Abstract
There are various surgical approaches to superior sulcus tumours according to the location of the tumour. The chief difficulties in the operation are broadening of the operative field and adhesiolysis. This study presents the case of surgical treatment of superior sulcus tumour following chemoradiation therapy with dense pleural adhesion due to a history of graft replacement of the descending thoracic aorta. The patient underwent left upper lobectomy via a transmanubrial osteomuscular-sparing approach combined with video-assisted thoracoscopic surgery (VATS). Transmanubrial approach combined with VATS offered a good overview during local tumour dissection.
Keywords: Superior sulcus tumours, Transmanubrial approach, Video-assisted thoracic surgery, Graft replacement of descending aorta, Dense pleural adhesion
INTRODUCTION
The surgical resection of superior sulcus tumours, also referred to as Pancoast tumours, remains a challenging surgical procedure. The combination of induction chemotherapy with local radiation followed by surgical resection has become an effective treatment strategy, resulting in high rates of complete resection and complete pathological response. After introduction of the multimodality therapy, local control and overall survival have improved [1–3]. The surgical standard for superior sulcus tumours is a radical en-bloc resection through an extended posterolateral thoracotomy [2]. A new anterior approach was reported by Dartevelle et al., who used a transclavicular approach [3]. Modifications to this technique were made by Grunenwald and Spaggiari [4], who described a transmanubrial osteomuscular-sparing approach. This study presents a patient with a superior sulcus tumour, who had a history of replacement of the descending thoracic aorta. He underwent resection of the tumour following a transmanubrial approach combined with video-assisted thoracic surgery lobectomy.
CASE REPORT
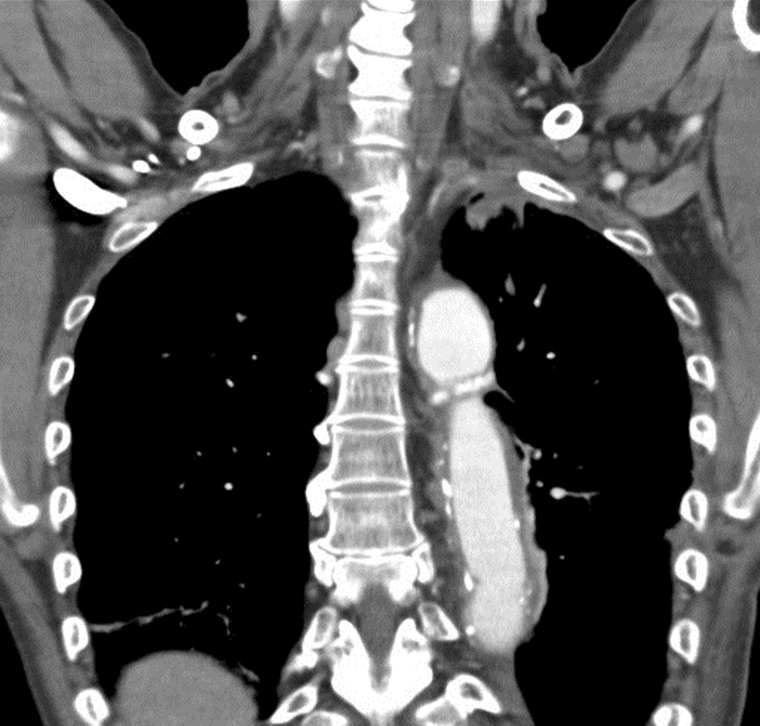
A 59-year old patient began to experience left shoulder pain since January 2010. In December 2009, he underwent replacement of the descending thoracic aorta for the treatment of a descending aortic aneurysm. Several medical examinations were conducted at a nearby hospital. Chest computed tomographic (CT) scan showed a superior sulcus tumour, which invaded the thoracic inlet at the anterior site, as well as the brachial plexus, and surrounded the subclavian artery (Fig. 1). Whole-body fluorodeoxyglucose–positron emission tomography showed no extrathoracic disease. The diagnosis of superior sulcus tumour in the left upper lobe was given.
Figure 1:
Chest computed tomography shows a superior sulcus tumour in the left upper lobe of the lung.
