Abstract
Arthroscopic examination and treatment is an ever-increasing part of modern orthopaedic practice in this age of minimally invasive surgery. Arthroscopic procedures have been widespread in surgery of the knee and the shoulder for many years; however, the hip until relatively recently, has been largely neglected. Even now hip arthroscopy is not widely available; this may be due to the complexity of the procedure, the requirement of specialist equipment and a reportedly long learning curve. On the other hand, it has gone through a period of rapid growth over the last decade and is being performed in large numbers routinely in some centres around the world. Hip arthroscopy now provides excellent visualisation of not only the articular surfaces of the hip joint but also of the peritrochanteric or extra-articular space around the hip. Pathology of both the femoral head and the acetabulum along with the soft tissues of the hip, namely the ligamentum teres, the acetabular labrum, the synovial folds and synovium, is readily diagnosed. Modern techniques provide therapeutic options for a myriad of conditions and allow modulation of pathological processes early. Additionally hip arthroscopy is a relatively safe procedure with few complications and contraindications. However, the key to good outcomes is in the careful selection of patients and meticulous surgical technique. The aim of this review is to bring the reader up to date with an overview of the evolution of arthroscopy of the hip, review the current practice and explore possible future developments.
Relevant anatomy and biomechanics
The hip joint is a ball and socket joint consisting of the femoral head articulating with the acetabulum of the pelvis. This highly congruent joint has three planes of movement, sagittal, transverse and frontal. The articular surfaces are entirely lined with type II collagen with the exception of the central portion of the acetabulum which is lined by a fatty layer (the pulvinar) surrounding the attachment of the ligamentum teres. This ligament helps stabilise the joint and is an important contributor to the blood supply of the femoral head in children.
The bony acetabulum is deepened by a triangular fibrocartilaginous structure called the acetabular labrum. This originates at the transverse acetabular ligament and attaches to the rim of the bony acetabulum. It increases the acetabular volume by a third and creates a negative intra-articular pressure to increase the inherent stability of the joint. Its second major function is to help the even distribution of forces within the joint [1]. Any dysplasia of the hip disrupts this and increases the load through the labrum [2] which may explain the higher incidence of labral tears in these conditions. The labrum also assists the unidirectional flow of synovial fluid, which depends on hip flexion and extension to drive the zona orbicularis like a bellows [3]. The labrum, much like the meniscus, derives most of its blood supply from the bony rim and is only vascularised in its peripheral third [4]. Nociceptors are present in all regions of the labrum particularly anterosuperiorly [5]. Thus damage to the labrum causes pain and tearing it from the rim may cause segments to be devascularised [6].
The capsule of the hip joint is reinforced by three ligaments, the most important of which, the iliofemoral ligament (of Bigelow), lies anteriorly. It forms an inverted Y shape and tightens with hip extension and is the strongest of the three. The pubofemoral ligament lies inferiorly and medially and tightens with hip extension and abduction. The third ligament, the ischiofemoral ligament, lies posteriorly and tightens with flexion.
The hip joint is subject to a large transmitted load. In a two-legged stance, the joint reaction force is half of the body weight above the hip. During the majority of the gait cycle the forces increase to approximately three times the body weight [7] with two significant peaks, one just after heel strike (four times the body weight) and one immediately before toe-off (seven times the body weight) [8].
The acetabular labrum can be placed under an undue amount of stress in conditions where the morphology of the hip is abnormal i.e. Dysplasia and Femoroacetabular Impingement (FAI) [9, 10]. FAI is a recently described condition wherein there is a painful contact between the femoral neck and the acetabular rim occuring within the physiologic range of motion of the hip joint [10]. There are essentially two morphological classifications that may lead to FAI [10]. Cam impingement occurs due to a non-spherical femoral head abutting against the anterior aspect of the acetabulum [11]. During flexion the non-spherical femoral head shears off the anterosuperior acetabular articular cartilage and there is chondrolabral separation. The second type of FAI, ‘pincer impingement’, is due to over-coverage of the anterior acetabulum or acetabular retroversion. This causes only limited cartilage damage in a narrow strip circumferentially, but the repeated abutment crushes the labrum between the acetabular rim and the femoral neck causing degeneration and ossification [12]. FAI has shown no influence on kinematics during walking but does reduce the range of movement of the hip, particularly abduction and flexion [13, 14]. This is most apparent during deep squatting [15] and may be associated with repetitive trauma of the peripheral articular cartilage [16, 17].
