Abstract
The article illustrates the main features of the concept of medicalization, starting from its theoretical roots. Although it is the process of extending the medical gaze on human conditions, it appears that medicalization cannot be strictly connected to medical imperialism anymore. Other “engines” of medicalization are influential: consumers, biotechnology and managed care. The growth of research and theoretical reflections on medicalization has led to the proposal of other parallel concepts like pharmaceuticalization, genetization and biomedicalization. These new theoretical tools could be useful in the analysis of human enhancement. Human enhancement can be considered as the use of biomedical technology to improve performance on a human being who is not in need of a cure: a practice that is increasingly spreading in what might be defined as a “bionic society”.
Keywords: Bionic society, Biomedicalization, Human enhancement, Medicalization, pharmaceuticalization, Risk
Introduction
The manipulation and transformation of human nature by biomedical technology is increasing. As Foucault (1976[10]) stated in the 1970's the sovereign-power of death (of giving death to people) has been replaced by the power of the State to give and improve life: biopower (and the welfare State is the main example of this). According to the Foucauldian scholar Nikolas Rose, molecular manipulation is the main trait of our society:
The “style of thought” of contemporary biomedicine considers life at the molecular level as a group of intelligible vital mechanisms which can be identified, isolated, manipulated, mobilized and recombined in intervention practices which are not constrained by the apparent normativity of a natural vital order (Rose, 2006, p.9[28]).
Therefore, it can be said that we are living in a society which is becoming increasingly bionic. That is, biology and genetics are seen as the main forces which affect human life, with social factors playing a minor role. Medicalization, and its developments, is the main component of the bionic society of today.
Medicalization can be defined as the process by which some aspects of human life come to be considered as medical problems, whereas before they were not considered pathological. In sociology, medicalization is not a “new” concept. Forty years ago Ivan Illich (1973[17]) made an accurate analysis of the iatrogenesis of many illnesses. The word iatrogenesis comes from the ancient Greek and means “originating from a physician/treatment”. According to Illich, social iatrogenesis is the proliferation of diseases caused by the extension of medical categories on everyday life. One practical example of social iatrogenesis given by Illich is the lowering of levels of tolerance for psychological discomfort or sadness, which brought about a steady increase of the diagnosis of depression (Horwitz and Wakefield, 2009[15]). In the same period, Foucault (1976[10]), considered the process of indefinite medicalization to be one of the main features of society. He stressed the role of doctors in deciding what was normal and what was pathological. In the words of Zola:
From sex to food, from aspirins to clothes, from driving your car to riding the surf, it seems that under certain conditions or in combination with certain other substances or activities or if done too much or too little, virtually anything can lead to medical problems (Zola, 1982, p. 49[34]).
In more recent times, Peter Conrad (Conrad, 2007[8]) has proposed to consider medicalization in three respects:
Conceptual medicalization: When medical lexicon is used to define non-medical entities (for example, the natural drooping of breasts after pregnancy diagnosed as “mammary ptosis”);
Institutional medicalization: When physicians have the power to steer non-medical personnel – what Eliot Freidson called “professional dominance” (Freidson, 1970[11]; for example, physicians being managers of hospitals without having any academic title in management or business administration);
Interactional medicalization: When the physician, in interaction with the patient, redefines a social problem into a medical one (for example, homosexuality was listed as a pathology in the DSM until 1983).
Yet, according to Conrad, there are also other “engines of medicalization”. These engines are consumers, biotechnology and managed care.
Engines of Medicalization
Consumers
Consumers are a factor of medicalization because health is increasingly becoming, and has become, a commodity (Turner, 2004[32]). People are increasingly using medical terminology in order to analyse their own health influenced from watching TV and browsing the internet (Barker, 2008[4]). Also, advertisements encourage people to consider health needs that otherwise they would not have thought about. New social representations of health and illness are emerging, for instance, the representations of idealized beauty and the parallel “treatments” of cosmetic surgery. The body is increasingly considered as a “text” through which people may transmit signals and information (Turner, 2004[32]).
