Abstract
The consequences of stigma are preventable. We argue that individual attention should be provided to patients when dealing with stigma. Also, in order to deal with the impact of stigma on an individual basis, it needs to be assessed during routine clinical examinations, quantified and followed up to observe whether or not treatment can reduce its impact. A patient-centric anti-stigma programme that delivers the above is urgently needed. To this end, this review explores the experiences, treatment barriers and consequences due to stigma. We also offer putative solutions to this problem.
Keywords: Barriers, Compliance, Intervention, Psychosis, Schizophrenia, Stigma, Treatment
Introduction
In part one of this two-part review (see this issue) we explored the causes of stigma and how they impact those with psychiatric illnesses, especially patients with psychosis. We illustrated that there are significant clinical consequences in which the mentally ill are discriminated against making it more likely that they will not seek treatment. Thus, there is obvious clinical risk associated with stigma.
In part two we continue to discuss stigma but emphasise non-compliance issues. We then suggest ways of combating stigma, first by dealing with stigma in the age old way of education, but we will follow that up by suggesting a new and novel client-centric approach in which the client is assessed with respect to the impact of stigma before and after stigma related intervention. We propose that the impact in terms of perception of stigma by the client should be addressed and assessed in the clinic. With specific interventions, the impact could be reduced leading to better compliance to treatment.
Non-compliance
Self-stigma is defined as a devaluation of the self by internalising negative stereotypes they attribute to themselves or/and attributed to them from external sources (Fung et al., 2007[7]). A study by Fung et al., (2008[6]) has found that self-stigma is one of the contributing factors in undermining treatment adherence. Individuals with schizophrenia often endorse a feeling of self-disregard and incompetence (Lysaker et al., 2008a[15], 2008b[16]). It may be possible that their self-stigmatised thoughts might, therefore, reduce their motivation and thus readiness for seeking therapy [Figure 1].
Figure 1.
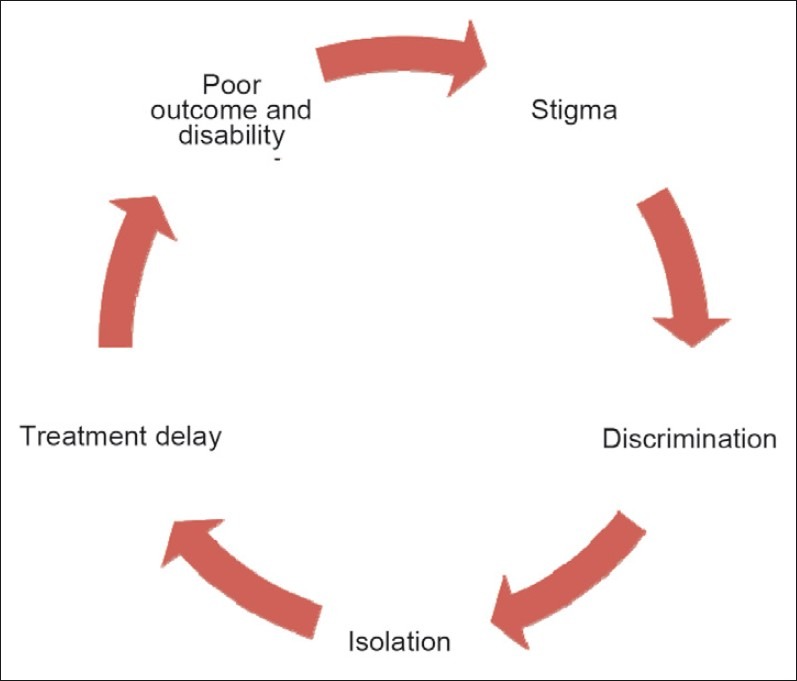
Circle of cause and effect from stigma. From this figure we suggest that stigma is interrelated with many other factors such as discrimination, isolation, and finally outcome.
