Abstract
Attention deficit hyperactivity disorder is a developmental disorder with an age onset prior to 7 years. Children with ADHD have significantly lower ability to focus and sustain attention and also score higher on impulsivity and hyperactivity. Stimulants, such as methylphenidate, have remained the mainstay of ADHD treatment for decades with evidence supporting their use. However, recent years have seen emergence of newer drugs and drug delivery systems, like osmotic release oral systems and transdermal patches, to mention a few. The use of nonstimulant drugs like atomoxetine and various other drugs, such as α-agonists, and a few antidepressants, being used in an off-label manner, have added to the pharmacotherapy of ADHD. This review discusses current trends in drug therapy of ADHD and highlights the promise pharmacogenomics may hold in the future.
Keywords: ADHD, α-agonists, Antidepressants, Atomoxetine, Attention deficit hyperactivity disorder, Bupropion, Children, Clonidine, Dopamine, Drug, delivery systems, Guanfacine, Lisdexamphetamine (LDX), Methylphenidate, Mixed Amphetamine Salts, Modafinil, Non-stimulants, Pemoline, Pharmacogenomics, Preschool ADHD, Reboxetine, Selegiline, Stimulants, Theophylline, Venlafaxine
Introduction
Attention deficit hyperactivity disorder (ADHD) is a common psychiatric problem in children. It presents as inattentiveness, over-activity, impulsivity, or a combination of these and affects 3-10% of school-going children worldwide (Biederman and Faraone, 2004[13]; Shastri et al., 2010[105]). The disorder is unique in showing marked variability over time, in different situations (for example at school, home and at the clinician's consultation), and within the same child and in similar situations. With an increase in the prevalence of ADHD, there has also been an increase in research based on pharmacotherapy of ADHD.
Pharmacotherapy remains the cornerstone for the management of ADHD, and there have been some recent advances in this area (Prince, 2006[93]; Boyle et al., 2011[18]; Sitholey et al., 2011[106]). First, there has been the development and availability of novel drug delivery systems for methylphenidate (MPH) and mixed amphetamine salts (MAS) that has made it possible to extend full day coverage with a single dose. Second, the emergence of atomoxetine (ATX), a noradrenergic medication, has allowed us access to alternate neurotransmitter systems in children where stimulants fail. These two, coupled with development in the pharmacogenomics of ADHD, are set to usher in various newer trends in its drug management.
This review article discusses various drugs used in ADHD management starting with older drugs like stimulants, moving on to ATX, and finally looking at off-label drugs. It deals mainly with current trends in ADHD Management. To our knowledge, we could not find any relevant Indian literature in this area, which underscores the need for future work in this field in the country.
Stimulants
Stimulants, such as MPH and MAS, are the most widely used medications approved by the US-FDA for the treatment of ADHD in children (Findling, 2008[38]). These medications have a paradoxical effect on individuals with ADHD, calming them and improving both the cognitive (inattention and impulsivity) and the non-cognitive (hyperactivity) domains of the disorder (Swanson et al., 2011[121]). All stimulants work by increasing the levels of dopamine in the brain, dopamine being associated with attention, pleasure and movement. When started at lower doses followed by gradual up-titration, stimulants are able to increase dopamine slowly and steadily, producing an effect similar to the natural production of dopamine in the brain. However, when taken in higher doses, or if the dose is increased in a shorter time, stimulants can increase brain dopamine rapidly, producing euphoria and an increased risk of abuse and dependence. Even though stimulants remain the US-FDA-approved medical treatment of choice for ADHD and are associated with an exceptional response rate (Wigal, 2009[131]), around 10-30% of all children and adults with ADHD either do not respond to, or do not tolerate treatment with stimulants (Banaschewski et al., 2004[5]).
Methylphenidate
MPH is a psychostimulant drug approved for ADHD. It increases norepinephrine and dopamine levels by inhibiting their reuptake and facilitating their release especially in the dorsolateral prefrontal cortex that improves attention, concentration, executive function and maintains wakefulness. Enhancement of dopamine actions in basal ganglia may explain the improvement seen in hyperactivity symptom of ADHD with MPH. This amplifying effect of MPH on release of dopamine improves attention and focus in individuals who have weak dopamine signals (Volkow et al., 2002[125]). MPH improves overall productivity and accuracy on arithmetic assignments, reduces disruptive behavior, and improves classroom rule-following and negative behavior in the child (Pelham et al., 2001[83]).
Expert consensus recommends MPH as the first line medication to be used in a treatment algorithm for ADHD in children and adolescents (Greenhill et al., 2002a[44]; Wolraich et al., 2010[139]). In case of no response or partial response, optimising the doses, or switching to other agents is the recommended step. It is also worth addressing and assessing non-compliance issues and any co-morbid conditions. There are various preparations of MPH available and various delivery forms to facilitate dosages in a once-a-day format.
Case Vignette: A 7-year-old female child was referred for poor concentration and reduced ‘interest’ in classes while the teacher was teaching. She would make careless mistakes while writing dictation, often coming home with incomplete notes. She would lose her things in school daily and would have difficulty sitting in one place for a long time with a lot of fidgetiness. She was also known to be hyperactive. The teachers would complain about her distractibility to the smallest of stimuli during teaching hours in class. Her IQ on Wechsler Intelligence Scale for Children was 115 and there were no other significant problems in her psychosocial history. Her father had a history of similar problems.
Discussion: This child with ADHD is a suitable candidate for MPH. Clinical experience shows that ADHD primarily of inattentive type responds better to MPH.
MPH – immediate release (MPH-IR)
Immediate release MPH (MPH-IR) has a short half-life of approximately 2 to 3 hours (Swanson et al., 1978[118]; Greenhill, 1992[43]; Atzori et al., 2009[4]). This requires multiple daily doses that pose problems for dosing during school timings and can thus compromise patient compliance. It also compromises confidentiality issues as the patient is required to take the medication during school hours (among other classmates), who may not be able to understand the patient's condition, further stigmatising his/her experience with the illness. The dose range for MPH-IR is 0.3-1mg/kg TID up to a maximum of 60 mg per day (Atzori et al., 2009[4]).
MPH – extended release (MPH-ER)
MPH extended release formulation provides the benefit of a lasting effect that is maintained even about 12 hours after dosing and is equivalent to twice- or thrice-daily dosing of plain MPH. Studies support the use of MPH-ER formulation that provides benefits throughout the day and early part of the evening (Pelham et al., 2001[83]; Mikami et al., 2009[73]). Some newer ER formulations produce therapeutic effects by the MPH dose being delivered initially by a bolus that achieves peak plasma concentrations in early morning within 2 hours of dosing, and a second extended and controlled delivery of the drug that achieves the required plasma concentrations in the afternoon (Swanson et al., 2002[119], 2003[120]; Mikami et al., 2009[73]). Thus, with the ER formulations, one achieves effective symptom control throughout the day. The dose range for MPH-ER is the same as for immediate release formulation, except that it has to be dosed once in the morning. [The IR- and ER- preparations are the more commonly and easily available formulations in different parts of the world, including India; however those mentioned hereafter are not yet universally available].
Newer Drug Delivery systems for MPH
MPH – osmotic release oral system (MPH-OROS)
This is a preparation of MPH with a novel drug delivery system using the osmotic pump process as a release mechanism. It was launched in the US in August 2000 and is not yet available in India. It consists of a 50:50 racemic mixture of D, l-threo MPH. It has a 12-hour coverage period per dose and, the release system being gradual, prevents any form of tachyphylaxis. It is available as an 18mg caplet, where 4mg is released as a bolus and additional delivery is in the form of an ascending profile similar to MPH-IR being given at a dose of 5mg thrice a day (Swanson et al., 2003[120]).
There have been some important randomised controlled trials using OROS-MPH with interesting findings. Though different dosages have been tried, it has been noted that the effect sizes with both MPH-IR and OROS-MPH have been the same (Wolraich et al., 2001[138]). Side effects have been mild in the form of headache, drowsiness and irritability (Pelham et al., 2001[83]). It has been noted that lower doses of OROS-MPH are needed in children with ADHD inattentive type compared to children with a combined type of ADHD (Stein et al., 2003[115]). There have been long-term studies for periods in the range of 8-24 months with OROS-MPH indicating good efficacy and tolerability (Wilens et al., 2003a[133]; Steele et al., 2004[114]).
MPH – modified release (MPH – MR)
This is a form of MPH that uses a release system made up of two types of coated beads consisting of MPH-IR and MPH-ER in a 30:70 ratio. It is available in 20mg capsules with 6mg of MPH-IR and 14mg of MPH-ER. The 1st peak in dosage is in 1.5 hours with MPH-IR and the second peak in dosage is in 4.5 hours with MPH-ER. The beads can be sprinkled on food or mixed in a drink. The capsule has been designed to simulate a twice a day MPH-IR dosage. Further studies are warranted to gauge the efficacy and usage of this preparation (Greenhill et al., 2002b[45]; Faraone and Buitelaar, 2010[36]).
Methylphenidate-extended release capsules (ERC)
This is a preparation of MPH that uses the spheroidal oral drug absorption system (SODAS). It is available as 10, 20, 30 and 40 mg capsules. It has bimodal release profile with 50% of the drug i.e. d,l-threo MPH releasing initially and the other 50% releasing after 3-5 hours. It thus provides 8-hour coverage. The side effect profile is mild too. A study has shown an effect size of 0.9 with this treatment and no major adverse effects (Biederman et al., 2003a[11]).
D-threo-methylphenidate, D – methylphenidate (D-MPH)
As originally formulated, MPH was produced as an equal mixture of D,l-threo-MPH and D,l-erythro-MPH. It was later recognised that the erythro form of MPH was responsible for the cardiovascular side effects of MPH, and thus MPH has been manufactured as an equal mixture of D and L-threo MPH. Studies have revealed that the D form is the primary active form of MPH (Ding et al., 1997[31], 2004[32]). Thus the D form is now available as tablets of 2.5, 5 and 10 mg. It is worth mentioning that 5 mg D-MPH is equivalent to 10 mg MPH-IR. The drug has been studied and is well tolerated in open trials and controlled studies with minimal side effects (Silva et al., 2004[107]; Wigal et al., 2004[129]). Using the SODAS beaded technique there is an extended release preparation of D-MPH available in 5, 10 and 20 mg capsules (Greenhill et al., 2006[47]).
MPH transdermal patch
MPH has been investigated for use as a transdermal patch in sizes of 6.25cm2(0.45mg/hour), 12.5cm2(0.9mg/hour) and 25cm2(1.8mg/hour). The only side effects noted in the study conducted were erythema at the site of the patch, mild insomnia in a few subjects, and decreased appetite (Pelham et al., 2005[84]). Such innovative yet investigational methods of drug delivery may pave the way for easy drug administration in a regular manner throughout the day in children with ADHD.
