Abstract
Objective
To explore the reasons why long-term weight loss is seldom achieved and to evaluate the consequences of various weight trajectories, including stability, loss, and gain.
Quality of evidence
Studies evaluating population weight metrics were mainly observational. Level I evidence was available to evaluate the influence of weight interventions on mortality and quality of life.
Main message
Sustained weight loss is achieved by a small percentage of those intending to lose weight. Mortality is lowest in the high-normal and overweight range. The safest body-size trajectory is stable weight with optimization of physical and metabolic fitness. With weight loss there is evidence for lower mortality in those with obesity-related comorbidities. There is also evidence for improved health-related quality of life in obese individuals who lose weight. Weight loss in the healthy obese, however, is associated with increased mortality.
Conclusion
Weight loss is advisable only for those with obesity-related comorbidities. Healthy obese people wishing to lose weight should be informed that there might be associated risks. A strategy that leads to a stable body mass index with optimized physical and metabolic fitness at any size is the safest weight intervention option.
Statistics show that of those who contract the habit of eating, very few survive.
George Bernard Shaw
The genesis of humankind from primates in sub-Saharan Africa, along with the evolution of human form and function, was influenced greatly by the availability of high-quality energy in the food supply. As our ancestors migrated out of Africa, they settled in fertile areas to the north where the Agricultural Revolution developed, enabling fewer people to look after the nutritional needs of many. Ensuing food security promoted rapid development of urbanization,1 knowledge, and innovation. Agriculture enabled increased consumption of carbohydrates from cereals and legumes, and saturated fats from domestic meats and dairy. Overweight and obesity were uncommon.2
In the late 18th century, continued success of the species and continued nurturing of the human brain2,3 brought about the Industrial Revolution. It became possible to easily remove fibre and germ from cereals. Refined sugars became more available; latterly, high-fructose corn syrup became a staple in the Western diet, with adverse metabolic consequences.4,5 It became possible to extract oils from seeds, leading to a relative increase in omega-6 over omega-3 fatty acids in the diet, diminishing the anti-inflammatory benefits of the latter.5,6 Hydrogenation of these oils produced novel and highly atherogenic trans isomers, which had never been found in traditional diets.7 Apart from their metabolic consequences, these manipulations have increased caloric density in our foods and greatly reduced the physical activity required to procure those foods.
It is popularly hypothesized that some of us evolved genetically to efficiently hold on to calories in times of famine (the thrifty genotype8). This might have occurred by means of a quick insulin “trigger,” which minimizes the renal wasting of glucose and encourages uptake into cells, including adipocytes, leading to hyperinsulinemia, obesity, and diabetes. This genetic subtype conferred survival advantages in times of episodic famine, but primitive genes did not have time to adapt in the context of a plentiful food supply. Those most adapted to survive intermittent famine and hardship were now at a disadvantage, and an environment of abundant processed foods and inadequate exercise has led to increased body size and chronic disease.9
Quality of evidence
A PubMed search was initially done using MeSH terms or text words including obesity or overweight and mortality and weight loss or weight trajectory, restricted to the past 10 years and to reviews or meta-analyses. Recent evidence from observational studies was preferred because of better statistical control over confounding variables. References from appropriate retrieved papers were used to obtain other interventional studies, with preference given to larger controlled prospective cohort trials or randomized controlled trials. Additional searches were carried out to clarify the effects of covariates, such as diet, exercise, and quality of life. Level I studies were preferred, but because diet and exercise interventions present difficulties with blinding and compliance, level II studies were deemed acceptable (Table 1).
Table 1.
Levels of evidence
| LEVEL OF EVIDENCE | FEATURES | OUTCOME CONSIDERED | COMMENTS |
|---|---|---|---|
| Level I | At least 1 properly conducted RCT, systematic review, or meta-analysis | Mortality | 2 good meta-analyses, 2 systematic reviews, 2 reviews of prospective cohort studies |
| Morbidity (HRQOL) | Numerous RCTs and prospective clinical trials | ||
| Interventions in weight trajectory | One meta-analysis, several RCTs, numerous traditional reviews | ||
| Level II | Other comparison trials; non-randomized, cohort, case-control, or epidemiologic studies; and preferably more than 1 study | Population weight metrics | Primarily population-based longitudinal, prospective cohort, and cross-sectional studies |
| Level III | Expert opinion or consensus statements | NA | NA |
HRQOL—health-related quality of life, NA—not applicable, RCT—randomized controlled trial.
Main message
Classification and prevalence of body size
The most common measure of body size is the body mass index (BMI), defined as the weight in kilograms divided by the height in metres squared. In adults, overweight is defined as a BMI in the 25- to 30-kg/m2 range. Values above 30 kg/m2 constitute obesity (Table 2).10,11 Classification in children is expressed as a BMI percentile based on the Centers for Disease Control and Prevention 2000 BMI-for-age growth charts. Values for BMI between the 85th and 95th percentiles are deemed overweight, while those above the 95th percentile are considered obese.12
Table 2.