Throughout history and in practically every culture, groups of persons, including mental patients, have been stigmatised. The reasons for such stigmatisation and its maintenance remain obscure. Its association to non adherence to treatment is common but unfortunately difficult to detect in patients with schizoaffective disorder and schizophrenia, of whom almost half take less than 70% of prescribed doses (Goff et al., 2010[8]). Like patients in all areas of medicine, patients with schizoaffective disorder weigh the perceived benefits of medications against perceived disadvantages; but this process is complicated by their impaired insight, the stigma of the diagnosis, and the often troubling side effects of antipsychotic medication. Interventions to improve adherence include encouraging acceptance of the illness, drawing analogies with treatment for chronic medical disease, and involving the patient in decision-making. Clinicians are required to remain non-judgemental, encouraging patients to disclose problems with adherence and anticipating that improvement in adherence may require a prolonged effort. Selection of antipsychotic medication is critical to avoid adverse side effects, and some medications may provide a sense of well-being, such as improvement in insomnia, anxiety, or depression (Goff et al., 2010[8]).
Research suggests that the stigma of mental illness can impair treatment utilization in two ways:
Through perceived public stigma, individuals with mental illness may seek to avoid the public label and stigmatisation of mental illness by choosing not to seek treatment or to discontinue treatment prematurely, and,
Through internalised stigma, individuals with mental illness may seek to avoid the negative feelings of shame and guilt about themselves by choosing not to seek treatment. These two constructs, public and internalised stigma, are manifest differently within individuals, but they clearly influence each other in their impact on the stigmatised individual. If an individual with mental illness perceives public stigma to be high, they may be more likely to internalise these negative stereotypes than if they perceive public stigma about mental illness to be low (Corrigan, 2004[3]).
Studies also show that interpersonal, economic, and policy factors also mitigate service use. For instance, patients with schizophrenia are less likely to perceive benefits of medications, due to their impaired insight, the stigma of the diagnosis, and the often troubling side effects of antipsychotic medication. Interventions to improve adherence include encouraging acceptance of the illness, drawing analogies with treatments for chronic medical diseases, and involving the patient in decision-making. Pandya et al., (2010[19]) reported that stigma must be understood through individual experience in specific contexts rather than as a unitary experience. They studied whether diagnosis disclosure can be beneficial. A convenience sample of 258 adults with schizophrenia recruited via the Internet and e-mail lists completed an online survey. Although reactions to disclosure varied, many report worse treatment by police (Patch et al., 1999[21]) and better treatment by parents after disclosure (Pandya, et al., 2010[19]). Many also experience worse treatment for medical problems after disclosing their schizophrenia diagnosis. These results emphasise the support for targeted anti-stigma interventions.
In a one-year cross-sectional study with 105 participants face-to-face interviews were conducted to assess participants’ level of self-stigma, readiness for change, insight, and general self-efficacy. The corresponding case therapists in this study reported participants’ level of treatment adherence, psychopathology, and global functioning. The study found that better readiness for action, and lower levels of self-stigma were associated with better treatment participation. Individuals with lesser severity of psychiatric symptoms and female participants had better treatment attendance. The results of a discriminant function analysis showed the combined scores of self-stigma, stages of change, and global functioning measures correctly classified 76.2% participants into adherent/non adherent group membership. Suggestions for further studies and development of self-stigma reduction programme to facilitate recovery and treatment adherence were made (Tsang et al., 2010[29]).
A critical component of stigma in schizophrenia is the perception that patients are extremely dangerous. The assessment of this concept in the general population by the use of reliable and valid instruments will allow the development of programmes aimed to reduce it. In one study designed to develop an assessment instrument of the public conception of aggressiveness in schizophrenia and to determine its reliability and validity in a community, they reported that more than 40% of the sample of Mexico City authors considered that a patient with schizophrenia was aggressive and dangerous. The CAQ had an adequate internal consistency (alpha=0.74). The results of the factorial analysis showed that two factors explained 61% of the variance. The items of CAQ showed two major areas to evaluate: a) perception of the presentation of aggressive behaviours; and, b) mental illness recognition and social aspects of the stigma of dangerousness. The CAQ is an instrument with adequate psychometric properties that could be useful to evaluate the perception of aggressiveness in schizophrenia among the general population (Fresán et al., 2010[5]).