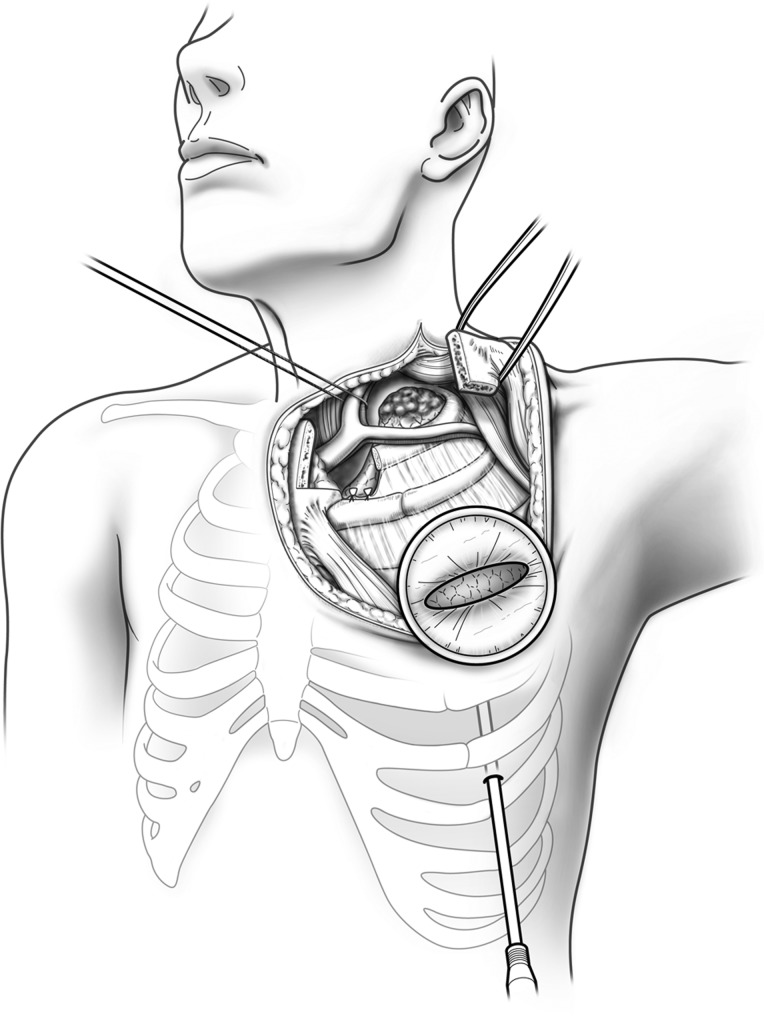
The patient was treated with five cycles of CDDP + MMC + vindesine concurrently with 45 Gy/25-fraction irradiation. The CT scan after induction chemoradiation revealed partial regression of the tumour (cT3N0M0, stage IIB). Surgical resection was scheduled 6 weeks after chemoradiation. Intraoperatively, the patient was placed in the supine position with double-lumen endotracheal tube for one-lung ventilation. First, we made an oblique neck incision along the anterior border of the left sternocleidomastoid muscle and a reverse L-shaped sternotomy, which was horizontally extended parallel to the left clavicle. A reverse L-shaped transmanubrial incision according to Grunenwald was performed with preservation of the sternoclavicular joint (Fig. 2). This allowed mobilization of an osteomuscular flap to the lateral border. Adhesion of the left subclavian artery to the tumour was minimal. Radical tumour resection with concomitant resection of surrounding tissue such as the T1 nerve roots of the brachial plexus, first rib and part of the left anterior scalene muscle was performed through this approach. Subsequently, left upper lobectomy was performed through video-assisted thoracoscopic surgery (VATS) procedure. The trocar for VATS lobectomy was inserted on the 6th intercostal space. The anterior L-shaped Grunenwald incision served as the second entrance. We did not need patient repositioning in this technique and could ablate hard adhesion by VATS. VATS also served for adhesiolysis between the prosthetic graft used to replace the descending aorta and surrounding tissue, especially the left lung. We dissected #2, #3a, #4, #5, #6 lymph nodes.
Figure 2:
Left transmanubrial approach. A wound retractor is inserted on the third intercostal space and a trocar on the sixth for VATS.
Macrospically, the tumour measured 2.9 × 2.0 × 0.9 cm. Definitive pathological examination of the specimen revealed a complete response with no vital tumour cells left. He had left lung atelectasis and phrenic nerve paralysis after surgery, but was discharged without any trouble. He had no recurrent signs and symptoms, including left shoulder pain.
DISCUSSION
Resection of superior sulcus tumours must be accompanied with lobectomy in order to be oncologically justified. One must also not be seduced into performing a smaller resection after a positive effect of chemoradiation on the tumour size because a small resection increases the risk of positive tumour margins.