Amphetamine and Related Drugs
Mixed amphetamine salts
In recent years, both immediate and extended release preparations of MAS have been studied in clinical trials. MAS tablets contain equal proportions of D-amphetamine saccharate, D,l-amphetamine asparate, D-amphetamine sulfate and D,l-amphetamine sulfate. The two isomers have different properties and some children may respond better to one isomer than the other. The peak behavioral effects of MAS occur later than MPH-IR and are more sustained. It has also been noted in studies that a twice-daily dosage is superior to a once-daily dosage (Plizska et al., 2000[87]; Greenhill et al., 2003[46]; Hechtman, 2011[53]).
MAS – extended release (MAS-ER)
The MAS-ER preparation contains a 50:50 ratio of immediate release beads designed to release MAS in a fashion similar to MAS tablets and delayed release beads designed to release MAS 4 to 6 hours after the dosing. Clinical trials in both large and small groups of prepubertal children have shown that response and effect size is good with stimulant naïve subjects, who respond equally well as compared to children who have been treated previously with stimulants. Long-term studies over 24 months have reported that MAS-ER has been well tolerated and resulted in significant and sustained clinical benefits (Biederman et al., 2002[10]; McGough et al., 2005[69]).
Pemoline
Pemoline is a central nervous system stimulant structurally different from amphetamine and MPH, and acts via enhancing central dopaminergic transmission. Since its availability in 1975, 15 cases of acute fulminant hepatic failure with pemoline have been reported. US-FDA recommends liver function tests every 2 weeks while on the drug. Hence the use of pemoline has been relegated to only rare circumstances (Sallee et al., 1992[100]; Patrick and Markowitz, 1997[82]; Safer et al., 2001[99]).
Lisdexamphetamine (LDX)
A recently approved prodrug stimulant, LDX converts to dextroamphetamine in the blood stream due to the action of a peptidase enzyme and provides a longer duration of effect that is consistent throughout the day (Findling, 2008[38]). As a prodrug it does not become active until after it is metabolized. This lowers its ability to be diverted and abused in an intranasal or intravenous manner. It is available in capsule form that can be dissolved in water when the patient may not be able to swallow. Its longer duration of action provides 12-hour coverage with a single dose (Biederman et al., 2007a[14]). Patients on LDX may complain of typical amphetamine side effects such as decreased appetite, nausea, weight loss, upper abdominal pain, insomnia, headache and irritability (Najib, 2009[77]). Studies suggest that LDX may form an integral part of a total treatment programme for ADHD in the future. Clinical evidence supports its efficacy and tolerability in the management of ADHD (Najib, 2009[77]). At equivalent doses, LDX had lower abuse potential compared with immediate release d-amphetamine (Findling, 2008[38]; Najib, 2009[77]). The recommended starting dosage is 30 mg orally daily that can be adjusted to a maximum dosage of 70 mg/day (Popovic et al., 2009[89]).
Side effects with stimulant drugs
Knowing the side effect profile of these drugs is important since side effects could be a major reason for non-adherence to treatment (Sitholey et al., 2011[106]). The various MPH formulations (IR and ER) are reported to have similar effect and side effect profile (Pelham et al., 2001[83]; Stiefel and Besag, 2010[117]). Various side effects of MPH include insomnia, headache, nervousness, irritability and dizziness. MPH may have gastrointestinal side effects like anorexia, nausea and abdominal pain. It is also reported to reduce seizure threshold in some patients, thus precipitating seizures. Although new onset seizures and drug-drug interactions between MPH and antiepileptic drugs (AEDs) have been reported, open-label trials suggest otherwise, with no effect of MPH on either seizure or AED serum levels (Baptista-Neto et al., 2008[8]). A worsening of tics with stimulants may be seen in some but not all patients, although this is a major limiting factor in their use in such patients (Pringsheim and Steeves, 2011[94]).
Treatment of ADHD comorbid with tic disorders cannot be ignored given the impact that ADHD has on these patients, and MPH appears to be the best-tolerated stimulant compound in such patients (Kurlan, 2003[63]). Although use of stimulants has been avoided in patients with autism spectrum disorders (ASD) due to the concern that they worsen stereotypies, studies suggest otherwise (Santosh et al., 2006[103]): autistic patients with ADHD show significant improvements in the symptom clusters of ADHD along with aggression and oppositionality seen in autism (Santosh et al., 2006[103]). MPH is also known to cause pupil dilation leading to blurring of vision (Jaanus, 1992[55]). Complex visual hallucinations have been reported with MPH (Halevy and Shuper, 2009[50]). There is some amount of risk of abuse with MPH-IR formulations (Findling, 2008[38]). Concerns on an increase in the risk of drug and alcohol abuse disorders later in life in ADHD children treated with stimulants have not been supported by research (Wilens et al., 2003b[134]; Biederman et al., 2008a[16]; Mannuzza et al., 2008[66]).
An emerging area of concern has been the effect of stimulant drugs on cardiovascular function. It is well known that these medications have an effect on heart rate (HR), systolic and diastolic blood pressure (SBP and DBP). On an average, patients on stimulant drugs reported that while on the medication in optimal doses, there is an increase in HR by 1-2 beats per minute, and SBP and DBP by 3-4 mmHg (Findling et al., 2001[37]). This increase is linear with increase in dosage. Although statistically significant there has been no clinical event as a result of these changes in cardiovascular parameters. It is, however, advised that an electrocardiogram (ECG) be done in every child before starting on stimulants, and this may be supplemented by a 2D echocardiography (2D ECHO) when needed (Findling et al., 2001[37]). Recent studies have reported statistically significant yet clinically minor changes in HR, SBP and DBP even with OROS-MPH and MAS-ER preparations (McBurnett and Starr, 2011[70]). There have been reports of sudden cardiac deaths with MPH and MAS, but in all cases, post mortem examination revealed a structural heart defect that was not investigated prior to starting medication (Wilens et al., 2004[135]).
Sleep disturbances are common in children with ADHD. The increased prevalence of sleep disturbances in ADHD has not been correlated to stimulant drugs that have been shown to have little detrimental effect on sleep characteristics (Cohen-Zion and Ancoli-Israel, 2004[23]). Melatonin and small doses of Clonidine have been advocated for the treatment of sleep problems in ADHD (Prince et al., 1996[92]; Tjon Pian Gi et al., 2003[122]). Patients treated with stimulants experience dose-related reduction in appetite and in some cases, weight loss (Rapport and Moffit, 2002[96]). Cyproheptadine, an antihistaminergic and antiserotonergic medication, has been suggested as useful for stimulant induced appetite suppression. Nutritional options with higher caloric diet may be another option (Daviss and Scott, 2004[29]). Coupled with appetite suppression, concern surrounds the impact of stimulant therapy on the rate and extent of growth in children (Biederman et al., 2003b[12]). The current consensus is that stimulants may infrequently produce a small negative impact on growth velocity; however, this delay may be related more to ADHD than to its treatment. The role of drug holidays or temporary periods of medication discontinuation to minimise the growth effect has not been supported by research data, though clinically this method may be more practical (MTA Cooperative Group, 2004[78]). It is worth noting that MPH has not been approved for use in children below six years of age (Vitiello, 2001[124]; Hermens et al., 2006[54]). Predictors of poor clinical response to MPH include ADHD combined type, comorbid oppositional defiant disorder and maternal ADHD symptoms (Chazan et al., 2011[21]).
Non Stimulants
Atomoxetine
ATX is the first non-stimulant treatment approved by the US FDA and is an effective alternative to stimulants, especially for patients who have comorbidities that contraindicate their use. It is also the first ADHD treatment to be approved for use in adults with ADHD (Simpson and Plosker, 2004[108]; Hammerness et al., 2009a[51]). ATX has a negligible risk of abuse and is therefore considered particularly useful for patients who may be at such risk. Patients with comorbid anxiety or tics, and oppositional symptoms, or those who do not wish to take a controlled substance may be given a trial of ATX. Dosing with ATX involves weight-based dosing up to 1.4 mg/kg/day; benefit is generally observed within 2-8 weeks of initiation of treatment (May and Kratochvil, 2010[68]). In the case of ADHD, practice parameters from the American Academy of Child and Adolescent Psychiatry provide clear guidelines and describe the three common approaches taken by clinicians in dose titration with ATX: prescribing and waiting for the effects to occur, gradual up-titration of the dose until behavioral improvement is seen, and increasing the dose until side effects occur with gradual reduction of the dose to the level before the side effects appeared (Greenhill et al., 2002b[45]; Manos et al., 2007[65]; Daughton and Kratochvil 2009[27]). It has been suggested that treatment algorithms involving the initial use of atomoxetine appear more cost-effective as compared to algorithms involving initial use of MPH or other medications (Garnock-Jones and Keating, 2009[40]).
Pivotal studies documenting the efficacy of ATX in ADHD started in 2001 (Spencer et al., 2001[110]). Results from large randomised controlled trials have shown that teachers and parents report similar improvements in their children when ATX is used over long periods (Weiss et al., 2005[127]). A recent meta-analysis has reported good efficacy and safety of ATX in children with ADHD (Cheng et al., 2007[20]). However, when studies on ADHD are reviewed, it is worth noting that superior effect sizes compared to ATX have always been consistently noted with MPH-IR and MPH-ER (Faraone et al., 2006[35]). In short term studies of 4-8 weeks, a greater improvement has been noted with MPH and MAS compared to ATX (Wigal et al., 2005[130]), while in long term studies over a period 10-14 weeks or more, ATX is as efficacious as MPH (Kratochvil et al., 2006[60]).
Theoretically, twice-a-day dosage of ATX appears better than a single dosage, but most studies document improvement with a once daily dosage alone (Michelson et al., 2002[72]; Kelsey et al., 2004[58]). Newcorn et al., 2008[80], demonstrated that ATX elicits a lower response from children who have received stimulants prior to starting ATX compared to children who are stimulant naïve. The mechanism for this is not yet understood but this has not been the case in other studies where ATX has shown an equivalent response in both the above groups (Quintana et al., 2007[95]; Hammerness et al., 2009b[52]). ATX has also been reported to be effective when combined with stimulants, though side effects like insomnia and reduced appetite increase with this combination (Carlson et al., 2007[19]). In case it is needed, shifting a patient from MPH to ATX requires gradual cross-titration and poses no major problem (Quintana et al., 2007[95]). ATX has also shown good efficacy in long-term studies over 2 years and 5 years with all effects sustained and well maintained (Kratochvil et al., 2006[60]; Spencer et al., 2007[111]). In other studies, when ATX has been used in children with ADHD and oppositional defiant disorder, it has been noted that larger doses of ATX were needed to reduce hyperactivity symptoms, but there was little change noted in oppositional behavior (Biederman et al., 2007b[15]; Bangs et al., 2008[7]). ATX has also been demonstrated, in small studies, to have a positive effect on anxiety and depressive symptoms that may accompany ADHD, unlike MPH (Geller et al., 2007[41]; Bangs et al., 2007[6]).