Combating Stigma
Experiments in dealing with stigma
Dealing with stigma is the first step in treatment and prevention of mental illness. There has been a strong focus on combating stigma from national and international psychiatric organisations, community leaders, mental health professionals and advocacy groups. Despite volumes of literature on stigma it is not completely understood and making specific standardised intervention is difficult to implement.
There are three important targets for combating stigma:
Interventions for the general public;
Intervention for improving image of psychiatry; and,
Interventions for dealing with stigmatising by psychiatrists.
It is best to deal with stigma on a one-to-one basis that allows for superior communication between the mental health professional and the patient. Only then can the mental health professional assess for qualitative change in the patient's life. A common approach at reducing stigma has been to target the sources themselves. In general these initiatives have been based upon public education and awareness with the assumption that flooding the public with more information about mental illness may decrease stigma and in turn improve the lives of patients and family members alike. In fact there is some evidence that improving people's knowledge about mental disorders during a “mental health first aid course” improves concordance with generally recommended therapies (Kitchener et al., 2004[11]). There is also some evidence that attitudes towards community-based facilities could be improved by providing information (Wolff et al., 1996[32]). It has been addressed at the level of: 1) People at large; 2) Patients and relatives; 3) Psychiatry as a discipline; and, 4) Mental health professionals and general health professionals. Accordingly, interventional studies have focused on all of the above targets.
Important methods used in combating stigma are focused on changing the public stigma of mental illnesses utilising models of protest, education and public contact, all targeted at local stigma change. These experiments have tried to make anti-stigma programmes a compelling agenda. Education, both conventional and web-based, has been successful. It has also been proposed to change the label of ‘mental illness’ under the presumption that the label itself is a source of stigma. School based programmes, for example, Battaglia et al. (1990[1]) found that a presentation given by a psychiatrist on mental health issues for high school students not only improved knowledge about mental health, but also improved help-seeking attitudes and appreciation of psychiatrists, possibly due to greater familiarity.
Imparting education that mental illnesses are biological is a double edge sword. On one side it generates hope that the aetiology has been known while one the other side people compare it with brain diseases with no answer and hope of recovery e.g. mental retardation. This approach has been criticized. More visible presence of psychiatry and psychiatric treatment is the present need (Stuart, 2006[27]). A series of recommendations have been made for national psychiatric societies and for individual psychiatrists. It has been a hope that psychiatrists can play a central role in the prevention of stigmatisation of psychiatry by stressing the need to develop a respectful relationship with patients, to strictly observe ethical rules in the practice of psychiatry, and to maintain professional competence. Further, the need for patients and clinicians to speak to a wider audience about the positive contributions of psychiatry is an important means of reducing stigma and should be a priority (Singh, 2007[24]).
More interventions aimed at modifying medical students’ and health professionals are required (McParland et al., 2003[17]; Singh et al., 1998[25]; Baxter et al., 2001[2]; Lambert et al., 2006[12]). They argue that tackling the negative image of psychiatry should start in medical school and continue in junior doctor training, in order to retain psychiatrists at their jobs. In the interest of reducing stigma within the medical profession, it is recommended to address stigma in the psychiatric education process (Cutler et al., 2009[4]). This would provide medical students with a more accurate picture of psychiatry as a discipline and offer positive role models. Waggoner et al. (1983[30]) and Spiessl et al. (2000[26]) suggest an easily accessible psychiatric liaison service for family physicians in order to reduce delays in referrals. Moreover, they suggest practice-oriented seminars for family physicians, informing them not only about mental illness but also about psychiatric facilities, as well as continuing education in the context of the psychiatric liaison service.
