Abstract
Purpose
The objective of this retrospective cohort study was to assess the long-term outcome of cementless femoral reconstruction in patients with previous intertrochanteric osteotomy (ITO).
Methods
We evaluated the clinical and radiographic results of a consecutive series of 45 patients (48 hips, mean age 50 years) who had undergone conversion hip replacement following ITO with a cementless, grit-blasted, double-tapered femoral component. Clinical outcome was determined using the Harris hip score. Stem survival for different end points was assessed using Kaplan-Meier survivorship analysis.
Results
At a mean follow-up of 20 (range, 16–24) years, 11 patients (12 hips) had died, and no patient was lost to follow-up. Six patients (six hips) underwent femoral revision, two for infection, three for aseptic loosening and one for periprosthetic fracture. Mean Harris hip score at final follow-up was 78 points (range, 23–100 points). Stem survival for all revisions was 89% (95%CI, 75–95) at 20 years, and survival for aseptic loosening was 93% (95%CI, 80–98).
Conclusions
The long-term results with this type of cementless femoral component in patients with previous intertrochanteric osteotomy are encouraging and compare well to those achieved in patients with normal femoral anatomy.
Introduction
Intertrochanteric femoral osteotomy (ITO) is a well-accepted joint preserving treatment for selected patients with various conditions of the hip, such as early symptomatic osteoarthritis, developmental dysplasia (DDH) or avascular necrosis of the femoral head (AVN) [1]. However, high failure rates for this procedure have been reported in the mid- and long-term, necessitating subsequent total hip arthroplasty (THA) in over 50% of patients in the second decade [2–4]. Conversion total hip arthroplasty (THA) in this subgroup of patients can be difficult, and inconsistent results have been reported with regard to complication rates, clinical outcomes and implant survival [5–7].
In primary THA, straight, cementless titanium stems have recently demonstrated good and excellent survival rates in the long-term [8–10], even for young patients [11–13]. In contrast to these findings, data on long-term stem performance (over ten years) in patients with secondary, end-stage osteoarthritis (OA) after proximal femoral osteotomy is very limited. There are few long-term studies for cemented [14–17] and particularly, for cementless [18] femoral components.
We have previously reported the clinical and radiographic outcomes of a consecutive series of 48 hips who had undergone conversion THA following intertrochanteric osteotomy using a straight, double tapered, grit-blasted titanium stem with a mean follow-up of 11 and 16 years [19, 20]. The purpose of this study was to determine survival rates and clinical and radiographic outcomes of cementless femoral reconstruction in this cohort at 20 years.
Methods
Patients
In a retrospective cohort study, we reviewed a consecutive series of 48 hips (45 patients) who underwent conversion THA following ITO with a cementless, straight, collarless titanium stem (CLS Spotorno, Zimmer, Warsaw, IN, USA; formerly Sulzer Orthopaedics, Switzerland, Fig. 1) between January 1985 and December 1989. An intertrochanteric osteotomy had been performed at a mean of 12 years (range, two to 33 years) before conversion to THA. Mean patient age at time of conversion was 50 years (range, 26–67 years). Patient demographics and diagnoses leading to ITO are given in Table 1.
Fig. 1.

CLS stem (Zimmer Inc., Warsaw, IN, USA)
Table 1.
Study cohort: patient demographics at conversion THA and diagnoses leading to intertrochanteric osteotomy
| Demographics | Value, n (% or range) |
|---|---|
| Age | 50 (range, 26–67) |
| BMI | 27 (range, 24–30) |
| Female | 36 (75%) |
| Male | 12 (25%) |
| Left | 22 (46%) |
| Right | 26 (54%) |
| Diagnoses | |
| DDH | 34 (69%) |
| AVN | 7 (15%) |
| Post-traumatic | 2 (5%) |
| Other | 5 (11%) |
DDH developmental dysplasia, AVN avascular necrosis of the femoral head
The femoral component used was wedge-shaped and tapered in all three planes with proximal, anterior and posterior ribs/flutes. The implant is made of Ti6Al7Nb alloy with a microporous surface treatment (Ra = 4.4 μm) and secondary osteointegration is achieved by osseous ongrowth onto the grit-blasted implant surface. In all patients, the femoral component with a neck-shaft angle of 145° was implanted using the press-fit technique as described by Spotorno et al. [21].