Technology
Technology is a driving factor of medicalization for many reasons. First, new diagnostic tools mean more chances to discover illnesses. Yet, often the risk factors are considered as pathological and therefore treated. Sometimes, the “discovery” of new diseases is done by pharmaceutical firms which also have the “right” treatment (‘disease mongering’).
Managed care
Managed care is also a force of medicalization. For instance, considering depression as a condition caused by a chemical imbalance legitimates a treatment based on pills rather than on expensive psychotherapy (Barker, 2008[4]). On these bases, social problems are transformed into medical ones. In the US, according to Conrad:
It seems likely that physicians prescribe pharmaceutical treatment for psychiatric disorders knowing that these are the types of medical interventions covered under managed care plans, accelerating psychotropic treatments for human problems (Conrad, 2007, p. 141[8]).
In the US, in 1997, laws regulating pharmaceutical advertisement became less restrictive which resulted in the expenditure for prescription drugs ads to increase four times between 1998 and 2007 (Murray, 2009[27]). The increase in advertising has also strongly stimulated disease mongering, which is the “invention of illnesses” (Moynihan e Cassels, 2005[26]). A commonly used strategy in the advertisement for drugs is the overstatement of the risks of certain situations which mislead consumers. People are increasingly encouraged to discover some diseases through a self-diagnosis based on a check-list (Jutel, 2009[18]).
From Medicalization to Pharmaceuticalization?
The use of pharmaceuticals and medicalization are not the same thing. Some aspects of medicalization are not directly connected to the use of drugs: conceptual and interactional medicalization, for instance (Conrad, 2009[7]). Moreover, there are situations of medicalization which do not include the consumption of pharmaceuticals as their main feature, even if pharmaceuticals have been used in those situations. This is the case of the medicalization of death, the medicalization of pregnancy and the medicalization of beauty. There are even pathological conditions in which the treatment is neither a pharmacological one nor a medical one strictly speaking, but require the patient to comply with a specific regimen or way of life. A typical example of this is coeliac disease, which is caused by a reaction to gliadin, a prolamin (gluten protein) found in wheat. At present, the only effective treatment is a life-long gluten-free diet.
According to Abraham (2010[1]), the socio-cultural aspects of pharmaceutical consumption have peculiar features which cannot be properly analysed by the medicalization framework; therefore, he proposes the concept of pharmaceuticalization. Pharmaceuticalization can be defined as “the process by which social, behavioral, or bodily conditions are treated, or deemed to be in need of treatment/intervention, with pharmaceuticals by doctors, patients or both” (Abraham, 2010, p. 290[1]). Main examples include: the treatment of mood by anxiolytics or antidepressants, treatment of ADHD with Methylphenidate (e.g., Ritalin®) and treatment of erectile dysfunction with Sildenafil citrate (e.g., Viagra®). In addition, even the treatment of heart-disease risk factors with cholesterol-lowering drugs, such as statins, may be considered an example of pharmaceuticalization. It should be noted that all the conditions mentioned above could also be treated in non-pharmaceutical ways – as they were in the past. The treatments could be medical, such as a psychotherapy, or non-medical, such as a change in lifestyle.
Among the factors that have fostered pharmaceuticalization, Abraham proposes to consider three main causes: the political economy of the pharmaceutical industry, the deregulatory state ideology, and consumerism. While the concept of consumerism has already been described, the other two factors deserve particular attention.
Abraham (2010, p. 299-301[1]) describes “deregulatory state ideology” as the pharmaceutical legislation in the EU, North America, Australasia that requires manufacturers to demonstrate the quality, safety and efficacy of their products (but not their therapeutic advance) in order to have a new drug approved by regulatory agencies. Therefore, there can be pharmaceutical innovation without therapeutic advance. As stated by Donald Light:
When pharmaceutical companies say a drug is “effective” or “more” “effective,” they usually mean more effective than a placebo, not more effective than existing drugs. (Light, 2010, p.7[19]).
