Abstract
Objectives
The present study aimed to validate screening tools that could be used to identify depression among workers.
Design
Diagnostic test study.
Settings
Workers from three Japanese companies agreed to participate.
Participants
Recruitment for the group 1 occurred between January 2001 and February 2004, and 89 participants (81 men and 8 women with a mean age of 38.4±6.6 years) (98.8%) took part in the study. Recruitment for the group 2 occurred between July 2000 and February 2004, and 1500 participants (1408 men and 92 women with a mean age of 40.9±7.2 years) (94.2%) took part in the study. Demographic data are shown in supplementary table 1.
Interventions
Primary and secondary outcome measures: the Beck Depression Inventory (BDI) and a two-question case-finding instrument (TQI) were administered to 89 workers and Mini-International Neuropsychiatric Interview was conducted to verify the diagnosis of depression. A second group of 1500 workers completed the BDI and TQI to detect possible sample bias for the distribution of depression. Specificity, sensitivity and positive predictive value were calculated in order to obtain the optimal cut-off scores for BDI and TQI and receiver operating characteristic curves, and Youden Index were applied to further refine the optimal cut-off scores.
Results
When paired together, BDI score ≥10 and TQI score of 2 adequately identified workers who had major depressive disorder and those who had other psychiatric disorders that are frequently comorbid with major depressive disorder.
Conclusions
The combination of BDI score ≥10 and TQI score of 2 can adequately screen for current and potential cases of depression among workers. Furthermore, BDI and TQI offer the advantage of being relatively easy to administer to a large number of workers. Early detection of depression could improve treatment outcomes and decrease economic burden.
Trail registration
Article summary
Article focus
Depression is associated with enormous economic burden and the social cost of depression is attributed to the functional impairment of employees.
Even though the magnitude of productivity loss from depression is substantial, a large number of depressed workers are untreated or inadequately treated.
An efficient screening tool for depression among workers is needed because it is difficult to interview and evaluate all employees.
Key messages
The combination use of the BDI and a two-question case-finding instrument adequately identified workers who had MDD.
Furthermore, it adequately identified workers who had other psychiatric disorders that are frequently comorbid with MDD.
Strength and limitations of this study
This study presents an effective way to screen for current and potential cases of depression in the workplace, which is easy to administer to a large number of workers.
The limitations of the study are as follows: the sample size was relatively small, the Japanese version of two-question case-finding instrument has not been validated, not all participants were diagnosed using the diagnostic interview and effect of socio-economical factors and clinical factors were not included in the analysis.
Introduction
Depression is a highly prevalent disorder, that is, associated with enormous economic costs. Major depressive disorder (MDD) was estimated to affect 18.1 million people living in the USA in 2000 and to have lifetime prevalence of 16.2% and an annual prevalence of 6.6%.1 2 The total economic burden (both direct and indirect costs) of depression was estimated to be more than US$ 83 billion and €118 billion in the USA and Europe, respectively.1 3 In Japan, MDD was estimated to have an annual prevalence of 2.2% and 7.0% of white collar workers were reported to meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for major depressive episode and score more than 40 points (depressive range) on the self-rating depression scale.4 5 The annual societal cost of depression and suicide was estimated at 2.7 trillion yen.6 Based on the epidemiological trends, depression will become the second leading cause of global disease burden by 20207 and is expected to rank first in disease burden in high-income countries by the 2030.8
The economic burden of depression is attributed to functional impairment of employees due to physical and cognitive symptoms. Moreover, the prevalence of depression is highest in the age group of 15–64, which corresponds to the typical working age.9 Indeed, it was reported that depressed workers in the USA have 1.5–3.2 times more short-term work-disability days per month than people who were not depressed.10 Furthermore, the European ESEMeD study revealed that depressed workers had 3–4 times more work-loss days per month compared with workers without depression.11 In addition to the cost of depression-related absenteeism, presenteeism, the state in which depressed workers stay at work but have reduced productivity as a result of their condition, needs to be considered.