Prevalence of overweight and obesity in adults
| WEIGHT CATEGORY | BODY MASS INDEX, KG/M2 |
PREVALENCE, % |
|
|---|---|---|---|
| CANADA | UNITED STATES | ||
| Underweight | < 18.5 | NA | NA |
| Normal weight | 18.5–24.9 | NA | NA |
| Overweight | 25.0–29.9 | 34.1 | 35.0 |
| Obesity | 18.1 | 33.8 | |
| • Class 1 | 30.0–34.9 | ||
| • Class 2 | 35.0–39.9 | ||
| • Class 3 | ≥ 40.0 | ||
Rates of obesity and overweight are high among adults (Table 2)10,11 and children (Table 3)12 in both Canada and the United States. The rate of increase has moderated in both countries in the past several years.10–12 Educational interventions might have had some effect, but it also seems possible that our susceptible primitive gene pool is becoming saturated by the obesogenic effects of the current environment.
Table 3.
Prevalence of overweight and obesity in children
| WEIGHT CATEGORY | BODY MASS INDEX |
PREVALENCE, % |
|
|---|---|---|---|
| CANADA | UNITED STATES | ||
| Overweight | In the 85th to 95th percentile | 16.1 | 21.3 |
| Obese | Above the 95th percentile | 13.5 | 16.9 |
Data from Ogden et al.12
Body-weight trajectory
Cross-sectional analyses of healthy populations show, on average and without intervention, a gradual increase in body weight with increasing age, with a gradual slowing of this trend in the fifth to sixth decades.13 Weight-gain velocity is greatest in men younger than 40 years and in women younger than 50 years. Maximum weight is achieved on average between ages 50 and 69. Beyond age 70, some weight loss is more common.14 Averaging all age groups, BMI tends to increase by 1.5% per decade.14,15 In Canadians, this translates to between 0.25 and 0.50 kg per year,10 enough to move most individuals into a higher BMI category over a lifetime. A disproportionate amount of this weight gain is seen in the class 2 and 3 obesity categories16,17 defined in Table 2.10,11
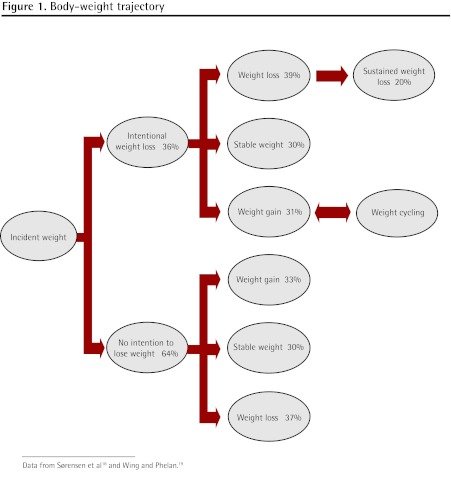
Sørensen et al,18 in a cross-sectional study of healthy adults, showed that at any given time, 36% of the population is attempting to lose weight, while 64% are taking no action to manage weight. Intervention in the weight trajectory, usually with diet and exercise, leads to weight loss, weight cycling with eventual gain, or weight stability. Remarkably, body-size outcomes are similar whether or not there is intention to lose weight—in both groups over the course of 6 years, 30% remain stable, 37% to 39% lose weight, and 31% to 33% cycle or gain weight (Figure 1).18,19
Figure 1.
Body-weight trajectory
Approximately 17% to 20% of overweight or obese people intentionally lose at least 10% of their body weight and maintain this loss for more than 1 year.19,20
Physiology underlying the weight trajectory
Recent increases in dietary caloric load and reduction in activity level produce an energy mismatch potentially leading to weight gain. Genetics might contribute 25% to 40% of weight-gain susceptibility21; however, the rapid increase in incidence of obesity suggests additional environmental causes, as genetic changes would take much more time.22
In an evolutionary sense, it seems likely that metabolic patterns would be preserved that resist depletion of energy stores in order to promote reproductive success and survival. It follows, therefore, that mechanisms would exist that resist a tendency to intentionally lose weight. Reduced lean body mass requires less energy intake. There is less physical effort required to move that reduced mass and diminished inclination to exercise,23,24 which further reduces energy requirements. There are other metabolic compensations. Ghrelin produced in the stomach increases with fasting, promoting return to previous weight.25 Leptin, a peptide produced in adipocytes, is instrumental in conserving weight under conditions of energy depletion.26,27 Levels drop, producing reduced resting energy expenditure by reducing sympathetic stimulation and increasing vagal activation. Vagal activity enhances insulin secretion, which drives fat back into cells and promotes energy storage.
In the obese state, levels of both insulin and leptin tend to be high, and leptin resistance is present,28,29 so that the mechanism to moderate body weight under conditions of energy repletion is ineffective. Obesity persists along with a state of hyperinsulinemia and continuing energy storage.