The femoral component was combined with three acetabular implants. In 45 cases (94%), smooth cementless threaded rings with polyethylene liners were used: forty hips (83%) received threaded spherical cementless Mecron rings (Mecron medizinische Produkte GmbH, Germany), and five hips (11%) threaded conical cementless Weill rings (Sulzer Orthopaedics, Switzerland). In three cases (6%), a cemented polyethylene cup (Aesculap, Tuttlingen, Germany) was implanted. All patients received 32-mm Biolox ceramic heads (Ceramtec, Plochingen, Germany).
The implantations were performed by three different senior surgeons in a university hospital setting. Either a modified Watson-Jones or a lateral transgluteal Bauer approach with the patient in a supine position was used. The femoral canal was prepared using a canal finder and a series of chipped tooth broaches of increasing size. No attempt was made to achieve cortical fixation. Postoperative partial weight bearing was encouraged for six weeks, and thereafter weight bearing as tolerated. No regular prophylaxis (irradiation or NSAIDs) for prevention of heterotopic ossification was administered. No standardised protocol for the removal of residual hardware was advocated. Removal was performed according to the surgeon’s preference, either in a separate procedure before conversion THA or during conversion THA.
All patients gave informed consent prior to inclusion in the study and procedures followed were approved by the institutional review board. The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2000.
Clinical and radiographic follow-up
Clinical outcome at final follow-up was determined using the Harris hip score (HHS) [22], and patient activity was assessed according to Devane et al. [23].
At final follow-up, low-centered pelvic radiographs and lateral radiographs of the hip were taken and independently examined by two blinded orthopaedic surgeons to determine stem positioning, subsidence, radiolucent lines, cortical hypertrophy, osteolysis, stress-shielding and femoral loosening. Radiolucent lines and areas of osteolysis were described according to the zones established by Gruen et al. [24]. Bone hypertrophy was defined as thickening of the periprosthetic diaphyseal bone of more than 2 mm on the most recent anteroposterior radiographs with reference to the initial postoperative radiograph. Osteolysis was defined as areas of localised bone resorption or endosteal erosion. Stress-shielding was determined according to the criteria of Engh et al. [25]. We considered only second, third, and fourth-degree stress-shielding with resorption of cortical bone medially, anteriorly, or laterally to be stress-shielding. The femoral stem was regarded as loose if a radiolucent line of over 2 mm in width was present around the entire implant or if a change in varus/valgus alignment of greater than 2° occurred on serial radiographs.
Statistics
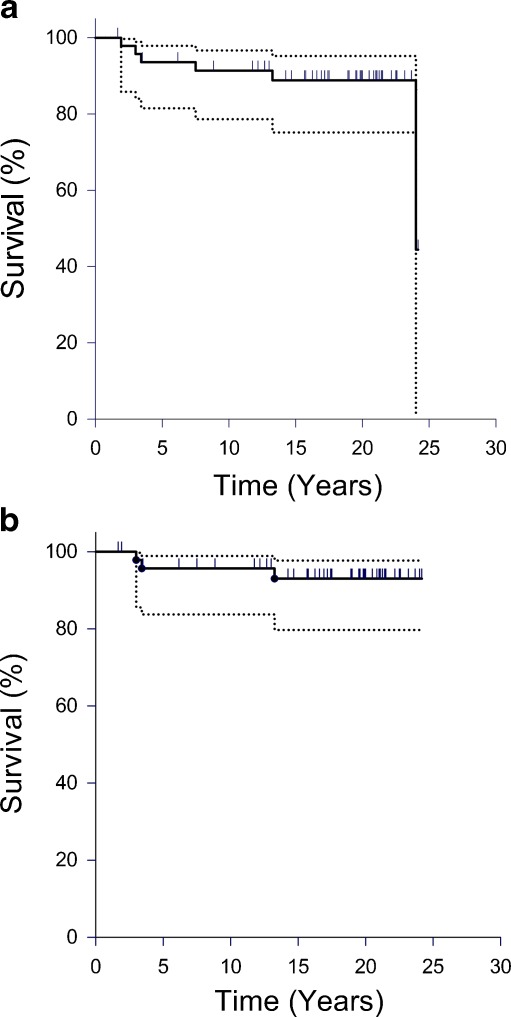
Kaplan-Meier survivorship analysis was performed to estimate stem survival rates with 95% confidence intervals for (1) stem revision for any reason (Fig. 2a) and (2) stem revision for aseptic loosening as endpoints (Fig. 2b). Patients were censored at death or at final follow-up, whichever event occurred first. Statistical analyses were carried out using SPSS Version 18.0 (SPSS, Chicago, IL, USA) and SigmaPlot Version 12.0 (Systat Software, San Jose, CA, USA).