Even though the magnitude of productivity loss from depression is substantial, a large number of depressed workers are untreated or inadequately treated.2 12 13 The increasing duration of untreated illness (DUI) may be associated with worse treatment outcomes of depression.14 Many studies have reported that DUI is a predictive factor for treatment outcome.15–17 In addition, early treatment of the first depressive episode is important because our previous study showed that a shorter DUI implied better remission outcomes in patients with the first MDD.18 Therefore, early identification of depressed workers is crucial in order to improve treatment outcomes and reduce cost.2 12 Moreover, since it is difficult to interview and evaluate all employees, an efficient screening tool for depression among workers is needed.
The aim of the present study was to establish an efficient way to identify workers who were diagnosed as having MDD (= workers with depression) and those who were not diagnosed as having MDD but had other psychiatric disorders that are frequently comorbid with MDD (= workers with comorbid disorders). We identified workers with depression using Mini-International Neuropsychiatric Interview (M.I.N.I.) and investigated an optimal pair of cut-off scores using a combination of Beck Depression Inventory (BDI) and a two-question case-finding instrument (TQI) for depression screening. Afterwards, we examined the specificity and sensitivity of the screening procedure for identification of both workers with depression and those with comorbid disorders. The current study is a continuation of the preliminary research conducted in 2003.19 In addition to the larger sample size used in the current study, we evaluated the receiver operating characteristic (ROC) curves and Youden Indices in order to calculate the optimal cut-off point for depression in the workplace.
Materials and methods
Participants
We selected two groups of participants. Group 1 was established in order to investigate the optimal pair of cut-off scores of BDI and TQI for screening of depression. Participants in group 1 answered both BDI and TQI, and their diagnosis was confirmed using the M.I.N.I.20 The M.I.N.I. Japanese version was used as a diagnostic standard for identifying cases. Recruitment occurred between January 2001 and February 2004, and it included 90 workers in a company who agreed to participate. One (1.1%) participant did not complete the questionnaires; 89 (98.8%) took part in the study. The mean age of them was 38.4 (SD, 6.6) and 81 (91.0%) were men.
Group 2 was established in order to investigate the sampling bias in the distribution of depression severity among group 1, which was a relatively small sample size. In group 2, a large number of subjects were necessary; therefore, only BDI and TQI were performed and the M.I.N.I. assessment was omitted. Recruitment occurred between July 2000 and February 2004, and 1591 workers from three companies agreed to participate. All the employees in the companies were invited to participate in the study. Ninety-one (5.7%) participants did not complete the questionnaire; 1500 (94.2%) took part in the study. The mean age of them was 40.9 (SD, 7.2) and 1408 (93.9%) were men. Demographic data of participants in each group are shown in supplementary table 1.
Measurements
Beck Depression Inventory
The BDI, developed by Beck et al,21 is one of the most widely used self-rating questionnaires for measuring the severity of depression. The BDI-I is a 21-item scale (range 0–60). We used the Japanese version of BDI-I, which has been validated and is widely used in Japan.22
Two-question case-finding instrument
A two-question depression-screening tool developed by Whooley et al was extracted from the Primary Care Evaluation of Mental Disorders questionnaire.23 24 It includes two questions about depressed mood and anhedonia: (1) ‘During the past month, have you often been bothered by feeling down, depressed, or hopeless?’ and (2) ‘During the past month, have you often been bothered by little interest or pleasure in doing things?’ The TQI operates in the range of many other validated depression-screening tools, and it eases the burden of administration by being succinct. For the two-question instrument, a ‘yes’ answer to either of the two questions was considered to indicate a positive result.
After obtaining consent from the author of the original work, the original TQI was carefully translated into Japanese. The semantic fidelity of the Japanese version of TQI was ascertained by means of back translation, whereby the first Japanese version was translated back into English by an independent researcher blind to the original English version, and any discrepancies between the original and the retranslations were corrected until the two were semantically equivalent.