There has as yet been no identified mechanism of metabolic compensation to moderate body weight in the obese state. With intentional energy restriction and consumption by diet and exercise, both insulin and leptin levels drop and metabolic processes are initiated for return to original weight. A 10% weight loss can reduce resting energy expenditure by 15%.30 The obese individual who has lost this weight must then continue to diet and exercise even to stabilize at the lower weight,24 otherwise weight cycling occurs, with gradual gain in 80% of those originally attempting weight reduction. The 20% who are successful in maintaining weight loss might not have this marked metabolic compensation,31 and it might be easier for these individuals to maintain their loss over time.32
Optimal weight and the effect of weight trajectory on mortality (Table 4).10,14,33–50
Table 4.
| WEIGHT TRAJECTORY | UNDERWEIGHT | NORMAL WEIGHT | OVERWEIGHT |
OBESE |
ELDERLY | ||
|---|---|---|---|---|---|---|---|
| CLASS 1 | CLASS 2 | CLASS 3 | |||||
| Stable | Increased | Optimal | Optimal | Optimal | Increased | Increased | Optimal |
| Weight gain | Reduced | Optimal | Optimal | Increased | Increased | Increased | Optimal |
| Weight loss | |||||||
| • Intentional, healthy | Increased | Increased | Increased | Increased | Increased | Increased | Increased |
| • Intentional, morbidity | Increased | Increased | Increased | Reduced | Reduced | Reduced | Reduced |
| • Not intentional | Increased | Increased | Increased | Increased | Increased | Increased | Increased |
Optimal weight to minimize all-cause mortality is either in the high-normal range14,33 or in the overweight range, in both Canada and the United States.10,34,35 A recent systematic review including 40 observational cohort studies even suggests there is no increase in mortality for those with class 1 obesity.35 Mortality is also minimized if weight remains stable at any level throughout adult life.36,37
Underweight status is associated with increased mortality.35,38 Mortality tends to rise progressively with class 2 and 3 obesity.35,39–43 The relative association of mortality with increased weight tends to decline with age,39 perhaps in part because obesity-related deaths have already occurred by the time elderly status is reached.
Weight gain is generally associated with mortality, particularly if it is excessive.44–46 One systematic review suggests avoidance of weight gain (or loss) of more than 4% in order to minimize effect on mortality. The exception to this is in the late middle years and old age, where a modest weight gain might be protective in those not already overweight or obese.36
Early observational studies suggested an association between weight loss and increased mortality, although these findings were not uniform and the studies did not do a good job of controlling for intentionality and comorbidities. A recent meta-analysis47 confirmed an 11% increase in all-cause mortality in healthy subjects who experienced weight loss. The same study identified a 13% reduction in all-cause mortality if the intentional weight loss occurred in those with weight-related comorbidities. Uniformly, unintentional weight loss is associated with increased mortality.
There is generally little evidence to support weight loss for mortality reduction in healthy subjects older than 60 years.48 There might be some benefit in the elderly with comorbidities such as osteoarthritis, coronary artery disease, and diabetes.49,50 Mortality in this age group has been shown to increase if weight reduction is unintentional, exceeds 5%, or reduces BMI to less than 22 kg/m2.50
Although there has been concern that weight cycling might be associated with increased mortality, there is currently no consensus, with various reviews presenting different conclusions.38,51–54
Weight trajectory and morbidity
Health-related quality of life tends to be lower at both ends of the weight spectrum.55,56 For women it is optimized in the normal weight range, but for men and the elderly it is optimized in the overweight range.56
It is generally agreed that weight loss in obesity can improve health-related quality of life57–59; in fact, if both diet and exercise interventions are employed, weight loss might not be required.60 Improvements to both diet and exercise give additive benefit,61 and exercise can produce improvements at any weight.62–64 Self-evaluated health is often rated higher by individuals who are obese and active than by those who are inactive at normal weight.64 While it is clear that obesity-related health problems are improved by weight interventions, there is disagreement as to whether there are psychological health benefits.
Intervening in the weight trajectory
While there is evidence for improved quality of life among obese patients who have lost weight, there is no evidence for mortality benefit unless there is weight-related comorbidity. Such comorbidity is common in class 1 to 3 obesity, affecting between 70% and 82% of individuals in these groups, depending on obesity severity.65 However, meta-analyses of the best cohort studies suggest that in other weight categories mortality increases with weight loss in otherwise healthy people (Table 4).10,14,33–50
The first priority is to stop excessive weight gain in children through behaviour modification, environmental change, reduction of dietary caloric density, and increased exercise (Table 5).66–68 Similar changes need to be applied for most adults to prevent the usual trajectory of gradual weight gain.
Table 5.
