Abstract
Objective
To describe a framework for visualizing the perineal body's complex anatomy using thin-slice MR imaging.
Study Design
Two mm-thick MR images were acquired in 11 women with normal pelvic support and no incontinence/prolapse symptoms. Anatomic structures were analyzed in axial, sagittal and coronal slices. 3-D models were generated from these images.
Results
Three distinct perineal body regions are visible on MRI: (1) a superficial region at the level of the vestibular bulb, (2) a mid region at the proximal end of the superficial transverse perineal muscle, and (3) a deep region at the level of the midurethra and puborectalis muscle. Structures are best visualized on axial scans while cranio-caudal relationships are appreciated on sagittal scans. The 3-D model further clarifies inter-relationships.
Conclusion
Advances in MR technology allow visualization of perineal body anatomy in living women and development of 3D models which enhance our understanding of its three different regions: superficial, mid and deep.
Keywords: perineal body, pelvic floor anatomy, posterior wall, MR imaging
Introduction
The perineal body is an anatomical structure encountered daily by obstetricians and gynecologists. Known to some as the “anchor of the pelvis,” its components have long been debated in the literature in cadaver dissections and histological studies [1-7]. Like the word “shoulder” which describes a distinct region of the body recognizable by most, the words “perineal body” would cause most to point to the region between the vagina and anus. But the question remains, what structures are involved in that region? Is there a distinct, identifiable structure called the perineal body, or is it made up of its component pieces all traversing or inserting into this region?
Understanding the relationships of its components is crucial for successful obstetrical laceration and fistula repairs, in addition to other procedures such as perineocele repair. (Figure 1) In this study, we sought to utilize advanced thin-slice MR images of living women to identify structures within the perineal body region, define their 3 dimensional location, and provide a framework for visualizing this region's complex anatomy.
Figure 1. Building 3-D Model.
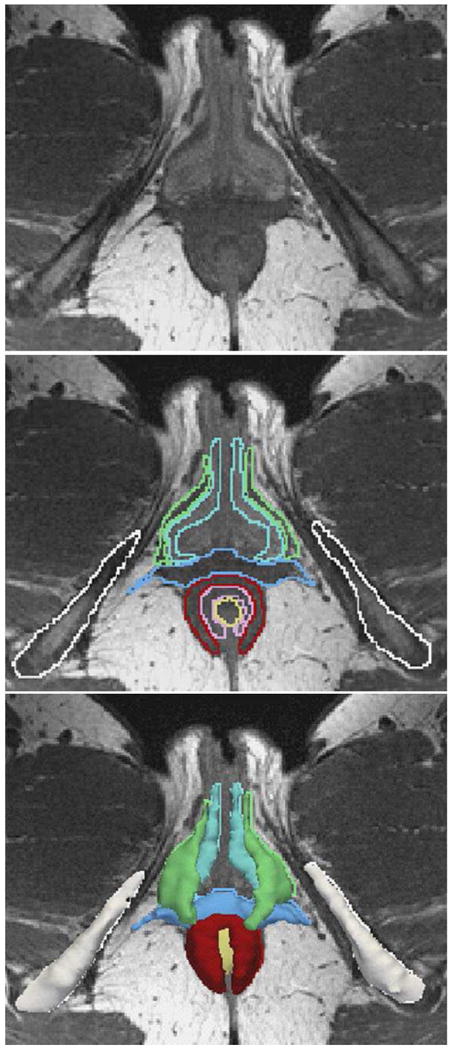
Top: axial image at level of vestibular bulb (VB). Middle: Outlines of structures including pelvic bones (white), VB (turquoise), bulbo-sponsiosus (BS, green), superficial transverse perineal (SPT, blue), external anal sphincter (EAS, red), internal anal sphincter (IAS, pink), and rectum (R, yellow). Bottom: 3-D model on MRI. © DeLancey 2010.
Materials and Methods
Thin-slice MRI scans were performed on 11 women (all controls) in an on-going University of Michigan institutional review board-approved (IRB # 1999-0395), case-control study of pelvic organ prolapse. Control group women were asymptomatic based on Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaires (PFIQ), had negative full bladder stress tests, had not had previous surgery for pelvic floor disorders, and had POP-Q (Pelvic Organ Prolapse Quantification system) points at least 1 cm above the hymenal ring. Women were recruited by newspaper advertisements and matched for age, race and parity with study subjects.