History and development
Endoscopes were developed over 200 years ago for the visualisation of vocal cords. However, it was not until the introduction of electricity and incandescent light sources that arthroscopes were first developed. Michael Burman, using a specifically designed 4-mm scope, examined over 90 cadaveric joints using fluid instillation to achieve distension [18]. He subsequently dissected each of the specimens and compared the arthroscopic visualisation with gross anatomy. Twenty of these joints were hips, which were examined without distraction. He noted that visualisation was limited to the articular surface of the femoral head and the intracapsular neck of femur (the peripheral compartment of today). Thus the acetabulum, acetabular fossa and the ligamentum teres were not visualised by Burman. He believed that it would be impossible to insert a needle between the femoral head and the acetabulum [18]. The misconception that it would be impossible to introduce a straight arthroscope into the hip led to stagnation in the practice of hip arthroscopy. The more straightforward arthroscopic approach to the knee meant that most innovation began with that joint. Bircher in the 1930s described the use of diagnostic arthroscopy to allow targeted open surgery of the knee [19] and arthroscopic techniques were further expanded in Japan by Takagi and Watanabe, who designed instrumentation for meniscectomy [20]. Takagi also performed some early arthroscopic examinations of the hip in 1939 [21].
The use of arthroscopic surgery in the knee and the shoulder became more widespread during the 1970s and 1980s with significant success. Concurrently, evidence began to emerge implicating the acetabular labrum both as a source of hip pain in the presence of normal looking radiographs and in the evolution of arthritis of the hip [22]. This led to resurgence of interest in arthroscopy of the hip with the first arthroscopic labral tear being described in 1986 [23]. The development of specialised equipment in the late 1990s and early 2000s coupled with improved surgical techniques and a better understanding of pathology has led to an increasing number of surgeons performing this procedure. Much of this earlier pioneering work was performed by James Glick, who described the lateral approach [24] and was also key to the development of specialised instrumentation required for this procedure. He was also one of the surgeons who encouraged the routine use of traction for access to the hip.
As the development of this procedure has progressed the hip has been divided into three compartments. The intracapsular region is split into the central and peripheral compartments with the labrum as the dividing line. The central compartment is intracapsular and truly intra-articular and consists of the weight-bearing area of the femoral head and the acetabulum along with the acetabular fossa and the ligamentum teres, whereas the peripheral compartment is intracapsular but extra-articular and consists of the remainder of the femoral head and neck up to the insertion of the capsule and the synovial folds. This distinction is important because traction is only necessary for visualisation of the central compartment [25]. Recently, a third compartment termed the lateral compartment or the peritrochanteric space has been described consisting of the space between the proximal femur and the tensor fascia lata [26].
Initially arthroscopic surgery of the hip was mainly diagnostic, but better understanding of the pathology, better examination techniques and better imaging have led to increasing numbers of therapeutic procedures being performed and also led to recognition of new pathologies. These conditions were difficult to diagnose with traditional modalities and required direct visualisation of the joint. Provocative manoeuvres during examination of the joint have been described but have limitations. Noninvasive radiological investigations typically have high false-negative rates in these conditions. Magnetic resonance imaging (MRI) has a false-negative rate of up to 42% in the diagnosis of intra-articular hip pathology [27] which can be improved by using intra-articular contrast. More invasive investigations such as a diagnostic injection of local anaesthetic into the hip joint may help differentiate between intra-articular and extra-articular sources of pain but does not provide any information about the nature of the pathology [28]. Thus for a lot of pathologies, arthroscopic evaluation is vital in the diagnosis and arthroscopic intervention may be the mainstay of treatment.