Need for a ‘client-centric’ approach
Treatment can reduce consequences of stigma
Even though there has been much discussion on the issue of stigma, we believe that there is room for expansion on the concept. Specifically, that stigma should be seen at the level of the individual. From this vantage point we are confident that stigma can be effectively managed. Thus, we believe that consequences of stigma are preventable. We argue that in order to deal with the impact of stigma on an individual basis, it needs to be assessed during routine clinical examination, assessed for quantification in order to obtain measurable objective deliverables and examined if treatment can reduce stigma and its impact. Public health measures have so far been effective in initiating anti-stigma programmes, but only at a higher level; at the health care provider levels, they lack focus, and fail to recognise, assess and deal with stigma in systems of patient care. A patient-centric anti-stigma programme is needed without delay, which can successfully measure, quantify and bring evidence of success in this approach. Furthermore, it needs to be brought into routine clinical practice. New and innovative anti-stigma programmes are required that need to be clinically driven to see the change in life of an individual by removing potential risks.
Mentally ill patients need to play an active role in evaluations meant to inform decisions about their care and treatment. Dealing with stigma is a large public health priority that needs research to guide advocates to the best approaches. Community-based participatory research (CBPR) is the research agenda that includes consumers and other stakeholders to be full partners in all aspects of the evaluation programme.
The basic requirement for dealing with an individual's stigma perception/experience is its proper assessment for origin, and impact, of stigma, in both a qualitative and quantitative manner. We further argue that quantification would allow its regular assessment and offer more effective intervention for patients. It will also be helpful in identifying modifiable social factors to enhance quality of care plan for management in hospitals and communities. The objective of quantification is to facilitate the development of an approach to bring assessment of stigma in clinical work and formulate customised strategies to deal with stigma at a patient's level. It would be expected that the assessment of stigma would become a part of routine clinical assessment to identify barriers to outcome.
Public and community based intervention
The availability of effective treatment was thought to be the most important method of reducing stigma, which will certainly aid in the access of mental health care for patients globally. The WPA ‘Programme to Reduce Stigma and Discrimination Because of Schizophrenia’ established projects to fight stigma in 20 countries, using social-marketing techniques to enhance their effectiveness (Thompson, 1992[28]). First steps at each site were to establish an action committee and conduct a survey of perceived stigma. Based on survey results, the action committees selected a few homogeneous and accessible target groups, such as employers and criminal justice personnel. Messages and media were selected, tested, and refined. Guidelines were provided for setting up a consumer (service-user) speakers’ bureau and for establishing a media-watch organisation, which could lobby news and entertainment media to exclude negative portrayals of people with mental illness. Improvements in knowledge about mental illness were effected in high school students and criminal justice personnel. Positive changes in attitude towards people with mental illness were achieved with high school students, but were more difficult to achieve with police officers. Local anti-stigma projects can be effective in reducing stigma and are relatively inexpensive. The involvement of consumers is important in working with police officers.
Project organisers should be on the lookout for useful changes that can become permanent (Warner, 2008[31]). The results do not support the utility of a broad approach for an anti-stigma campaign, but rather suggest a more specific focus, such as perceived dangerousness (Thompson et al., 2002[28]). Results showed that higher global functioning, better readiness for action, and lower self-esteem decrement were significant predictors for better treatment participation. As for treatment attendance, results showed that individuals with lesser severity of psychiatric symptoms, and female participants, were more likely to have better attendance.
Measures to reduce stigma have been developed on large scales and on an individual level. Thompson's report (Thompson et al., 2002[28]) highlighted that people who live with mental illnesses are among the most stigmatised groups in society. In 1996, in recognition of the particularly harsh burden caused by stigma associated with schizophrenia, the WPA initiated a global anti-stigma programme, ‘Open-the-Doors′, with a broader mandate to reduce stigma and discrimination caused by mental disabilities in general (Sartorius et al., 2010[22]) . In order to evaluate the effectiveness of the WPA campaign “Open the Doors - against Stigma and Discrimination because of Schizophrenia”, five years upon completion of the campaign, a comparative study was performed to assess the possible changes in the general public's attitudes towards schizophrenia. The results of this study showed that 22.3 % of the population did not want to have any associations with the term “schizophrenia,” 81.3 % did not want to be further informed about the illness, and 64.1 % agreed with the statement that patients suffering from schizophrenia are dangerous; there was a significant increase in this category compared to the survey in 1998 (Grausgruber et al., 2009[9]).