Each woman underwent supine MR imaging at rest using a 3 Telsa Philips Achieva scanner (Philips Medical Systems, Best, The Netherlands) with a 6 channel phased array coil. Turbo spin echo (TSE) techniques were used to image the sagittal, coronal, and axial planes. Thirty images were obtained in each plane (repetition time (TR) range 2300-3000, echo time (TE) 30, 0.2 mm gap for 2 mm slices and 1 mm gap for 5 mm slices, NSA 2, 256 × 255). To maximize visibility of small perineal body structures, 2 mm thick multi-planar proton density MR images were acquired in axial and coronal planes.
Utilizing Oh and Kark's description of the female perineal body location [3], individual structures were identified the region bounded anteriorly by the posterior vaginal wall and posteriorly by the anterior anal wall on axial, sagittal and coronal scans. The longitudinal extent of the perineal body region was defined as extending from the superficial transverse perineal muscle and external anal sphincter to the fusion of the longitudinal muscle of the rectum with the internal anal sphincter which occurs at the caudal extent of the rectovaginal space [1]. The structures were consistently identified by two different observers with oversight by the senior author. Images were reviewed and a representative subject selected for the clarity of her anatomy from whom to generate a computer model of this region using 3-D Slicer® program (version 2.1b1, Brigham and Women's Hospital, Boston, MA). The original 2-mm axial and coronal DICOM (Digital Imaging and Communications in Medicine) images were aligned, ensuring that structures co-localized in these axes by simultaneous review of scan planes in the viewer. A 3-D model was made of the pelvic bones, bladder, urethra, vagina, rectum, and perineal body structures by tracing the structure outlines on axial images and creating 3-D models from these outlines (Figure 1). Each structure was validated by overlaying the model with original source images in orthogonal planes. Although only one model was made for demonstration purposes, observations were based on all 11 subjects.
Names conforming to Terminologia Anatomica [8] were used except for the levator ani muscles where we have chosen the term “pubovisceral muscle” rather than “pubococcygeal muscle” to more accurately reflect its insertions [9]. As described by Kearney [9], the components of the pubovisceral muscle are the same as those referenced in theTerminologia Anatomica [8] for the pubococcygeal muscle: the pubovaginalis, puboperinealis, and pubo-analis.
Results
The mean age of the 11 study participants was 61 ± 10 years (SD), mean body mass index (BMI) was 24.8 ± 4.7 kg/m2, median parity was 2, and 91% were Caucasian. Pelvic organ prolapse quantification points (POP-Q) are shown along with the demographics in Table 1. No subject reported having a significant obstetrical laceration with their deliveries. No subject had undergone a hysterectomy or pelvic organ prolapse surgery. None had pelvic floor dysfunction symptoms as determined by responses to validated questionnaires (PFDI and PFIQ).
Table 1. Demographics.
| Characteristics | Study Population (n=11) |
|---|---|
| Age (yrs)* | 60 ± 10 |
| BMI (kg/m2)* | 24.8 ± 4.7 |
| Median parity | 2 |
| Caucasian* | 10 (91%) |
| POP-Q* | |
| Ba | -1.8 ± 0.8 |
| C | -5.8 ± 1.4 |
| Bp | -1.8 ± 0.6 |
| GHrest | 2.8 ± 1.0 |
| PBrest | 3.2 ± 1.3 |
| Hysterectomy* | 0 (0%) |
mean ± standard deviation or n (%)
Perineal body structures are best visualized in the axial plane, revealing three distinct regions: superficial, mid and deep. In the superficial portion at the level of the vestibular bulb (VB), the bulbospongiosus (BS) inserts into the lateral margins of the perineal body, while the superficial transverse perineal muscle (STP) and external anal sphincter (EAS) traverse the region (Figure 2, panels -1.8 to -0.6). In the perineal body's mid-region at the proximal end of the superficial transverse perineal muscle, the puboperinealis muscle (one component of the pubovisceral muscle) inserts into the lateral margins of the perineal body and in some individuals can be seen to cross the midline. This region also contains the distal internal anal sphincter. The pubo-analis muscle is also visible as it inserts in the intersphincteric groove between internal and external anal sphincters (Figure 2, panels 0.0 to +0.4). The pubo-analis muscle and internal anal sphincter extend into the perineal body's most deep region at the level of the midurethra. Here the pubovaginalis muscle also becomes visible as it fuses with the vaginal sidewall, sending fibers posteriorly to the perineal body. In this location, the longitudinal muscle of the rectum may be visible in the midline (Figure 2, starting at panel +0.2 through +0.8). The puborectalis muscle forms a loop behind the rectum at this level, but does not contribute fibers to the perineal body.
