10 months from the study enrollment date. All follow-up interviews involved a SA and CATI interview similar to the baseline assessment, and SAs were required to be completed prior to the CATI interview at all assessment points. Monetary incentives were awarded following each assessment including baseline ($25); 1-week postcounseling ($25); and 4 ($30), 7 ($40), and 10 ($40) month postbaseline assessments, respectively. In addition, a $40 bonus was awarded for completion of all assessments. All assessments and counseling protocols were translated into Spanish. The Institutional Review Board at the University of Washington approved all study protocols.
Intervention Conditions
Both study conditions consisted of one-on-one sessions with a counselor over the telephone. The active condition, MET, involved up to three sessions with each lasting up to 90 min. The first session was required to be completed within 30 days of the baseline CATI, and the remaining session(s) within 42 days of baseline CATI. MET is a systematic approach for evoking change based on principles of motivational psychology and designed to produce rapid, internally motivated change (17–19). Motivational interviewing techniques allow for a client-centered, nonthreatening interaction between counselor and participant (20). This treatment approach does not attempt to train the client, step by step, but instead employs motivational strategies to mobilize the individual’s own change resources. Components include feedback of personal behavior, emphasis on personal responsibility, clear advice to change, a menu of alternative change options, therapist empathy, and facilitation of optimism to change. Counselors listened for and reinforced statements of motivation that were consistent with safer sex practices and, when appropriate, facilitated goal setting and identified possible risk reduction strategies. Participants randomized to the MET were mailed a personalized feedback report (PFR) prior to their first counseling session. A PFR was developed for each participant based on the responses they provided in their baseline assessment interview. The PFR was designed to guide the counseling session through a review of the participant’s knowledge about HIV/AIDS, their current sexual activity, substance use patterns and their relation to safe sex practices, intentions to use condoms, reasons for having sex that included perceived benefits and losses regarding condom use/safe sex practices, and self-efficacy for strategies to avoid unsafe sex. Because the PFR summarized the participant’s sexual practice behavior, it allowed the session(s) to be “tailored” to each participant’s risk profile and most salient concerns.
The control condition, the KC, involved a single didactic session that typically lasted between 30 and 45 min and was required to occur within 30 days of the baseline date. The session was designed to provide information similar to what an individual would receive when contacting an AIDS Hotline or undergoing HIV pretest counseling. The counselor began by delivering a brief (15 min) HIV/sexually transmitted disease educational update that was tailored for the individual’s risk profile (sexual and intravenous drug use [IDU]), based on his baseline assessment. The counselor also corrected participant misinformation concerning HIV, based on incorrect answers to the HIV knowledge component in the baseline assessment.
Counselors and Clinical Supervision
Both intervention conditions were conducted in collaboration with a community based organization, Gay City Health Project. Five counselors were employed over the course of the study, and all received extensive training in motivational interviewing (MI). Training consisted of reading the manual and related materials, watching the MI training videos, and workshops with didactic and experiential exercises targeted to enhance specific MI skills. Counselors received additional training to be competent to discuss the latest trends in STIs that included information about symptoms, treatment resources, and epidemiology of various types of STIs. Because this study was conducted entirely by telephone, counselors were trained to deliver the intervention using role-plays via telephone. Two counselors were bilingual (English/Spanish) and were native Spanish-language speakers. Counseling sessions were monitored by the clinical director on an ongoing basis throughout the trial, and weekly supervisory meetings were held to ensure consistent clinical practice between counselors. Approximately 10% of all counseling sessions were coded by the clinical director using a modified version of the Motivational Interviewing Treatment Integrity coding system (21) to assess adherence to MET. In addition, a counselor behavior checklist designed specifically for the study was completed by the clinical director and counselor. The MET fidelity measure consisted of counting MI-consistent behaviors, including questions (open and closed), reflections (repeat, rephrase, paraphrase, and summary), affirmations, and information giving (with and without the participant’s permission). Counselors were provided feedback on their performance by looking over the behavior counts of the session and competency indexes such as reflection to question ratio and percentage of high-level (paraphrase and summary) versus low-level (repeat and rephrase) reflections. Both types of intervention sessions were coded in this manner to ensure discriminability between conditions.
Measures
Demographics and personal history
Demographic characteristics (age, race, and education), sexual identity, and participant’s HIV status were collected at the initial screening assessment. Depressive symptoms was measured as a potential intervention moderator using the 20-item Center for Epidemiologic Studies Depression scale (α = .93) (22) referenced to the prior 7 days.