Some research has shown that education videotapes can have some positive effects; mostly in terms of improvement in responsibility (people with mental illness are not to blame for their symptoms and disabilities). Watching videotaped contact with individuals with mental illness led to significant improvement in empathy, empowerment, coercion, and segregation.
Recommendation for dealing with stigma
The study we carried out in Mumbai (Shrivastava et al., 2011[23]) highlighted patients’ opinions to be the most important focus in dealing with stigma. It recommended investigating a number of issues: 1) relapse prevention (88%); 2) complete treatment (85%); 3) Educating the community (83%) 4) Rehabilitation (81%); 5) Early identification (77%); and 6) Social integration (65%).
The Mayo clinic (Mayo clinic staff, 2011[18]) has developed guidelines in dealing with stigma for patients and relatives. They suggest that dealing with stigma will result in more favourable outcomes. In short, they provide guidelines for reducing the impact of stigma and psychosis, paraphrased here:
Get treatment to provide relief from the symptoms that contribute to the stigmatising behaviours.
Don’t allow for stigma to create self-doubt and shame. Sometimes mistaken beliefs can interfere with a proper evaluation of the condition.
Don’t isolate yourself. This will only produce more stigma as symptoms would most likely be more poorly controlled.
Don’t equate yourself with your illness. You are not defined by your illness. You have an illness that requires management. This simple suggestion prevents a patient from addressing himself as a schizophrenic first and a person second.
Join support groups that can provide coping strategies for dealing with stigma as they may actively fight against stigma.
Get help at school. Talk to teachers, professors or administrators about the best approach and available resources. If a teacher doesn’t know about a student's disability, it can lead to discrimination, barriers to learning and poor grades.
And finally, speak out against stigma. Make the public aware of the injustices and misinformation about schizophrenia. This will help educate the public and in turn reduce stigma (Mayo clinic staff, 2011[18])
To combat stigma the highest priority should be given to efforts to unify the profession and to increase psychiatry's participation in organized medicine. This theme also urges psychiatrists to limit self-revelation and self-exploration in the media, to emphasize the broad range of knowledge and skills that makes them uniquely suited to perform evaluative and triage functions, and to halt the current practices of shunting whole classes of patients off to other disciplines for care, and of educating other disciplines in psychiatric techniques
Concluding Remarks [See also Figure 2: Flowchart of Paper]
Figure 2.
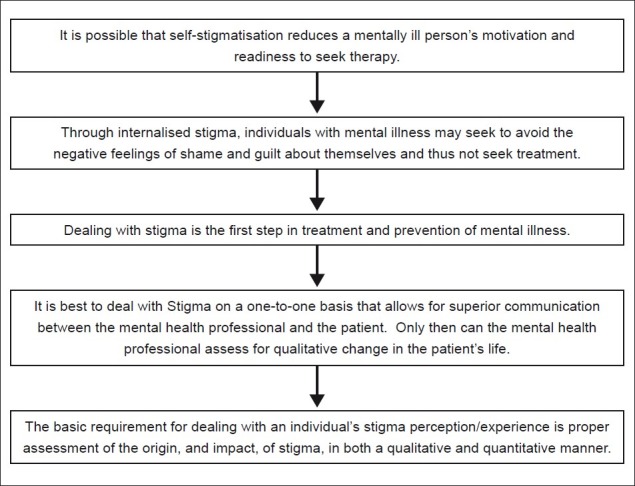
Flowchart of paper
Stigma leads to discrimination, isolates people, and finally, reduces opportunity and willingness to seek treatment. It is clearly known that stigma is a clinical risk, causes barrier to treatment and also results in non-compliance. The barriers are many. So far the approach has been only use of media, the medical profession and familial support (th Pandve et al., 2007[20]).
Stigma does not have to be so ubiquitous and prevalent in the lives of those with mental illnesses. We argue that, in order for this to change, there have to be targeted client-centered anti-stigma campaigns and programmes. It needs to be handled at the level of patients, which can directly improve their self-esteem [Figure 2].