Side effects with atomoxetine
The side effect profile of ATX is milder than that of stimulants. Common side effects include decreased appetite and weight, irritability, sedation or insomnia, dizziness, abdominal pain and fatigue. While patients may complain of an initial loss in expected height and weight, this may eventually return to normal in the long term (Garnock-Jones and Keating, 2009[40]); hence reassuring concerned parents about this is important. Although considered safer, there have been rare case reports of exacerbation (Parraga et al., 2007[81]) or development (Sears and Patel, 2008[104]; Ledbetter, 2005[64]) of tics with ATX. It is important to keep a watch for suicidal ideations in patients on atomoxetine (Polzer et al., 2007[88]) though such episodes may be rare. At routinely prescribed doses and as seen in various trials there is no significant effect of ATX on the cardiovascular system in children as well as no reports of sudden cardiac death (Perrin et al., 2008[86]). There are rare reports of seizures with ATX and the percentage has been 0.1-0.2% (Wernicke et al., 2007[128]). No deaths have been reported when poison centre reports were analysed for ATX overdoses, and doses up to 2840 mg have been reported to cause seizures and GI problems (Kashani and Ruha, 2007[56]; Spiller et al., 2005[113]). In a double-blind study in 6- to 16-year-old outpatients with ADHD from three different countries, Wang et al., 2007[126], reported a higher incidence of adverse effects with ATX compared to MPH.
Case Vignette: Parents brought a 9-year-old boy with a history of deteriorating grades in school and poor peer relations. The parents were receiving frequent complaints from school regarding his inattention and increasingly mischievous behavior during class, which led to punishments. This problematic behavior did not improve despite changing his sitting position. He was a known case of seizure disorder since past 3 years and was on regular medications with no seizures in the past 2 years. His father was a known case of alcohol dependence with multiple failed attempts at abstinence and was presently not on any treatment.
Discussion: The drug of choice in this child would preferably be ATX. Two risk factors in this child's history push the decision in favor of ATX: history of seizures in him, and of substance use in his family.
Non US FDA approved Medication used in ADHD
While stimulants are clearly the most effective agents, other drugs may also be useful. Additional therapy with non-stimulants (other than ATX) is warranted if the patient fails to respond to trials of two different stimulants, has intolerable side effects with stimulants, or fails to respond to ATX (Manos et al., 2007[65]).
Clonidine and guanfacine
Alpha-adrenergic agonists have been recommended in patients with a suboptimal response to psychostimulants, or in whom they cannot be tried (Sallee, 2010[102]). Both these drugs are available in India. Studies have shown that guanfacine extended release can be safely administered with MPH or amphetamine and gives good clinical results in ADHD (Spencer et al., 2009[112]). The rationale for combining α-adrenergic agonists with stimulants is the complementary mechanisms of action of the two classes of drugs involving different neurotransmitter systems that together modulate prefrontal cortex functioning (Sallee, 2010[102]). Various adverse effects include headache, fatigue, sedation and cardiovascular adverse events. One has to be vigilant and monitor changes in blood pressure and heart-rate during treatment with guanfacine; it is also better to avoid this drug in children with cardiovascular pathology (Connor and Rubin, 2010[25]).
Immediate release clonidine and guanfacine have limited use as they are rapidly absorbed and cleared from the body and have negative side effects. However, the newer controlled-release formulations of these two drugs have overcome these limitations and have proven effective in ADHD. A selective alpha (2A) adrenoceptor agonist, guanfacine extended-release is a once a day formulation that significantly improves the symptoms of inattention and hyperactivity-impulsivity in a dose range of 1-4 mg/day. Its efficacy has been demonstrated in both short-term and long-term studies (Biederman et al., 2008b[17]; Sallee et al., 2009[101]).
Bupropion
Bupropion has been used in certain cases of ADHD but has been associated with the onset or exacerbation of tics in these children (Ledbetter, 2005[64]). It is found to be useful in some cases of ADHD coupled with nicotine dependence because of its primary effect on smoking cessation (Upadhyaya et al., 2004[123]). It has also been useful to lift depressive symptoms that may accompany ADHD (Daviss et al., 2001[28]). Its efficacy is lesser than that of stimulants or ATX. Irritability and tics are commonly noted side effects. It is available as immediate release, extended release and sustained release preparations (Wilens et al., 2005[136]; Daviss et al., 2005[30]).
Modafinil
A novel stimulant distinct from amphetamine, modafinil has been US FDA approved for the treatment of narcolepsy and is easily available in Indian markets. It acts by activating specific hypothalamic regions. It has been shown to improve cognitive and meta-cognitive skills in non-sleep deprived adults (Baranski et al., 2004[9]). Published trials in ADHD show mixed results but definitely advocate the case for modafinil as a supplemental medication in the management of ADHD (Biederman et al., 2003b[12]).
Other drugs with anecdotal evidence
Certain studies have shown the benefits of selective norepinephrine reuptake inhibitor drug Reboxetine in the management of ADHD (Cohen-Yahin et al., 2009[22]; Arabgol et al., 2009[3]; Hechtman, 2011[53]). Similar reports exist for Venlafaxine, a drug from the same family (Ratner et al., 2005[97]). Selegiline, another drug, is an irreversible type B monoamine oxidase inhibitor that is metabolised into amphetamine and methampetamine. Certain trials show modest efficacy of this drug in children with ADHD, but potentially life threatening reactions with tyramine rich foods such as cheese, impede the use of selegiline in children who are unlikely to remember or adhere to the dietary restrictions (Akhondzadeh et al., 2003[1]; Mohammadi et al., 2004a[74]). Medications used to slow the decline in Alzheimer's disease have also generated interest in enhancing cognition in the treatment of ADHD.
The effect of cholinergic modulation on attention remains unclear. Studies of these drugs till date remain restricted to case series (Wilens et al., 2000[132]; Narahashi et al., 2004[79]). Based on the high rates of cigarette smoking in adolescents in ADHD and the cognitive enhancing properties of nicotine, transdermal nicotine has been tried in isolated studies to improve the fronto-striatal attention networks in ADHD. At this point though, nicotine is not a viable or recommended treatment, but remains a potential target for the development of novel treatments (Rezvani and Levin, 2001[98]; Potter and Newhouse, 2004[91]). Theophylline, an adenosine receptor antagonist, is a psychostimulant widely used as a bronchodilator. Adenosine antagonism may have an effect on central dopaminergic and noradrenergic neurotransmission and may benefit in conditions like ADHD. Pilot studies support the role of theophylline in paediatric ADHD (Guieu et al., 1996[49]; Mohammadi et al., 2004b[75]). Other agents such as polyunsaturated fatty acids (PUFA), acetyl-L-carnitine, and iron supplements have been shown to improve ADHD symptoms (Dopheide and Pliszka, 2009[33]).
The Treatment of Preschool ADHD
ADHD in pre-schoolers has become established as a valid psychiatric disorder, with prevalence estimates ranging from 2% to 6% in community samples (Keenan and Wakschlag, 2000[57]). Despite some differences in symptom presentation in younger children, similar patterns of comorbidity and impairment have been identified (DuPaul et al., 2001[34]). Many areas of impairment have been identified among pre-schoolers with ADHD, including relationships with parents, siblings, peers, and teachers, as well as their ability to cooperate with family activities and behave appropriately in public, which requires limitations of activities outside the home (Angold et al., 2000[2]; Murray, 2010[76]). Academically, preschoolers with ADHD perform more poorly on tests of pre-academic skills (Cunningham and Boyle, 2002[26]) and have identified deficits in working memory, planning, and delay of gratification (Sonuga-Barke et al., 2003[109]). Evidence indicates that ADHD may be more severe and complicated in younger children and those with earlier onset ADHD. Within a sample of clinically diagnosed children 3 to 5.5 years of age with ADHD, parents and teachers rated symptoms as more severe in younger children (Posner et al., 2007[90]). Earlier age at onset of ADHD (recalled by parents in annual increments from birth to 6 years of age) within a clinical sample of elementary school-age children was also associated with higher rates of parent-reported aggressive symptoms (Connor et al., 2003[24]). Diagnosis during the preschool years also predicts the development of other psychiatric disorders and creates significant risk for the development of secondary impairments such as school failure and peer difficulties during adolescence.
Prescription guidelines from the US FDA indicate that stimulant medications should not be used in children younger than 6 years of age. However, off-label use has increased dramatically since the 1990s, when 34% of paediatricians and 15% of family practitioners reported prescribing stimulants to pre-schoolers with ADHD (Wolraich et al., 1990[137]; Murray, 2010[76]; March, 2011[67]). Understandably, many concerns have been raised about these practices, including ethical objections to using any medication for children this young, concerns about side effects, and the limited body of efficacy data. Extensive data spanning several decades supports the safety and efficacy of stimulant medication in school-age children; however, few studies have included preschoolers. Prior to the National Institutes of Health– funded PATS, initiated in 2000 (Kollins et al., 2006[59]), there were only 11 publications of 10 controlled stimulant treatment studies, including less than 280 total participants, with many methodological limitations that affected interpretation of outcomes (Greenhill et al., 2008[48]). In particular, most of these studies were not placebo controlled, sample sizes were small, duration of the trials was short, and the diagnostic procedures and side effect reporting were highly variable. The results were mixed, with six reporting good efficacy and safety, two failing to show benefit, and two reporting higher rates of adverse events, including sadness and social withdrawal.
There are only a handful of studies with non-stimulants in preschool-age children with ADHD. One study treated 5 and 6-year-olds with ATX in open-label fashion for 8 weeks in combination with parent education in behavior management adapted from ‘Helping the Non Compliant Child’ (HNC) provided at each pharmacotherapy visit (Kratochvil et al., 2007[61]). A significant decrease in ADHD symptoms was observed at a dose of 1.25 mg/kg, which is similar to the dosing for school-age children. Similar to adverse events seen with stimulants, mood lability, decreased appetite and weight loss were common. Results of a recent 8-week, double-blind, placebo-controlled trial of ATX by the same authors in 101, 5 and 6 year olds recruited across two sites show similar findings (Kratochvil et al., 2011[62]). Although 3 and 4-year-olds were not included, and any effects of the psychoeducational component cannot be separated out, this study will greatly increase the existing knowledge base and inform clinicians considering non-stimulant treatment for preschoolers with ADHD (Pelham and Fabiano, 2008[85]).
Despite significant advances made recently in our knowledge of medication use for preschoolers with ADHD, many important questions relevant for clinical practice remain. In particular, stimulant dosing parameters and tolerability issues need further examination, as do the effects of sustained-release formulations in this group. There are literally no data on use of non-stimulants such as ATX in children younger than 5 years. Although there is evidence of benefit of stimulant medication for preschool-age children with ADHD, effects do not seem to be as large, and some of the side effects may be greater than for school-age children, including growth slowing. The long-term impact of medication use for preschoolers beyond 1 year is unclear, although follow-up studies should address this in the near future.