Substance use
An inventory of alcohol, recreational drugs, or improperly used prescription drugs (alcohol, marijuana, Viagra, poppers, cocaine, amphetamines, sedatives, hallucinogens, GHB, ecstasy, and heroin or other opiates), and a self-assessment of substance abuse (“Do you feel you need to quit or cut back on your use of …”) were collected during the CATI. The Drug Abuse Screening Test (23) was also administered. Drug use items were referenced to the prior 90 days or time since the participant’s last interview.
IMB model mediating constructs
To assess HIV knowledge (i.e., information), we used a 30-item scale adapted from Carey and colleagues (17) that primarily focused on factors affecting HIV transmission or proper condom use.
Several indicators of motivation were assessed given that the active intervention model focused on motivational enhancement. Outcome expectancies about condoms were captured with five items specific to “costs” associated with condom use (α = .70) and five items specific to “benefits” of their use (α = .66); each item was measured using a 4-point scale (strongly disagree, disagree, agree, strongly agree). Stage of change (24) specific to UA was assessed separately for primary and nonprimary partners. Each question offered five responses that categorized the participant as a precontemplator (no plans to change behavior), a contemplator (might consider behavior change but no plans to initiate change during next 30 days), in preparation (planning to initiate change in next 30 days), in action (initiated changes, but less than 90 days ago), or in maintenance (initiated and maintained changes more than 90 days ago). Current motivation to adopt safer sex behaviors (5-point item from not at all strong to extremely strong), and perceived risk for HIV transmission referenced to the prior 90 days (none, slight, somewhat, a great deal of risk) were also assessed. Participants also reported their intentions to use condoms during insertive and receptive anal intercourse with a primary partner (two items) and a nonprimary partner (two items). Each item was assessed using a 5-point Likert scale (extremely unlikely, unlikely, 50–50 chance, likely, extremely likely).
Behavioral skills enactment was captured with 12 items that measured the frequency of use of behavior strategies to practice safer sex. Each item was measured on a 5-point scale (never, rarely, half the time, often, always) and responses of often or always were used to indicate frequent use of the strategy (α = .83).
Sexual Behavior Outcomes
Sexual behavior measures included the number of male partners by partner type (primary, occasional, one time), sex with a female partner, sex in a paid/paying context, and type of sex reported (insertive or receptive anal or oral sex, with and without condoms). Primary partners were defined as “sexual partners whom you may or may not live with, but have a strong emotional commitment to” and occasional partners as partners “you had sex with two or more times in the past, but do not consider as your primary partner.” Occasional and one-time partners are treated as nonprimary partners. Five items (yes or no responses) were used to assess the presence of an STI in the prior 6 weeks (e.g., Have you had an open sore on your penis? Have you had burning or pain when urinating?).
Frequencies of sex behaviors were collected specific to each of the participant’s three most recent partners, and in aggregate form by partner type category for any additional male partners. Participants were asked to report the number of episodes of unprotected and protected, insertive and receptive anal intercourse in the prior 90 days at baseline, and since their last interview at each of the follow-up assessments.
Data Analysis
Baseline differences between study groups were evaluated using t tests for continuous measures and chi-square tests for categorical variables. A p value cutoff of .10 was used to identify variables for inclusion in subsequent multivariate models. Paired t tests (continuous measures) or rank sum tests (categorical measures) were used to evaluate within sample changes over time among mediating/IMB constructs; changes were evaluated between baseline and the 1 week (i.e., immediate postcounseling assessment) and between baseline and the 10-month assessment to assess durability of changes.
Outcomes measures are behavioral count data collected at the baseline, 4-, 7-, and 10-month follow-ups. Descriptive results are presented for baseline, 4-month (short-term outcome), and 10-month (long-term outcome) assessment points.
STATA 8.0 (25) was used to evaluate counseling efficacy using data from baseline, 4-, 7-, and 10-month assessments. Effect sizes of the counseling intervention (MET vs. KC) for each of the behavioral outcomes were determined using random effects negative binomial regression method (26) and are presented as relative risks comparing the MET to the KC group. Change in behavior over time was also assessed using these methods by inserting dummy variable indicators for each assessment point into the models, and interactions between assessment point and treatment group were tested to determine if changes in behavior over time differed by treatment group.
Statistical significance was set at .05 when evaluating the effects of counseling. All results are based on intent-to-treat principles and inclusion is therefore independent of level of participation in the counseling intervention.
RESULTS
A total of 391 participants enrolled in this trial. Results are based on 319 (81%) participants who completed their 10-month follow-up assessment. Although all project materials and services were available in Spanish, only 3 (1%) of the analysis cohort utilized this service. Baseline characteristics including demographic, motivation, and behavior measures are presented in Table 1. Most measures indicate that the study groups were comparable at baseline, indicative of successful randomization procedures.
TABLE 1.
