Abstract
Rhino-orbito-cerebral mucormycosis is a fungal infection that can be fatal especially in immunocompromised patients. It is extremely rare in immunocompetent individuals. We describe here an immunocompetent patient who survived rhino-orbito-cerebral mucormycosis due to Saksenaea vasiformis, and provide a literature review of this rare entity.
Keywords: Immunocompetent, Saksenaea vasiformis, Rhino-Orbito-Cerebral Mucormycosis
INTRODUCTION
Mucormycosis is a rare but aggressive opportunistic fungal infection that is commonly caused by members of the family Mucoraceae that include Rhizopus, Rhizomucor, Mucor and Absidia. Mucormycosis can cause severe, sometimes fatal disease in susceptible individuals with uncontrolled diabetic ketoacidosis, neutropenia, chronic glucocorticoid use, hematological malignancy, chronic malnutrition and burn patients.1–3
Rhino-orbito-cerebral mucormycosis (ROCM) is an uncommon infection in immunocompetent hosts. ROCM invades vessels, soft tissue, nerves, bone and cartilage producing tissue infarction and ultimately leading to tissue necrosis and vessel thrombosis.4 We present a case of an immunocompetent patient who survived ROCM due to Saksenaea vasiformis, and review the literature of this fatal condition.
CASE REPORT
A 40-year-old healthy male presented with painful swelling in the left eye for two weeks. Other symptoms included blurring of vision and diplopia. There was no history of eye trauma, dental carries, recent surgery, sinusitis or skin infection. The visual acuity was 6/60 in the left eye with 2-mm axial proptosis, with conjunctival congestion and limited ocular motility. The pupils were reactive bilaterally, with no evidence of a relative afferent pupillary defect in either eye.
The patient was diagnosed with orbital cellulitis in the left eye. However, the primary cause was undetermined. Broad spectrum antibiotic therapy was initiated that included intravenous cloxacillin 500 mg every 6 h, cefuroxime 750 mg every 8 h and metronidazole 500 mg every 8 h. There was minimal clinical improvement with the above regime after one week of hospitalization. Thus, the patient elected to discharge himself against the medical advice.
The patient presented two weeks later to a tertiary hospital with severe pain and persistent purulent discharge and no light perception in the left eye. The left globe perforated with extensive regions of necrotic tissue. Both upper and lower lids were swollen with discharging fistula proximal to the lateral canthus [Figure 1]. The right eye was normal with 6/6 visual acuity. General examination revealed an alert, afebrile and well-oriented patient with no neurologic deficit.
Figure 1.

Complete loss of globe structure and fistula formation on presentation
Plasma glucose, blood urea, full blood count and liver function test were normal. HIV serology was non-reactive. Computed tomography (CT) of the brain and orbit showed destruction of the left eye, with an ill-defined mass and ring enhancement involving left pterygopalatine, inferotemporal fossa and adjacent bony destruction. It extended posteriorly to the orbital apex, causing a widening of the optic nerve canal and the superior orbital fissure. The cavernous sinus showed signs of thrombosis and presence of areas of infiltrate at the left maxillary, frontal and sphenoidal sinuses [Figure 2].
Figure 2.
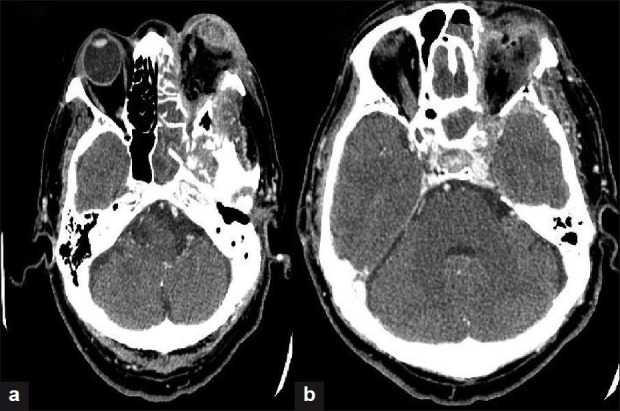
(a) CT scan of the orbit showing proptosis and distortion of the left globe (b) CT scan of brain (post contrast) showing an enhancement of the cavernous sinus suggestive of thrombosis
A presumptive clinical diagnosis of ROCM was made. Intravenous amphotericin B 1.0 mg/kg/day was initiated after a test dose. The patient had no significant side effects due to intravenous Amphotericin B. The patient consented to exenteration of left eye and extensive sinus debridement surgery. Histopathology revealed broad, aseptate, long and right angled branching hyphae consistent with mucormycosis [Figure 3]. A tissue culture grew Saksenaea vasiformis. The intravenous Amphotericin B stopped after 4 weeks of therapy and he was discharged with instructions to instill topical Amphotericin B for another four weeks.