Clinical Aspects of Pharmacogenomics in ADHD
Preliminary evidence suggests that in ADHD, genetic variability plays some role in predicting treatment response (McGough, 2005[71]). The results may differ based on whether teachers or parents are informants. Correlations between various outcome measures, even in the same subjects, are known to be fairly weak, raising the question as to which outcome measure defines the best result. Pharmacogenetic effects are also known to vary amongst ethnic groups. Most published studies in the pharmacogenetics of ADHD examine response to MPH, which is an obvious choice considering the known pathophysiology of DAT1 and its association with ADHD serving as a specific target for stimulant action (Friedel et al., 2007[39]).
Certain prerequisites are essential when conducting pharmacogenetic studies in ADHD (Goldstein, 2003[42]). These are as follows –
Pharmacogenetic studies in ADHD should be methodologically rigorous in terms of the pharmacological intervention, which means that the trial should meet criteria for being published on its own.
There must be more randomised assignment to treatment or control groups. Response in the trial should always be measured in different ways and at different time points. Functional outcomes, adverse events and symptom ratings must also be evaluated.
Different doses of the drug or the optimal dose must be evaluated and dose ranging or forced titration designs are more likely to elicit pharmacogenetic effects than flexible dosing designs.
Multiple genes must be examined.
Genotyping quality control must be performed by laboratory checks.
Samples large enough to look at gene-environment interactions must be studied.
Trials sponsored by pharmaceutical companies should routinely collect DNA for pharmacogenetic and subgroup analysis.
ADHD pharmacogenetics may pave the way for development of novel treatments. Gene discovery may promote the discovery of new drug targets. Genotyping may lead to identifying patients who are more likely to show response to a particular drug and thus treatment failures can be minimised. The hope that arises out of this is that ADHD treatments will eventually improve through a more personalised and individualised approach, and personalised ADHD therapy shall soon move from the promise phase to a practical one (Stein and McGough, 2008[116]) [Figure 1].
Figure 1.
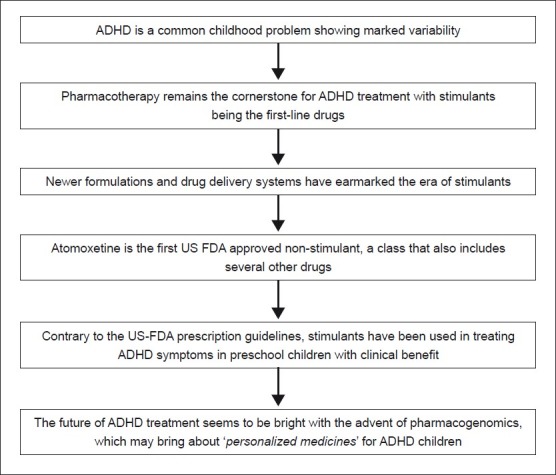
Flowchart of paper
Concluding Remarks [See also Figure 1: Flowchart of Paper]
Overall, pharmacotherapy of ADHD in children is proven to be effective. There is an abundance of evidence in this context, especially for MPH and ATX. In contrast to many other drugs used by relatively large proportions of children, drugs for treating ADHD are licensed and on-label for children. Although ADHD medication is being increasingly used for adolescents and adults, not much is published on specific efficacy and safety issues in these age categories. In general, we may conclude that though stimulant use has increased over the years, there is a lack of studies on long-term effects of ADHD drugs in all ages. Since ATX is new and has been used on a relatively small scale, not much is known yet about its adverse events. This may at times bias the ATX – MPH choice discussion in favor of the first. There are few studies that provide a head on comparison between various drugs used in ADHD. Multiple studies with small and large number of subjects using different scales and methods, along with varying durations, make meta-analyses in ADHD an onerous task. Although MPH has been used for decades, physicians also need to be aware that rare and possibly severe adverse events might come up. Also, the increased longevity of ADHD medication use may give rise to new concerns, which stresses the importance of monitoring people who use this medication for such a long period.
Take home message
There have been recent advances in the pharmacotherapy of ADHD with studies showing that MPH, MAS and ATX are useful in children with ADHD.
Stringent monitoring of treatment emerging side effects with these drugs is essential when a patient is taking them for a long time.
There are various novel drug delivery methods available for MPH that allows optimal dosage and once a day dosing.
Various anecdotal case reports, case series and small trials have shown the usefulness of medications like Bupropion, Reboxetine, Clonidine and Selegiline in ADHD. These agents may be used in non-responders to MPH or ATX.
Compared to the earlier contrary belief, it is noted from certain studies that ADHD treatment may need initiation right in the preschool years between ages 3 to 6.
In the near future, Pharmacogenomics, though at an investigational stage, holds promise to individualise and personalise ADHD treatment based on patient genotype.
Conflict of interest
None declared.
Declaration
This is our original unpublished work, not submitted for publication elsewhere.
Questions that this Paper Raises
Are we fully equipped with current pharmacotherapy for a complete management of ADHD?
What do we expect from newer drugs for ADHD – ease of dosage and better drug delivery systems, or newer mechanisms of action?
Is it wise to keep trying off label drugs in ADHD when US FDA approved medications fail?
Should ADHD be treated with medication in preschool children?
What is future of the treatment of ADHD with the advent of pharmacogenomics?
About the Author

Avinash De Sousa is a consultant psychiatrist and psychotherapist with a private practice in Mumbai. He is an avid reader and has over 90 publications in national and international journals. His main areas of interest are alcohol dependence, child and adolescent psychiatry, mental retardation, autism and developmental disabilities. He is also the academic director of the Institute of Psychotherapy Training and Management, Mumbai. He teaches psychiatry, child psychology and psychotherapy at over 18 institutions as a visiting faculty. He is also the founder trustee of Desousa Foundation – a charitable trust aimed at spreading mental health awareness, training and education across all sectors
About the Author

Gurvinder Singh Kalra is an Assistant Professor of Psychiatry at Lokmanya Tilak Medical College and Sion General Hospital in Mumbai. His main areas of interest are mood disorders, psychosexual disorders, alternate sexualities, and cinemeducation. He uses film and cinema modules to teach various aspects of psychiatry and sexuality to resident trainees and has published nationally and internationally on the same. Some of his important research works have been on geriatric sexuality and the ‘hijra’ community in India. He also volunteers his time working closely with various NGOs and groups that help individuals with alternate sexuality in the city of Mumbai
Footnotes
Conflict of interest: None declared
Declaration
This is our original unpublished work, not submitted for publication elsewhere.
CITATION: De Sousa A, Kalra G. Drug Therapy of Attention Deficit Hyperactivity Disorder: Current Trends. Mens Sana Monogr 2012; 10: 45-69.
References
- 1.Akhondzadeh S, Tavakolian R, Davari-Ashtiani R, Arabgol F, Amini H. Selegiline in the treatment of attention deficit hyperactivity disorder in children: A double blind and randomized trial. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27:841–5. doi: 10.1016/S0278-5846(03)00117-9. PMID: 12921918. [DOI] [PubMed] [Google Scholar]
- 2.Angold A, Erkanli A, Egger HL, Costello EJ. Stimulant treatment for children: A community perspective. J Am Acad Child Adolesc Psychiatry. 2000;39:975–84. doi: 10.1097/00004583-200008000-00009. PMID: 10939226. [DOI] [PubMed] [Google Scholar]
- 3.Arabgol F, Paanaghi L, Hebrani P. Reboxetine versus Methylphenidate in the treatment of children and adolescents with ADHD. Eur Child Adolesc Psychiatry. 2009;18:53–9. doi: 10.1007/s00787-008-0705-9. PMID: 18563471. [DOI] [PubMed] [Google Scholar]
- 4.Atzori P, Usala T, Carucci S, Danjou F, Zuddas A. Predictive factors for the persistent use and compliance of immediate release methylphenidate: A 36 month naturalistic study. J Child Adolesc Psychopharmacol. 2009;19:673–81. doi: 10.1089/cap.2008.0146. PMID: 20035585. [DOI] [PubMed] [Google Scholar]
- 5.Banaschewski T, Roessner V, Dittmann RW, Santosh PJ, Rothenberger A. Non-stimulant medications in the treatment of ADHD. Eur Child Adolesc Psychiatry. 2004;13(Suppl 1):102–16. doi: 10.1007/s00787-004-1010-x. PMID: 15322961. [DOI] [PubMed] [Google Scholar]
- 6.Bangs ME, Emslie GJ, Spencer TJ, Ramsey JL, Carlson C, Bartky EJ, et al. Efficacy and safety of atomoxetine in adolescents with attention deficit/hyperactivity disorder and major depression. J Child Adolesc Psychopharmacol. 2007;17:407–20. doi: 10.1089/cap.2007.0066. PMID: 17822337. [DOI] [PubMed] [Google Scholar]
- 7.Bangs ME, Hazell P, Danckaerts M, Hoare P, Coghill DR, Wehmeier PM, et al. Atomoxetine for the treatment of attention deficit/hyperactivity disorder and oppositional defiant disorder. Pediatrics. 2008;21(2):e314–20. doi: 10.1542/peds.2006-1880. PMID: 18245404. [DOI] [PubMed] [Google Scholar]