Baseline Demographic, Motivational, External, and Behavioral Risk Measures, by Study Group
| Characteristic | % of Samplea | METb (%) | KCc (%) | p |
|---|---|---|---|---|
| Demographics | ||||
| Age group (%) | .669 | |||
| 16–19 | 5.6 | 6.4 | 4.9 | |
| 20–24 | 15.0 | 17.2 | 13.0 | |
| 25–29 | 17.2 | 18.5 | 16.0 | |
| 30–39 | 27.6 | 25.5 | 29.6 | |
| 40+ | 34.5 | 32.5 | 36.4 | |
| Race/Ethnicity (%) | .502 | |||
| Black | 11.5 | 13.0 | 10.0 | |
| Latino | 13.4 | 13.6 | 13.1 | |
| White | 70.7 | 67.5 | 73.8 | |
| Otherd | 4.5 | 5.8 | 3.1 | |
| Education (%) | .483 | |||
| ≤High school/GED | 22.6 | 24.2 | 21.0 | |
| Vocational/trade/Some college/2-year degree | 41.1 | 42.7 | 39.5 | |
| College graduate | 36.4 | 33.1 | 39.5 | |
| Sexual identity (%) | .083 | |||
| Gay/Queer | 87.3 | 84.1 | 90.6 | |
| Bisexual | 12.7 | 15.9 | 9.4 | |
| Female partner (%) | .112 | |||
| No | 96.6 | 94.9 | 98.1 | |
| Yes | 3.4 | 5.1 | 1.9 | |
| Motivations | ||||
| Motivation to be safer (%) | .682 | |||
| Slightly strong | 25.1 | 22.9 | 27.2 | |
| Moderately strong | 35.7 | 36.9 | 34.6 | |
| Very strong | 39.2 | 40.1 | 38.3 | |
| Perceived HIV risk (%) | .432 | |||
| None/Slight | 54.5 | 54.1 | 54.9 | |
| Somewhat | 30.1 | 28.0 | 32.1 | |
| Great deal | 15.4 | 17.8 | 13.0 | |
| External factors | ||||
| HIV status (%) | .599 | |||
| Not tested/unknown | 9.4 | 10.8 | 8.0 | |
| Negative | 69.3 | 69.4 | 69.1 | |
| Positive | 21.3 | 19.7 | 22.8 | |
| Depressive symptomse | .253 | |||
| No indication | 51.4 | 56.1 | 46.9 | |
| Mild depression | 16.3 | 15.3 | 17.3 | |
| Major depression | 32.3 | 28.7 | 35.8 | |
| DAST (>2) | 35.1 | 41.4 | 29.0 | .020 |
| Feels need to cut back or quit substance use Behaviors | 38.7 | 43.3 | 34.2 | .094 |
| No. male partners in past 90 days (M, SD) | 8.3 [12.4] | 8.7 [14.1] | 7.9 [10.4] | .547 |
| Primary partner (%) | 55.8 | 58.0 | 53.7 | .444 |
| Occasional partner (%) | 66.8 | 66.9 | 66.7 | .968 |
| One-time partner (%) | 73.4 | 77.7 | 69.1 | .083 |
| Any STI symptoms | 15.7 | 16.6 | 14.8 | .668 |
| Sex in paid/paying situations | 10.0 | 10.2 | 9.9 | .926 |
Note. DAST = Drug Abuse Screening Test; STI = sexually transmitted infections.
N = 319.
n = 157.
n = 162.
Fourteen participants include 2 Native American, 6 Asian/Pacific Islander, and 6 multiracial.
Twenty-item Center for Epidemiologic Studies Depression Scale.
Information, Motivation, Behavioral Skills Mediating Constructs
Again, MET and KC study groups were comparable at baseline. Knowledge about HIV (e.g., factors associated with disease transmission) was high for both study groups; participants correctly answered 80% of the 30 items at baseline. With regard to motivation measures, participants reported an average of 2.0 costs and 1.7 benefits of condom use for anal sex. A pattern specific to partner type emerged regarding stage of change and intentions to use condoms; nearly two thirds considered themselves to be precontemplators or contemplators regarding their readiness to change anal sex behaviors with a primary partner, compared to about 40% relative to nonprimary partners. Similarly, participants reported lower intentions to use condoms for anal sex with primary partners (M = 5.0) compared to nonprimary partners (M = 6.4). Finally, a mean of 6.2 behavioral enactment skills, measured as the number of strategies often or always used to be sexually safer, was observed.
There were few between-group differences among these constructs at any of the follow-up assessment points. However, significant within sample (i.e., MET and KC participants combined) changes over time were noted between baseline and the 1-week and 10-month assessment points. Specifically, increases in knowledge, decreases in costs of condom use, increases in benefits of condom use, increases in intentions to use condoms with both primary and nonprimary partners, and increases in the use of safer sex strategies were noted at the 1-week post counseling and 10-month follow-up assessment points, relative to baseline (data not shown).