Technique
There are numerous technical challenges to performing arthroscopy of the hip. The thick muscular envelope and subcutaneous fat layer require longer arthroscopic portals and instruments. In addition, the instruments are required to be more flexible than conventional arthroscopic equipment to accommodate for the ball and socket nature of the joint. The patient may be placed in either the lateral [24] or supine [29] position with traction to help distract the joint. Prerequisites for this traction include a broad, well-padded perineal post and a well-padded boot. The joint is then distracted under fluoroscopic guidance and distension of the joint is maintained by traction and fluid instillation under pressure using a fluid management system. Due to the anatomy of the capsular ligaments this distraction is best achieved in slight flexion. This however does draw the sciatic nerve closer to the hip joint therefore putting it at risk of damage especially via using a posterior portal. The tough capsule surrounding the joint may require an equivalent force of between 25 and 50 lb to achieve 8–10 mm of distraction. Adequate distraction is demonstrated by the ‘halo’ sign on the image intensifier, which represents the formation of a vacuum within the joint [30]. The joint is then entered using a long 17 G needle and distended with 30–40 ml of saline; a nitinol guide wire is passed into the joint via the needle and the needle withdrawn. A 4.5 mm to a 5.5 mm arthroscope can then be passed over the guide wire into the joint. A 70° arthroscope is usually used for viewing the hip joint and then other portals are made under direct vision. Typically three portals are used: one direct lateral paratrochanteric portal and another anterolateral paratrochanteric portal, which combine to provide excellent visualisation of the joint in its entirety. Saline is infused under a pressure of up to 100 mmHg [31] (pressures of 50–60 mmHg are more typical) to assist with capsular distension. In common with other arthroscopic techniques a diagnostic sweep is usual prior to the treatment of any identified pathology. Use of slotted cannulae and flexible instruments allow a wide variety of procedures to be undertaken in the joint. Following visualisation and treatment of any pathology in the central compartment the traction is released and the peripheral compartment dealt with in turn. Access to the peripheral compartment may be achieved using the same standard portals or a specific anterosuperior portal which lies between the anterior superior iliac spine and the greater trochanter. In order to visualise the lateral compartment the anterior portal is usually redirected between the bursa overlying the greater trochanter and the iliotibial band.
Current indications
The diagnostic role of hip arthroscopy has increased as more varied pathologies have been described. There are numerous pathologies that are difficult to diagnose either clinically or using conventional radiology. The arthroscope is therefore often used in the investigation of unexplained hip or groin pain. It may also be used to investigate a hip effusion or synovitis. This may represent an isolated finding on MRI and arthroscopy allows inspection, washout and synovial biopsy to aid diagnosis. It cannot be overemphasised that proper patient selection is vital and relies on recognition of appropriate indications.
The therapeutic indications may be divided into intra-articular and extra-articular pathologies.
Intra-articular indications
A common use of any arthroscope is the lavage of an infected joint and the hip is no exception. This may mean that hip arthroscopy becomes a routine part of the workup for a septic hip. Due to the depth of the joint from the skin it is more difficult to aspirate the hip joint for diagnostic purposes when compared to the knee or the shoulder. A hip arthroscopic procedure may therefore allow both the diagnosis and initial treatment to be undertaken in the same sitting. Further benefits of arthroscopic diagnosis include the assessment of the cartilaginous surface. Clinical series indicate support for its use in both the adult and paediatric populations [32, 33]. However, any evidence of osteomyelitis or abscess formation requires open surgery. There may also be an analgesic benefit in the lavage of a hip affected by crystal arthropathy though this is more controversial.
Another clear indication for hip arthroscopy is the removal of loose bodies. They may be ossified or radiolucent. The more common radiolucent fragments are difficult to diagnose with conventional radiographs but the diagnosis may be evident from the history alone. They classically present with catching or locking which may be intermittent. The poor prognosis of retained loose bodies has been well established and the removal of these fragments is important. Loose bodies may represent post-traumatic osteochondral fragments, bony fragments in Perthes’ disease or may be related to a hip prosthesis. Furthermore, synovial osteochondromatosis may lead to the accumulation of multiple intra-articular loose bodies. Arthroscopic removal of these fragments is associated with rapid and profound relief of symptoms [34] and may be coupled with thermal ablation of the synovium with the aim of preventing recurrence, albeit with limited success. Other synovial abnormalities including collagen vascular diseases and pigmented villonodular synovitis may also be amenable to arthroscopic partial synovectomy.