- 8.Baptista-Neto L, Dodds A, Rao S, Whitney J, Torres A, Gonzalez-Heydrich J. An expert opinion on methylphenidate treatment for attention deficit hyperactivity disorder in pediatric patients with epilepsy. Expert Opin Investig Drugs. 2008;17:77–84. doi: 10.1517/13543784.17.1.77. PMID: 18095920. [DOI] [PubMed] [Google Scholar]
- 9.Baranski JV, Pigeau R, Dinich P, Jacobs I. Effects of modafinil on cognitive and meta-cognitive performance. Hum Psychopharmacol. 2004;19:323–32. doi: 10.1002/hup.596. PMID: 15252824. [DOI] [PubMed] [Google Scholar]
- 10.Biederman J, Lopez FA, Boellner SW, Chandler MC. A randomized double-blind placebo-controlled, parallel-group study of SLI381 (Adderall XR) in children with attention-deficit/hyperactivity disorder. Pediatrics. 2002;110:258–66. doi: 10.1542/peds.110.2.258. PMID: 12165576. [DOI] [PubMed] [Google Scholar]
- 11.Biederman J, Quinn D, Weiss M, Markabi S, Weidenman M, Edson K, et al. Efficacy and safety of Ritalin LA, a new, once daily, extended-release dosage form of methylphenidate, in children with attention deficit hyperactivity disorder. Pediatr Drugs. 2003a;5:833–41. doi: 10.2165/00148581-200305120-00006. PMID: 14658924. [DOI] [PubMed] [Google Scholar]
- 12.Biederman J, Faraone SV, Monuteaux MC, Plunkett EA, Gifford J, Spencer T. Growth deficits and attention-deficit/hyperactivity disorder revisited: Impact of gender, development and treatment. Pediatrics. 2003;111(5 Pt 1):1010–6. doi: 10.1542/peds.111.5.1010. PMID: 12728081. [DOI] [PubMed] [Google Scholar]
- 13.Biederman J, Faraone SV. Attention deficit hyperactivity disorder: A worldwide concern ;192:453-4. J Nerv Ment Dis. 2004;192:453–4. doi: 10.1097/01.nmd.0000131803.68229.96. PMID: 15232314. [DOI] [PubMed] [Google Scholar]
- 14.Biederman J, Boellner SW, Childress A, Lopez FA, Krishnan S, Zhang Y. Lisdexamfetamine dimesylate and mixed amphetamine salts extended-release in children with ADHD: A double-blind, placebo-controlled, crossover analog classroom study ;62:970-6. Biol Psychiatry. 2007a;62:970–6. doi: 10.1016/j.biopsych.2007.04.015. PMID: 17631866. [DOI] [PubMed] [Google Scholar]
- 15.Biederman J, Spencer TJ, Newcorn JH, Gao H, Milton DR, Feldman PD, et al. Effect of comorbid symptoms of oppositional defiant disorder on responses to atomoxetine in children with ADHD: A meta-analysis of controlled clinical trial data. Psychophramacology (Berl) 2007b;190:31–41. doi: 10.1007/s00213-006-0565-2. PMID: 17093981. [DOI] [PubMed] [Google Scholar]
- 16.Biederman J, Monuteaux MC, Spencer T, Wilens TE, Macpherson HA, Faraone SV. Stimulant therapy and risk for subsequent substance use disorders in male adults with ADHD: A naturalistic controlled 10-year follow-up study. Am J Psychiatry. 2008a;165:597–603. doi: 10.1176/appi.ajp.2007.07091486. PMID: 18316421. [DOI] [PubMed] [Google Scholar]
- 17.Biederman J, Melmed RD, Patel A, McBurnett K, Donahue J, Lyne A. Long-term, open-label extension study of guanfacine extended release in children and adolescents with ADHD. CNS Spectr. 2008b;13:1047–55. doi: 10.1017/s1092852900017107. PMID: 19179940. [DOI] [PubMed] [Google Scholar]
- 18.Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Visser S, et al. Trends in the prevalence of developmental disabilities in the US 1997-2008. Pediatrics. 2011;127:1034–42. doi: 10.1542/peds.2010-2989. PMID: 21606152. [DOI] [PubMed] [Google Scholar]
- 19.Carlson GA, Dunn D, Kelsey D, Ruff D, Ball S, Ahrbecker L, et al. A pilot study for augmenting atomoxetine with methylphenidate: Safety of concomitant therapy in children with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatry Ment Health. 2007;1:10–8. doi: 10.1186/1753-2000-1-10. PMID: 17897473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng JY, Chen RY, Ko JS, Ng EM. Efficacy and safety of atomoxetine for attention-deficit/hyperactivity disorder in children and adolescents-meta-analysis and meta-regression analysis. Psychopharmacology (Berl) 2007;194:197–209. doi: 10.1007/s00213-007-0840-x. PMID: 17572882. [DOI] [PubMed] [Google Scholar]
- 21.Chazan R, Borowski C, Pianca T, Ludwig H, Rohde LA, Polanczyk G. Do phenotypic characteristics, parental psychopathology, family functioning, and environmental stressors have a role in the response to methylphenidate in children with attention-deficit/hyperactivity disorder.A naturalistic study from a developing country? J Clin Psychopharmacol. 2011;31:309–17. doi: 10.1097/JCP.0b013e318217b4df. PMID: 21508864. [DOI] [PubMed] [Google Scholar]
- 22.Cohen-Yahin I, Yoran-Hegesh R, Strous RD, Kotler M, Weizman A, Spivak B. Efficacy of Reboxetine in the treatment of attention deficit hyperactivity diosrders in boys with intolerance to methylphenidate: An open 8 week methylphenidate controlled trial. Clin Neuropharmacol. 2009;32(4):179–82. doi: 10.1097/WNF.0b013e318183796d. PMID: 19644227. [DOI] [PubMed] [Google Scholar]
- 23.Cohen-Zion M, Ancoli-Israel S. Sleep in children with attention-deficit hyperactivity disorder: A review of naturalistic and stimulant intervention studies. Sleep Med Rev. 2004;8:379–402. doi: 10.1016/j.smrv.2004.06.002. PMID: 15336238. [DOI] [PubMed] [Google Scholar]
- 24.Connor DF, Edwards G, Fletcher KE, Baird J, Barkley RA, Steingard RJ. Correlates of comorbid psychopathology in children with ADHD. J Am Acad Child Adolesc Psychiatry. 2003;42:193–200. doi: 10.1097/00004583-200302000-00013. PMID: 12544179. [DOI] [PubMed] [Google Scholar]
- 25.Connor DF, Rubin J. Guanfacine extended release in the treatment of attention deficit hyperactivity disorder in children and adolescents. Drugs Today (Barc) 2010;46:299–314. doi: 10.1358/dot.2010.46.5.1450095. PMID: 20517532. [DOI] [PubMed] [Google Scholar]
- 26.Cunningham CE, Boyle MH. Preschoolers at risk for attention-deficit hyperactivity disorder and oppositional defiant disorder: Family, parenting, and behavioral correlates. J Abnorm Child Psychol. 2002;30:555–69. doi: 10.1023/a:1020855429085. PMID: 12481971. [DOI] [PubMed] [Google Scholar]
- 27.Daughton JM, Kratochvil CJ. Review of ADHD pharmacotherapies: Advantages, disadvantages and clinical pearls. J Am Acad Child Adolesc Psychiatry. 2009;48:240–8. doi: 10.1097/CHI.0b013e318197748f. PMID: 19242289. [DOI] [PubMed] [Google Scholar]
- 28.Daviss WB, Bentivoglio P, Racusin R, Brown KM, Bostic JQ, Wiley L. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression.J Am Acad Child Adolesc Psychiatry. 2001;40:307–14. doi: 10.1097/00004583-200103000-00010. PMID: 11288772. [DOI] [PubMed] [Google Scholar]
- 29.Daviss WB, Scott J. A chart review of cyproheptadine for stimulant-induced weight loss. J Child Adolesc Psychopharmacol. 2004;14:65–73. doi: 10.1089/104454604773840508. PMID: 15142393. [DOI] [PubMed] [Google Scholar]
- 30.Daviss WB, Perel JM, Rudolph GR, Axelson DA, Gilchrist R, Nuss S, et al. Steady-state pharmacokinetics of bupropion SR in juvenile patients. J Am Acad Child Adolesc Psychiatry. 2005;44:349–57. doi: 10.1097/01.chi.0000153225.26850.26. PMID: 15782082. [DOI] [PubMed] [Google Scholar]
- 31.Ding YS, Fowler JS, Volkow ND, Dewey SL, Wang GJ, Logan J, et al. Chiral drugs: comparison of the pharmacokinetics of [11C] d-threo and L-threo-methylphenidate in the human and baboon brain. Psychopharmacology (Berl) 1997;131:71–8. doi: 10.1007/s002130050267. PMID: 9181638. [DOI] [PubMed] [Google Scholar]
- 32.Ding YS, Gatley SJ, Thanos PK, Shea C, Garza V, Xu Y, et al. Brain kinetics of methylphenidate (Ritalin) enantiomers after oral administration. Synapse. 2004;53:168–75. doi: 10.1002/syn.20046. PMID: 15236349. [DOI] [PubMed] [Google Scholar]
- 33.Dopheide JA, Pliszka SR. Attention-deficit-hyperactivity disorder: An update. Pharmacotherapy. 2009;29:656–79. doi: 10.1592/phco.29.6.656. PMID: 19476419. [DOI] [PubMed] [Google Scholar]
- 34.DuPaul GJ, McGoey KE, Eckert TL, VanBrakle J. Preschool children with attention-deficit/hyperactivity disorder: Impairments in behavioral, social, and school functioning. J Am Acad Child Adolesc Psychiatry. 2001;40:508–15. doi: 10.1097/00004583-200105000-00009. PMID: 11349694. [DOI] [PubMed] [Google Scholar]
- 35.Faraone SV, Biederman J, Spencer TJ, Aleardi M. Comparing the efficacy of medications for ADHD using meta-analysis. Med Gen Med. 2006;22:498–512. PMID: 17415287. [PMC free article] [PubMed] [Google Scholar]
- 36.Faraone SV, Buitelaar J. Comparing the efficacy of stimulants for attention deficit hyperactivity disorder in children and adolescents using meta analyses. Eur Child Adolesc Psychiatry. 2010;19:353–64. doi: 10.1007/s00787-009-0054-3. PMID: 19763664. [DOI] [PubMed] [Google Scholar]
- 37.Findling RL, Short EJ, Manos MJ. Short-term cardiovascular effects of methylphenidate and Adderall. J Am Acad Child Adolesc Psychiatry. 2001;40:525–9. doi: 10.1097/00004583-200105000-00011. PMID: 11349696. [DOI] [PubMed] [Google Scholar]
- 38.Findling RL. Evolution of the treatment of attention-deficit/hyperactivity disorder in children: A review. Clin Ther. 2008;30:942–57. doi: 10.1016/j.clinthera.2008.05.006. PMID: 18555941. [DOI] [PubMed] [Google Scholar]
- 39.Friedel S, Saar K, Sauer S, Dempfle A, Walitza S, Renner T, et al. Association and linkage of allelic variants of the dopamine transporter gene in ADHD. Mol Psychiatry. 2007;12:923–33. doi: 10.1038/sj.mp.4001986. PMID: 17579611. [DOI] [PubMed] [Google Scholar]