Figure 2. Axial MR images showing perineal body (PB) anatomy.
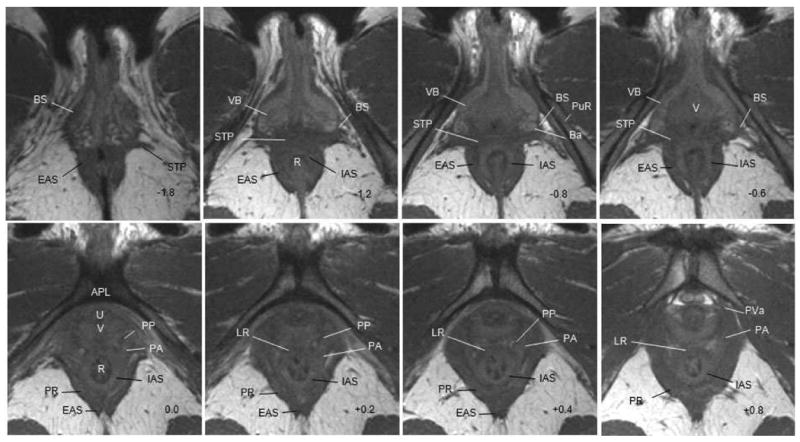
Arcuate pubic ligament (APL) as reference slice. (-) numbers are caudal and (+) numbers cephalad to APL. Abbreviations list: PB-perineal body, B-bladder, U-urethra, V-vagina, R-rectum, PS-pubic symphysis, IC-iliococcygeous, VB-vestibular bulb, PuR-pubic rami, Ba-Bartholins, IAS-internal anal sphincter, PR-puborectalis. Table 2 lists PB component abbreviations. © DeLancey 2010.
While the perineal body's structures are best visualized in the axial plane, cranio-caudal relationships can be appreciated on sagittal images. In the mid-sagittal plane, the perineal body's recognizable pyramidal structure is visible between the vagina and the rectum (Figure 3, panel 0.0). As you move laterally, the perineal membrane is visible above the bulbospongiosus muscle and vestibular bulb in the mid region of the perineal body. The fibers of the pubovisceral muscle extend across the perineal body, while the dorsal portion of the external anal sphincter extends caudal to the perineal body (Figure 3, panel R1.0). These findings as well as the findings on axial images are summarized in Table 2. Even though coronal images can delineate the immediate perianal structures, they are not as helpful for delineating the perineal body region because of the orientation of the anatomy.
Figure 3. Sagittal MR images showing perineal body (PB) anatomy.
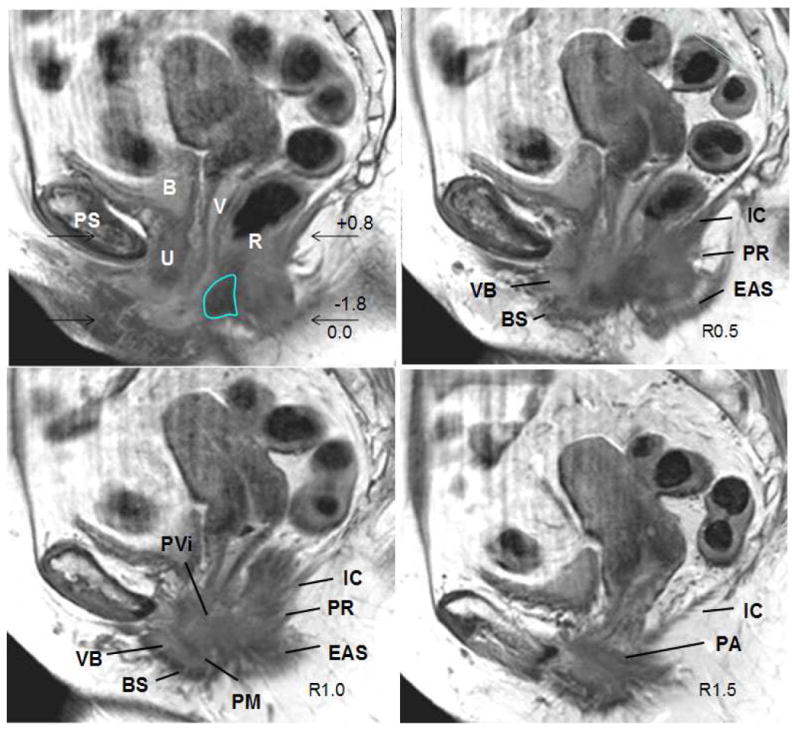
Midsagittal slice as reference slice with “R” to the right. PB outlined in turquoise. Abbreviations list: PB-perineal body, B-bladder, U-urethra, V-vagina, R-rectum, PS-pubic symphysis, IC-iliococcygeous, VB-vestibular bulb, PuR-pubic rami, IAS-internal anal sphincter, PR-puborectalis. Table 2 lists PB component abbreviations. The region that corresponds to the images shown in Figure 2 is indicated, however, please note, this is a different subject than shown in Figure 2 so that minor variations in spatial relationships exist. © DeLancey 2010.