Criterion standard
The M.I.N.I. is a short structured diagnostic interview, developed jointly by psychiatrists and clinicians in the USA and Europe, for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition and International Classification of Diseases, Tenth Edition psychiatric disorders.20 With an administration time of approximately 15 min, M.I.N.I. was designed to meet the need for a short but accurate structured psychiatric interview for multicenter clinical trials and epidemiology studies and to be used as a first step in outcome tracking in non-research clinical settings. Trained psychiatrists and clinical psychologists performed the Japanese version of M.I.N.I. structured interview, and the results were used to validate the optimal pair of cut-off scores of BDI and TQI.
Study design and procedure
In group 1, participants were assessed by BDI and TQI and then they were additionally diagnosed using the M.I.N.I. In group 2, only BDI and TQI assessments were performed. Subsequently, we investigated the frequency distributions of BDI and TQI in two groups and compared them to confirm that there were no significant differences between the two experimental groups. After confirming that group 1 was not a biased sample, we explored the optimal pair of cut-off scores of BDI and TQI for identifying workers with depression.
The frequency distributions of BDI and TQI were compared using Mann–Whitney U test (p<0.05) to examine whether there were statistically significant differences between the two groups. The sensitivity (Se), specificity (Sp) and positive predictive value (PPV) were calculated for all possible cut-off scores for BDI, TQI and all possible pairs of cut-off scores of BDI and TQI to identify workers with depression in group 1. Sensitivity refers to the proportion of correctly identified cases and specificity to the proportion of correctly identified non-cases. PPV is the probability that depressed workers identified using the optimal cut-off score are cases according to the M.I.N.I.
To determine the optimal cut-off point, the ROC curve was created for all possible cut-off scores of BDI, TQI and all possible pairs of cut-off scores of BDI and TQI. The Youden Indices were calculated, concurrently. The ROC curve is a popular graphical method of displaying the discriminatory accuracy of a diagnostic test for distinguishing between two populations. The ROC curve is a plot of Se and 1−Sp for all possible cut-off scores of the test. To evaluate the discriminatory ability of a diagnostic test, it is common to summarise the information of the ROC curve into a single global value or index.25 The Youden Index is the easiest to apply and frequently used in practice. This index can be defined as {Se + Sp − 1} and provides a criterion for the ‘optimal’ threshold value; the threshold value for which Se + Sp−1 is maximised.26
Furthermore, we applied the screening thresholds to identify workers with comorbid disorders in addition to those with depression. The Se, Sp and PPV were calculated for all possible cut-off scores for BDI, TQI and all possible pairs of cut-off scores of BDI and TQI to identify both workers with depression and those with comorbid disorders. Subsequently, the ROC curve was created and the Youden Indices were calculated.
Results
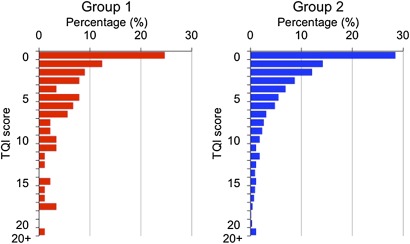
The frequency distributions of BDI and TQI in each group are presented in figure 1 and table 1, respectively. Mann–Whitney U test revealed that there was no significant difference in the frequency distribution of BDI between the two groups. However, significant difference was found in the frequency distributions of TQI between two groups (p=0.003). The diagnoses of the participants in group 1 based on M.I.N.I. are listed in table 2.
Figure 1.
Frequency distribution.
Table 1.
Frequency distributions of two-question case-finding instrument
| Number of ‘yes’ answers | Group 1 | Group 2 |
| N (%) | N (%) | |
| 0 | 51 (57.3) | 1097 (73.1) |
| 1 | 25 (28.1) | 229 (15.3) |
| 2 | 13 (14.6) | 174 (11.6) |
Table 2.