Pharmaceutical companies are increasingly investing in advertising and marketing and decreasing their financial efforts devoted to research for new therapies (Angell, 2004[2]). As said, an important component of marketing campaigns is advertising: “direct-to-consumer advertising does not simply attempt to sell particular products but strives to reshape consumers’ understanding of their problems into conditions that should be treated by medications” (Horwitz, 2010, p.110-111[13]).
It is not only the loosening of advertising restrictions, marketing campaigns and consumerism that foster pharmaceuticalization and medicalization. Science also plays a great role in legitimising this tendency. For example, as it is shown in the next section, the Diagnostic and Statistical Manual of Mental Disorders, by giving the description of many mental disorders in terms of symptoms, strongly suggests pharmaceutical treatments.
Normality and pathology in mental health
Mental health is likely the most medicalized aspect of human life. Emotions like sadness and shyness, if framed through a pathologizing gaze, can easily be turned into illnesses (Maturo, 2010a[22]). It is hard to believe that 6% of the population in Great Britain meet the criteria for major depressive disorder at any time (Scott and Dikey, 2003[29]) and even harder to believe that more that 5% of Americans suffer from bipolar disorder: “Awareness among general practitioners and psychiatrics that the broad clinical spectrum of bipolar disorders probably affects 5% of the population – rather than the often quoted figure of 1% – is regrettably low” (Smith, Ghaemi and Craddock, 2008, p. 398[31]).
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is the commonly used basis for any mental disorder diagnosis. While the first two editions of the DSM were characterized by a strong theoretical view, mainly based on psychoanalysis, DSM-III and, even more, DSM-IV, try to be atheoretical and symptom-based. Thus, in the two last versions of the DSM, the psychiatric nosography became more and more descriptive and standardized, although not value-free (Fulford, 2010[12]). To define an illness, the emphasis was put on symptoms, while causes were neglected. [Of course one may say causes were not neglected; they are simply not known, since ‘etiology unknown’ is still the hall-mark of psychiatry.] The focus of DSM-III and DSM-IV therefore shifted from illnesses to disorders and syndromes – the latter being multiple symptoms. The key-assumption of this “diagnostic psychiatry” is that “overt symptoms indicate discrete underlying diseases. Whenever enough symptoms are present to meet the criteria for a diagnosis, a particular mental disorder exists” (Horwitz, 2002, p. 106[14]). Therefore the main consequences of the latest version of the DSM are reductionism and the proliferation of disorders (by shifting from illnesses to syndromes, the complexity of mental illness is reduced, because it coincides with its symptoms and virtually almost everything may be considered pathological), and the likeliness of pharmaceutical treatment (if disorders become more easily identifiable and cognisable it becomes easier to associate them with a specific therapy, and if the task of psychiatry is to relieve symptoms, then medicines are the best way to do so). This trajectory puts psychiatry together with all the other medical specialties, aligning mental illness with any other kind of biological disease.
It is not possible to demonstrate that corporations are involved in the designing of the DSM, but, in describing the onset of the medicalization of mood, Horwitz and Wakefield present a good point:
There is no evidence that pharmaceutical companies had a role in developing DSM-III diagnostic criteria. Yet, serendipitously, the new diagnostic model was ideally suited to promoting the pharmaceutical treatment of the conditions it delineated (Horwitz and Wakefield, 2007, p.182[16]).
Risk in the Theoretical Discourse
Presently, the concept of risk seems to be very important in contemporary society. According to many scholars we have passed from a society dominated by dangers to a society dominated by risks.
According to Douglas (1992[9]), risks are the outcome of human actions, while dangers have to do with the unpredictability of nature. If damages can be seen as a consequence of a decision of ours then we can speak about risk; if damages are caused by something overcoming our will, something “external”, then we can speak about danger. To use an extreme example: while in the past, falling ill with cancer was a danger, nowadays, thanks to the screening technology, falling ill with cancer has become a risk of a missed prevention. To view it in a different way, Luhmann (1993[21]) wrote that when man discovered the umbrella, rain was not a danger anymore but a risk. Another important feature of risk is calculability: the word “risk” has its origin in the field of insurance, and therefore one of its main connotations is the likeliness of an event to occur.