Take home message
Stigma prevents people from seeking treatment, causes non-compliance and leads to poor outcome.
Stigma is recognized as a potential treatment barrier.
Stigma is a clinical risk.
Anti-stigma measures need to be client-centric.
Stigma needs to be assessed and treated in medical settings.
Questions that this Paper Raises
What are the clinical consequences of stigma?
How best can anti-stigma programmes be made client-centric?
How do we quantify impact of stigma for clinical usage?
Will a client-centric approach be feasible?
About the Author

Amresh Shrivastava, MD, MRCPsych, trained from KEM hospital in Mumbai and worked as consultant psychiatrist and as a Founding Director of PRERANA Charitable Trust for Suicide prevention in Mumbai, India He is Secretary of the Psychoendocrinology section “World Psychiatric Association” and works in the field of International mental health. Dr. Shrivastava's teaching and research interest are related to suicide behaviour and schizophrenia, particularly early psychosis, at-risk candidates and outcome measures. Currently he is the Physician Lead, Early Intervention program, Regional Mental Health Care, St.Thomas; Associate Professor of Psychiatry, University of Western Ontario; and Associate Scientist, Lawson Health Research Centre, London, Ontario, Canada
About the Author

Megan Johnston, MA, is currently a PhD Candidate in Psychology at the University of Toronto in Toronto, Ontario, Canada. Her primary research interests involve parental and socialisation influences on moral development and antisocial and prosocial behaviour in adolescence. She is also affiliated with Regional Mental Health Care – St. Thomas, Ontario, Canada where her research focuses on the social and clinical outcomes of schizophrenia and suicide risk assessment and prevention
About the Author

Yves Bureau, PhD, earned an undergraduate degree in neuroscience (1991), a MSc in biology (1994) and a PhD in the area of experimental psychology (2001). He completed two post- doctoral fellowships, one at Merck Frosst Canada and Company in Kirkland Québec in Neuropharmacology (2002), and the other at the Lawson Health Research Institute in London, Ontario, in Neuroimaging (2004). He is presently an adjunct professor in the psychology and medical biophysics departments at The University of Western Ontario. He is also an associate scientist at the Lawson Health Research Institute and the director of Inferential Statistics for the Imaging division. Currently his research interests are in the areas of behavioural neuroscience and psychiatry
Footnotes
Conflict of interest: None declared
Declaration
This is our original unpublished work, not under consideration for publication elsewhere.
CITATION: Shrivastava A, Johnston M, Bureau Y. Stigma of Mental Illness-2: Non-compliance and Intervention. Mens Sana Monogr 2012; 10: 85-97.
References
- 1.Battaglia J, Coverdale JH, Bushong CP. Evaluation of a mental illness awareness week program in public schools. Am J Psychiatry. 1990;147:324–9. doi: 10.1176/ajp.147.3.324. PMID: 2309950. [DOI] [PubMed] [Google Scholar]
- 2.Baxter H, Singh SP, Standen P, Braganza D. The attitudes of ‘tomorrow's doctors’ towards mental illness and psychiatry: Changes during the final undergraduate year. Med Educ. 2001;35:381–3. doi: 10.1046/j.1365-2923.2001.00902.x. PMID: 11319003. [DOI] [PubMed] [Google Scholar]
- 3.Corrigan PW, Watson AC. At issue: Stop the stigma: call mental illness a brain disease. Schizophr Bull. 2004;30:477–9. doi: 10.1093/oxfordjournals.schbul.a007095. PMID: 15631240. [DOI] [PubMed] [Google Scholar]