The diagnoses of participants in group 1 according to mini-international neuropsychiatric interview
| Diagnosis | N (%) |
| No diagnosis | 60 (67.4) |
| Substance use disorder | 16 (17.9) |
| Anxiety disorder | 6 (6.7) |
| Major depressive disorder | 3 (3.3 |
| Bipolar disorder | 1 (1.1) |
| Dysthymia | 1 (1.1) |
| Bipolar disorder + substance use disorder | 1 (1.1) |
| Major depressive disorder + substance use disorder + anxiety disorder | 1 (1.1) |
The sensitivity, specificity and PPV for all possible cut-off scores of BDI, TQI and all possible pairs of cut-off scores of BDI and TQI to identify workers with depression are listed in table 3. The ROC curves are showed in supplementary figure 1, and the Youden Indices are listed in table 3. The maximum value of the Youden Index was derived from neither BDI nor TQI alone but the combination of the BDI and TQI: 0.776 at the point of BDI score ≥10 and TQI score =2. The pair of scores of BDI ≥10 and TQI =2 was considered to be optimal to identify workers with depression; both those whose BDI score was ≥10 and those whose TQI score was =2 were defined as ‘cases’.
Table 3.
The sensitivity, specificity, PPV and Youden Indices for all possible cut-off scores for BDI, TQI and all possible pairs of cut-off scores of BDI and TQI to identify workers who were diagnosed with major depressive disorder
| Sensitivity | Specificity | PPV | Youden Index | |
| BDI cut-off score | ||||
| 4 | 100 | 56.4 | 9.7 | 0.564 |
| 5 | 100 | 60.0 | 10.5 | 0.600 |
| 6 | 75.0 | 67.0 | 9.6 | 0.420 |
| 7 | 75.0 | 74.1 | 12.0 | 0.491 |
| 8 | 75.0 | 80.0 | 15.0 | 0.550 |
| 9 | 75.0 | 82.3 | 16.6 | 0.573 |
| 10 | 75.0 | 84.7 | 18.7 | 0.597 |
| 11 | 50.0 | 87.0 | 15.3 | 0.370 |
| 12 | 50.0 | 90.5 | 20.0 | 0.405 |
| 13 | 50.0 | 91.7 | 22.2 | 0.417 |
| 14 | 50.0 | 92.9 | 25.0 | 0.429 |
| 15 | 50.0 | 92.9 | 25.0 | 0.429 |
| 16 | 25.0 | 94.1 | 16.6 | 0.191 |
| 17 | 25.0 | 95.2 | 20.0 | 0.202 |
| 18 | 0 | 98.8 | 25.0 | 0.214 |
| TQI cut-off score | ||||
| 1 | 100 | 60.0 | 10.5 | 0.600 |
| 2 | 75.0 | 88.2 | 23.0 | 0.632 |
| BDI | TQI | Sensitivity | Specificity | PPV | Youden Index |
| Pairs of cut-off scores | |||||
| 4 | 2 | 100 | 56.4 | 9.7 | 0.564 |
| 5 | 2 | 100 | 60.0 | 10.5 | 0.600 |
| 6 | 2 | 100 | 65.8 | 12.1 | 0.658 |
| 7 | 2 | 100 | 72.9 | 14.8 | 0.729 |
| 8 | 2 | 100 | 75.2 | 16.0 | 0.752 |
| 9 | 2 | 100 | 76.4 | 16.6 | 0.764 |
| 10 | 2 | 100 | 77.6 | 17.3 | 0.776 |
| 11 | 2 | 75.0 | 80.0 | 15.0 | 0.550 |
| 12 | 2 | 75.0 | 82.3 | 16.6 | 0.573 |
| 13 | 2 | 75.0 | 82.3 | 16.6 | 0.573 |
| 14 | 2 | 75.0 | 83.5 | 17.6 | 0.585 |
| 15 | 2 | 75.0 | 83.5 | 17.6 | 0.585 |
| 16 | 2 | 75.0 | 84.7 | 18.7 | 0.597 |
| 17 | 2 | 75.0 | 85.8 | 20.0 | 0.608 |
| 18 | 2 | 75.0 | 87.0 | 21.4 | 0.620 |
| 4 | 1 | 100 | 47.0 | 8.1 | 0.470 |
| 5 | 1 | 100 | 49.4 | 8.5 | 0.491 |
| 6 | 1 | 100 | 52.9 | 9.0 | 0.529 |
| 7 | 1 | 100 | 55.2 | 9.5 | 0.552 |
| 8 | 1 | 100 | 56.4 | 9.7 | 0.564 |
| 9 | 1 | 100 | 56.4 | 9.7 | 0.564 |
| 10 | 1 | 100 | 56.4 | 10.0 | 0.576 |
| 11 | 1 | 100 | 57.6 | 10.0 | 0.576 |
| 12 | 1 | 100 | 57.6 | 10.5 | 0.600 |
| 13 | 1 | 100 | 60.0 | 10.5 | 0.600 |
| 14 | 1 | 100 | 60.0 | 10.5 | 0.600 |
| 15 | 1 | 100 | 60.0 | 10.5 | 0.600 |
| 16 | 1 | 100 | 60.0 | 10.5 | 0.600 |
| 17 | 1 | 100 | 60.0 | 10.5 | 0.600 |
| 18 | 1 | 100 | 60.0 | 10.5 | 0.600 |
BDI, Beck Depression Inventory; PPV, positive predictive value; TQI, two-question case-finding instrument.
