Abstract
Computed tomography-guided transthoracic lung biopsy is a common clinical procedure for the diagnosis of a broad range of pulmonary pathological conditions. Mild self-limiting pneumothorax and haemoptysis are common complications of this procedure. Air embolism is a potentially life-threatening but extremely rare complication. We report a case of an air embolism in the left ventricle of the heart that developed after a computed tomography-guided percutaneous needle biopsy of the lung. The patient did not exhibit cardiac or cerebral symptoms after conservative treatment. The patient underwent a successful left thoracotomy with a lobectomy of the left lower lobe of the lung 5 days after the biopsy and recovered uneventfully.
Keywords: CT-guided transthoracic lung biopsy, Air embolism
CASE REPORT
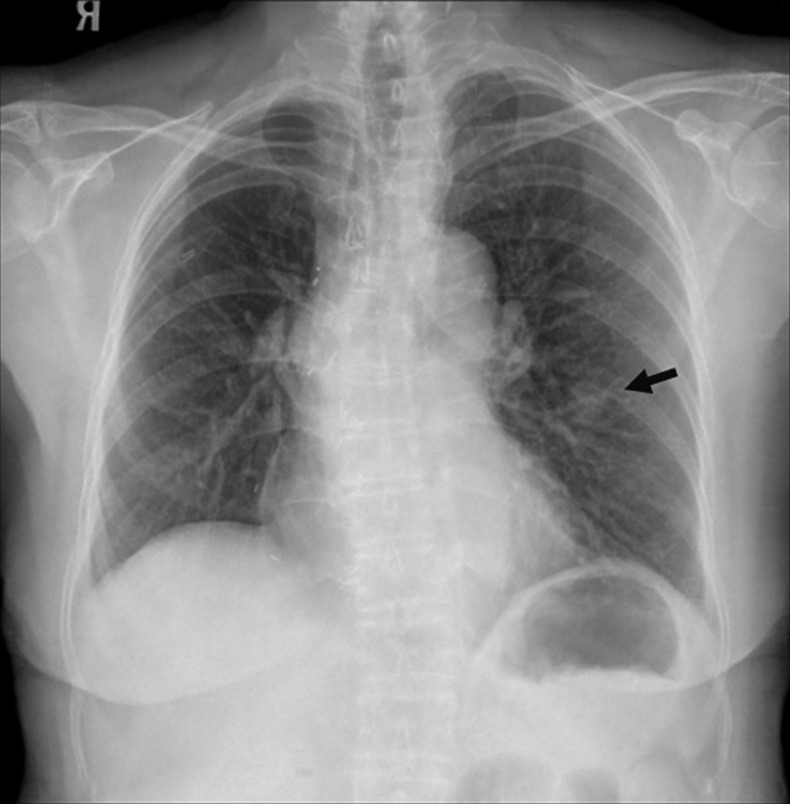
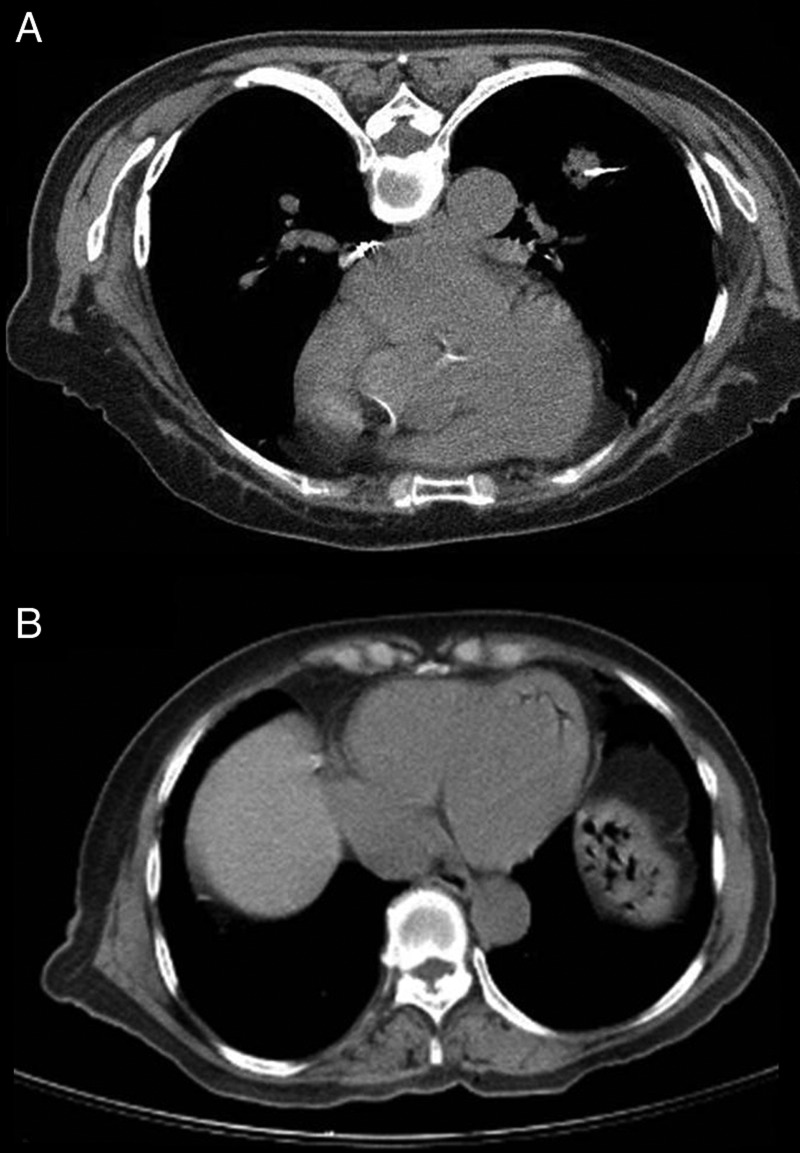
The patient had a 6-year history of a diffuse mucosa-associated lymphoid tissue (MALT)-type malignant B-cell lymphoma in the right upper lobe of the lung and underwent lobectomy. After operation, she did not regularly attend follow-up. One month before admission, she presented at our oncology outpatient department, where a chest X-ray showed a new nodule in the left lung field (Fig. 1). The patient was referred for a core needle biopsy of the left lung under the guidance of computed tomography (CT) for histopathological diagnosis. The patient was placed in the supine position and a 17-gauge coaxial needle system was used for the procedure. The needle biopsy was performed under CT/fluoroscopic guidance by an experienced radiologist (Fig. 2a) and one core biopsy sample was obtained. The patient did not cough or move during the procedure. After withdrawal of the needle, there was no obvious pneumothorax or parenchymal haemorrhage; however, an air embolism at the left ventricle was noted (Fig. 2b).