Fig. 2.
a Kaplan-Meier plot: stem survival for all revisions as endpoint. The upper and lower curves represent the 95% confidence intervals. Vertical lines show censored patients. b Kaplan-Meier plot: stem survival for aseptic loosening as endpoint. The upper and lower curves represent the 95% confidence intervals. Vertical lines show censored patients
Results
Clinical findings
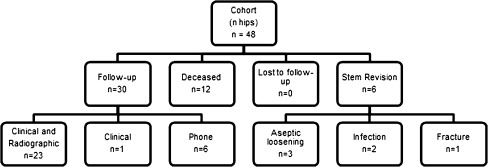
Mean follow-up was 20 years (range, 16–24 years). During the follow-up period, 11 patients (12 hips) died and six stems were revised: three for aseptic loosening (two revisions at three years, one revision at 13 years), two for infection (one revision at two years and one revision at 24 years) and one for periprosthetic fracture (at eight years). No patient was lost to follow-up.
Of the remaining 30 hips, clinical and radiographic follow-up was obtained for 23 hips. One patient (one hip) had clinical follow-up only, and six patients (six hips) were contacted by phone (Fig. 3). In all remaining patients, the stem had not been revised and no patient was awaiting revision. Mean Harris hip score at final follow-up was 78 points (range, 23–100 points). Assessment of patient activity at final follow-up according to Devane indicated that the patient cohort was active, in general, with a mean score of 2.75. Activity levels were grade 1 (zero patients), grade 2 (seven patients, eight hips), grade 3 (13 patients, 14 hips), and grade 4 (two patients, two hips), respectively. One patient reported mild thigh pain but radiographs at final follow-up did not show any radiographic signs of loosening, subsidence, osteolysis or change in stem position.
Fig. 3.
Distribution of hips at a mean follow-up of 20 years (range, 16–24 years)
Complications
Two patients sustained an undisplaced femoral fracture during canal preparation which was stabilised with cerclages and required no further treatment. One postoperative dislocation occurred and was successfully treated by closed reduction.
Radiographic findings
On radiographic evaluation at final follow-up, no radiographic signs of progressive stress-shielding, stem subsidence, cortical hypertrophy or change in varus/valgus alignment of the stem were observed (Fig. 4). The position of the femoral component was neutral in 20 patients; two stems had a varus position and one stem had a valgus position. Radiolucent lines were detected in eight hips and were limited to Gruen zones 1 (n = 4) and 7 (n = 4). Incomplete pedestal formation occurred in one case. Osteolysis (<1 cm2) was present in zone 7 in one case.
Fig. 4.
Preoperative, postoperative and 24-year follow-up radiographs of a male patient who was 53 years of age at time of conversion THA. Harris Hip Score was 91 points at final follow-up. Mild calcar rounding is present at 24 years and the osteotomy site is still visible
Cup revisions
Of the patients available for follow-up, 18 cups (60%) had been revised and one hip was awaiting cup revision.
Stem survival
Kaplan-Meier survivorship analysis revealed a stem survival rate of 89% (95%CI, 75–95) at 20 years for all revisions as endpoint (Fig. 2a). Survival for aseptic loosening was 93% (95%CI, 80–98) at 20 years (Fig. 2b).
Discussion
Apart from pain relief and restoration of joint function, the major goal of intertrochanteric osteotomy is to delay or even avert the progression of secondary osteoarthritis by a realignment of cartilage surfaces and a redistribution of joint forces. Moreover, the preservation of proximal femoral bone stock and the absence of THA related complications such as infection, dislocation or wear are further advantages so that the procedure is considered a valuable option for young patients [1]. However, the results of ITO are often impaired by progression of OA and the subsequent need for conversion THA is seen in a substantial percentage of patients in the mid- and long-term [2–4]. Femoral reconstruction in patients with previous osteotomy presents a major technical challenge as a result of distorted anatomy with malalignment, residual deformity, sclerosis, cortical holes or residual hardware [26]. Higher intra- and postoperative complication rates have been reported in this group of patients [6, 26–28]. There is still dispute whether proximal femoral osteotomy adversely affects the results of subsequent THA so that the potential benefits of joint preserving osteotomies must be weighed against the long-term outcome of conversion THA.