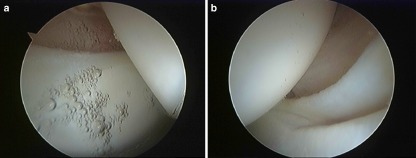
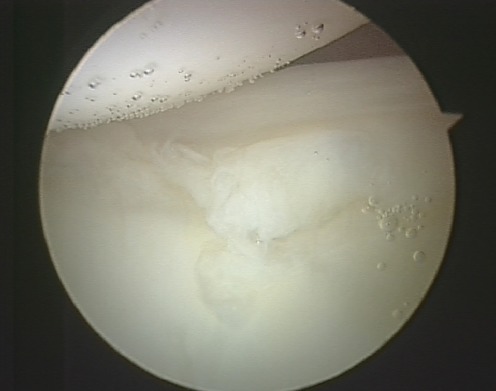
The most common indication for arthroscopic hip surgery remains pathology of the acetabular labrum though these lesions are notoriously hard to diagnose [35]. The majority occur in the anterosuperior quadrant [36]. The labrum is easily visible and readily accessible via the arthroscope. Its pathology is particularly suitable for an arthroscopic approach (Fig. 1a, b). Acute labral tears may cause persistent pain following the closed reduction of a hip dislocation and may be associated with simpler mechanisms such as twisting or squatting. The majority are related to degenerative change and are associated with numerous pathologies including Perthes’, acetabular dysplasia and slipped upper capital epiphysis (SUFE) and FAI [37]. Once present these tears tend to heal poorly due to the tenuous blood supply. The mainstay of treatment is delineating areas of labral degeneration that may be amenable to resection or repair. Labral tears (Fig. 2) are technically challenging to repair and such procedures historically were reserved for acute traumatic tears of the labrum. However, newer suture anchors and knotless anchors have increased the number of tears which are amenable to repair. The results of labral repair also seem promising in the short and medium term [38], but resection remains the treatment of choice for those tears that are impossible to reconstruct.
Fig. 1.
a Arthroscopic view of the hip joint showing the anterosuperior aspect of the acetabular labrum. b Arthroscopic view of the hip joint showing the posterior aspect of the labrum with the normal sulcus
Fig. 2.
Arthroscopic view of the hip joint showing a tear of the acetabular labrum
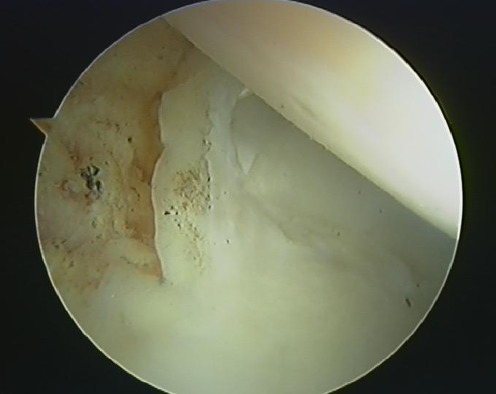
The final effect of numerous pathological processes, including labral tears, is chondrolabral separation and chondral damage causing a defect in the articular cartilage of either the acetabulum or uncommonly the femoral head. Repetitive loading cycles force synovial fluid between layers of the articular cartilage causing delamination and a stepwise progression from a simple chondral split to a flap lesion (Fig. 3) ending as a subchondral cyst. These defects may also be secondary to a direct compressive injury [39], are often associated with loose bodies and most commonly occur in the anterior aspect of the acetabulum [6]. They are distinguished from generalised degenerative wear by the local nature of the defect compared with the more widespread chondral thinning and exposure of subchondral bone associated with degenerative change. Arthroscopic debridement of the chondral tear to its stable margins has been associated with rapid resolution of symptoms [40]. Simple splits may be treated using a radiofrequency probe to coalesce the defect, whereas more extensive defects require resection to improve symptoms. The exposed subchondral bone may be microfractured [41]. Outcomes of treatment are usually good with rapid resolution of symptoms particularly if only partial resection is required [42]. Prognosis is certainly improved by early diagnosis [43], worsened when defects are present in both the acetabulum and femoral head and also if the defect is greater than 1 cm2.
Fig. 3.
Arthroscopic view of the hip joint showing a chondral flap
FAI is a challenging clinical entity both to diagnose and treat. As explained above the end result of these anatomical abnormalities is chondral damage and labral tears. In addition to treating these lesions hip arthroscopy may be used to treat the underlying abnormality. The surgical aim is to improve the clearance available during hip flexion. This may be achieved in cam lesions by recreating adequate offset of the femoral head by removing excess anterior bone from the femoral neck using a burr. In pincer lesions this may be achieved by recessing the acetabular rim [44]. In practice, the forms of FAI may coexist as mixed impingement and therefore a combination of procedures is required [11]. Normalising the joint mechanics should theoretically prevent further microtrauma and either slow or halt the progression to degenerative joint disease.