Sexual Behavior Outcomes
Patterns of behavior change with regard to numbers of partners (by partner type and serostatus) and frequencies of behaviors were found to be similar to those described for the IMB constructs. Significant declines in risk behavior occurred over time and, with few exceptions, between-group differences were not detected (see multivariate results, next). At baseline, MET participants reported a mean of 8.1 (SD = 14.0) nonprimary partners compared to 7.3 (SD = 10.6) among KC participants (p = .58). Declines in the number of nonprimary partners were observed for both MET and KC participants at both the 4-month assessment (M = 5.2 and 5.6, respectively) and the 10-month assessment (M = 4.4, SD = 11.3; M = 4.8, SD = 11.5, respectively).
Reductions samplewide were also observed in frequencies of UA (both receptive and insertive behaviors) over time. For example, at baseline MET and KC conditions reported means of 2.1 (SD = 7.2) and 2.2 (SD = 5.7) episodes of UA-receptive with nonprimary partners, respectively, and by the 10-month follow-up had reduced to 0.8 episodes (SD = 3.1) and 0.8 episodes (SD = 3.9], whereas UA-insertive behavior with nonprimary partners declined from 2.1 (MET) and 2.4 (KC) episodes at baseline to 1.0 and 1.4 episodes at the 10-month follow-up, respectively.
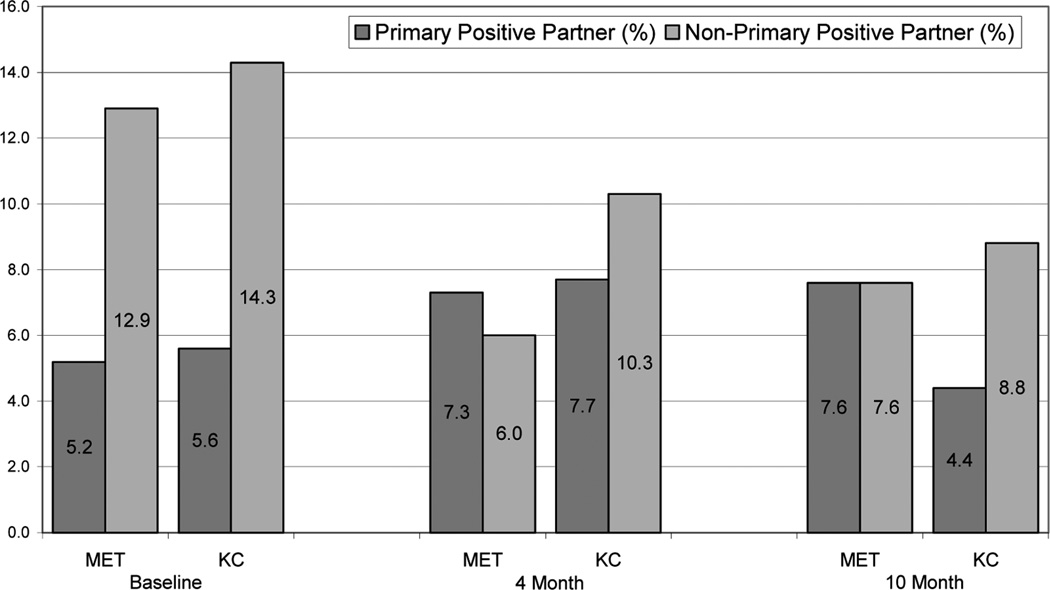
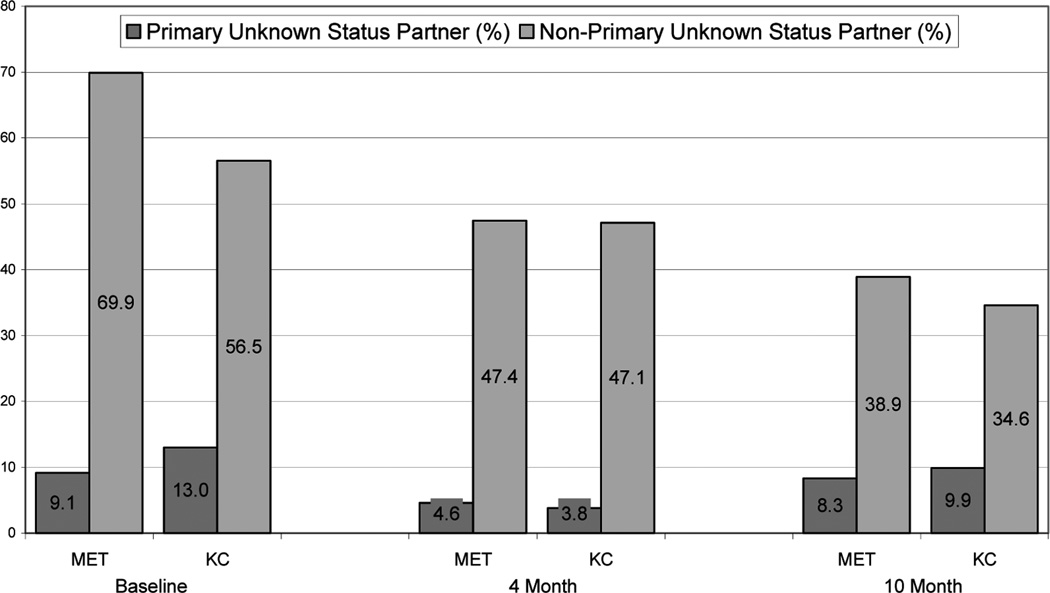
Similarly, declines in the proportion of participants reporting a nonprimary, HIV-positive partner or a nonprimary partner of unknown serostatus were reported (see Figures 2 and 3). However, a slight increase in the proportion of men reporting a primary positive partner was noted at the 4-month assessment (MET and KC) and 10-month assessment (MET only). Finally, the proportion of men reporting unknown status primary partners declined between baseline and each follow-up assessment.