Figure 3.
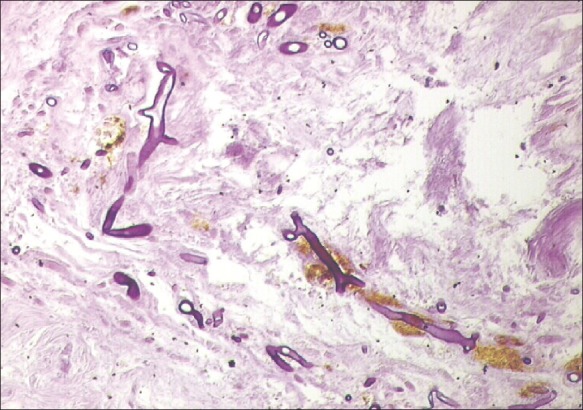
Photomicrograph showing aseptate, long broad, slender right angled branching hyphae, which is pathognomonic of mucormycosis
Postoperatively, the patient refused to repeat imaging and implantation of eye prosthesis due to poor family support and financial constraints. To date, the patient has been followed up for two and a half years with recurrence of ROCM.
DISCUSSION
ROCM is usually associated with a fatal outcome especially in immunocompromised patients. For the last decade, ROCM has been increasingly reported in healthy individuals. We reviewed 11 cases of ROCM in immunocompetent hosts published in PubMed from 2000 to 2011. Table 1 summarizes age, gender, presentations, risk factor, causative organism and final outcome.
Table 1.
Summary of previous literature on Rhino-orbito-cerebral mucormycosis in immunocompetent patients published in PubMed from 2000 to 2011
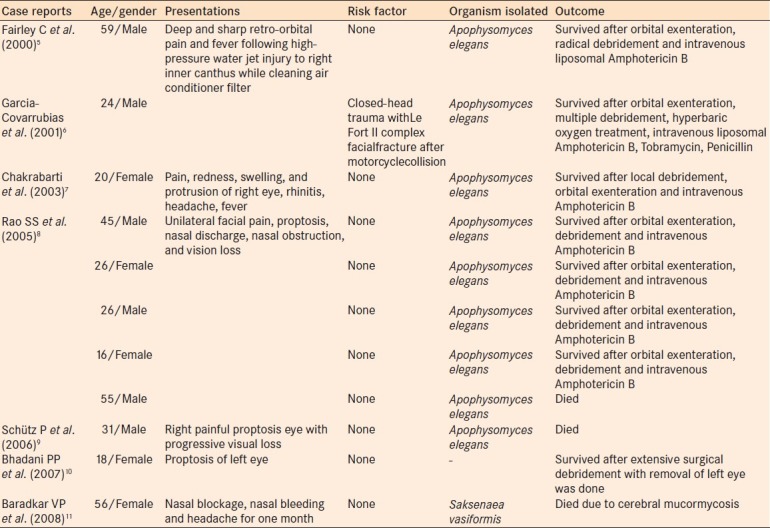
The presenting age ranged between 16 and 59 years and both genders were equally affected. Nine out of 11 published cases were due to Apophysomyces elegans.5–9 There was only one reported case of ROCM caused by Saksenaea vasiformis.11 Apophysomyces elegans is an emerging pathogen that causes ROCM via inhalation. Whereas, Saksenaea vasiformis is a soil saprophytic fungus and the only species in the genus Saksenaea.
In the previously reported cases, 7 immunocompetent patients who survived were infected by Apophysomyces elegans.5–8 Among three patients who died, two were infected by Apophysomyces elegans and one with Saksenaea vasiformis.8,9,11 Two of these three patients were above 50 years of age and died due to extensive brain involvement and severe cerebral vascular insult.8,11 This finding is similar to the findings of Hargrove et al.12 that patients older than 46 years with concurrent frontal sinus involvement and fever were less likely to survive orbital mucormycosis.