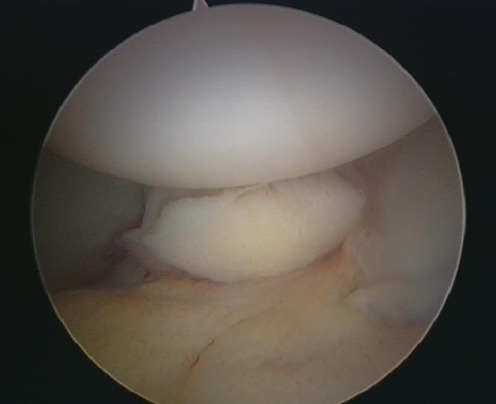
Trauma to the hip may result in clinical subluxation with an associated tear of the ligamentum teres (Fig. 4). The avulsion of this ligament from the fovea may result in pain directly or be implicated in impingement syndromes [45]. The arthroscopic resection of this ligamentous stump often results in near complete resolution of symptoms [46].
Fig. 4.
Arthroscopic view of the hip joint showing the ligamentum teres
The role of hip arthroscopy in degenerative joint disease of the hip is less clear. It seems that the patients that derive most benefit are those who have had recent onset of symptoms and those who are young. Currently hip arthroscopy is only a temporising measure in these patients [47] helping to delay the need for arthroplasty especially in the young. Hip arthroscopy has also been found useful in cases of the painful hip arthroplasty by releasing soft tissue bands, removing retained cement or loose bodies, addressing iliopsoas impingement following resurfacing and also excising residual cam impingement following a resurfacing.
Extra-articular indications
Extra-articular indications for arthroscopic surgery of the hip include snapping hip, trochanteric bursitis and gluteus medius tears [48]. Trochanteric bursitis may be treated with arthroscopic debridement of the bursa [49] and tears of gluteus medius may be directly repaired [50]. Snapping hip is a condition characterised by a painful audible click originating around the hip as moved. It can be subclassified by aetiology into lateral (external), medial (internal) and intra-articular types with lateral being the most frequent. Lateral snapping hip is commonly caused by either the iliotibial band or gluteus tendon snapping over the greater trochanter [51], whereas medial snapping hip seems to be caused by iliopsoas tendon snapping over either the iliopectineal eminence or the femoral head itself [52]. A loose body or a labral tear commonly lead to an intra-articular snapping of the hip. The diagnosis may be made clinically by the site of clicking (either lateral or anterior) and the movement, which elicits the symptoms with rotation localising the pathology intra-articularly. Whilst many snapping hips settle with nonoperative management using nonsteroidal anti-inflammatory medication and physiotherapy, refractory cases do require surgery. Arthroscopy of the hip allows ready access both trans-articularly for release of the iliopsoas for medial snapping and extra-articularly using the lateral portal to access the iliotibial band.
In common with much other arthroscopic practice there has been increasing interest in the role of hip arthroscopy in athletes. They are a younger population of physically active individuals who put larger strain on their joints increasing the risk of the pathologies outlined above. In addition, they may suffer from other rare pathologies such as recurrent subluxation, which may cause hip pain and necessitate treatment with thermal capsular shrinkage or capsular plication [53]. The thermal shrinkage of the capsule has also been proposed as treatment for those patients who demonstrate ligamentous laxity such as patients with Ehlers-Danlos syndrome.
Complications
The report rate of complications is low (1.4%) and it is a relatively safe procedure [54]. Intra-operative complications include the small risk of bleeding and infection present with any invasive procedure and damage to the femoral head. This scuffing of the articular surface may be reduced by meticulous technique and placement of the secondary portals under vision. There have been reports of direct damage to the lateral cutaneous nerve of thigh during the creation of portal sites though this is exceptionally rare [55]. The majority of the remaining early complications are related to the requirement for traction. Thus traction time should be ideally kept to below 2 hours. These complications include neuropraxia of the sciatic, femoral or pudendal nerves. Other related complications are due to direct damage to the perineal area by the post; in local haematoma, vaginal tears and scrotal ischaemia [56]. Late complications include trochanteric bursitis and bleeding from portal sites. Finally, rare cases of osteonecrosis, iatrogenic dislocation of the femoral head and fluid extravasation into the abdomen have been reported as well [57]. However, if carried out judiciously and meticulously it does remain a safe and effective procedure.