FIGURE 2.
Percentage of participants reporting an HIV-positive sex partner, by partner type, study group, and assessment time. Note. MET = Motivational Enhancement Therapy; KC = Knowledge Check.
FIGURE 3.
Percentage of participants reporting an HIV unknown status sex partner, by partner type, study group, and assessment time. Note. MET = Motivational Enhancement Therapy; KC = Knowledge Check.
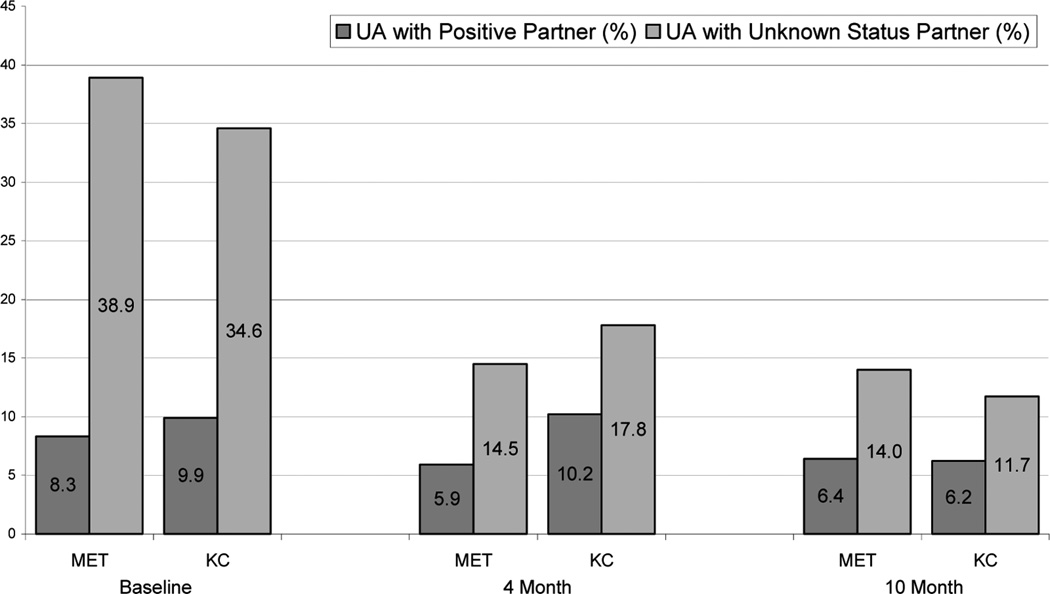
The overall decline in the proportion of men reporting HIV-positive partners was reflected in the decrease in men reporting UA with an HIV-positive partner; at baseline 8.3% of MET and 9.9% of KC reported this behavior compared to 6.4% MET and 6.2% KC at 10 months (Figure 4). The higher prevalence of UA with partners of unknown serostatus at baseline allowed for greater declines in this behavior at both the 4- and 10-month assessments. More than one third of both MET and KC participants reported this behavior at baseline compared to 14% MET and 11.7% KC at 10 months.
FIGURE 4.
Percentage of participants reporting unprotected anal intercourse (UA), by partner serostatus, study group, and assessment time. Note. MET = Motivational Enhancement Therapy; KC = Knowledge Check.