Measures for prevention of excess childhood weight gain
| INTERVENTION | RECOMMENDATION |
|---|---|
| Fruits and vegetables | ≥ 5 servings per day |
| Sugars and sugar-sweetened beverages | Minimize or eliminate (including soft drinks and juices) |
| Breakfast | Eaten every day |
| Family meals | 5–6 per week minimum |
| Meals outside the home | Minimize; no “fast foods” |
| Food insecurity | Eliminate67 |
| Food portions | Self-regulated by child |
| Physical activity | ≥ 1 hour per day |
| Sleep time | > 11.5 hours at 5–6 years of age68 |
| Screen time | No exposure younger than 2 years of age; 1–2 hours per day after 2 years of age; no television or video games in bedroom |
Data from Spear et al.66
Dietary calorie restriction and compliance are the prominent issues for those attempting weight loss, as results tend to be similar despite manipulation of specific carbohydrate, fat, and protein macronutrients.69 The low-carbohydrate diet is most effective in moderating cardiac risk factors, and the Mediterranean diet provides the maximum benefit for glycemic control. Both tend to be superior to the low-fat diet in affecting these secondary end points.70 Several large prospective cohort studies, however, have raised concerns about increased long-term mortality with the low-carbohydrate diet.71–73 The Mediterranean diet is currently the only intervention consistently associated with reduced mortality.74–76
Exercise is particularly useful in ongoing weight maintenance77,78 and modification of cardiovascular risk factors.79–81 The particularly harmful inflammatory effects of visceral obesity and metabolic syndrome are substantially moderated by exercise.82,83 Ongoing social and environmental change will be necessary to make healthy food choices more available and to increase opportunities for exercise leading to aerobic fitness.21,84
There are some indications for planned weight loss (Table 6), and any strategy should involve thorough examination of harms and possible benefits, along with realistic appreciation of prospects for success. Because compliance is among the most important variables in weight intervention,69 and because the change needs to be lifelong, it is important to consult with the patient to craft a strategy that is likely to be followed. Weight loss, however, need not be a prerequisite to better health. Improved physical fitness, reduction of highly metabolically active abdominal fat, and improvement of cardiovascular risk factors can happen equally well at a stable elevated weight with a commitment to healthier food choices and appropriate exercise.80,82,85–88
Table 6.
Possible indications for intentional weight loss
| INDICATION | EXAMPLES |
|---|---|
| Personal choice | Esthetics Beliefs and values Quality of life |
| Weight-related comorbidity | Coronary artery disease Diabetes Metabolic syndrome Knee osteoarthritis Obstructive sleep apnea Nonalcoholic fatty liver disease |
| Improved quality of life | Relief of symptoms Improved cardiovascular risk Improved self-image |
Conclusion
Prescribed weight loss as a target for all-cause mortality reduction among the overweight and healthy obese is a failed concept both in terms of evidence for benefit and in terms of implementation. Weight reduction among obese individuals with comorbidities or diminished weight-related quality of life can be of demonstrated benefit. In all cases, the aim should be to avoid initial weight gain, prevent ongoing weight gain, and realize physical and metabolic fitness at any size.
KEY POINTS
Obesity and overweight are more common than “normal” weight in our society. Weight gain averages 0.25 to 0.50 kg per year. Metabolic pathways exist that resist intentional weight loss and that tend to return body mass to the obese state. Weight loss might increase mortality among the healthy obese. Mortality is actually minimized with body mass in the high-normal or overweight range, and the safest body-mass trajectory is weight stabilization with no further gain and optimized physical and metabolic fitness at any size. Initial and continuing weight gain must be avoided through mitigation of the toxic effects of poor diet and low physical activity levels common in our current environment.
Footnotes
This article has been peer reviewed.
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de mai 2012 à la page e246.
Competing interests
None declared
References
- 1.Homer-Dixon T. The upside of down: catastrophe, creativity, and the renewal of civilization. Toronto, ON: Knopf Canada; 2006. [Google Scholar]
- 2.Pijl H. Obesity: evolution of a symptom of affluence. How food has shaped our existence. Neth J Med. 2004;69(4):159–66. [PubMed] [Google Scholar]
- 3.Broadhurst CL, Cunnane SC, Crawford MA. Rift Valley lake fish and shellfish provided brain-specific nutrition for early Homo. Br J Nutr. 1998;79(1):3–21. doi: 10.1079/bjn19980004. [DOI] [PubMed] [Google Scholar]