Contraindications
The future
The development of this technique and the production of specialised instrumentation have allowed an increasing number of procedures to be undertaken. This in turn has led to an increased understanding of intra-articular hip pathology and possible indications for arthroscopy. These indications will continue to expand and be refined as longer-term outcomes emerge. Furthermore, as techniques improve other procedures may become possible, for example arthroscopic reconstruction of the ligamentum teres, which has already been reported. This would allow the resolution of the pain and mechanical symptoms, which result from its disruption without sacrificing the possible biological and structural roles, which it may play. The addition of computer-aided techniques [59] to the arthroscopic treatment of impingement may allow better, earlier, more targeted interventions with an associated improvement in outcomes. The potential of arthroscopy to slow or halt progression of degenerative joint disease may be the most exciting potential application of this technique. In the presence of an increasingly active, elderly population the incidence of degenerative joint disease will continue to rise. When coupled with other new technologies such as implantation of autologous chondrocytes it may allow minimally invasive biological reconstruction of the articular surface [60]. Finally, arthroscopy may have a large role to play in the management of the painful hip arthroplasty [61] and certainly an area which is expanding rapidly is extra-articular hip endoscopy. The future for this procedure is certainly bright, but the learning curve remains steep and therefore investment in time for adequate training is essential.
References
- 1.Ferguson SJ, Bryant JT, Ganz R, et al. The acetabular labrum seal: a poroelastic finite element model. Clin Biomech (Bristol, Avon) 2000;15:463–468. doi: 10.1016/S0268-0033(99)00099-6. [DOI] [PubMed] [Google Scholar]
- 2.Henak CR, Ellis BJ, Harris MD, Anderson AE, Peters CL, Weiss JA. Role of the acetabular labrum in load support across the hip joint. J Biomech. 2011;44:2201–2206. doi: 10.1016/j.jbiomech.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Field RE, Rajakulendran K. The labro-acetabular complex. J Bone Joint Surg Am. 2011;93(Suppl 2):22–27. doi: 10.2106/JBJS.J.01710. [DOI] [PubMed] [Google Scholar]
- 4.Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH., Jr Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232–240. doi: 10.1097/00003086-200101000-00031. [DOI] [PubMed] [Google Scholar]
- 5.Kim YT, Azuma H. The nerve endings of the acetabular labrum. Clin Orthop Relat Res. 1995;320:176–181. [PubMed] [Google Scholar]
- 6.McCarthy JC, Noble PC, Schuck MR, et al. The watershed labral lesion: its relationship to early arthritis of the hip. J Arthroplasty. 2001;16(8 Suppl:1):81–87. doi: 10.1054/arth.2001.28370. [DOI] [PubMed] [Google Scholar]
- 7.Philippon MJ (2003) Arthroscopy of the hip in the management of the athlete. In: McGinty JB (ed) Operative arthroscopy. Lippincott, Williams & Wilkins, Philadelphia, pp 879–883
- 8.Nordin M, Frankel VH (2001) Basic biomechanics of the musculoskeletal system, 3rd edn. Lippencott Williams & Wilkins, Philadelphia, pp 208–215
- 9.Safran MR, Giordano G, Lindsey DP, Gold GE, Rosenberg J, Zaffagnini S, Giori NJ. Strains across the acetabular labrum during hip motion: a cadaveric model. Am J Sports Med. 2011;39(Suppl):92S–102S. doi: 10.1177/0363546511414017. [DOI] [PubMed] [Google Scholar]
- 10.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 11.Samirul Imam & Vikas Khanduja. Current Concepts in the diagnosis and Management of Femoroacetabular Impingement. IO 35:1427–1435 [DOI] [PMC free article] [PubMed]
- 12.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy MJ, Lamontagne M, Beaulé PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait: walking biomechanics of FAI. Gait Posture. 2009;30(1):41–44. doi: 10.1016/j.gaitpost.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Kubiak-Langer M, Tannast M, Murphy SB, Siebenrock KA, Langlotz F. Range of motion in anterior femoroacetabular impingement. Clin Orthop Relat Res. 2007;458:117–124. doi: 10.1097/BLO.0b013e318031c595. [DOI] [PubMed] [Google Scholar]