- 40.Garnock-Jones KP, Keating GM. Atomoxetine: a review of its use in attention-deficit hyperactivity disorder in children and adolescents. Paediatr Drugs. 2009;11:203–26. doi: 10.2165/00148581-200911030-00005. PMID: 19445548. [DOI] [PubMed] [Google Scholar]
- 41.Geller D, Donnelly C, Lopez F, Rubin R, Newcorn J, Sutton V, et al. Atomoxetine treatment for pediatric patients with ADHD and comorbid anxiety. J Am Acad Child Adolesc Psychiatry. 2007;46:1119–27. doi: 10.1097/chi.0b013e3180ca8385. PMID: 17712235. [DOI] [PubMed] [Google Scholar]
- 42.Goldstein DB. Pharmacogenetics in the laboratory and the clinic. N Engl J Med. 2003;348:553–6. doi: 10.1056/NEJMe020173. PMID: 12571264. [DOI] [PubMed] [Google Scholar]
- 43.Greenhill LL. Pharmacologic treatment of attention deficit hyperactivity disorder. Psychiatr Clin North Am. 1992;15:1–27. PMID: 1347936. [PubMed] [Google Scholar]
- 44.Greenhill LL, Pliszka S, Dulcan MK, Bernet W, Arnold V, Beitchman J, et al. Practice parameters for the use of stimulant medications in the treatment of children, adolescents and adults. J Am Acad Child Adolesc Psychiatry. 2002a;41(2 Suppl) doi: 10.1097/00004583-200202001-00003. PMID: 11833633. [DOI] [PubMed] [Google Scholar]
- 45.Greenhill LL, Beyer DH, Finkleson J, Shaffer D, Biederman J, Conners CK, et al. Guidelines and algorithms for the use of methylphenidate in children with Attention-Deficit/Hyperactivity Disorder. J Atten Disord. 2002b;6(Suppl 1):S89–100. doi: 10.1177/070674370200601s11. PMID: 12685523. [DOI] [PubMed] [Google Scholar]
- 46.Greenhill LL, Swanson JM, Steinhoff K, Fried J, Posner K, Lerner M, et al. A pharmacokinetic/pharmacodynamic study comparing a single morning dose of adderall to twice-daily dosing in children with ADHD. J Am Acad Child Adolesc Psychiatry. 2003;42:1234–41. doi: 10.1097/00004583-200310000-00015. PMID: 14560174. [DOI] [PubMed] [Google Scholar]
- 47.Greenhill LL, Muniz R, Ball RR, Levine A, Pestreich L, Jiang H. Efficacy and safety of dexmethylphenidate extended-release capsules in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006;45:817–23. doi: 10.1097/01.chi.0000220847.41027.5d. PMID: 16832318. [DOI] [PubMed] [Google Scholar]
- 48.Greenhill LL, Posner K, Vaughan BS, Kratochvil CJ. Child Adolesc Psychiatr Clin N Am. Attention deficit hyperactivity disorder in preschool children. 2008;17:347–66. doi: 10.1016/j.chc.2007.11.004. PMID: 18295150. [DOI] [PubMed] [Google Scholar]
- 49.Guieu R, Couraud F, Pouget J. Adenosine and the nervous system: Clinical implications. Clin Neuropharmacol. 1996;19:459–74. doi: 10.1097/00002826-199619060-00001. PMID: 8937786. [DOI] [PubMed] [Google Scholar]
- 50.Halevy A, Shuper A. Methylphenidate induction of complex visual hallucinations. J Child Neurol. 2009;24:1005–7. doi: 10.1177/0883073808331357. PMID: 19502578. [DOI] [PubMed] [Google Scholar]
- 51.Hammerness P, McCarthy K, Mancuso E, Gendron C, Geller D. Atomoxetine for the treatment of attention-deficit/hyperactivity disorder in children and adolescents: A review. Neuropsychiatr Dis Treat. 2009a;5:215–26. doi: 10.2147/ndt.s3896. PMID: 19557116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hammerness P, Doyle R, Kotarski M, Georgiopoulos A, Joshi G, Zeitlin S. Atomoxetine in children with attention-deficit hyperactivity disorder with prior stimulant therapy: A prospective open-label study. Eur Child Adolesc Psychiatry. 2009b;18:493–8. doi: 10.1007/s00787-009-0017-8. PMID: 19377865. [DOI] [PubMed] [Google Scholar]
- 53.Hechtman L. Treatment of attention deficit hyperactivity disorder in patients unresponsive to stimulants. J Psych Neurosci. 2011;36:216–8. PMID: 21496443. [Google Scholar]
- 54.Hermens DF, Rowe DL, Gordon E, Williams LM. Integrative neuroscience approach to predict ADHD stimulant response. Expert Rev Neurother. 2006;6:753–63. doi: 10.1586/14737175.6.5.753. PMID: 16734523. [DOI] [PubMed] [Google Scholar]
- 55.Jaanus SD. Ocular side-effects of selected systemic drugs. Optom Clin. 1992;2:73–96. PMID: 1363080. [PubMed] [Google Scholar]
- 56.Kashani J, Ruha AM. Isolated atomoxetine overdose resulting in seizure. J Emerg Med. 2007;32:175–8. doi: 10.1016/j.jemermed.2006.05.048. PMID: 17307628. [DOI] [PubMed] [Google Scholar]
- 57.Keenan K, Wakschlag LS. More than the terrible twos: the nature and severity of behavioural problems in clinic-referred preschool children. J Abnorm Child Psychol. 2000;28:33–46. doi: 10.1023/a:1005118000977. PMID: 10772348. [DOI] [PubMed] [Google Scholar]
- 58.Kelsey DK, Sumner CR, Casat CD, Coury DL, Quintana H, Saylor KE, et al. Once-daily atomoxetine treatment for children with attention-deficit/hyperactivity disorder, including an assessment of morning and evening behavior: A double-blind placebo-controlled trial. Pediatrics. 2004;114:e1–8. doi: 10.1542/peds.114.1.e1. PMID: 15231966. [DOI] [PubMed] [Google Scholar]
- 59.Kollins S, Greenhill LL, Swanson J, Wigal S, Abikoff H, McCracken J, et al. Rationale, design, and methods of the Preschool ADHD Treatment Study (PATS) J Am Acad Child Adolesc Psychiatry. 2006;45:1275–83. doi: 10.1097/01.chi.0000235074.86919.dc. PMID: 17023869. [DOI] [PubMed] [Google Scholar]
- 60.Kratochvil CJ, Wilens TE, Greenhill LL, Gao H, Baker KD, Feldman PD, et al. Effects of long-term atomoxetine treatment for young children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006;45:919–27. doi: 10.1097/01.chi.0000222788.34229.68. PMID: 16865034. [DOI] [PubMed] [Google Scholar]
- 61.Kratochvil CJ, Vaughan BS, Mayfield-Jorgensen ML, March JS, Kollins SH, Murray DW, et al. A pilot study of atomoxetine in young children with attention-deficit/ hyperactivity disorder. J Child Adolesc Psychopharmacol. 2007;17:175–85. doi: 10.1089/cap.2006.0143. PMID: 17489712. [DOI] [PubMed] [Google Scholar]
- 62.Kratochvil CJ, Vaughan BS, Stoner JA, Daughton JM, Lubberstedt BD, Murray DW, et al. A double blind placebo controlled trial of atomoxetine in young children with attention deficit hyperactivity disorder. Pediatrics. 2011;127:862–8. doi: 10.1542/peds.2010-0825. PMID: 21422081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kurlan R. Tourette's syndrome: are stimulants safe? Curr Neurol Neurosci Rep. 2003;3:285–8. doi: 10.1007/s11910-003-0004-2. PMID: 12930697. [DOI] [PubMed] [Google Scholar]
- 64.Ledbetter M. Atomoxetine use associated with onset of a motor tic. J Child Adolesc Psychopharmacol. 2005;15:331–3. doi: 10.1089/cap.2005.15.331. PMID: 15910218. [DOI] [PubMed] [Google Scholar]
- 65.Manos MJ, Tom-Revzon C, Bukstein OG, Crismon ML. Changes and challenges: managing ADHD in a fast-paced world. J Manag Care Pharm. 2007;13(9 Suppl B):S2–13. doi: 10.18553/jmcp.2007.13.9-b.1. PMID: 18062734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mannuzza S, Klein RG, Truong NL, Moulton JL, 3rd, Roizen ER, Howell KH, et al. Age of methylphenidate treatment initiation in children with ADHD and later substance abuse: Prospective follow-up into adulthood. Am J Psychiatry. 2008;165:604–9. doi: 10.1176/appi.ajp.2008.07091465. PMID: 18381904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.March JS. The Preschool ADHD Treatment Study (PATS) as the culmination of 20 years of clinical trials in pediatric psychopharmacology. J Am Acad Child Adolesc Psychiatry. 2011;50:427–30. doi: 10.1016/j.jaac.2010.09.018. PMID: 21515189. [DOI] [PubMed] [Google Scholar]
- 68.May DE, Kratochvil CJ. Attention-deficit hyperactivity disorder: Recent advances in paediatric pharmacotherapy. Drugs. 2010;70:15–40. doi: 10.2165/11530540-000000000-00000. PMID: 20030423. [DOI] [PubMed] [Google Scholar]
- 69.McGough JJ, Biederman J, Wigal SB, Lopez FA, McCracken JT, Spencer T, et al. Long-term tolerability and effectiveness of once-daily mixed amphetamine salts (Adderall XR) in children with ADHD. J Am Acad Child Adolesc Psychiatry. 2005;44:530–8. doi: 10.1097/01.chi.0000157550.94702.a2. PMID: 15908835. [DOI] [PubMed] [Google Scholar]
- 70.McBurnett K, Starr HL. OROS Methylphenidate for adult patients with attention deficit hyperactivity disorder. Exp Opin Pharmacother. 2011;12:315–24. doi: 10.1517/14656566.2011.546058. PMID: 21226641. [DOI] [PubMed] [Google Scholar]
- 71.McGough JJ. Attention- deficit/hyperactivity disorder pharmacogenomics. Biol Psychiatry. 2005;57:1367–73. doi: 10.1016/j.biopsych.2004.10.021. PMID: 15950009. [DOI] [PubMed] [Google Scholar]
- 72.Michelson D, Allen AJ, Busner J, Casat C, Dunn D, Kratochvil CJ, et al. Once daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: A randomized placebo controlled study. Am J Psychiatry. 2002;159:1896–901. doi: 10.1176/appi.ajp.159.11.1896. PMID: 12411225. [DOI] [PubMed] [Google Scholar]
- 73.Mikami AY, Cox DJ, Davis MT, Wilson K, Merkel RL, Burket R. Sex differences in the efficacy of extended release methylphenidate among adolescents with ADHD. J Clin Psychol Med Settings. 2009;16:233–42. doi: 10.1007/s10880-009-9165-8. PMID: 19418208. [DOI] [PubMed] [Google Scholar]
- 74.Mohammadi MR, Ghanizadeh A, Alaghband-Rad J, Tehranidoost M, Mesgarpour B, Soori H. Selegiline in comparison with methylphenidate in attention deficit hyperactivity disorder in children and adolescents in a double-blind, randomized clinical trial. J Child Adolesc Psychopharmacol. 2004a;14:418–25. doi: 10.1089/cap.2004.14.418. PMID: 15650498. [DOI] [PubMed] [Google Scholar]