Risk and health
In the discourse on health, risk may be connected to the individualization of social problems, biological reductionism, and the shifting borders between normal and pathological. As it will be shown in the next pages, it can be easier for political institutions to embrace a clinical and biological definition of a disease instead of addressing the social causes underlying these pathological conditions. Considering illness as an external risk, the responsibility to avoid it is shifted from social policy to the individual, despite pathology being strongly connected to social and economic conditions. Nowadays, health is increasingly considered an individual responsibility. People should avoid smoking, becoming overweight, and they are also encouraged to push back the ageing process as much as possible. Therefore, prevention is socially constructed as an individual duty. Moreover, huge investments in diagnostics and genetics have led to neglect of social causes of diseases, and to consider them only in biological terms (Clarke and Shim, 2011[6]). Although many researchers have demonstrated that in rich countries social determinants are more influential in health status than an increase in health expenditure, social and economic conditions are seldom mentioned in biomedical discourse on health (Link and Phelan, 2010[20]). It is cheaper, and simpler, to label an unruly child as someone suffering from a chemical imbalance instead of taking other factors into account: the possible unemployment of parents, poverty of the neighborhood, or other issues in the family. If we consider depression as the effect of the lack of serotonin in the brain, instead of the natural and normal answer to a condition of deprivation and stress, we implicitly reject the role of social policy. As Barker puts it:
It is far more politically expeditous to make claims on the welfare state (even the miserly US welfare state) to address discrete medical needs of homeless patients, than it is to fulfil the rights of homeless citizens to housing and employment. Again in the US context, it is more politically palatable to expand State Children's Health Insurance Program (SCHIP) than it is to address what sociological research consistently demonstrates to be the single best predictor of children's current and future health status; namely, social class (Barker, 2009, p. 101[3])
Doing so, an individualistic and neoliberal view of society is legitimised, in which the State has increasingly less responsibilities for citizens’ welfare. Moreover, the emphasis on a healthy lifestyle may be misplaced. There is evidence that the “cause of causes” of illness is the socio-economic status (Link and Phelan, 2010[20]). The connection between lifestyle and health, on which the risk-factor model is based, is only one side of the etiological link between health and society. The risk-factor model's explanation for health inequalities proceeds according to a seemingly persuasive logic: “social conditions are related to health because of their influence on a host of risk factors that lie between social conditions and disease in a chain of causality” (Link and Phelan, 2010, p. 3[20]). What is lacking in the risk-factor model is that social and economic conditions powerfully shape the capacity to modify or eliminate identified risk factors. They put people “at risk of risk”. It is difficult to eat expensive organic food if you are unemployed. Perhaps people are not inclined to jog if they live in an urban sprawl close to the junction. And it is easier to quit smoking if you are a member of Harvard soccer team than a member of a gang in a Brazilian slum.
There are two more features of the idea of risk that should be mentioned. The first one is connected to the threshold. One of the most effective ways to widen the pathological sphere is to alter the threshold level. It is by lowering the threshold at which someone is considered “pre-sick” that prevention has been medicalized. The main examples of the medicalization of prevention is hypertension. Blood pressure rises with age and is one of the several factors that can increase the risk of stroke:
But because blood pressure is amenable to drugs, a world of marketing and guidelines developed around it. What constitute “high” blood pressure is open to opinion, and the US guidelines set by expert panels have periodically lowered the criteria so that millions of more people are labelled as ‘having hypertension’, or now ‘prehypertension’, and being ‘at risk’ of heart disease (Light, 2010, p. 22[19]).