Table 2. Characteristic MR features of the perineal body (PB).
| Structure | Axial (Fig 3) |
Sagittal (Fig 4) |
|---|---|---|
| Superficial | ||
| Superficial Transverse Perineal (STP) | Extends laterally across midline, adjacent to EAS (-1.2 to -0.6); portion visible in -1.8. | Not well seen |
| Bulbospongiosus (BS) | Surrounds vestibular bulb on lateral border (-1.2 to -0.6); portion visible in -1.8. | Caudal to VB with dorsal fibers to PB (R1.0) |
| External Anal Sphincter (EAS) | Crosses midline ventrally, dorsal tear drop shape (-1.2 to +0.4); portion visible in -1.8. | Dorsal portion extends caudal to PB, ventral portion not well seen (R0.5 to R1.0) |
| Mid | ||
| Internal Anal Sphincter (IAS) | Innermost circular muscular layer (-1.2 to +0.8) | Not well seen |
| Pubovisceral portion of levator (PVi) Puboperinealis M. (PP) Pubo-analis M. (PA) | Origins on pubic rami difficult to visualize in these cuts, however, can appreciate fusion with appropriate viscera (0.0 to +0.8) | PVi lateral to midsagittal extending across PB. (R1.0) PA more lateral than PP/PVa. (R1.5) |
| Perineal Membrane (PM) | Not well seen | Cranial to VB, inserting into PB (R1.0) |
| Still present: EAS | ||
| Deep | ||
| Longitudonal Fibers of Rectum (LR) | Ventral to IAS (+0.4 to +0.8) | Not well seen |
| Pubovisceral portion of levator (PVi) Pubovaginalis M. (PVa) | PVa is ventral component of PVi that inserts into vagina (+0.4 - +0.8) | PVi lateral to midsagittal extending across PB. (R1.0) PA more lateral than PP/PVa. (R1.5) |
| Still present: IAS, PA |
Figure 4 illustrates a 3-D model of the perineal body generated from MR images, further clarifying structural inter-relationships and facilitating recognition of the three perineal body regions: superficial, mid and deep. The model helps provide a framework for understanding normal anatomy (Figure 4).
Figure 4. 3D Model of perineal body (PB).
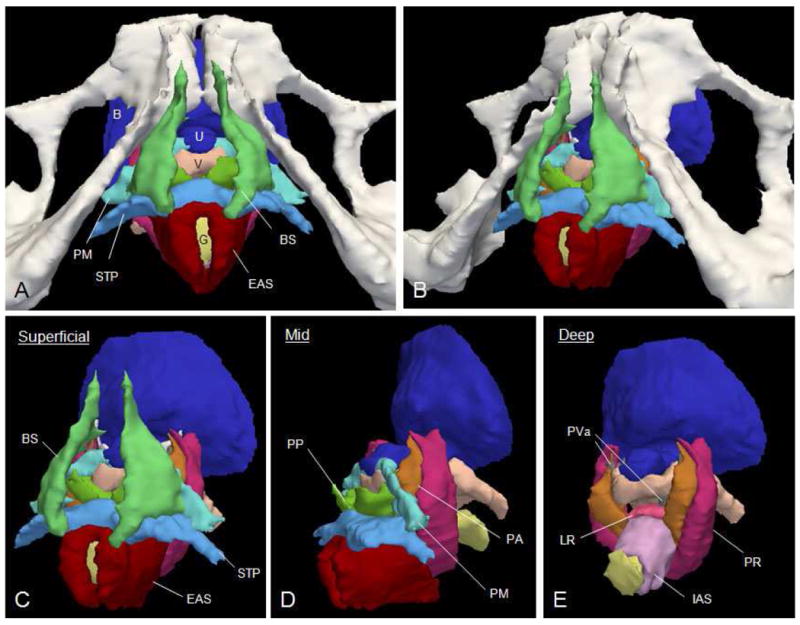
(A) Dorsal lithotomy view and (B) left lateral aspect of same image. With removal of pelvic bones able to better appreciate superficial region (C) with BS, STP and EAS. (D) Lateral view with BS removed to illustrate mid region at proximal STP with PP, PM and PA. With removal of EAS, STP, PP, and PM can visualize deep region (E) with LR, PVa, PA. IAS visible with EAS removed. PVa muscle is barely visible lateral to the vagina in this image. PR-puborectalis, B-bladder, U-urethra, V-vagina, G-GI tract; all other abbreviations in Table 2. © DeLancey 2010.