- 15.Lamontagne M, Kennedy MJ, Beaulé PE. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop Relat Res. 2009;467(3):645–650. doi: 10.1007/s11999-008-0620-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leunig M, Beck M, Dora C, Ganz R. Femoroacetabular impingement: etiology and surgical concept. Oper Tech Orthop. 2005;15(3):247–255. doi: 10.1053/j.oto.2005.06.005. [DOI] [Google Scholar]
- 17.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83(2):171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 18.Burman MS. Arthroscopy or the direct visualisation of joints. J Bone Joint Surg Br. 1931;13:669–695. [Google Scholar]
- 19.Kieser C, Jackson R. Eugen Bircher (1882–1956) the first knee surgeon to use diagnostic arthroscopy. Arthroscopy. 2003;19(7):771–776. doi: 10.1016/S0749-8063(03)00693-5. [DOI] [PubMed] [Google Scholar]
- 20.Jackson RW. Memories of the early days of arthroscopy: 1965–1975. The formative years. Arthroscopy. 1987;3(1):1–3. doi: 10.1016/S0749-8063(87)80002-6. [DOI] [PubMed] [Google Scholar]
- 21.Takagi K. The arthroscope: the second report. J Jpn Orthop Assoc. 1939;14:441–466. [Google Scholar]
- 22.Altenberg AR. Acetabular labral tears: a cause of pain and degenerative arthritis. South Med J. 1977;70:174–175. doi: 10.1097/00007611-197702000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Suzuki S, Awaya G, Okada Y, et al. Arthroscopic diagnosis of ruptured acetabular labrum. Acta Orthop Scand. 1986;57(6):513–515. doi: 10.3109/17453678609014781. [DOI] [PubMed] [Google Scholar]
- 24.Glick JM, Sampson TG, Gordon RB, Behr JT, Schmidt E. Hip arthroscopy by the lateral approach. Arthroscopy. 1987;3:4–12. doi: 10.1016/S0749-8063(87)80003-8. [DOI] [PubMed] [Google Scholar]
- 25.Dienst M, Gödde S, Seil R, et al. Hip arthroscopy without traction: in vivo anatomy of the peripheral hip joint cavity. Arthroscopy. 2001;17(9):924–931. doi: 10.1053/jars.2001.25342. [DOI] [PubMed] [Google Scholar]
- 26.Voos JE, Ranawat AS, Kelly BT. The peritrochanteric space of the hip. Instr Course Lect. 2009;58:193–201. [PubMed] [Google Scholar]
- 27.Bryd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32(7):1668–1674. doi: 10.1177/0363546504266480. [DOI] [PubMed] [Google Scholar]
- 28.McCarthy JC, Lee JA. Hip arthroscopy: indications, outcomes, and complications. Instr Course Lect. 2006;55:301–308. [PubMed] [Google Scholar]
- 29.Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280. doi: 10.1016/S0749-8063(05)80111-2. [DOI] [PubMed] [Google Scholar]
- 30.Villar RN. Hip arthroscopy. Oxford: Butterworth-Heinmann; 1992. The technique of hip arthroscopy; pp. 39–53. [Google Scholar]
- 31.Khanduja V, Villar RN. Arthroscopy of the hip: current concepts and recent advances. J Bone Joint Surg Br. 2006;88-B:1557–1566. doi: 10.1302/0301-620X.88B12.18584. [DOI] [PubMed] [Google Scholar]
- 32.El-Sayed AM. Treatment of early septic arthritis of the hip in children: comparison of results of open arthrotomy versus arthroscopic drainage. J Child Orthop. 2008;2(3):229–237. doi: 10.1007/s11832-008-0094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rutz E, Brunner R. Septic arthritis of the hip - current concepts. Hip Int. 2009;19(Suppl 6):S9–S12. doi: 10.1177/112070000901906s03. [DOI] [PubMed] [Google Scholar]
- 34.Boyer T, Dorfmann H. Arthroscopy in primary synovial chondromatosis of the hip: description and outcome of treatment. J Bone Joint Surg Br. 2008;90(3):314–318. doi: 10.1302/0301-620X.90B3.19664. [DOI] [PubMed] [Google Scholar]
- 35.Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15:132–137. doi: 10.1053/ar.1999.v15.015013. [DOI] [PubMed] [Google Scholar]
- 36.Fitzgerald RH., Jr Acetabular labrum tears. Diagnosis and treatment. Clin Orthop. 1995;311:60–68. [PubMed] [Google Scholar]
- 37.Wenger DE, Kendell KR, Miner MR, et al. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop. 2004;426:145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