Our study investigated the clinical performance of a cementless tapered femoral component following ITO. The implant has been frequently used in Europe since 1983. We observed a low postoperative complication rate and a good long-term stem survival after 20 years. Radiolucent lines remained limited to Gruen zones 1 and 7. Radiographically, no case of severe stress-shielding or cortical hypertrophy was detected which indicates that the tapered design in combination with the rough surface of the component allow good primary stability, durable osteointegration and meta-diaphyseal load transfer, even in the presence of proximal femoral deformity and sclerosis. Interestingly, only one case showed radiographic evidence of osteolysis (<1 cm2) after 20 years.
Despite a high rate of cup revisions (60%) seen in the cohort, stem survival was not adversely affected. The unacceptably high failure rates of the threaded cups implanted in this cohort have been reported previously [29, 30] and can be explained by the smooth surface treatment of these components which impedes osteointegration. These implants are no longer in clinical use. Thus, the comparably low Harris hip score has to be interpreted with caution, as it is not only dependent on stem performance but also on the situation after intertrochanteric osteotomy and the high rate of acetabular revision.
Although osteolysis and consequently acetabular revision are potentially associated with a higher risk for stem revision, the exchange of the initial polyethylene bearing surface in a substantial percentage of patients of this cohort might have prevented excessive production of polyethylene wear particles and subsequent osteolysis.
We acknowledge the following limitations of the study. First, the cohort of 48 hips is small, limiting the number of patients available for clinical and radiographic follow-up. Second, the study design was retrospective and we cannot report pre-operative clinical parameters. However, we were able to obtain a complete follow-up of this cohort for a minimum of 16 years.
To date, we are not aware of any reports on long-term results of cementless THA after this condition of more than 15 years, despite the fact that cementless stem designs are favoured by many surgeons and are commonly offered to young patients.
Recent studies have evaluated the results of cementless femoral reconstruction after proximal femoral osteotomy in the short and mid-term. Lee et al. [28] and Kawasaki et al. [31] evaluated the outcome of conversion THA following transtrochanteric osteotomy for avascular necrosis of the femoral head, and reported longer operating times and higher intraoperative blood loss compared to primary THA. However, both authors independently concluded that no difference between primary and conversion THA was seen with respect to stem performance. Suzuki et al. [32] reported a stem survival of 100% at a mean follow-up of seven years for cementless components implanted in a cohort of patients with previous valgus osteotomy for advanced OA.
Our study confirms these promising results for cementless femoral reconstruction after proximal femoral osteotomy for the long-term. Our findings compare favourably to the reported long-term outcomes of cemented conversion THA [17]. This might be attributed to the fact that failures of cemented stems are mainly due to an inadequate cement mantle caused by distorted femoral anatomy [14]. Moreover, residual cortical holes may compromise cement pressurisation during implantation. We believe that fixation of a cementless tapered stem is less demanding and may be more predictable, especially under unusual anatomical conditions.
In conclusion, previous intertochanteric osteotomy did not impair the outcome of cementless femoral reconstruction in this study. The reliable and durable long-term results with this type of cementless femoral component in patients with previous intertrochanteric osteotomy are encouraging and compare well to those achieved in patients with normal femoral anatomy.
Acknowledgments
Conflict of interest
Financial support was received by the non-profit foundation Deutsche Arthrose Hilfe e.V.. The authors declare that they have no potential conflict of interest.
Contributor Information
Christian Merle, Phone: +49-622-1965, FAX: +49-622-1966347, Email: christian.merle@med.uni-heidelberg.de.
Marcus R. Streit, Email: marcus.streit@med.uni-heidelberg.de
Moritz Innmann, Email: moritz.innmann@med.uni-heidelberg.de.
Tobias Gotterbarm, Email: tobias.gotterbarm@med.uni-heidelberg.de.