- 4.Basciano H, Federico L, Adeli K. Fructose, insulin resistance, and metabolic dyslipidemia. Nutr Metab (Lond) 2005;2(1):5. doi: 10.1186/1743-7075-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tappy L, Lê KA. Metabolic effects of fructose and the worldwide increase in obesity. Physiol Rev. 2010;90(1):23–46. doi: 10.1152/physrev.00019.2009. [DOI] [PubMed] [Google Scholar]
- 6.Hibbeln JR, Nieminen LR, Blasbalg TL, Riggs JA, Lands WE. Healthy intakes of n-3 and n-6 fatty acids: estimations considering worldwide diversity. Am J Clin Nutr. 2006;83(6 Suppl):1483S–93S. doi: 10.1093/ajcn/83.6.1483S. [DOI] [PubMed] [Google Scholar]
- 7.Simopoulos AP. Evolutionary aspects of diet, the omega-6/omega-3 ratio and genetic variation: nutritional implications for chronic diseases. Biomed Pharmacother. 2006;60(9):502–7. doi: 10.1016/j.biopha.2006.07.080. Epub 2006 Aug 28. [DOI] [PubMed] [Google Scholar]
- 8.Neel JV, Weder AB, Julius S. Type II diabetes, essential hypertension, and obesity as “syndromes of impaired genetic homeostasis”: the “thrifty genotype” hypothesis enters the 21st century. Perspect Biol Med. 1998;42(1):44–74. doi: 10.1353/pbm.1998.0060. [DOI] [PubMed] [Google Scholar]
- 9.Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, et al. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005;81(2):341–54. doi: 10.1093/ajcn.81.2.341. [DOI] [PubMed] [Google Scholar]
- 10.Orpana HM, Tremblay MS, Fines P. Trends in weight change among Canadian adults: evidence from the 1996/1997 to 2004/2005 National Population Health Survey. Ottawa, ON: Statistics Canada; 2006. Available from: www.statcan.gc.ca/pub/82-618-m/82-618-m2006005-eng.htm. Accessed 2011 Nov 3. [PubMed] [Google Scholar]
- 11.Public Health Agency of Canada, Canadian Institute for Health Information . Obesity in Canada. A joint report from the Public Health Agency of Canada and the Canadian Institute for Health Information. Ottawa, ON: Canadian Institute for Health Information; 2011. Available from: http://secure.cihi.ca/cihiweb/products/Obesity_in_canada_2011_en.pdf. Accessed 2011 Nov 3. [Google Scholar]
- 12.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–9. doi: 10.1001/jama.2009.2012. Epub 2010 Jan 13. [DOI] [PubMed] [Google Scholar]
- 13.Østbye T, Malhotra R, Landerman LR. Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 cohort (1981–2006) Int J Epidemiol. 2011;40(1):240–50. doi: 10.1093/ije/dyq142. Epub 2010 Sep 5. [DOI] [PubMed] [Google Scholar]
- 14.Prospective Studies Collaboration. Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. doi: 10.1016/S0140-6736(09)60318-4. Epub 2009 Mar 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shah M, Hannan PJ, Jeffery RW. Secular trend of body mass index in the adult population of three communities in the upper mid-western part of the USA: the Minnesota Heart Health Program. Int J Obes. 1991;15(8):499–503. [PubMed] [Google Scholar]
- 16.Penman AD, Johnson WD. The changing shape of the body mass index distribution curve in the population: implications for public health policy to reduce the incidence of adult obesity. Prev Chronic Dis. 2006;3(3):1–4. Available from: www.cdc.gov/pcd/issues/2006/jul/05_0232.htm. Accessed 2011 Nov 5. [PMC free article] [PubMed] [Google Scholar]
- 17.Orpana HM, Berthelot JM, Kaplan MS, Feeney DH, McFarland B, Ross NA. BMI and mortality: results from a national longitudinal study of Canadian adults. Obesity (Silver Spring) 2010;18(1):214–8. doi: 10.1038/oby.2009.191. Epub 2009 Jun 18. [DOI] [PubMed] [Google Scholar]
- 18.Sørensen TI, Rissanen A, Korkeila M, Kaprio J. Intention to lose weight, weight changes, and 18-y mortality in overweight individuals without comorbidities. PLoS Med. 2005;2(6):e171. doi: 10.1371/journal.pmed.0020171. Epub 2005 Jun 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 Suppl):222S–5S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- 20.Kraschnewski JL, Boan J, Esposito J, Sherwood NE, Lehman EB, Kephart DK, et al. Long-term weight loss maintenance in the United States. Int J Obes (Lond) 2010;34(11):1644–54. doi: 10.1038/ijo.2010.94. Epub 2010 May 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wadden TA, Foster GD, Brownell KD. Obesity: responding to the global epidemic. J Consult Clin Psychol. 2002;70(3):510–25. doi: 10.1037//0022-006x.70.3.510. [DOI] [PubMed] [Google Scholar]
- 22.Rosenbaum M, Nicolson M, Hirsch J, Murphy E, Chu F, Leibel RL. Effects of weight change on plasma leptin concentrations and energy expenditure. J Clin Endocrinol Metab. 1997;82(11):3647–54. doi: 10.1210/jcem.82.11.4390. [DOI] [PubMed] [Google Scholar]
- 23.De Groot LC, van Es AJ, van Raaij JM, Vogt JE, Hautvast JG. Adaptation of energy metabolism of overweight women to alternating and continuous low energy intake. Am J Clin Nutr. 1989;50(6):1314–23. doi: 10.1093/ajcn/50.6.1314. [DOI] [PubMed] [Google Scholar]