- 4.Cutler JL, Harding KJ, Mozian SA, Wright LL, Pica AG, Masters SR, et al. Discrediting the notion “working with ‘crazies’ will make you ‘crazy’”: Addressing stigma and enhancing empathy in medical student education. Adv Health Sci Educ Theory Pract. 2009;14:487–502. doi: 10.1007/s10459-008-9132-4. PMID: 18766453. [DOI] [PubMed] [Google Scholar]
- 5.Fresán A, Robles-García R, de Benito L, Saracco R, Escamilla R. Development and psychometric properties of a brief instrument to measure the stigma of aggressiveness in schizophrenia. Actas Esp Psiquiatr. 2010;38:340–4. PMID: 21188673. [PubMed] [Google Scholar]
- 6.Fung KM, Tsang HW, Corrigan PW. Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. th Psychiatr Rehabil J. 2008;32:95–104. doi: 10.2975/32.2.2008.95.104. PMID: 18840563. [DOI] [PubMed] [Google Scholar]
- 7.Fung KM, Tsang HW, Corrigan PW, Lam CS, Cheung WM. Measuring self-stigma of mental illness in China and its implications for recovery. Int J Soc Psychiatry. 2007;53:408–18. doi: 10.1177/0020764007078342. PMID: 18018663. [DOI] [PubMed] [Google Scholar]
- 8.Goff DC, Hill M, Freudenreich O. Strategies for improving treatment adherence in schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2010;71:20–6. doi: 10.4088/JCP.9096su1cc.04. PMID: 21190649. [DOI] [PubMed] [Google Scholar]
- 9.Grausgruber A, Schöny W, Grausgruber-Berner R, Koren G, Apor BF, Wancata J, et al. Schizophrenia has many faces-evaluation of the Austrian Anti-Stigma-Campaign 2000-2002. Psychiatr Prax. 2009;36:327–33. doi: 10.1055/s-0029-1220386. PMID: 19724998. [DOI] [PubMed] [Google Scholar]
- 10.Kelly BD. Structural violence and schizophrenia. Soc Sc Med. 2005;61:721–30. doi: 10.1016/j.socscimed.2004.12.020. PMID: 15899329. [DOI] [PubMed] [Google Scholar]
- 11.Kitchener BA, Jorm AF. Mental health first aid training in a workplace setting: A randomized controlled trial. BMC Psychiatry. 2004;15:23. doi: 10.1186/1471-244X-4-23. PMID: 15310395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lambert TW, Turner G, Fazel S, Goldacre MJ. Reasons why some UK medical graduates who initially choose psychiatry do not pursue it as a long-term career. Psychol Med. 2006;36:679–84. doi: 10.1017/S0033291705007038. PMID: 16426488. [DOI] [PubMed] [Google Scholar]
- 13.Lysaker PH, Roe D, Yanos PT. Toward understanding the insight paradox: Internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophr Bull. 2007;33:192–9. doi: 10.1093/schbul/sbl016. PMID: 16894025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lysaker PH, Buck KD, Taylor AC, Roe D. Associations of metacognition and internalized stigma with quantitative assessments of self-experience in narratives of schizophrenia. Psychiatry Res. 2007;157:31–8. doi: 10.1016/j.psychres.2007.04.023. PMID: 18023881. [DOI] [PubMed] [Google Scholar]
- 15.Lysaker PH, Tsai J, Yanos P, Roe D. Associations of multiple domains of self-esteem with four dimensions of stigma in schizophrenia. Schizophr Res. 2008;98:194–200. doi: 10.1016/j.schres.2007.09.035. PMID: 18029145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lysaker PH, Ringer JM, Davis LW. Associations of social anxiety and self-esteem across six months for persons living with schizophrenia spectrum disorders. Psychiatr Rehabil J. 2008;32:132–4. doi: 10.2975/32.2.2008.132.134. PMID: 18840569. [DOI] [PubMed] [Google Scholar]
- 17.McParland M, Noble LM, Livingston G, McManus C. The effect of a psychiatric attachment on students’ attitudes to and intention to pursue psychiatry as a career. Med Educ. 2003;37:447–54. doi: 10.1046/j.1365-2923.2003.01491.x. PMID: 12709187. [DOI] [PubMed] [Google Scholar]