- 75.Mohammadi MR, Kashani L, Akhondzadeh S, Izadian ES, Ohadinia S. Efficacy of theophylline compared to methylphenidate for the treatment of attention-deficit hyperactivity disorder in children and adolescents: A pilot double-blind randomized trial. J Clin Pharm Ther. 2004b;29:129–44. doi: 10.1111/j.1365-2710.2004.00545.x. PMID: 15068402. [DOI] [PubMed] [Google Scholar]
- 76.Murray DW. Treatment of pre-schoolers with attention-deficit/hyperactivity disorder. Curr Psychiatry Rep. 2010;12:374–81. doi: 10.1007/s11920-010-0142-6. PMID: 20676944. [DOI] [PubMed] [Google Scholar]
- 77.Najib J. The efficacy and safety profile of lisdexamfetamine dimesylate, a prodrug of d-amphetamine, for the treatment of attention-deficit/hyperactivity disorder in children and adults. Clin Ther. 2009;31:142–76. doi: 10.1016/j.clinthera.2009.01.015. PMID: 19243715. [DOI] [PubMed] [Google Scholar]
- 78.MTA Cooperative Group. National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: Changes in effectiveness and growth after the end of treatment. Pediatrics. 2004;113:762–9. doi: 10.1542/peds.113.4.762. PMID: 15060225. [DOI] [PubMed] [Google Scholar]
- 79.Narahashi T, Moriguchi S, Zhao X, Marszalec W, Yeh JZ. Mechanisms of action of cognitive enhancers on neuroreceptors. Biol Pharm Bull. 2004;27:1701–6. doi: 10.1248/bpb.27.1701. PMID: 15516710. [DOI] [PubMed] [Google Scholar]
- 80.Newcorn JH, Kratochvil CJ, Allen AJ, Casat CD, Ruff DD, Moore RJ, et al. Atomoxetine and osmotically released methylphenidate for the treatment of attention deficit hyperactivity disorder: Acute comparison and differential response. Am J Psychiatry. 2008;165:721–30. doi: 10.1176/appi.ajp.2007.05091676. PMID: 18281409. [DOI] [PubMed] [Google Scholar]
- 81.Párraga HC, Párraga MI, Harris DK. Tic exacerbation and precipitation during atomoxetine treatment in two children with attention-deficit hyperactivity disorder. Int J Psychiatry Med. 2007;37:415–24. doi: 10.2190/PM.37.4.e. PMID: 18441629. [DOI] [PubMed] [Google Scholar]
- 82.Patrick KS, Markowitz JS. Pharmacology of methylphenidate, amphetamine enantiomers and pemoline in attention-deficit hyperactivity disorder. Hum Psychopharmacol. 1997;12:527–46. [ABSTRACT ] [FULL TEXT ] [PUBMED ] [Google Scholar]
- 83.Pelham WE, Gnagy EM, Burrows-Maclean L, Williams A, Fabiano GA, Morrisey SM, et al. Once-a-day Concerta methylphenidate versus three-times-daily methylphenidate in laboratory and natural settings. Pediatrics. 2001;107:E105. doi: 10.1542/peds.107.6.e105. PMID: 11389303. [DOI] [PubMed] [Google Scholar]
- 84.Pelham WE, Manos MJ, Ezzell CE, Tresco KE, Gnagy EM, Hoffman MT, et al. A dose ranging study of methylphenidate transdermal system in children with ADHD. J Am Acad Child Adolesc Psychiatry. 2005;44:522–9. doi: 10.1097/01.chi.0000157548.48960.95. PMID: 15908834. [DOI] [PubMed] [Google Scholar]
- 85.Pelham WE, Jr, Fabiano GA. Evidence-based psychosocial treatment for attention-deficit/hyperactivity disorder: An update. J Clin Child Adolesc Psychol. 2008;37:184–214. doi: 10.1080/15374410701818681. PMID: 18444058. [DOI] [PubMed] [Google Scholar]
- 86.Perrin JM, Friedman RA, Knilans TK Black Box Working Group. Section on Cardiology and Cardiac Surgery. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451–3. doi: 10.1542/peds.2008-1573. PMID: 18676566. [DOI] [PubMed] [Google Scholar]
- 87.Pliszka SR, Browne RG, Olvera RL, Wynne SK. A double-blind, placebo-controlled study of Adderall and methylphenidate in the treatment of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2000;39:619–26. doi: 10.1097/00004583-200005000-00016. PMID: 10802980. [DOI] [PubMed] [Google Scholar]
- 88.Polzer J, Bangs ME, Zhang S, Dellva MA, Tauscher-Wisniewski S, Acharya N, et al. Meta-analysis of aggression or hostility events in randomized, controlled clinical trials of atomoxetine for ADHD. Biol Psychiatry. 2007;61:713–9. doi: 10.1016/j.biopsych.2006.05.044. PMID: 16996485. [DOI] [PubMed] [Google Scholar]
- 89.Popovic B, Bhattacharya P, Sivaswamy L. Lisdexamfetamine: A prodrug for the treatment of attention-deficit/hyperactivity disorder. Am J Health Syst Pharm. 2009;66:2005–12. doi: 10.2146/ajhp080353. PMID: 19890083. [DOI] [PubMed] [Google Scholar]
- 90.Posner K, Melvin GA, Murray DW, Gugga SS, Fisher P, Skrobala A, Cunningham C, et al. Clinical presentation of attention-deficit/hyperactivity disorder in preschool children: the Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS) J Child Adolesc Psychopharmacol. 2007;17:547–62. doi: 10.1089/cap.2007.0075. PMID: 17979577. [DOI] [PubMed] [Google Scholar]
- 91.Potter AS, Newhouse PA. Effects of acute nicotine administration on behavioral inhibition in adolescents with attention-deficit/hyperactivity disorder. Psychopharmacology (Berl) 2004;176:182–94. doi: 10.1007/s00213-004-1874-y. PMID: 15083253. [DOI] [PubMed] [Google Scholar]
- 92.Prince JB, Wilens TE, Biederman J, Spencer TJ, Wozniak JR. Clonidine for sleep disturbances associated with attention-deficit hyperactivity disorder: A systematic chart review of 62 cases. J Am Acad Child Adolesc Psychiatry. 1996;35:599–605. doi: 10.1097/00004583-199605000-00014. PMID: 8935206. [DOI] [PubMed] [Google Scholar]
- 93.Prince JB. Pharmacotherapy of attention-deficit hyperactivity disorder in children and adolescents: Update on new stimulant preparations, atomoxetine and novel treatments. Child Adolesc Psychiatr Clin N Am. 2006;15:13–50. doi: 10.1016/j.chc.2005.08.002. PMID: 16321724. [DOI] [PubMed] [Google Scholar]
- 94.Pringsheim T, Steeves T. Pharmacological treatment for Attention Deficit Hyperactivity Disorder (ADHD) in children with comorbid tic disorders. Cochrane Database Syst Rev. 2011;4:CD007990. doi: 10.1002/14651858.CD007990.pub2. PMID: 21491404. [DOI] [PubMed] [Google Scholar]
- 95.Quintana H, Cherlin EA, Duesenberg DA, Bangs ME, Ramsey JL, Feldman PD, et al. Transition from methylphenidate or amphetamine to atomoxetine in children and adolescents with attention-deficit/hyperactivity disorder: a preliminary tolerability and efficacy study. Clin Ther. 2007;29:1168–77. doi: 10.1016/j.clinthera.2007.06.017. PMID: 17692731. [DOI] [PubMed] [Google Scholar]
- 96.Rapport MD, Moffitt C. Attention deficit/hyperactivity disorder and methylphenidate: A review of height/weight, cardiovascular and somatic complaint side effects. Clin Psychol Rev. 2002;22:1107–31. doi: 10.1016/s0272-7358(02)00129-0. PMID: 12436807. [DOI] [PubMed] [Google Scholar]
- 97.Ratner S, Laor N, Bronstein Y, Weizman A, Toren P. Six-week open-label reboxetine treatment in children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:428–33. doi: 10.1097/01.chi.0000155327.30017.8c. PMID: 15843764. [DOI] [PubMed] [Google Scholar]
- 98.Rezvani AH, Levin ED. Cognitive effects of nicotine. Biol Psychiatry. 2001;49:258–67. doi: 10.1016/s0006-3223(00)01094-5. PMID: 11230877. [DOI] [PubMed] [Google Scholar]
- 99.Safer DJ, Zito JM, Gardner JE. Pemoline hepatotoxicity and post marketing surveillance. J Am Acad Child Adolesc Psychiatry. 2001;40:622–9. doi: 10.1097/00004583-200106000-00006. PMID: 11392339. [DOI] [PubMed] [Google Scholar]
- 100.Sallee FR, Stiller RL, Perel JM. Pharmacodynamics of pemoline in attention deficit disorder with hyperactivity. J Am Acad Child Adolesc Psychiatry. 1992;31:244–51. doi: 10.1097/00004583-199203000-00010. PMID: 1564025. [DOI] [PubMed] [Google Scholar]
- 101.Sallee FR, Lyne A, Wigal T, McGough JJ. Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19:215–26. doi: 10.1089/cap.2008.0080. PMID: 19519256. [DOI] [PubMed] [Google Scholar]
- 102.Sallee FR. The role of alpha-2-adrenergic agonists in attention-deficit/hyperactivity disorder. Postgrad Med. 2010;122:78–87. doi: 10.3810/pgm.2010.09.2204. PMID: 20861591. [DOI] [PubMed] [Google Scholar]
- 103.Santosh PJ, Baird G, Pityaratstian N, Tavare E, Gringras P. Impact of comorbid autism spectrum disorders on stimulant response in children with attention deficit hyperactivity disorder: A retrospective and prospective effectiveness study. Child Care Health Dev. 2006;32:575–83. doi: 10.1111/j.1365-2214.2006.00631.x. PMID: 16919137. [DOI] [PubMed] [Google Scholar]
- 104.Sears J, Patel NC. Development of tics in a thirteen-year-old male following atomoxetine use. CNS Spectr. 2008;13:301–3. doi: 10.1017/s1092852900016412. PMID: 18408649. [DOI] [PubMed] [Google Scholar]
- 105.Shastri PC, Shastri J, Shastri DJ. Research in child and adolescent psychiatry in India. Indian J Psychiatry. 2010;52:219–23. doi: 10.4103/0019-5545.69235. PMID: 21836681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sitholey P, Agarwal V, Chamoli S. A preliminary study of factors affecting adherence to medication in clinic children with attention deficit hyperactivity disorder. Indian J Psychiatry. 2011;53:41–4. doi: 10.4103/0019-5545.75561. PMID: 21431007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Silva R, Tilker HA, Cecil JT, Kovalik S, Khetani V, Faleck H, et al. Open-label study of dexmethylphenidate hydrochloride in children and adolescents with attention deficit hyperactivity disorder. J Child Adolesc Psychopharmacol. 2004;14:555–63. doi: 10.1089/cap.2004.14.555. PMID: 21431007. [DOI] [PubMed] [Google Scholar]