Figure 1:
A postero-anterior chest roentgenogram showing the new mass lesion.
Figure 2:
(A) Computed tomography of the chest: a core needle biopsy was performed under CT/fluoroscopic guidance. (B) Computed tomography image of the chest obtained after a CT-guided transthoracic lung biopsy showing air emboli in the left atrium.
The patient did not exhibit cardiac or cerebral symptoms. There was no air in the systemic circulation after echocardiography and CT of the brain. She was transferred to the intensive care unit for treatment with 100% oxygen. The air embolism resolved within 3 days without morbidity, during which time the patient was under close observation. Histopathological analysis revealed a MALT-type B-cell lymphoma. After 5 days, the patient underwent a left thoracotomy with lobectomy of the left lower lobe of the lung. Her postoperative recovery was uneventful.
DISCUSSION
CT-guided transthoracic lung biopsy is commonly performed for the diagnosis of pulmonary lesions. It is generally a safe method and the most common complication is pneumothorax, the incidence of which was 25% in lung biopsies performed in the USA [1] and 35% in lung biopsies performed in Japan [2]. Severe complications such as tumour seeding through the biopsy track, tension pneumothorax, pulmonary haemorrhage and systemic air embolism are rare, occurring in 0.75% of patients, 0.061% develop an air embolism, 0.1% develop haemothorax and 0.07% die from the sequelae of major complications [2]. Systemic air embolism is a rare but potentially threatening complication of CT-guided transthoracic lung biopsy. Its reported incidence is 0.07% [3], although its true incidence is considered to be higher because of underdiagnosis of asymptomatic patients [2, 4].