The second feature is a distorted idea of causality. An example of this distortion is the concept of genetization: the tendency to consider genes as the main factor responsible for any kind of condition. In this kind of reductionism: “a complex understanding of the causes of human development is displaced by one in which genes are perceived as the ‘true cause’ of difference” (Shostak and Frese, 2010, p. 419[30]). Research has demonstrated that genes are “our destiny” only in a few cases (Maturo, 2009b[25]).
Human Enhancement and Biomedicalization
In the debate on medicalization, a new topic has emerged in the last years: the opportunity of using biotechnology – mainly drugs – not to treat pathology, but to enhance normal conditions. Human enhancement can be defined as the use of biomedical technology to improve (physical, cognitive, emotional or social) performance on a human being who does not need any cure (Maturo, 2009a[24]). Human enhancement is part of the concept of biomedicalization proposed by Clarke and Shim (2011[6]). Biomedicalization differs from the concept of medicalization because it takes into consideration the aspect of human enhancement and also the role of pharmaceuticalization in contemporary society (Cipolla, 2010[5]).
Indeed, the topic of human enhancement has everything to do with the shift of medicine, or a section of it, from the treatment of pathologies to the optimization and possibility of going beyond normality: better than well. Some examples of human enhancement are: prosthetic limbs, cosmetic surgery, and emotional and cognitive enhancement through pharmaceuticals. The line between the medicalization of pathologies and the enhancement of normality is blurred, as there are actions carried out at the borders that do not fall into either category. Moreover, it is likely that the enhanceable of today becomes the pathological of tomorrow, which brings about an ever-broader area in which biomedical interventions are required [Figure 1].
Figure 1.
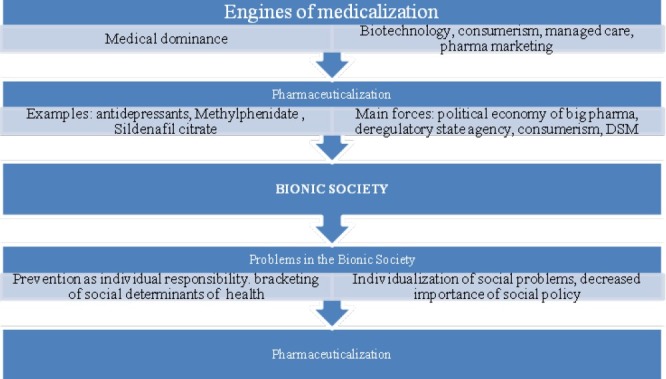
Flowchart of paper
Concluding Remarks: Are we Heading toward a Bionic Society?
The World Health Organization definition's of health as a “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (WHO, 1946[33]) has been often criticized because it proposes an extremely wide and ambitious concept of health. An edenic idea of health! Instead, it seems that today these three dimensions – body, psyche and society – are fully involved in the medicalization process. Moreover, health should be considered more as a “process”, than a state. A process in which “physical, mental and social well-being” is constructed, maintained and rebuilt. An asyntotic process without an end – as biocorporations and advertising know very well.
As already stated, the expansion of medical categories into social spheres, which were not previously “read” medically, may play a reassuring role. For example, if we think that boisterous children are sick and have neurological problems and chemical imbalances, we allow ourselves to avoid looking at social problems like unemployment, social cohesion in ghettos and integration of the immigrants. A pill which works on serotonin levels is easy to prescribe, and is cheaper and “cleaner” than any social policy. Another example of medical colonization can be seen in food. In supermarkets, shelves of health foods are constantly growing. Food is increasingly advertised, packed and branded in ways which connect it to medical contexts. We have probiotic yoghurt which reduces the risk of ictus, blueberry drinks which improve our vision, and mineral waters which “purify”.
To sum up, the bionic society can be described by at least three intertwining forces:
A strong emphasis on health as considered by its chemical, neurological and genetic dimensions;
The extension of medical ways of thinking (not only medical treatments) in areas which were not medicalized previously – or were only partially medicalized – like prevention, cosmetic, nutrition;
A growing pharmaceuticalization which questions the borders between normality, pathology and enhancement, and therefore also between nature and nurture (Maturo, 2010b[23]).