- 108.Simpson D, Plosker GL. Atomoxetine: A review of its use in adults with attention deficit hyperactivity disorder. Drugs. 2004;64:205–22. doi: 10.2165/00003495-200464020-00005. PMID: 14717619. [DOI] [PubMed] [Google Scholar]
- 109.Sonuga-Barke EJ, Daley D, Thompson M, Swanson J. Preschool ADHD: Exploring uncertainties in diagnostic validity and utility, and treatment efficacy and safety. Expert Rev Neurother. 2003;3:465–76. doi: 10.1586/14737175.3.4.465. PMID: 19810931. [DOI] [PubMed] [Google Scholar]
- 110.Spencer T, Biederman J, Heiligenstein J, Wilens T, Faries D, Prince J, et al. An open-label, dose-ranging study of atomoxetine in children with attention deficit hyperactivity disorder. J Child Adolesc Psychopharmacol. 2001;11:251–65. doi: 10.1089/10445460152595577. PMID: 11642475. [DOI] [PubMed] [Google Scholar]
- 111.Spencer TJ, Kratochvil CJ, Sangal RB, Saylor KE, Bailey CE, Dunn DW, et al. Effect of atomoxetine on growth in children with attention-deficit/hyperactivity disorder following upto five years of treatment. J Child Adolesc Psychopharmacol. 2007;17:689–700. doi: 10.1089/cap.2006.0100. PMID: 17979588. [DOI] [PubMed] [Google Scholar]
- 112.Spencer TJ, Greenbaum M, Ginsberg LD, Murphy WR. Safety and effectiveness of coadministration of guanfacine extended release and psychostimulants in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19:501–10. doi: 10.1089/cap.2008.0152. PMID: 19877974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Spiller HA, Lintner CP, Winter ML. Atomoxetine ingestions in children: A report from poison centers. Ann Pharmacother. 2005;39:1045–48. doi: 10.1345/aph.1E646. PMID: 15870137. [DOI] [PubMed] [Google Scholar]
- 114.Steele M, Ricardelli R, Binder C. Effectiveness of OROS methylphenidate versus usual care with immediate release methylphenidate in ADHD children. Paper presented at the American Psychiatric Society Annual Meeting, New York (NY), May 1st to 6th. 2004 [Google Scholar]
- 115.Stein MA, Sarampote CS, Waldman ID, Robb AS, Conlon C, Pearl PL, et al. A dose-response study of OROS methylphenidate in children with attention-deficit/hyperactivity disorder. Pediatrics. 2003;112:e404. doi: 10.1542/peds.112.5.e404. PMID: 14595084. [DOI] [PubMed] [Google Scholar]
- 116.Stein MA, McGough JJ. The pharmacogenomic era: promise for personalizing attention deficit hyperactivity disorder therapy. Child Adolesc Psychiatr Clin N Am. 2008;17:475–90. doi: 10.1016/j.chc.2007.11.009. PMID: 18295157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Stiefel G, Besag FM. Cardiovascular side effects of methylphenidate, amphetamines and atomoxetine in the treatment of attention deficit hyperactivity disorder. Drug Safety. 2010;33:821–42. doi: 10.2165/11536380-000000000-00000. PMID: 20812768. [DOI] [PubMed] [Google Scholar]
- 118.Swanson J, Kinsbourne M, Roberts W, Zucker K. Time-response analysis of the effect of stimulant medication on the learning ability of children referred for hyperactivity. Pediatrics. 1978;61:21–9. PMID: 400817. [PubMed] [Google Scholar]
- 119.Swanson JM, Lerner M, Wigal T, Steinhoff K, Greenhill L, Posner K, et al. The use of a laboratory school protocol to evaluate concepts about efficacy and side effects of new formulations of stimulant medications. J Atten Disord. 2002;6(suppl 1):S73–88. doi: 10.1177/070674370200601s10. PMID: 12685522. [DOI] [PubMed] [Google Scholar]
- 120.Swanson J, Gupta S, Lam A, Shoulson I, Lerner M, Modi N, et al. Development of a new once-a-day formulation of methylphenidate for the treatment of attention-deficit/hyperactivity disorder: Proof-of-concept and proof-of-product studies. Arch Gen Psychiatry. 2003;60:204–11. doi: 10.1001/archpsyc.60.2.204. PMID: 12578439. [DOI] [PubMed] [Google Scholar]
- 121.Swanson J, Baler RD, Volkow ND. Understanding the effects of stimulant medications on cognition in individuals with attention-deficit hyperactivity disorder: A decade of progress. Neuropsychopharmacology. 2011;36:207–26. doi: 10.1038/npp.2010.160. PMID: 20881946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tjon Pian Gi CV, Broeren JP, Starreveld JS, Versteegh FG. Melatonin for the treatment of sleeping disorders in children with attention deficit/hyperactivity disorder: A preliminary open label study. Eur J Pediatr. 2003;162:554–5. doi: 10.1007/s00431-003-1207-x. PMID: 12783318. [DOI] [PubMed] [Google Scholar]
- 123.Upadhyaya HP, Brady KT, Wang W. Bupropion SR in adolescents with comorbid ADHD and nicotine dependence: A pilot study. J Am Acad Child Adolesc Psychiatry. 2004;43:199–205. doi: 10.1097/00004583-200402000-00016. PMID: 14726727. [DOI] [PubMed] [Google Scholar]
- 124.Vitiello B. Psychopharmacology for young children: Clinical needs and research opportunities. Pediatrics. 2001:108983–3. doi: 10.1542/peds.108.4.983. PMID: 11581454. [DOI] [PubMed] [Google Scholar]
- 125.Volkow ND, Fowler JS, Wang G, Ding Y, Gatley SJ. Mechanism of action of methylphenidate: Insights from PET imaging studies. J Atten Disord. 2002;6(Suppl 1):S31–43. doi: 10.1177/070674370200601s05. PMID: 12685517. [DOI] [PubMed] [Google Scholar]
- 126.Wang Y, Zheng Y, Du Y, Song DH, Shin YJ, Cho SC, et al. Atomoxetine versus methylphenidate in paediatric outpatients with attention deficit hyperactivity disorder: A randomized, double-blind comparison trial. Aust N Z J Psychiatry. 2007;41:222–30. doi: 10.1080/00048670601057767. PMID: 17464703. [DOI] [PubMed] [Google Scholar]
- 127.Weiss M, Tannock R, Kratochvil C, Dunn D, Velez-Borras J, Thomason C, et al. A randomized, placebo-controlled study of once-daily atomoxetine in the school setting in children with ADHD. J Am Acad Child Adolesc Psychiatry. 2005;44:647–55. doi: 10.1097/01.chi.0000163280.47221.c9. PMID: 15968233. [DOI] [PubMed] [Google Scholar]
- 128.Wernicke JF, Holdridge KC, Jin L, Edison T, Zhang S, Bangs ME, et al. Seizure risk in patients with attention-deficit-hyperactivity disorder treated with atomoxetine. Dev Med Child Neurol. 2007;49(7):498–502. doi: 10.1111/j.1469-8749.2007.00498.x. PMID: 17593120. [DOI] [PubMed] [Google Scholar]
- 129.Wigal S, Swanson JM, Feifel D, Sangal RB, Elia J, Casat CD, et al. A double-blind, placebo-controlled trial of dexmethylphenidate and d,l-threo-methylphenidate in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2004;43:1406–14. doi: 10.1097/01.chi.0000138351.98604.92. PMID: 15502600. [DOI] [PubMed] [Google Scholar]
- 130.Wigal SB, McGough JJ, McCracken JT, Biederman J, Spencer TJ, Posner KL, et al. A laboratory school comparison of mixed amphetamine salts extended release (Adderall XR) and atomoxetine (Strattera) in school aged children with attention deficit/hyperactivity disorder. J Atten Disord. 2005;9:275–89. doi: 10.1177/1087054705281121. PMID: 16371674. [DOI] [PubMed] [Google Scholar]
- 131.Wigal SB. Efficacy and safety limitations of attention-deficit hyperactivity disorder pharmacotherapy in children and adults. CNS Drugs. 2009;23(Suppl 1):21–31. doi: 10.2165/00023210-200923000-00004. PMID: 19621975. [DOI] [PubMed] [Google Scholar]
- 132.Wilens TE, Biederman J, Wong J, Spencer TJ, Prince JB. Adjunctive donepezil in attention deficit hyperactivity disorder youth: case series. J Child Adolesc Psychopharmacol. 2000;10:217–22. doi: 10.1089/10445460050167322. PMID: 11052411. [DOI] [PubMed] [Google Scholar]
- 133.Wilens T, Pelham W, Stein M, Conners CK, Abikoff H, Atkins M, et al. ADHD treatment with once-daily OROS methylphenidate: interim 12-month results from a long term open-label study. J Am Acad Child Adolesc Psychiatry. 2003a;42:424–33. doi: 10.1097/01.CHI.0000046814.95464.7D. PMID: 12649629. [DOI] [PubMed] [Google Scholar]
- 134.Wilens TE, Faraone SV, Biederman J, Gunawardene S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003b;111:179–85. doi: 10.1542/peds.111.1.179. PMID: 12509574. [DOI] [PubMed] [Google Scholar]
- 135.Wilens TE, Biederman J, Lerner M Concerta Study Group. Effects of once-daily osmotic-release methylphenidate on blood pressure and heart rate in children with attention-deficit/hyperactivity disorder: Results from a one-year follow-up study. J Clin Psychopharmacol. 2004;24:36–41. doi: 10.1097/01.jcp.0000106223.36344.df. PMID: 14709945. [DOI] [PubMed] [Google Scholar]
- 136.Wilens TE, Haight BR, Horrigan JP, Hudziak JJ, Rosenthal NE, Connor DF, et al. , Buproprion XL in adults with attention-deficit/hyperactivity disorder: A randomized placebo-controlled study. Biol Psychiatry. 2005;57:793–801. doi: 10.1016/j.biopsych.2005.01.027. PMID: 15820237. [DOI] [PubMed] [Google Scholar]
- 137.Wolraich ML, Lindgren S, Stromquist A, Milich R, Davis C, Watson D. Stimulant medication use by primary care physicians in the treatment of attention deficit hyperactivity disorder. Pediatrics. 1990;86:95–101. PMID: 2359688. [PubMed] [Google Scholar]
- 138.Wolraich ML, Greenhill LL, Pelham W, Swanson J, Wilens T, Palumbo D, et al. Randomized, controlled trial of OROS methylphenidate once a day in children with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108:883–92. doi: 10.1542/peds.108.4.883. PMID: 11581440. [DOI] [PubMed] [Google Scholar]
- 139.Wolraich ML, Bard DE, Stein MT, Rushton JL, O’Connor KG. Pediatrician's attitudes and practice on ADHD before and after the development of ADHD practice guidelines. J Atten Disord. 2010;13:563–72. doi: 10.1177/1087054709344194. PMID: 19706877. [DOI] [PubMed] [Google Scholar]