Comment
This study describes the complex anatomy of the perineal body as seen in thin-slice MR imaging of living women with normal support and no pelvic floor dysfunction. Axial images provide the clearest view of individual structures within this region, while sagittal images illustrate cranio-caudal relationships. This study suggests a novel framework for organization of this region into three parts: superficial, mid and deep. The findings we have described were seen in the scans of all 11 subjects.
Our findings confirm published data from cadaver and histological studies regarding the complexity of the perineal body. Oh [3] describes this region between the “anterior anal wall and the posterior vaginal wall” as a “heavily used traffic center.” He acknowledges the difficulty with dissecting this region, and because of this, supplemented his dissections with histological analysis. Although his article focuses on male anatomy, in the female, he describes a region bounded by the vagina anteriorly, the anterior anal wall posteriorly, and the transverse perinea muscles and external anal sphincter muscles superficially and discusses the difficulties in identifying the proximal “longitudinal” border. Although he describes it as a solid, inseparable musculotendinous mass, our MR images complement his careful work and not only allow visualization of distinct structures within this region but introduce the possibility of generating a 3D model. Axial images allow visualization of the pubovisceral portion of the levator muscle in the perineal region (pubo-analis, puboperinealis and pubovaginalis components) which likely correlate with what Oh describes as the “pubopre-rectal” muscle. Similarly, we show how the puborectalis muscle loops behind the rectum likely helping suspend the perineal body from the pubic bone as described by Oh [3]; however it lies lateral to the iliococcygeal muscle and does not contribute fibers to the perineal body.
Findings of the present study contradict and extend what is currently in the literature by utilizing advances in MR technology to better visualize this region and describe its anatomy. In their MR imaging study of the anal canal and perianal structures, Morren et al describe the female perineal body as “clearly visible as a separate anatomical structure located between the posterior vaginal wall and anterior anal canal.” In addition to the distinct perineal body, they describe the visible superficial transverse perineal muscle as well as a puboperinealis muscle which likely corresponds to our pubovisceral components. It is likely that the stronger MR magnet (3 Tesla vs. 1.5 Tesla) and thinner slices (2 mm vs. 3mm) improved visibility in this region to allow determination of individual components within what Morren recognized as a single structure [2].
In addition, findings of the present study extend what is present in current literature by providing a different approach to organizing the anatomy of this region. In his published cadaveric and histological studies Shafik proposes an approach to dividing the perineal body into three layers: a superficial layer including the EAS, a tendinous extension of STP muscles, and a third layer of tendinous fibers of the deep transverse perineal muscles. In his cadaveric studies a relationship between with the levator ani and perineal body could not be confirmed. This approach is different than our approach to organize the anatomy of the perineal body as it excludes several components of this region visible on our advanced MR imaging, and does include the deep transverse perineal muscles which are not evident in our study [6]. In previous publications, DeLancey discusses how this muscle has now been revised to include the compressor urethra and urethrovaginal sphincter which were not evident as part of that region in our images [1].
Several factors must be considered when interpreting the results of this study. This study was performed on women who were asymptomatic vaginally parous women in whom clinical testing confirmed normal support and questionnaires confirmed absence of pelvic floor dysfunction and known obstetrical laceration. This group represents the majority of women in the reproductive age seen by clinicians. Whether this anatomy is different in nulliparous women deserves further study. The second consideration concerns the impact of missing information not only within the thickness of the MR slices, but also the spaces between each slice. We have tried to minimize this while studying this region's small structures by reducing the slice thickness from the standard 5 mm to 2 mm. Even using these thin slices, the termination fibers and connective tissue which insert into bone are not visible on MR imaging. As a result, our models incorporate the belly of the muscles, but not these insertions. Although this need be kept in mind while viewing the 3-D model, it does not impact identification muscle mass in the perineal body region. Additionally, as described in the results section, the identification of the longitudinal muscle is limited by resolution of this MR technology. Endoanal MR imaging does capture this anal region better because of proximity to the coil [7, 10]. Lastly, this approach to studying anatomy with MR imaging and not histology from cadaveric dissections may seem counterintuitive. However, we would argue that our findings complement Oh's cadaveric and histological studies [3] and offer the benefit that utilizing images of living women minimizes distortion that occurs in cadaveric specimens. In the future, this technique also allows studies to be conducted on women with and without known pelvic organ support defects; something not possible in cadavers.