In the near future, it seems that a bionic healthscape could lead to the transformation of social problems into medical problems of the single individual, therefore de-responsabilizing political and social institutions. On the other side, the emphasis on genetics and neurological dimensions might foster fatalism and passivity, leading to the deresponsabilization of the individuals for their health choices. All of this happening in a context where the lines between natural and artificial, normal and pathological, treatment and enhancement, are increasingly blurred.
Take home message
The transformation of human conditions into medical problems is increasing. In the past, medical profession was considered the main driver of this trend. Today other factors should also be taken into consideration: consumerism, managed care, marketing for pharmaceuticals and biotechnology.
The risk of medicalization is to neglect the role of social determinants in shaping human health. A new phenomenon which is emerging is human enhancement, that is, use of biomedical devices to optimise normality (and not to cure illness).[34]
Questions that this Paper Raises
What role will the welfare State play in a bionic society?
Are diagnosis discovered or constructed?
How are the borders between normality and pathology changing?
Why is mental health so medicalized?
How is prevention changing in a bionic society?
What are the connections between human enhancement and social justice?
About the Author

Antonio Maturo is Associate Professor of Medical Sociology at Bologna University and Visiting Professor at Brown University. He is also member of the Executive Committee of the European Society for Health and Medical Sociology and Scientific Secretary of the Italian journal Salute e Società (Health and Society).
Footnotes
Conflict of interest: None declared
Declaration
This is my original, unpublished work, not submitted for publication elsewhere.
CITATION: Maturo A. Medicalization: Current Concept and Future Directions in a Bionic Society. Mens Sana Monogr 2012; 10: 122-133.
References
- 1.Abraham J. The Sociological Concomitants of the Pharmaceutical Industry and Medications. In: Bird C., Conrad P., Fremont A., Timmermans S., editors. Handbook of Medical Sociology. Nashville: Vanderbilt U.P; 2010. pp. 290–308. [Google Scholar]
- 2.Angell M. The truth about the drug companies. London: Random House; 1988. [Google Scholar]
- 3.Barker K. Medicalization, multiplication of diseases, and human enhancement. Salute e Società. 2009;8:99–122. [Google Scholar]
- 4.Barker K. Electronic support group, patient-consumers, and medicalization: The case of contested illness. J Health Soc Behav. 2008;49:20–36. doi: 10.1177/002214650804900103. PMID: 18418983. [DOI] [PubMed] [Google Scholar]
- 5.Cipolla C. Why we cannot consider ourselves Darwinists anymore (Why Dunant won over Darwin) Salute e Società. 2010;9:138–42. [Google Scholar]
- 6.Clarke A, Shim J. Medicalization and Biomedicalization Revisited: Technoscience and Transformations of Health, Illness, and Biomedicine. In: Pescosolido B. A., et al., editors. Handbook of the Sociology of Health, Illness, and Healing. New York: Springer; 2011. pp. 173–200. [Google Scholar]
- 7.Conrad P. The Shifting Engines of Medicalization. Salute e Società. 2009;8:31–48. [Google Scholar]
- 8.Conrad P. The Medicalization of Society: On the Transformation of Human Conditions into Treatable Disorders. Baltimore, MD: Johns Hopkins University Press; 2007. [Google Scholar]
- 9.Douglas M. Risk and Blame. London: Routledge; 1992. [Google Scholar]
- 10.Foucault M. Crisis de un modelo en la medicina?. Revista centroamericana de Ciencias de la Salud. 1976;3:202–19. [Google Scholar]