Peter R. Aldinger, Email: peter.aldinger@diak-stuttgart.de
References
- 1.Turgeon TR, Phillips W, Kantor SR, Santore RF. The role of acetabular and femoral osteotomies in reconstructive surgery of the hip: 2005 and beyond. Clin Orthop Relat Res. 2005;441:188–199. doi: 10.1097/01.blo.0000193541.72443.73. [DOI] [PubMed] [Google Scholar]
- 2.McGrory BJ, Estok DM, 2nd, Harris WH. Follow-up of intertrochanteric osteotomy of the hip during a 25 year period. Orthopedics. 1998;21(6):651–653. doi: 10.3928/0147-7447-19980601-07. [DOI] [PubMed] [Google Scholar]
- 3.Ito H, Matsuno T, Minami A. Intertrochanteric varus osteotomy for osteoarthritis in patients with hip dysplasia: 6 to 28 years followup. Clin Orthop Relat Res. 2005;433:124–128. doi: 10.1097/01.blo.0000152881.57924.39. [DOI] [PubMed] [Google Scholar]
- 4.Zweifel J, Honle W, Schuh A. Long-term results of intertrochanteric varus osteotomy for dysplastic osteoarthritis of the hip. Int Orthop. 2011;35(1):9–12. doi: 10.1007/s00264-009-0870-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iwase T, Hasegawa Y, Iwasada S, Kitamura S, Iwata H. Total hip arthroplasty after failed intertrochanteric valgus osteotomy for advanced osteoarthrosis. Clin Orthop Relat Res. 1999;364:175–181. doi: 10.1097/00003086-199907000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Rijnen WH, Lameijn N, Schreurs BW, Gardeniers JW. Total hip arthroplasty after failed treatment for osteonecrosis of the femoral head. Orthop Clin North Am. 2009;40(2):291–298. doi: 10.1016/j.ocl.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Boos N, Krushell R, Ganz R, Muller ME. Total hip arthroplasty after previous proximal femoral osteotomy. J Bone Joint Surg Br. 1997;79(2):247–253. doi: 10.1302/0301-620X.79B2.6982. [DOI] [PubMed] [Google Scholar]
- 8.Aldinger PR, Jung AW, Breusch SJ, Ewerbeck V, Parsch D. Survival of the cementless spotorno stem in the second decade. Clin Orthop Relat Res. 2009;467(9):2297–2304. doi: 10.1007/s11999-009-0906-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suckel A, Geiger F, Kinzl L, Wulker N, Garbrecht M. Long-term results for the uncemented Zweymuller/alloclassic hip endoprosthesis. A 15 year minimum follow-up of 320 hip operations. J Arthroplasty. 2009;24(6):846–853. doi: 10.1016/j.arth.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 10.Belmont PJ, Jr, Powers CC, Beykirch SE, Hopper RH, Jr, Engh CA, Jr, Engh CA. Results of the anatomic medullary locking total hip arthroplasty at a minimum of twenty years. a concise follow-up of previous reports. J Bone Joint Surg Am. 2008;90(7):1524–1530. doi: 10.2106/JBJS.G.01142. [DOI] [PubMed] [Google Scholar]
- 11.Aldinger PR, Jung AW, Pritsch M, Breusch S, Thomsen M, Ewerbeck V, Parsch D. Uncemented grit-blasted straight tapered titanium stems in patients younger than fifty-five years of age. Fifteen to twenty-year results. J Bone Joint Surg Am. 2009;91(6):1432–1439. doi: 10.2106/JBJS.H.00297. [DOI] [PubMed] [Google Scholar]
- 12.McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component in patients younger than 50 years. J Arthroplasty. 2011;26(1):9–15. doi: 10.1016/j.arth.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 13.Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish arthroplasty register. Acta Orthop. 2006;77(1):57–70. doi: 10.1080/17453670610045704. [DOI] [PubMed] [Google Scholar]
- 14.Shinar AA, Harris WH. Cemented total hip arthroplasty following previous femoral osteotomy: an average 16 year follow-up study. J Arthroplasty. 1998;13(3):243–253. doi: 10.1016/S0883-5403(98)90168-1. [DOI] [PubMed] [Google Scholar]
- 15.Echeverri A, Shelley P, Wroblewski BM. Long-term results of hip arthroplasty for failure of previous surgery. J Bone Joint Surg Br. 1988;70(1):49–51. doi: 10.1302/0301-620X.70B1.3339060. [DOI] [PubMed] [Google Scholar]