The sensitivity, specificity and PPV at all possible cut-off scores for BDI, TQI and all possible pairs of cut-off scores of BDI and TQI to identify both workers with depression and those with comorbid disorders are listed in table 4. The ROC curves are showed in supplementary figure 2, and the Youden Indices are listed in table 4. The maximum value of the Youden Index was derived from neither BDI nor TQI alone but from the combination of BDI and TQI: 0.316 at the point of BDI score ≥9 and TQI =2. The combination of BDI ≥10 and TQI =2, which was considered to be optimal to identify workers with depression, showed the Youden Index of 0.281 to identify both workers with depression and those with comorbid disorders. There was little difference in the Youden Index between the two points, and the primary purpose of this screening was to identify workers with depression; therefore, the pair of scores of BDI ≥10 and TQI =2 would be adequate to identify both workers with depression and those with comorbid disorders.
Table 4.
The sensitivity, specificity, PPV and Youden Indices for all possible cut-off scores for BDI, TQI, and all possible pairs of cut-off scores BDI and TQI to identify both workers who were diagnosed as having MDD and those who were not diagnosed as having MDD but had other psychiatric disorders frequently comorbid with MDD
| Sensitivity | Specificity | PPV | Youden Index | |
| BDI cut-off score | ||||
| 4 | 62.0 | 61.6 | 43.9 | 0.237 |
| 5 | 58.6 | 65.0 | 44.7 | 0.236 |
| 6 | 51.7 | 73.3 | 48.3 | 0.250 |
| 7 | 44.8 | 80.0 | 52.0 | 0.248 |
| 8 | 41.3 | 86.6 | 60.0 | 0.280 |
| 9 | 41.3 | 90.0 | 66.6 | 0.313 |
| 10 | 37.9 | 91.6 | 68.7 | 0.295 |
| 11 | 31.0 | 93.3 | 69.2 | 0.243 |
| 12 | 27.5 | 96.6 | 80.0 | 0.242 |
| 13 | 27.5 | 98.3 | 88.8 | 0.259 |
| 14 | 24.1 | 98.3 | 87.5 | 0.224 |
| 15 | 24.1 | 98.3 | 87.5 | 0.224 |
| 16 | 17.2 | 98.3 | 83.3 | 0.155 |
| 17 | 13.7 | 98.3 | 80.0 | 0.121 |
| 18 | 10.3 | 98.3 | 75.0 | 0.086 |
| TQI cut-off score | ||||
| 1 | 48.2 | 60.0 | 36.8 | 0.082 |
| 2 | 20.2 | 88.3 | 46.1 | 0.090 |
| BDI | TQI | Sensitivity | Specificity | PPV | Youden Index |
| Pairs of cut-off scores | |||||
| 4 | 2 | 62.0 | 61.6 | 43.9 | 0.237 |
| 5 | 2 | 58.6 | 65.0 | 44.7 | 0.236 |
| 6 | 2 | 55.1 | 71.6 | 48.4 | 0.268 |
| 7 | 2 | 48.2 | 78.3 | 51.8 | 0.266 |
| 8 | 2 | 48.2 | 81.6 | 56.0 | 0.299 |
| 9 | 2 | 48.2 | 83.3 | 58.3 | 0.316 |
| 10 | 2 | 44.8 | 83.3 | 56.5 | 0.281 |
| 11 | 2 | 37.9 | 85.0 | 55.0 | 0.229 |
| 12 | 2 | 34.4 | 86.6 | 55.5 | 0.211 |
| 13 | 2 | 34.4 | 86.6 | 55.5 | 0.211 |
| 14 | 2 | 31.0 | 86.6 | 52.9 | 0.177 |
| 15 | 2 | 31.0 | 86.6 | 52.9 | 0.177 |
| 16 | 2 | 27.5 | 86.6 | 50.0 | 0.142 |
| 17 | 2 | 24.1 | 86.6 | 46.6 | 0.108 |
| 18 | 2 | 20.6 | 86.6 | 42.8 | 0.073 |
| 4 | 1 | 62.0 | 48.3 | 36.7 | 0.104 |
| 5 | 1 | 58.6 | 50.0 | 36.1 | 0.086 |
| 6 | 1 | 58.6 | 55.0 | 38.6 | 0.136 |