- 24.Maclean PS, Bergouignan A, Cornier MA, Jackman MR. Biology’s response to dieting: the impetus for weight gain. Am J Physiol Regul Integr Comp Physiol. 2011;301(3):R581–600. doi: 10.1152/ajpregu.00755.2010. Epub 2011 Jun 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cummings DE, Wiegle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346(21):1623–30. doi: 10.1056/NEJMoa012908. [DOI] [PubMed] [Google Scholar]
- 26.Kelesidis T, Kelesidis I, Chou S, Mantzoros CS. Narrative review: the role of leptin in human physiology: emerging clinical applications. Ann Intern Med. 2010;152(2):93–100. doi: 10.1059/0003-4819-152-2-201001190-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldsmith R, Joanisse DR, Gallagher D, Pavlovich K, Shamoon E, Leibel RL, et al. Effects of experimental weight perturbation on skeletal muscle work efficiency, fuel utilization, and biochemistry in human subjects. Am J Physiol Regul Integr Comp Physiol. 2010;298(1):R79–88. doi: 10.1152/ajpregu.00053.2009. Epub 2009 Nov 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morrison CD, Huypens P, Stewart LK, Gettys TW. Implications of crosstalk between leptin and insulin signalling during the development of diet induced obesity. Biochim Biophys Acta. 2009;1792(5):409–16. doi: 10.1016/j.bbadis.2008.09.005. Epub 2008 Sep 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reinehr T, Kleber M, de Sousa G, Andler W. Leptin concentrations are a predictor of overweight reduction in a lifestyle intervention. Int J Pediatr Obes. 2009;4(4):215–23. doi: 10.3109/17477160902952464. [DOI] [PubMed] [Google Scholar]
- 30.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med. 1995;332(10):621–8. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 31.Wyatt HR, Grunwald GK, Seagle HM, Klem ML, McGuire MT, Wing RR, et al. Resting energy expenditure in reduced-obese subjects in the National Weight Control Registry. Am J Clin Nutr. 1999;69(6):1189–93. doi: 10.1093/ajcn/69.6.1189. [DOI] [PubMed] [Google Scholar]
- 32.Klem ML, Wing RR, Lang W, McGuire MT, Hill JO. Does weight loss maintenance become easier over time? Obes Res. 2000;8(6):438–44. doi: 10.1038/oby.2000.54. [DOI] [PubMed] [Google Scholar]
- 33.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 34.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. Epub 2010 Jan 13. [DOI] [PubMed] [Google Scholar]
- 35.Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666–78. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 36.Strandberg TE, Strandberg AY, Salomaa VV, Pitkälä KH, Tilvis RS, Sirola J, et al. Explaining the obesity paradox: cardiovascular risk, weight change, and mortality during long-term follow-up in men. Eur Heart J. 2009;30(14):1720–7. doi: 10.1093/eurheartj/ehp162. Epub 2009 May 9. [DOI] [PubMed] [Google Scholar]
- 37.Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, et al. Body weight and mortality among women. N Engl J Med. 1995;333(11):677–85. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- 38.Arnold AM, Newman AB, Cushman M, Ding J, Kritchevsky S. Body weight dynamics and their association with physical function and mortality in older adults: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 2010;65(1):63–70. doi: 10.1093/gerona/glp050. Epub 2009 Apr 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL. The effect of age on the association between body-mass index and mortality. N Engl J Med. 1998;338(1):1–7. doi: 10.1056/NEJM199801013380101. [DOI] [PubMed] [Google Scholar]
- 40.Wee CC, Huskey KW, Ngo LH, Fowler-Brown A, Leveille SG, Mittlemen MA, et al. Obesity, race, and risk for death or functional decline among Medicare beneficiaries. Ann Intern Med. 2011;154(10):645–55. doi: 10.7326/0003-4819-154-10-201105170-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L, et al. Obesity in adulthood and its consequences for life expectancy: a life table analysis. Ann Intern Med. 2003;138(1):24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 42.Maru S, van der Schouw YT, Gimbrère CH, Grobbee DE, Peeters PH. Body mass index and short-term weight change in relation to mortality in Dutch women after age 50 y. Am J Clin Nutr. 2004;80(1):231–6. doi: 10.1093/ajcn/80.1.231. [DOI] [PubMed] [Google Scholar]
- 43.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 44.Yaari S, Goldbourt U. Voluntary and involuntary weight loss: associations with long term mortality in 9,228 middle-aged and elderly men. Am J Epidemiol. 1998;148(6):546–55. doi: 10.1093/oxfordjournals.aje.a009680. [DOI] [PubMed] [Google Scholar]
- 45.Andres R, Muller DC, Sorkin JD. Long-term effects of change in body weight on all-cause mortality. A review. Ann Intern Med. 1993;119(7 Pt 2):737–43. doi: 10.7326/0003-4819-119-7_part_2-199310011-00022. [DOI] [PubMed] [Google Scholar]
- 46.Pérez Morales ME, Jiménez Cruz A, Bacardí Gascón M. The effect of weight loss on mortality: a systematic review from 2000 to 2009 [article in Spanish] Nutr Hosp. 2010;25(5):718–24. [PubMed] [Google Scholar]