In the surgical treatment of superior sulcus tumours, different surgical approaches exist [5]. In this case, the anterior approach reported by Gruenwald was chosen. If the tumour is situated in the anterior inlet, this approach offers a good overview during local tumour dissection [6]. A main disadvantage of this approach is that lobectomy can only be completed via the same incision in specific cases; therefore, additional thoracotomy is necessary to perform lobectomy [7]. In this case, the patient was suspected to have severe pleural adhesion around the descending thoracic aorta including the prosthetic graft after the graft replacement of the descending aorta, anterior transmanubrial approach was combined with VATS to complete the surgery of posterior vessel division and posterior pleural adhesiolysis.
The opening created by the anterior approach can be used as the utility incision of the VATS lobectomy. This incision provides enough space for the dissection with standard non-endoscopic instruments and for the removal of the specimen. Only one small additional incision is required to perform the posterior hilar division and posterior pleural adhesiolysis around the descending thoracic aorta including the prosthetic graft.
The VATS approach is especially useful for pulmonary hilar stripping and vessel division in superior sulcus tumours because pulmonary hilum and central pulmonary vessels is often not impaired due to chemoradiation [8]. Therefore, the lobectomy can be performed in a normal hilar anatomy.
If the thoracoscope is introduced during the operation, it is beneficial during the dissection of the tumour. The thoracoscope will help to determine the intercostal space through which the incision has to be made for the lobectomy. Furthermore, it is useful in spreading out the view and division of the adhesion after replacement of the descending thoracic aorta and chemoradiation therapy. The combined VATS approach enables us to perform safe vessel division despite severe posterior pleural adhesion.
On the other hand, if the tumour is situated in the posterior position, a high posterolateral thoracotomy is the classical approach. In this situation, a new entrance through an intercostal space must be made to perform the lobectomy. The VATS approach could also be of help to avoid extra intercostal incision, which can lead to increased morbidity.
CONCLUSION
The patient with a superior sulcus tumour after replacement of the descending thoracic aorta and neoadjuvant chemoradiation therapy was successfully treated.
He underwent left upper lobectomy with mediastinal lymph node dissection by the transmanubrial approach combined with VATS. The approach is indeed beneficial for this case with difficulty in surgical treatment only through the anterior approach such as posterior pleural adhesiolysis and inter-lobar fusion.
Conflict of interest: none declared.
REFERENCES
- 1.Rusch VW, Giroux DJ, Kraut MJ, Crowley J, Hazuka M, Winton T, et al. Induction chemoradiation and surgical resection for superior sulcus non-small-cell lung carcinomas: long-term results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160) J Clin Oncol. 2007;25:313–8. doi: 10.1200/JCO.2006.08.2826. [DOI] [PubMed] [Google Scholar]
- 2.Rusch VW. Management of pancoast tumours. Lancet Oncol. 2006;7:997–1005. doi: 10.1016/S1470-2045(06)70974-3. [DOI] [PubMed] [Google Scholar]
- 3.Marshall MB, Kucharczuk JC, Shrager JB, Kaiser LR. Anterior surgical approaches to the thoracic outlet. J Thorac Cardiovasc Surg. 2006;131:1255–60. doi: 10.1016/j.jtcvs.2006.01.044. [DOI] [PubMed] [Google Scholar]
- 4.Grunenwald D, Spaggiari L. Transmanubrial osteomuscular sparing approach for apical chest tumors. Ann Thorac Surg. 1997;63:563–6. doi: 10.1016/s0003-4975(96)01023-5. [DOI] [PubMed] [Google Scholar]
- 5.Matsuguma H, Nakahara R, Ishikawa Y, Suzuki H, Ui A, Yokoi K. Transmanubrial osteomuscular sparing approach for lung cancer invading the anterior part of the thoracic inlet. Gen Thorac Cardiovasc Surg. 2010;58:149–54. doi: 10.1007/s11748-009-0484-3. [DOI] [PubMed] [Google Scholar]
- 6.Di Rienzo G, Surrente C, Lopez C, Urgese AL. Transmanubrial osteomuscular sparing approach: different indications. Interact CardioVasc Thorac Surg. 2010;11:482–4. doi: 10.1510/icvts.2010.243238. [DOI] [PubMed] [Google Scholar]
- 7.Truin W, Siebenga J, Belgers E, Bollen EC. The role of video-assisted thoracic surgery in the surgical treatment of superior sulcus tumors. Interact CardioVasc Thorac Surg. 2010;11:512–4. doi: 10.1510/icvts.2010.237941. [DOI] [PubMed] [Google Scholar]