| 7 | 1 | 55.1 | 56.6 | 38.0 | 0.118 |
| 8 | 1 | 55.1 | 58.3 | 39.0 | 0.135 |
| 9 | 1 | 55.1 | 58.3 | 39.0 | 0.135 |
| 10 | 1 | 51.7 | 58.3 | 37.5 | 0.100 |
| 11 | 1 | 48.2 | 58.3 | 37.5 | 0.100 |
| 12 | 1 | 48.2 | 60.0 | 36.8 | 0.082 |
| 13 | 1 | 48.2 | 60.0 | 36.8 | 0.082 |
| 14 | 1 | 48.2 | 60.0 | 36.8 | 0.082 |
| 15 | 1 | 48.2 | 60.0 | 36.8 | 0.082 |
| 16 | 1 | 48.2 | 60.0 | 36.8 | 0.082 |
| 17 | 1 | 48.2 | 60.0 | 36.8 | 0.082 |
| 18 | 1 | 48.2 | 60.0 | 36.8 | 0.082 |
BDI, Beck Depression Inventory; MDD, major depressive disorder; PPV, positive predictive value; TQI, two-question case-finding instrument.
Discussion
The present study revealed that combined implementation of BDI and TQI is useful to screen for depressed workers, and the optimal pair of cut-off scores is a BDI score ≥10 and a TQI score =2. Furthermore, all diagnosed workers in our sample were considered to be depressed because substance use disorder and anxiety disorder are frequently comorbid with depression and patients with bipolar disorder and dysthymia often experience depression. Our results also suggest that it is also possible to identify workers who are likely to be depressed using two instruments with the cut-off scores; therefore, the combination use is considered to be effective as a screening tool in the workplace.
Several studies have investigated the cut-off point of BDI in general populations and failed to get consistent results.13 21 Furthermore, there has been no study that investigated optimal cut-off scores of BDI and TQI in the workplace. Beck suggested that a total score of <10 is not associated with depressive disorders; scores between 10 and 18 indicate mild to moderate depression; scores between 19 and 29 correlate with moderate and severe depression and scores of more than 30 indicate severe depression. Indeed, a BDI score ≥10 has been selected as a cut-off in many studies.27–29 However, Lasa et al29 reported that a BDI score ≥13 had high sensitivity and specificity for detecting depression and was an optimal cut-off in a general population. We speculate that the difference between the cut-off detected in our study and that reported in the previous study is related to differences between the two study populations. Specifically, almost half of the participants in the Lasa study were women (50.16%) and a high BDI score (≥13) was more common among women than men. However, as the majority of participants in the current study were men, difference in terms of gender composition might have contributed to the low cut-off score of BDI in this study as compared with that in the Lasa study. In our study, better sensitivity and specificity was achieved by an additional use of TQI. TQI is less time consuming; therefore, the combination use of BDI and TQI as a screening tool in the workplace is considered to be reasonable, especially for companies with large numbers of employees.