- 11.Freidson E. Profession of Medicine. New York: Dodd, Mead; 1970. [Google Scholar]
- 12.Fulford KW. Neuroscience and values: A case study illustrating developments in policy, training and research in the UK and internationally. Mens Sana Monographs. 2010;9:79–92. doi: 10.4103/0973-1229.77428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Horwitz A. Pharmaceuticals and the Medicalization of Social Life. In: Light D., editor. The Risks of Prescription Drugs. New York: Columbia U.P.; 2010. pp. 92–115. [Google Scholar]
- 14.Horwitz A. Creating Mental Illness. Chicago: University of Chicago U.P.; 2002. [Google Scholar]
- 15.Horwitz A, Wakefield J. The Medicalization of Sadness. Salute e Società. 2009;8:49–66. [Google Scholar]
- 16.Horwitz A, Wakefield J. The Loss of Sadness. How Psychiatry Transformed Normal Sorrow Into Depressive Disorder. New York: Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- 17.Illich I. Limits to Medicine – Medical Nemesis: The Expropriation of Health. London: Marion Boyars Publisher Ltd; 1973. [Google Scholar]
- 18.Jutel A. Sociology of diagnosis: A preliminary review. Soc Health Illness. 2009;31:278–99. doi: 10.1111/j.1467-9566.2008.01152.x. [DOI] [PubMed] [Google Scholar]
- 19.Light D. Bearing the Risks of Prescription Drugs. In: Light D., editor. The Risks of Prescription Drugs. New York: Columbia U.P.; 2010. pp. 40–69. [Google Scholar]
- 20.Link B, Phelan J. Social Conditions as Fundamental Causes of Health Inequalities. In: Bird C., Conrad P., Fremont A., Timmermans S., editors. Handbook of Medical Sociology. Nashville: Vanderbilt U.P; 2010. pp. 3–17. [Google Scholar]
- 21.Luhmann N. Risk: A Sociological Theory. Berlin: De Gruyter; 1993. [Google Scholar]
- 22.Maturo A. Bipolar Disorder and the Medicalization of Mood: An Epidemics of Diagnosis? In: Mukherjea A., editor. Understanding Emerging Epidemics: Social and Political Approaches. London: Emerald; 2010a. pp. 225–42. [Google Scholar]
- 23.Maturo A. Towards a bionic society? Salute e Società. 2010b;9:215–20. [Google Scholar]
- 24.Maturo A. Shifting borders of medicalization: Perspectives and dilemmas of human enhancement. Salute e Società. 2009a;8:13–31. [Google Scholar]
- 25.Maturo A. Médicalisation, marketing pharmaceutique et inégalité sociales. Revue Sociologie Santé. 2009b;30:177–86. [Google Scholar]
- 26.Moynihan R, Cassels A. Selling sickness. How drug companies are turning us into patients. New York: Nation Books; 2005. [Google Scholar]
- 27.Murray J. Direct-to-consumer prescription drug advertising in a global context: A comparison between New Zealand and the US. Salute e Società. 2009a;8:189–201. [Google Scholar]
- 28.Rose N. The Politics of Life. Princeton: Princeton University Press; 2006. [Google Scholar]
- 29.Scott J, Dikey B. Global burden of depression: The intersection of culture and medicine. Br J Psychiatry. 2003;183:92–4. doi: 10.1192/bjp.183.2.92. PMID: 12893658. [DOI] [PubMed] [Google Scholar]
- 30.Shostak S, Frese J. Gene-Environment Interaction and Medical Sociology. In: Bird C., Conrad P., Fremont A., Timmermans S., editors. Handbook of Medical Sociology. Nashville: Vanderbilt U.P; 2010. pp. 418–34. [Google Scholar]
- 31.Smith DJ, Ghaemi SN, Craddock N. The broad clinical spectrum of bipolar disorder: Implications for research and practice. J Psychopharmacol. 2008;22:397–400. doi: 10.1177/0269881108089585. [DOI] [PubMed] [Google Scholar]
- 32.Turner B. The New Medical Sociology. London: Norton & Company; 2004. [Google Scholar]
- 33.World Health Organization. New York: Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference; 1946. Jun 19-22, [Google Scholar]
- 34.Zola I.K. Socio-Medical Inquires. Philadelphia: Temple U.P.; 1982. [Google Scholar]