- 47.Harrington M, Gibson S, Cottrell RC. A review and meta-analysis of the effect of weight loss on all-cause mortality risk. Nutr Res Rev. 2009;22(1):93–108. doi: 10.1017/S0954422409990035. [DOI] [PubMed] [Google Scholar]
- 48.Witham MD, Avenell A. Interventions to achieve long-term weight loss in obese older people: a systematic review and meta-analysis. Age Ageing. 2010;39(2):176–84. doi: 10.1093/ageing/afp251. Epub 2010 Jan 18. [DOI] [PubMed] [Google Scholar]
- 49.Bales CW, Buhr G. Is obesity bad for older persons? A systematic review of the pros and cons of weight reduction in later life. J Am Med Dir Assoc. 2008;9(5):302–12. doi: 10.1016/j.jamda.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 50.Chapman IM. Weight loss in older persons. Med Clin North Am. 2011;95(3):579–93. doi: 10.1016/j.mcna.2011.02.004. Epub 2011 Mar 26. [DOI] [PubMed] [Google Scholar]
- 51.Weight cycling. National Task Force on the Prevention and Treatment of Obesity. JAMA. 1994;272(15):1196–202. [PubMed] [Google Scholar]
- 52.Muls E, Kempen K, Vansant G, Saris W. Is weight cycling detrimental to health? A review of the literature in humans. Int J Obes Relat Metab Disord. 1995;19(Suppl 3):S46–50. [PubMed] [Google Scholar]
- 53.Williamson DF. “Weight cycling” and mortality: how do the epidemiologists explain the role of intentional weight loss? J Am Coll Nutr. 1996;15(1):6–13. doi: 10.1080/07315724.1996.10718559. [DOI] [PubMed] [Google Scholar]
- 54.Jeffery RW. Does weight cycling present a health risk? Am J Clin Nutr. 1996;63(3 Suppl):452S–5S. doi: 10.1093/ajcn/63.3.452. [DOI] [PubMed] [Google Scholar]
- 55.Garner RE, Feeny DH, Thompson A, Bernier J, McFarland BH, Huguet N, et al. Bodyweight, gender, and quality of life: a population-based longitudinal study. Qual Life Res. 2011 Aug 13; doi: 10.1007/s11136-011-9989-1. Epub ahead of print. Erratum in: Qual Life Res 2011 Dec 1. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Imai K, Gregg EW, Chen YJ, Zhang P, de Rekeneire N, Williamson DF. The association of BMI with functional status and self-rated health in US adults. Obesity (Silver Spring) 2008;16(2):402–8. doi: 10.1038/oby.2007.70. [DOI] [PubMed] [Google Scholar]
- 57.Engel SG, Crosby RD, Kolotkin RL, Hartley GG, Williams GR, Wonderlich SA, et al. Impact of weight loss and regain on quality of life: mirror image or differential effect? Obes Res. 2003;11(10):1207–13. doi: 10.1038/oby.2003.166. [DOI] [PubMed] [Google Scholar]
- 58.Kolotkin RL, Crosby RD, Williams GR, Hartley GG, Nicol S. The relationship between health-related quality of life and weight loss. Obes Res. 2001;9(9):564–71. doi: 10.1038/oby.2001.73. [DOI] [PubMed] [Google Scholar]
- 59.Maciejewski ML, Patrick DL, Williamson DF. A structured review of randomized controlled trials of weight loss showed little improvement in health-related quality of life. J Clin Epidemiol. 2005;58(6):568–78. doi: 10.1016/j.jclinepi.2004.10.015. Epub 2005 Apr 18. [DOI] [PubMed] [Google Scholar]
- 60.Blissmer B, Riebe D, Dye G, Ruggiero L, Greene G, Caldwell M. Health-related quality of life following a clinical weight loss intervention among overweight and obese adults: intervention and 24 month follow-up effects. Health Qual Life Outcomes. 2006;4:43. doi: 10.1186/1477-7525-4-43. Available from: www.hqlo.com/content/4/1/43. Accessed 2011 Nov 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Imayama I, Alfano CM, Kong A, Foster-Schubert KE, Bain CE, Xiao L, et al. Dietary weight loss and exercise interventions effects on quality of life in overweight/obese postmenopausal women: a randomized controlled trial. Int J Behav Nutr Phys Act. 2011;8:118. doi: 10.1186/1479-5868-8-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Blair SN, Church TS. The fitness, obesity and health equation: is physical activity the common denominator? JAMA. 2004;292(10):1232–4. doi: 10.1001/jama.292.10.1232. [DOI] [PubMed] [Google Scholar]
- 63.Martin CK, Church TS, Thompson AM, Earnest CP, Blair SN. Exercise dose and quality of life: results of a randomized controlled trial. Arch Intern Med. 2009;169(3):269–78. doi: 10.1001/archinternmed.2008.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Herman KM, Hopman WM, VanDenKerkhof EG, Rosenberg MW. Physical activity, body mass index, and health-related quality of life in Canadian adults. Med Sci Sports Exerc. 2011. Oct 1, Epub ahead of print. Available from: http://journals.lww.com/acsm-msse/pages/articleviewer.aspx?year=9000&issue=00000&article=98820&type=abstract. Accessed 2011 Nov 22. [DOI] [PubMed]
- 65.Padwal RS, Pajewski NM, Allison DB, Sharma AM. Using the Edmonton Obesity Staging System to predict mortality in a population-representative cohort of people with overweight and obesity. CMAJ. 2011;183(14):E1059–66. doi: 10.1503/cmaj.110387. Epub 2011 Aug 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Spear BA, Barlow SE, Ervin C, Ludwig DS, Saelens BE, Schetzina KE, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S254–88. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- 67.Eisenmann JC, Gundersen C, Lohman BJ, Garasky S, Stewart SD. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obes Rev. 2011;12(5):e73–83. doi: 10.1111/j.1467-789X.2010.00820.x. Epub 2011 Mar 8. [DOI] [PubMed] [Google Scholar]