- 38.Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 39.Byrd JW. Lateral impact injury. A source of occult hip pathology. Clin Sports Med. 2001;20:801–815. doi: 10.1016/S0278-5919(05)70286-6. [DOI] [PubMed] [Google Scholar]
- 40.Robertson WJ, Kadrmas WR, Kelly BT. Arthroscopic management of labral tears in the hip: a systematic review of the literature. Clin Orthop Relat Res. 2007;455:88–92. doi: 10.1097/BLO.0b013e31802c7e0f. [DOI] [PubMed] [Google Scholar]
- 41.Crawford K, Philippon MJ, Sekiya JK, Rodkey WG, Steadman JR. Microfracture of the hip in athletes. Clin Sports Med. 2006;25:327–335. doi: 10.1016/j.csm.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 42.O’Donnell JM. Second look arthroscopy after debridement of articular cartilage defects [abstract]. Advances in hip arthroscopy meeting. 2006. p. 115. [Google Scholar]
- 43.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 44.Lavigne M, Parvizi J, Beck M, et al. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop. 2004;418:61–66. doi: 10.1097/00003086-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 45.Rao J, Zhou YX, Villar RN. Injury to the ligamentum teres. Mechanism, findings, and results of treatment. Clin Sports Med. 2001;20:791–799. doi: 10.1016/S0278-5919(05)70285-4. [DOI] [PubMed] [Google Scholar]
- 46.Bardakos NV, Villar RN. The ligamentum teres of the adult hip. J Bone Joint Surg Br. 2009;91(1):8–15. doi: 10.1302/0301-620X.91B1.21421. [DOI] [PubMed] [Google Scholar]
- 47.Kelly BT, Williams RJ, 3rd, Phillippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–1037. doi: 10.1177/03635465030310060701. [DOI] [PubMed] [Google Scholar]
- 48.Shindle MK, Voos JE, Heyworth BE, et al. Hip arthroscopy in the athletic patient: current techniques and spectrum of disease. J Bone Joint Surg Am. 2007;89(Suppl 3):29–43. doi: 10.2106/JBJS.G.00603. [DOI] [PubMed] [Google Scholar]
- 49.Wiese M, Rubenthaler F, Willburger RE, et al. Early results of endoscopic trochanteric bursectomy. Int Orthop. 2004;28:218–221. doi: 10.1007/s00264-004-0569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Voos JE, Shindle MK, Pruett A, Asnis PD, Kelly BT. Endoscopic repair of gluteus medius tendon tears of the hip. Am J Sports Med. 2009;37:743–747. doi: 10.1177/0363546508328412. [DOI] [PubMed] [Google Scholar]
- 51.Jacobson T, Allen WC. Surgical correction of the snapping iliopsoas tendon. Am J Sports Med. 1990;18(5):470–474. doi: 10.1177/036354659001800504. [DOI] [PubMed] [Google Scholar]
- 52.Dobbs MB, Gordon JE, Luhmann SJ, Szymanski DA, Schoenecker PL. Surgical correction of the snapping iliopsoas tendon in adolescents. J Bone Joint Surg Am. 2002;84(3):420–424. doi: 10.2106/00004623-200203000-00013. [DOI] [PubMed] [Google Scholar]
- 53.Philippon MJ. The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med. 2001;20:817–829. doi: 10.1016/S0278-5919(05)70287-8. [DOI] [PubMed] [Google Scholar]
- 54.Clarke MT, Arora A, Villar RN. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res. 2003;406:84–88. doi: 10.1097/00003086-200301000-00014. [DOI] [PubMed] [Google Scholar]
- 55.Frich LH, Lauritzen J, Juhl M. Arthroscopy in diagnosis and treatment of hip disorders. Orthopedics. 1989;12:389–392. doi: 10.3928/0147-7447-19890301-09. [DOI] [PubMed] [Google Scholar]
- 56.Griffin DR, Villar RN. Complications of arthroscopy of the hip. J Bone Joint Surg Br. 1999;81-B:604–606. doi: 10.1302/0301-620X.81B4.9102. [DOI] [PubMed] [Google Scholar]
- 57.Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 58.McCarthy JC. Hip arthroscopy: when it is and when it is not indicated. Instr Course Lect. 2004;53:615–621. [PubMed] [Google Scholar]
- 59.Brunner A, Horisberger M, Herzog RF. Evaluation of a computed tomography-based navigation system prototype for hip arthroscopy in the treatment of femoroacetabular cam impingement. Arthroscopy. 2009;25:382–391. doi: 10.1016/j.arthro.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 60.Fontana AF. Autologous chondrocyte transplantation [abstract]. Advances in hip arthroscopy meeting. 2006. p. 185. [Google Scholar]
- 61.Bajwa AS, Villar RN. Arthroscopy of the hip in patients following joint replacement. J Bone Joint Surg Br. 2011;93(7):890–896. doi: 10.1302/0301-620X.93B7.24902. [DOI] [PubMed] [Google Scholar]