- 18.Mayo clinic staff. [Accessed 31 Oct 2011];Mental health: Overcoming the stigma of mental illness. 2011 Available from http://www.mayoclinic.com/health/mental-health/MH00076 . [Google Scholar]
- 19.Pandya A, Bresee C, Duckworth K, Gay K, Fitzpatrick M. Perceived impact of the disclosure of a schizophrenia diagnosis. Community Ment Health J. 2011;47:613–21. doi: 10.1007/s10597-010-9341-1. PMID: 20703941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pandve H, Banerjee A. Do popular media such as movies aggravate the stigma of mental disorders? Indian J Psychiatry. 2007;49:144. doi: 10.4103/0019-5545.33267. PMID: 20711402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patch PC, Arrigo BA. Police officer attitudes and use of discretion in situations involving the mentally ill: The need to narrow the focus. Int J Law Psychiatry. 1999;22:23–35. doi: 10.1016/s0160-2527(98)00014-4. PMID: 10086288. [DOI] [PubMed] [Google Scholar]
- 22.Sartorius N, Gaebel W, Cleveland HR, Stuart H, Akiyama T, Arboleda-Flórez J, et al. WPA guidance on how to combat stigmatization of psychiatry and psychiatrists. World Psychiatry. 2010;9:131–44. doi: 10.1002/j.2051-5545.2010.tb00296.x. PMID: 20975855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shrivastava A, Johnston ME, Thakar M, Shrivastava S, Sarkhel G, Sunita I, et al. Origin and impact of stigma and discrimination in schizophrenia - patients’ perception: Mumbai study. Stigma Res Action. 2011;1:67–72. [Google Scholar]
- 24.Singh AR. The task before psychiatry today. Indian J Psychiatry. 2007;49:60–5. doi: 10.4103/0019-5545.31521. PMID: 20640068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh SP, Baxter H, Standen P, Duggan C. Changing the attitudes of ‘tomorrow's doctors’ towards mental illness and psychiatry: A comparison of two teaching methods. Med Educ. 1998;32:115–20. doi: 10.1046/j.1365-2923.1998.00162.x. PMID: 9743760. [DOI] [PubMed] [Google Scholar]
- 26.Spiessl H, Cording C. Collaboration of the general practitioner and the psychiatrist with the psychiatric hospital: A literature review. Fortschr Neurol Psychiatr. 2000;68:206–15. doi: 10.1055/s-2000-11633. PMID: 10858945. [DOI] [PubMed] [Google Scholar]
- 27.Stuart H. Media portrayal of mental illness and its treatments: What effect does it have on people with mental illness? CNS Drugs. 2006;20:99–106. doi: 10.2165/00023210-200620020-00002. PMID: 16478286. [DOI] [PubMed] [Google Scholar]
- 28.Thompson AH, Stuart H, Bland RC, Arboleda-Florez J, Warner R, Dickson RA, et al. Attitudes about schizophrenia from the pilot site of the WPA worldwide campaign against the stigma of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2002;37:475–82. doi: 10.1007/s00127-002-0583-2. PMID: 12242626. [DOI] [PubMed] [Google Scholar]
- 29.Tsang HW, Fung KM, Chung RC. Self-stigma and stages of change as predictors of treatment adherence of individuals with schizophrenia. Psychiatry Res. 2010;180:10–5. doi: 10.1016/j.psychres.2009.09.001. PMID: 20493552. [DOI] [PubMed] [Google Scholar]
- 30.Waggoner RW, Waggoner RW., Jr Psychiatry's image, issues, and responsibility. Psychiatr Hosp. 1983;14:34–8. PMID: 10258440. [PubMed] [Google Scholar]
- 31.Warner R. Implementing local projects to reduce the stigma of mental illness. Epidemiol Psichiatr Soc. 2008;17:20–5. PMID: 18444453. [PubMed] [Google Scholar]
- 32.Wolff G, Pathare S, Craig T, Leff J. Public education for community care: A new approach. Br J Psychiatry. 1996;168:441–7. doi: 10.1192/bjp.168.4.441. PMID: 8730940. [DOI] [PubMed] [Google Scholar]