- 16.Ferguson GM, Cabanela ME, Ilstrup DM. Total hip arthroplasty after failed intertrochanteric osteotomy. J Bone Joint Surg Br. 1994;76(2):252–257. [PubMed] [Google Scholar]
- 17.Haverkamp D, Jong PT, Marti RK. Intertrochanteric osteotomies do not impair long-term outcome of subsequent cemented total hip arthroplasties. Clin Orthop Relat Res. 2006;444:154–160. doi: 10.1097/01.blo.0000194066.10227.1e. [DOI] [PubMed] [Google Scholar]
- 18.Eskelinen A, Remes V, Ylinen P, Helenius I, Tallroth K, Paavilainen T. Cementless total hip arthroplasty in patients with severely dysplastic hips and a previous Schanz osteotomy of the femur: techniques, pitfalls, and long-term outcome. Acta Orthop. 2009;80(3):263–269. doi: 10.3109/17453670902967273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breusch SJ, Lukoschek M, Thomsen M, Mau H, Ewerbeck V, Aldinger PR. Ten-year results of uncemented hip stems for failed intertrochanteric osteotomy. Arch Orthop Trauma Surg. 2005;125(5):304–309. doi: 10.1007/s00402-005-0800-z. [DOI] [PubMed] [Google Scholar]
- 20.Parsch D, Jung AW, Thomsen M, Ewerbeck V, Aldinger PR. Good survival of uncemented tapered stems for failed intertrochanteric osteotomy: a mean 16 year follow-up study in 45 patients. Arch Orthop Trauma Surg. 2008;128(10):1081–1085. doi: 10.1007/s00402-007-0444-2. [DOI] [PubMed] [Google Scholar]
- 21.Spotorno L, Romagnoli S, Ivaldo N, Grappiolo G, Bibbiani E, Blaha DJ, Guen TA. The CLS system. Theoretical concept and results. Acta Orthop Belg. 1993;59(Suppl 1):144–148. [PubMed] [Google Scholar]
- 22.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 23.Devane PA, Robinson EJ, Bourne RB, Rorabeck CH, Nayak NN, Horne JG. Measurement of polyethylene wear in acetabular components inserted with and without cement. A randomized trial. J Bone Joint Surg Am. 1997;79(5):682–689. doi: 10.2106/00004623-199705000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 25.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69(1):45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 26.Mortazavi SM, Restrepo C, Kim PJ, Parvizi J, Hozack WJ. Cementless femoral reconstruction in patients with proximal femoral deformity. J Arthroplasty. 2011;26(3):354–359. doi: 10.1016/j.arth.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Delbarre JC, Hulet C, Schiltz D, Aubriot JH, Vielpeau C. Total hip arthroplasty after proximal femoral osteotomy: 75 cases with 9 year follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2002;88(3):245–256. [PubMed] [Google Scholar]
- 28.Lee YK, Ha YC, Kim KC, Yoo JJ, Koo KH. Total hip arthroplasty after previous transtrochanteric anterior rotational osteotomy for femoral head osteonecrosis. J Arthroplasty. 2009;24(8):1205–1209. doi: 10.1016/j.arth.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 29.Clarius M, Jung AW, Raiss P, Streit MR, Merle C, Aldinger PR. Long-term results of the threaded weill cup in primary total hip arthroplasty: a 15–20 year follow-up study. Int Orthop. 2010;34(7):943–948. doi: 10.1007/s00264-009-0844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clarius M, Jung AW, Streit MR, Merle C, Raiss P, Aldinger PR. Long-term results of the threaded Mecron cup in primary total hip arthroplasty: a 15–20 year follow-up study. Int Orthop. 2010;34(8):1093–1098. doi: 10.1007/s00264-009-0843-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kawasaki M, Hasegawa Y, Sakano S, Masui T, Ishiguro N. Total hip arthroplasty after failed transtrochanteric rotational osteotomy for avascular necrosis of the femoral head. J Arthroplasty. 2005;20(5):574–579. doi: 10.1016/j.arth.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 32.Suzuki K, Kawachi S, Matsubara M, Morita S, Jinno T, Shinomiya K. Cementless total hip replacement after previous intertrochanteric valgus osteotomy for advanced osteoarthritis. J Bone Joint Surg Br. 2007;89(9):1155–1157. doi: 10.1302/0301-620X.89B9.19082. [DOI] [PubMed] [Google Scholar]