Multivariate analyses confirmed the lack of significant associations between intervention conditions with regard to numbers of nonprimary partners and frequencies of risk behaviors with nonprimary partners (see Table 2). However, a model specific to primary partners revealed thatMET participants reported a significantly higher rate of UA-receptive behavior with primary partners compared toKCparticipants (adjusted relative risk [RR] = 1.82, 95% confidence interval [CI] = 1.15–2.90), and a modestly (although nonsignificant) greater rate of UA-insertive behavior with primary partners (adjusted RR = 1.35, 95% CI = 0.86–2.14).
TABLE 2.
Association Between Study Condition (MET vs. KC) and Behavioral Outcomes
| Outcome Measure | Adjusted RRa,b (MET vs. KC) |
95% CI |
|---|---|---|
| No. nonprimary partners | 1.08 | 0.87–1.35 |
| UA: Receptive with nonprimary partners | 1.01 | 0.69–1.48 |
| UA: Insertive with nonprimary partners | 0.88 | 0.64–1.21 |
| UA: Receptive with primary partners | 1.82 | 1.15–2.90 |
| UA: Insertive with primary partners | 1.35 | 0.86–2.14 |
Note. MET = Motivational Enhancement Therapy; KC = Knowledge Check; RR = relative risk; CI = confidence interval.
Adjusted for measures that were unbalanced across treatment groups at baseline (see Table 1): sexual identity (bisexual vs. gay), hazardous drug use (Drug Abuse Screening Test [DAST] > 2), having any one-time partners.
In each analysis, indicators for 4-, 7-, and 10-month assessment points were inversely significantly associated with outcome, suggesting a decrease in behavior at follow-up relative to baseline levels.
Notably, changes in behavior over time were detected in each of the models. Indicators for the 4-, 7-, and 10month assessments points, compared to baseline, reveal that risk behavior was significantly lower at each of the follow-up points (all behaviors reported, all comparisons). For example, participants reported fewer nonprimary partners at the 10-month follow-up compared to baseline (RR = 0.48, 95% CI = 0.42–0.55). Again, this pattern held for each risk behavior represented in Table 2 at each follow-up assessment. There were no significant interactions (i.e., Treatment Group × Time), indicating that reductions in risk behavior occurred samplewide and were not associated with one treatment group relative to the other.
Secondary Outcomes–Risk Reduction Strategies
Finally, several risk reduction strategies were assessed as secondary outcomes including monogamy, negotiated safety relationships, using condoms for all anal sex occasions, and abstaining from anal sex (data not shown). At the 10-month follow-up, sexual behavior histories indicated that 15.9% of MET and 14.8% of KC participants were in a monogamous relationship (i.e., reports only one male partner with whom they had UA), whereas 16.0% and 15.9% of MET and KC, respectively, had a pattern of behavior consistent with a negotiated safety relationship (i.e., reported multiple partners but UA with only one partner). Nearly one third (31.8%) of MET and 23.5% of KC participants reported only condom-protected anal intercourse occasions, and an additional 19.7% of MET and 25.3% of KC participants abstained from anal intercourse—protected or unprotected occasions. Overall, 83.4% of MET and 79.6% of KC participants used one of these risk reduction strategies at the 10-month follow-up.
DISCUSSION
This study demonstrates that a brief, telephone-based intervention designed to allow high-risk MSM to “take stock” of their current sexual behaviors is an effective strategy for engaging MSM in prevention interventions. Although there were few between group differences found, it is notable that the one statistically significant finding revealed that MET participants engaged in greater unprotected anal receptive intercourse with their primary partners, compared to those in the KC group. This finding suggests that exposure to the MET intervention may have resulted in a behavioral strategy that reduced risks to their partners while potentially increasing risks to themselves. This speculative interpretation is consistent with past findings from brief risk reduction counseling interventions (11) and suggests the need for further research on patterns of change and behavioral substitution strategies following risk reduction interventions.
Our study found consistent evidence of risk reduction, including declines over time in the number of sex partners and frequencies of unprotected sex acts, particularly with regard to behaviors with nonprimary partners. The use of behavior strategies such as monogamy and negotiated safety agreements were also found to be prevalent (samplewide) at follow-up. In addition, positive changes in a variety of constructs theorized to mediate HIV-related risk behaviors were identified among both MET and KC participants. Although these results, documented via periodic assessments up to 10 months following enrollment, fail to endorse MET as a superior technique for achieving behavior change, they support the potential of brief behavioral interventions to act as effective catalysts for adopting safer sex behaviors and can therefore play a critical role in reducing risk.
There are several factors that may have contributed to these findings. The comparison condition in this trial may have had more potency than expected in this high-risk sample. The effects of measurement, or assessment effects (27,28), have long been discussed in the HIV prevention literature. Ironically, completion of both our SA and the interviewer-administered questionnaire satisfied a primary objective of our MET condition; this process afforded all of our participants the opportunity to “take stock” of their behaviors and attitudes. Interviewers and counselors alike reported anecdotal evidence that many participants commented that the assessments “made them think” about their behavior, and some commented that they “had not realized they were being so unsafe” in their behaviors. The inclusion of a no-treatment/no-contact control condition would have strengthened our study design and potentially enabled us to draw firmer conclusions about the impact of this intervention, particularly given the unexpected null results.