Our patient was very fortunate to survive this fatal condition despite delayed diagnosis and treatment. This is likely due to his relatively young age and the lack of a pre-existing chronic medical illness. To the best of our knowledge, this is the first reported case of an immunocompetent patient with ROCM due to Saksenaea vasiformis who survived.
Our patient and other immunocompetent patients who survived ROCM were treated with a combination of systemic Amphotericin B, orbital exenteration and adjacent tissue debridement.5–8 This is consistent with Roden et al.,1 who reported a survival rate of 70% for cases treated with antifungal and surgery. In contrast, only 61% of cases treated with amphotericin B deoxycholate only, 57% of cases that underwent only surgery and only 3% of untreated patients survived.1
In conclusion, diagnosis of ROCM in immunocompetent patients is always misleading and possibly causes delay in treatment. It is essential to alert the managing ophthalmologist of the emergence of this rare disease among healthy individuals.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis. 2005;41:634–53. doi: 10.1086/432579. [DOI] [PubMed] [Google Scholar]
- 2.Chakrabarti A, Das A, Sharma A, Panda N, Das S, Gupta KL, et al. Ten years’ experience in zygomycosis at a tertiary care centre in India. Clin Infect Dis. 2001;42:261–6. doi: 10.1053/jinf.2001.0831. [DOI] [PubMed] [Google Scholar]
- 3.Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000;13:236–301. doi: 10.1128/cmr.13.2.236-301.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sugar AM. Mucormycosis. Clin Infect Dis. 1992;14:5126–9. [Google Scholar]
- 5.Fairley C, Sullivan TJ, Bartley P, Allworth T, Lewandoski R. Survival after rhino-orbital-cerebral mucormycosis in an immunocompetent patient. Ophthalmology. 2000;107:555–8. doi: 10.1016/s0161-6420(99)00142-6. [DOI] [PubMed] [Google Scholar]
- 6.Garcia-Covarrubias L, Bartlett R, Barratt DM, Wassermann RJ. Rhino-orbitocerebral mucormycosis attributable to Apophysomyceselegans in an immunocompetent individual: Case report and review of the literature. J Trauma. 2001;50:353–7. doi: 10.1097/00005373-200102000-00027. [DOI] [PubMed] [Google Scholar]
- 7.Chakrabarti A, Ghosh A, Prasad GS, David JK, Gupta S, Das A, et al. Apophysomyces elegans: An emerging zygomycete in India. J Clin Microbiol. 2003;41:783–8. doi: 10.1128/JCM.41.2.783-788.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rao SS, Naresh KP, Pragache G, Chakrabarti A, Saravanan K. Sinoorbital mucormycosis due to Apophysomyces elegans in immunocompetent individuals-an increasing trend. Am J Otolaryngol. 2006;27:366–9. doi: 10.1016/j.amjoto.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Schütz P, Behbehani JH, Khan ZU, Ahmad S, Kazem MA, Dhar R, et al. Fatal rhino-orbito-cerebral zygomycosis caused by Apophysomyces elegans in a healthy patient. J Maxillofac Surg. 2006;64:1795–802. doi: 10.1016/j.joms.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 10.Bhadani PP, Bhadani UK, Thapliyal N, Sen R. A rare presentation of invasive rhino-orbital mucormycosis in an immunocompetent young girl: A case report. Indian J Pathol Microbiol. 2007;50:785–6. [PubMed] [Google Scholar]
- 11.Baradkar VP, Mathur M, Taklikar S, Rathi M, Kumar S. Fatal rhino-orbito-cerebral infection caused by Saksenaea vasiformis in an immunocompetent individual: First case report from India. Indian J Med Microbiol. 2008;26:385–7. doi: 10.4103/0255-0857.43572. [DOI] [PubMed] [Google Scholar]
- 12.Hargrove RN, Wesley RE, Klippenstein KA, Fleming JC, Haik BG. Indication for orbital exenteration in mucormycosis. Ophthal Plast Reconstr Surg. 2006;22:286–91. doi: 10.1097/01.iop.0000225418.50441.ee. [DOI] [PubMed] [Google Scholar]