Several important limitations of our study design should be considered when interpreting the results. In particular, the facts that our sample size was relatively small and the vast majority of the participants were men may affect the precision of calculated estimates based on the data presented in our study. We conducted additional analyses in the men-only sample and presented the results in the supplementary materials (supplementary tables 2, 3, 4 and 5 and supplementary figures 3, 4 and 5). Other methodological problems are as follows: the Japanese version of TQI has not been validated and the MINI interview was not performed in the larger group. Validation of the Japanese version of TQI would have contributed to improve accuracy of the present results. Performing the diagnostic interview even in shorter versions of MINI in the larger group would have contributed to increase the number of subjects for analysis. Moreover, a statistically significant difference was found in the frequency distribution of TQI between groups 1 and 2, although there was no significant difference in BDI between the two groups. The score range of BDI is wide (0–60), and it has been proved that BDI can be used as a measure of depression symptom severity. On the other hand, the score range of TQI is 0–2, and TQI is considered to be a tool that can help to make the diagnosis of depression, but not to evaluate symptom severity. Therefore, BDI is thought to be suitable to compare the distributions of severity of depression, whereas the difference in the frequency distributions of TQI would be negligible. Finally, no data of the socio-economical status were collected in this study; therefore, effect of socio-economical factors was not included in the analyses.
We conclude that combined application of BDI and TQI is an efficient way to identify not only workers who are depressed but also those who are likely to be depressed in the workplace. Although further investigations using larger samples are needed, the BDI and TQI combination is a useful screening tool, especially for big companies that have many employees.
Supplementary Material
Footnotes
To cite: Adachi Y, Aleksic B, Nobata R, et al. Combination use of Beck Depression Inventory and two-question case-finding instrument as a screening tool for depression in the workplace. BMJ Open 2012;2:e000596. doi:10.1136/bmjopen-2011-000596
Contributors: YA, BA, KY and NO substantially contributed to conception and design, acquisition of data or analysis and interpretation of data. YA, BA, RN, TS, KY, YO and NO drafted the article or revising it critically for important intellectual content. YA, BA, RN, TS, KY, YO and NO provided final approval of the version to be published.
Funding: Funding for this study was provided by research grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan and the Ministry of Health, Labor and Welfare of Japan.
Competing interests: None.
Ethics approval: This study was approved under the guidelines for epidemiological studies by the Nagoya University Graduate School of Medicine and Nagoya University Hospital Ethics Review Committee and was conducted in accordance with the Helsinki Declaration. Written informed consent was obtained from each subject before the start of the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no additional data available.