Our results also confirm that several key external “moderating” factors demand attention to facilitate sexual behavior. Specifically, substance use/abuse and depression were identified as two important correlates of unsafe sexual behavior yet are difficult to intervene with in the context of a brief intervention. In this regard, brief interventions may need to adopt a more formal role of diagnostic screening and strategize ways for those identified to receive effective services.
One important limitation of this study to consider is that, despite the implementation of study design features (e.g., telephone modality, anonymous participation option) meant to encourage participation by men who are not open about their sexual relations with men and men who are less acculturated in the gay community, only a small proportion of those enrolled reported female partners or a bisexual identity. Alliances with a variety of “trusted” community agencies may help broaden the appeal of these type of services among individuals with differing needs or concerns.
Nevertheless, the findings of the intervention trial reported here suggest that engaging individuals who may not otherwise seek traditional treatment settings and prevention programs is of critical importance and can potentially result in positive outcomes. Although our results are positive in the context of harm reduction principles (29)—a variety of risk reduction strategies were being used by more than three fourths of study participants at the final follow-up—the role of motivational interviewing techniques in effecting sexual risk behavior change with high-risk MSM is less certain. It may be that self-reflective assessments, client-centered services that provide objective information about HIV/AIDS, and acknowledgment of the individual’s goals and contextual factors influencing their risk can change HIV risk behavior to a degree sufficient enough to impact HIV transmission rates. Further research is needed to evaluate the impact of assessment (e.g., conduct a study that includes an assessment-free condition) as well as to identify the minimal necessary intervention elements needed to achieve public health meaningful reductions in HIV transmission risk behaviors among high-risk MSM.
Acknowledgments
This research was supported by the National Institutes of Mental Health grant RO1 MH062976. We thank Dr. Bob Wood and Frank Chaffee at Seattle King County Public Health for their insight and helpful suggestions, and our community collaborators at Gay City Health Project including Fred Swanson (executive director), and Luis Viquez and Brian Davis (counselors). We thank project staff for the dedication and skill they brought to this study, including Michael McKee (project coordinator), Josh Semerjian (enrollment and retention specialist), Jennifer Katz (assessor), Roberto Orellana (assessor and counselor), Shannon Carroll (outreach specialist), and Devon Bushnell (program coordinator), and many other staff members for their professionalism, energy, and enthusiasm. Finally, we especially appreciate our participants for their contributions to HIV prevention research.
Contributor Information
Joseph F. Picciano, School of Social Work, University of Washington
Roger A. Roffman, School of Social Work, University of Washington
Seth C. Kalichman, Department of Psychology, University of Connecticut
Denise D. Walker, School of Social Work, University of Washington
REFERENCES
- 1.Halkitis PN, Green KA, Remien RH, et al. Seroconcordant sexual partnerings of HIV-seropositive men who have sex with men. AIDS. 2005;19(Suppl. 1):S77–S86. doi: 10.1097/01.aids.0000167354.09912.83. [DOI] [PubMed] [Google Scholar]
- 2.Parsons JT, Schrimshaw EW, Bimbi DS, et al. Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositive gay and bisexual men. AIDS. 2005;19(Suppl. 1):S87–S97. doi: 10.1097/01.aids.0000167355.87041.63. [DOI] [PubMed] [Google Scholar]
- 3.Crawford JM, Rodden P, Kippax S, Van de Ven P. Negotiated safety and other agreements between men in relationships: Risk practice defined. International Journal of STD & AIDS. 2001;12:164–170. doi: 10.1258/0956462011916965. [DOI] [PubMed] [Google Scholar]
- 4.Davidovich U, de Wit JB, Stroebe W. Assessing sexual risk behaviour of young gay men in primary relationships: The incorporation of negotiated safety and negotiated safety compliance. AIDS. 2000;14:701–706. doi: 10.1097/00002030-200004140-00009. [DOI] [PubMed] [Google Scholar]
- 5.Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: A review of social, psychological, and medical findings. AIDS. 2002;16:135–149. doi: 10.1097/00002030-200201250-00002. [DOI] [PubMed] [Google Scholar]