- 68.Von Kries R, Toschke AM, Wurmser H, Sauerwald T, Koletzko B. Reduced risk for overweight and obesity in 5- and 6-y-old children by duration of sleep—a cross-sectional study. Int J Obes Relat Metab Disord. 2002;26(5):710–6. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 69.Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein and carbohydrates. N Engl J Med. 2009;360(9):859–73. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shai I, Schwarzfuchs D, Henkin Y, Shahar RD, Witkow S, Greenberg I, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359(3):229–41. doi: 10.1056/NEJMoa0708681. Erratum in: N Engl J Med 2009;361(27):2681. [DOI] [PubMed] [Google Scholar]
- 71.Trichopoulou A, Psaltopoulou T, Orfanos P, Hsieh CC, Trichopoulos D. Low-carbohydrate-high-protein diet and long term survival in a general population cohort. Eur J Clin Nutr. 2007;61(5):575–81. doi: 10.1038/sj.ejcn.1602557. Epub 2006 Nov 29. [DOI] [PubMed] [Google Scholar]
- 72.Lagiou P, Sandin S, Weiderpass E, Lagiou A, Mucci L, Trichopoulos D, et al. Low carbohydrate-high protein diet and mortality in a cohort of Swedish women. J Intern Med. 2007;261(4):366–74. doi: 10.1111/j.1365-2796.2007.01774.x. [DOI] [PubMed] [Google Scholar]
- 73.Fung TT, van Dam RM, Hankinson SE, Stampfer M, Willett WC, Hu FB. Low-carbohydrate diets and all-cause and cause-specific mortality: two cohort studies. Ann Intern Med. 2010;153(5):289–98. doi: 10.1059/0003-4819-153-5-201009070-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Knoops KT, deGroot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women. JAMA. 2004;292(12):1433–9. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 75.Trichopoulou A, Bamia C, Trichopoulos D. Anatomy of health effects of Mediterranean diet: Greek EPIC prospective cohort study. BMJ. 2009;338:b2337. doi: 10.1136/bmj.b2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sofi F, Cesari F, Abbate R, Gensini GF, Casini A. Adherence to Mediterranean diet and health status: meta-analysis. BMJ. 2008;337:a1344. doi: 10.1136/bmj.a1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Schaar B, Moos-Thiele C, Platen P. Effects of exercise, diet, and a combination of exercise and diet in overweight and obese adults—a meta-analysis of the data. Open Sports Med J. 2010;4:17–28. [Google Scholar]
- 78.Ross R, Janssen I, Dawson J, Kungl A, Kuk J, Wong SL, et al. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res. 2004;12(5):789–98. doi: 10.1038/oby.2004.95. [DOI] [PubMed] [Google Scholar]
- 79.Goodpaster BH, DeLany JP, Otto AD, Kuller L, Vockley J, South-Paul JE, et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA. 2010;304(16):1795–802. doi: 10.1001/jama.2010.1505. Epub 2010 Oct 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ross R, Janiszewski PM. Is weight loss the optimal target for obesity-related cardiovascular disease reduction? Can J Cardiol. 2008;24(Suppl D):25D–31D. doi: 10.1016/s0828-282x(08)71046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ross R, Bradshaw AJ. The future of obesity reduction: beyond weight loss. Nat Rev Endocrinol. 2009;5(6):319–25. doi: 10.1038/nrendo.2009.78. [DOI] [PubMed] [Google Scholar]
- 82.Hainer V, Toplak H, Stich V. Fit or fat: what is more important? Diabetes Care. 2009;32(Suppl 2):S392–7. doi: 10.2337/dc09-S346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Irwin ML, Yasui Y, Ulrich CM, Bowen D, Rudolph RE, Schwartz RS, et al. Effect of exercise on total and intra-abdominal body fat in postmenopausal women: a randomized controlled trial. JAMA. 2003;289(3):323–30. doi: 10.1001/jama.289.3.323. [DOI] [PubMed] [Google Scholar]
- 84.Hill JO. Understanding and addressing the epidemic of obesity: an energy balance perspective. Endocr Rev. 2006;27(7):750–61. doi: 10.1210/er.2006-0032. Epub 2006 Nov 22. [DOI] [PubMed] [Google Scholar]
- 85.Nicklas BJ, Wang X, You T, Lyles MF, Demons J, Easter L, et al. Effect of exercise intensity on abdominal fat loss during calorie restriction in overweight and obese postmenopausal women: a randomized, controlled trial. Am J Clin Nutr. 2009;89(4):1043–52. doi: 10.3945/ajcn.2008.26938. Epub 2009 Feb 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Robison J, Putnam K, McKibbin L. Health at every size: a compassionate effective approach for helping individuals with weight-related concerns—part I. AAOHN J. 2007;55(4):143–50. doi: 10.1177/216507990705500402. [DOI] [PubMed] [Google Scholar]
- 87.Bacon L, Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutr J. 2011;10:9. doi: 10.1186/1475-2891-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Heini A. Contraindications to weight reduction [article in German] Ther Umsch. 2000;57(8):537–41. doi: 10.1024/0040-5930.57.8.537. [DOI] [PubMed] [Google Scholar]