In summary, this study illustrates how technological advances in MR imaging allow visualization of perineal body anatomy in living women without pelvic floor dysfunction and help to unravel the mystery behind its components. Organization of this region into three parts – superficial, mid and deep – provides a framework for visualizing its normal anatomy. MRI generated 3-D models greatly expand our ability to understand the structural relationships of the complex, yet frequently encountered region. Just as MR imaging is used to direct surgical repairs in the shoulder, by helping us gain insight into normal anatomy, MR imaging of the perineal body moves us one step closer to identifying specific failures and appropriately tailoring surgical repairs in this region of the body as well.
Acknowledgments
We gratefully acknowledge support from the National Institute of Child Health and Human Development Grants R01 HD 38665 with additional investigator support from the Office for Research on Women's Health SCOR on Sex and Gender Factors Affecting Women's Health 1 P50 HD044406.
Footnotes
Poster presentation at the 30th American Urogynecologic Society Meeting, Hollywood, Florida, September 2009.
Dr. John OL DeLancey receives research support from American Medical Systems and is a consultant for Johnson and Johnson. Dr. Dee Fenner receives research support from American Medical Systems. The other authors have no disclosures to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.DeLancey JO. Structural anatomy of the posterior pelvic compartment as it relates to rectocele. Am J Obstet Gynecol. 1999;180(4):815–23. doi: 10.1016/s0002-9378(99)70652-6. [DOI] [PubMed] [Google Scholar]
- 2.Morren GL, Beets-Tan RG, van Engelshoven JM. Anatomy of the anal canal and perianal structures as defined by phased-array magnetic resonance imaging. Br J Surg. 2001;88(11):1506–12. doi: 10.1046/j.0007-1323.2001.01919.x. [DOI] [PubMed] [Google Scholar]
- 3.Oh C, Kark AE. Anatomy of the perineal body. Dis Colon Rectum. 1973;16(6):444–54. doi: 10.1007/BF02588867. [DOI] [PubMed] [Google Scholar]
- 4.Shafik A, Ahmed I, Shafik AA, El-Ghamrawy TA, El-Sibai O. Surgical anatomy of the perineal muscles and their role in perineal disorders. Anat Sci Int. 2005;80(3):167–71. doi: 10.1111/j.1447-073x.2005.00109.x. [DOI] [PubMed] [Google Scholar]
- 5.Shafik A, Shafik IA, el-Sibai O, Shafik AA. Physioanatomical relationship of the external anal sphincter to the bulbocavernosus muscle in the female. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(8):851–6. doi: 10.1007/s00192-006-0246-z. [DOI] [PubMed] [Google Scholar]
- 6.Shafik A, Sibai OE, Shafik AA, Shafik IA. A novel concept for the surgical anatomy of the perineal body. Dis Colon Rectum. 2007;50(12):2120–5. doi: 10.1007/s10350-007-9064-8. [DOI] [PubMed] [Google Scholar]
- 7.Stoker J, Wallner C. The anatomy of the pelvic floor and sphincters. In: Stoker J, Taylor SA, DeLancey JO, editors. Imaging Pelvic Floor Disorders. Second. Germany: Springer; 2008. pp. 19–29. [Google Scholar]
- 8.Federative Committee on Anatomical Terminology. Terminologia Anatomica. New York: Thieme Stuttgart, Germany; 1998. [Google Scholar]
- 9.Kearney R, Sawhney R, DeLancey JO. Levator ani muscle anatomy evaluated by origin-insertion pairs. Obstet Gynecol. 2004;104(1):168–73. doi: 10.1097/01.AOG.0000128906.61529.6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hussain SM, Stoker J, Lameris JS. Anal sphincter complex: Endoanal MR imaging of normal anatomy. Radiology. 1995;197(3):671–7. doi: 10.1148/radiology.197.3.7480737. [DOI] [PubMed] [Google Scholar]