- 6.Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: A meta-analysis. Psychological Bulletin. 1999;125:90–132. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- 7.Lightfoot M, Song J, Rotheram-Borus MJ, Newman P. The influence of partner type and risk status on the sexual behavior of young men who have sex with men living with HIV/AIDS. Journal of Acquired Immune Deficiency Syndromes. 2005;38:61–68. doi: 10.1097/00126334-200501010-00012. [DOI] [PubMed] [Google Scholar]
- 8.Kamb ML, Fishbein M, Douglas JM, Jr, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: A randomized controlled trial. Project RESPECT Study Group. Journal of the American Medical Association. 1998;280:1161–1167. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- 9.Belcher L, Kalichman S, Topping M, et al. A randomized trial of a brief HIV risk reduction counseling intervention for women. Journal of Consulting and Clinical Psychology. 1998;66:856–861. doi: 10.1037//0022-006x.66.5.856. [DOI] [PubMed] [Google Scholar]
- 10.Kalichman SC, Cain D, Weinhardt L, et al. Experimental components analysis of brief theory-based HIV/AIDS risk-reduction counseling for sexually transmitted infection patients. Health Psychology. 2005;24:198–208. doi: 10.1037/0278-6133.24.2.198. [DOI] [PubMed] [Google Scholar]
- 11.Patterson TL, Shaw WS, Semple SJ. Reducing the sexual risk behaviors of HIV+ individuals: Outcome of a randomized controlled trial. Annals of Behavioral Medicine. 2003;25:137–145. doi: 10.1207/S15324796ABM2502_10. [DOI] [PubMed] [Google Scholar]
- 12.Miller WR, Sovereign R, Krege B. Motivational interviewing with problem drinkers: II. The Drinker’s Check-up as a preventive intervention. Behavioural Psychotherapy. 1988;16:251–268. [Google Scholar]
- 13.Miller WR, Sovereign RG. The check-up: A model for early intervention in addictive behaviors. In: Loberg T, Miller WR, Nathan PE, Marlatt GA, editors. Addictive Behaviors: Prevention and Early Intervention. Amsterdam: Swets & Zeitlinger; 1989. pp. 219–231. [Google Scholar]
- 14.Picciano JF, Roffman RA, Kalichman SC, Rutledge SE, Berghuis JP. A telephone based brief intervention using motivational enhancement to facilitate HIV risk reduction among MSM: A pilot study. AIDS and Behavior. 2001;5:251–262. [Google Scholar]
- 15.McKee MB, Picciano JF, Roffman RA, Swanson F, Kalichman SC. Marketing the ‘Sex Check’: Evaluating recruitment strategies for a telephone-based HIV prevention project for gay and bisexual men. AIDS Education and Prevention. 2006;18:116–131. doi: 10.1521/aeap.2006.18.2.116. [DOI] [PubMed] [Google Scholar]
- 16.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychology Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 17.Carey MP, Maisto SA, Kalichman SC, et al. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals With Alcohol Abuse and Dependence. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. (Project MATCH Monograph Series, Vol. 2; DHHS Publication No. 92-1894). [Google Scholar]
- 19.Miller WR, Heather N, editors. Treating Addictive Behaviors: Processes of Change. 2nd Ed. New York: Plenum; 1998. [Google Scholar]
- 20.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. 2nd Ed. New York: Guilford; 2002. [Google Scholar]
- 21.Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1979;1:385–401. [Google Scholar]
- 23.Gavin DR, Ross HE, Skinner HA. Diagnostic validity of the Drug Abuse Screening Test in the assessment of DSM-III drug disorders. British Journal of Addiction. 1989;84:301–307. doi: 10.1111/j.1360-0443.1989.tb03463.x. [DOI] [PubMed] [Google Scholar]
- 24.Prochaska JO, Redding CA, Harlow LL, Rossi JS, Velicer WF. The transtheoretical model of change and HIV prevention: A review. Health Education Quarterly. 1994;21:471–486. doi: 10.1177/109019819402100410. [DOI] [PubMed] [Google Scholar]
- 25.StataCorp. Stata Statistical Software: Release 8. College Station, TX: STATACORP LP; 2001. [Google Scholar]
- 26.Glynn RJ, Buring JE. Ways of measuring rates of recurrent events. British Medical Journal. 1996;312:364–367. doi: 10.1136/bmj.312.7027.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roffman RA, Picciano JF, Ryan R, et al. HIV prevention group counseling delivered by telephone: An efficacy trial with gay and bisexual men. AIDS and Behavior. 1997;1:137–154. [Google Scholar]
- 28.Weinhardt LS, Carey KB, Carey MP. HIV risk sensitization following a detailed sexual behavior interview: A preliminary investigation. Journal of Behavioral Medicine. 2000;23:393–398. doi: 10.1023/a:1005505018784. [DOI] [PubMed] [Google Scholar]
- 29.Marlatt GA. Harm Reduction: Pragmatic Strategies for Managing High Risk Behaviors. New York: Guilford; 1998. [Google Scholar]