References
- 1.Greenberg PE, Kessler RC, Birnbaum HG, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry 2003;64:1465–75 [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003;289:3095–105 [DOI] [PubMed] [Google Scholar]
- 3.Sobocki P, Jonsson B, Angst J, et al. Cost of depression in Europe. J Ment Health Policy Econ 2006;9:87–98 [PubMed] [Google Scholar]
- 4.Kawakami N, Takeshima T, Ono Y, et al. Twelve-month prevalence, severity, and treatment of common mental disorders in communities in Japan: preliminary finding from the World Mental Health Japan Survey 2002-2003. Psychiatry Clin Neurosci 2005;59:441–52 [DOI] [PubMed] [Google Scholar]
- 5.Tokuyama M, Nakao K, Seto M, et al. Predictors of first-onset major depressive episodes among white-collar workers. Psychiatry Clin Neurosci 2003;57:523–31 [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Health Labour and Welfare The Annual Societal Cost of Suicide and Depression. 2010. http://www.mhlw.go.jp/stf/houdou/2r9852000000qvsy.html [Google Scholar]
- 7.World Health Organization Information on Mental Health Disorders Management: Depression. 2006. http://www.who.int/mental_health/management/depression/definition/en [Google Scholar]
- 8.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3:e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patten SB, Wang JL, Williams JV, et al. Descriptive epidemiology of major depression in Canada. Can J Psychiatry 2006;51:84–90 [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Barber C, Birnbaum HG, et al. Depression in the workplace: effects on short-term disability. Health Aff (Millwood) 1999;18:163–71 [DOI] [PubMed] [Google Scholar]
- 11.Alonso J, Angermeyer MC, Bernert S, et al. Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand 2004;109(Suppl 420):38–46 [DOI] [PubMed] [Google Scholar]
- 12.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:629–40 [DOI] [PubMed] [Google Scholar]
- 13.Young AS, Klap R, Sherbourne CD, et al. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry 2001;58:55–61 [DOI] [PubMed] [Google Scholar]
- 14.Shapiro RW, Keller MB. Initial 6-month follow-up of patients with major depressive disorder. A preliminary report from the NIMH collaborative study of the psychobiology of depression. J Affect Disord 1981;3:205–20 [DOI] [PubMed] [Google Scholar]
- 15.Ionescu R, Popescu C, Jipescu I. Predictors of outcome in depression. Rom J Neurol Psychiatry 1994;32:153–73 [PubMed] [Google Scholar]
- 16.Hirschfeld RM, Russell JM, Delgado PL, et al. Predictors of response to acute treatment of chronic and double depression with sertraline or imipramine. J Clin Psychiatry 1998;59:669–75 [DOI] [PubMed] [Google Scholar]
- 17.de Diego-Adelino J, Portella MJ, Puigdemont D, et al. A short duration of untreated illness (DUI) improves response outcomes in first-depressive episodes. J Affect Disord 2010;120:221–5 [DOI] [PubMed] [Google Scholar]
- 18.Okuda A, Suzuki T, Kishi T, et al. Duration of untreated illness and antidepressant fluvoxamine response in major depressive disorder. Psychiatry Clin Neurosci 2010;64:268–73 [DOI] [PubMed] [Google Scholar]
- 19.Suzuki T, Nobata A, Kim N, et al. Evaluation of questionnaires (Two-question case-finding instrument and beck depression inventory) as a tool for screening and Intervention of depression in work Place. Seishinigaku 2003;45:699–708 [Google Scholar]
- 20.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59(Suppl 20):22–33 [PubMed] [Google Scholar]
- 21.Beck AT, Beamesderfer A. Assessment of depression: the depression inventory. Mod Probl Pharmacopsychiatry 1974;7:151–69 [DOI] [PubMed] [Google Scholar]
- 22.Hazama N. Validation of the Japanese version of beck depression Investory (BDI). The Kyushu Neuro-psychiatry 1989;35:28–32 [Google Scholar]
- 23.Whooley MA, Avins AL, Miranda J, et al. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med 1997;12:439–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994;272:1749–56 [PubMed] [Google Scholar]
- 25.Greiner M, Pfeiffer D, Smith RD. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med 2000;45:23–41 [DOI] [PubMed] [Google Scholar]
- 26.Youden WJ. Index for rating diagnostic tests. Cancer 1950;3:32–5 [DOI] [PubMed] [Google Scholar]
- 27.Ahola K, Honkonen T, Kivimaki M, et al. Contribution of burnout to the association between job strain and depression: the health 2000 study. J Occup Environ Med 2006;48:1023–30 [DOI] [PubMed] [Google Scholar]
- 28.Aben I, Verhey F, Lousberg R, et al. Validity of the beck depression inventory, hospital anxiety and depression scale, SCL-90, and hamilton depression rating scale as screening instruments for depression in stroke patients. Psychosomatics 2002;43:386–93 [DOI] [PubMed] [Google Scholar]
- 29.Lasa L, Ayuso-Mateos JL, Vazquez-Barquero JL, et al. The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis. J Affect Disord 2000;57:261–5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.