CT-guided transthoracic lung biopsies cause fewer systemic air embolisms than cardiac surgery, percutaneous coronary angiography, neurosurgical procedures in the upright position and barotrauma secondary to positive-pressure ventilation [5].
Mansour et al. [6] listed three ways whereby air can enter the systemic circulation during a needle biopsy of the lung. First, there is communication between the atmosphere and the pulmonary vein when the needle tip is placed within the pulmonary vein and the stylet has been removed. Secondly, when the needle passes through the lung parenchyma, a bronchovenous fistula may be created. There may be communication between intra-alveolar or intrabronchial air and the pulmonary vein when the airway pressure is elevated. Thirdly, air in the pulmonary arterial circulation may reach the pulmonary venous circulation by traversing the pulmonary microvasculature. We think that, in our patient, air was introduced into the pulmonary vein via the biopsy needle by negative intrathoracic pressure.
The application of positional therapy such as the Trendelenburg position or left lateral decubitus is controversial and may be more helpful for cases of shock induced by right ventricular air emboli, although some authors consider a flat supine position sufficient. Because the volume of gas in an enclosed space is inversely proportional to the pressure exerted on it, hyperbaric oxygen therapy reduces the size of air bubbles and accelerates the dissolution of nitrogen by replacing nitrogen with oxygen. However, conservative therapy consisting of inhalation of an atmosphere consisting of 100% oxygen resulted in a significant improvement within 4 h in an asymptomatic patient [4]. Our patient did not receive hyperbaric therapy but recovered from the near-fatal condition without any sequelae.
Several precautionary methods have been designed to minimize the risk of developing this fatal complication. Patients who are compliant should hold their breath when instructed and avoid coughing during the procedure. The needle should be inserted rapidly to prevent inadvertent ingress of air when the needle is open to the atmosphere. The opening should be closed immediately using the operator's finger or a biopsy needle. However, it should be remembered that this complication may occur even when excellent techniques are applied to a cooperative patient by an experienced, skillful operator. Awareness of this complication cannot be overemphasized; clinicians should be aware of the possible presence of systemic air and should be familiar with management techniques for dealing with this eventuality.
Conflict of interest: none declared.
REFERENCES
- 1.Richardson CM, Pointon KS, Manhire AR, Macfarlane JT. Percutaneous lung biopsies: a survey of UK practice based on 5444 biopsies. Br J Radiol. 2002;75:731–5. doi: 10.1259/bjr.75.897.750731. [DOI] [PubMed] [Google Scholar]
- 2.Tomiyama N, Yasuhara Y, Nakajima Y, Adachi S, Arai Y, Kusumoto M, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol. 2006;59:60–4. doi: 10.1016/j.ejrad.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Sinner WN. Complications of percutaneous transthoracic needle aspiration biopsy. Acta Radiol Diagn (Stockh) 1976;17:813–28. doi: 10.1177/028418517601700609. [DOI] [PubMed] [Google Scholar]
- 4.Hiraki T, Fujiwara H, Sakurai J, Iguchi T, Gobara H, Tajiri N, et al. Nonfatal systemic air embolism complicating percutaneous CT-guided transthoracic needle biopsy: four cases from a single institution. Chest. 2007;132:684–90. doi: 10.1378/chest.06-3030. [DOI] [PubMed] [Google Scholar]
- 5.Peirce EC. Cerebral gas embolism (arterial) with special reference to iatrogenic accidents. HBO Rev. 1980;1:161–84. [Google Scholar]
- 6.Mansour A, AbdelRaouf S, Qandeel M, Swaidan M. Acute coronary artery air embolism following CT-guided lung biopsy. Cardiovasc Intervent Radiol. 2005;28:131–4. doi: 10.1007/s00270-004-0118-1. [DOI] [PubMed] [Google Scholar]