Abstract
Local anesthesia forms the major part of pain-control techniques in dentistry. The prevention and elimination of pain during dental treatment has benefited patients, their doctors and dental hygienists, enabling the dental profession to make tremendous therapeutic advances that would otherwise have been impossible. Introduced in the late 1940s, the amide local anesthetics represent the most used drugs in dentistry. Local anesthetics also represent the safest and most effective drugs in all of medicine for the prevention and management of pain. They are also accompanied by various adverse effects which should be well known and be able to be controlled by the clinician. The article reviews the types of agents used as local anesthetics and their effects on the human body.
Keywords: Anesthesia, anesthetics, dental, local/adverse effects, pharmacology, vasoconstrictor agent
INTRODUCTION
Local anesthetics are the most commonly used drugs in dentistry. Pain and dentistry are often synonymous in the minds of patients, especially those with poor dentition due to multiple extractions, periodontal disease requiring surgery or symptomatic teeth requiring endodontic therapy. Dental practitioners, before the procedure, identify a good anesthetic as one that allows them to focus solely on operative procedures without distractions from pain-induced patient movements. Research has shown that the fear of pain associated with dentistry is closely associated with intraoral administration of local anesthetics, which is the most common method for blocking pain during dental procedures. This is considered aversive due to the pain associated with the injection and the perceived threat of needle puncture prior to the injection.[1] Another survey finding was that those individuals who reported themselves as highly fearful of dentistry were worried about receiving oral injections and demonstrated an association between high dental anxieties and missed or delayed appointments.[2] This article provides a brief overview of local anesthetics to reinforce clinician's knowledge of these agents.
History of local anesthesia
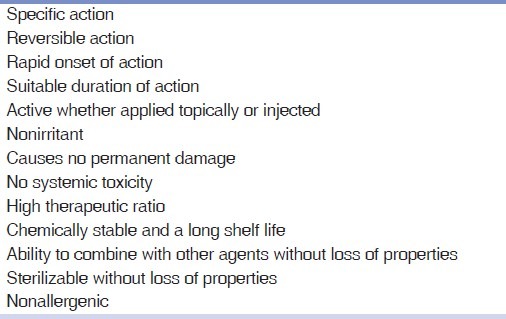
The history of local anesthesia started in 1859, when cocaine was isolated by Niemann. In 1884, the opthalmologist Koller was the first, who used cocaine for topical anesthesia in ophthalmological surgery. In 1884, regional anesthesia in the oral cavity was first performed by the surgeon Halsted, when he removed a wisdom tooth without pain. However, a number of adverse effects were observed with the clinical use of cocaine. Thus, other local anesthetic agents had to be developed. In 1905, Einhorn reported the synthesis of procaine, which was the first ester-type local anesthetic agent. Procaine was the most commonly used local anesthetic for more than four decades. In 1943, Löfgren synthesized lidocaine, which was the first modern local anesthetic agent, since it is an amide-derivate of diethylamino acetic acid. Lidocaine was marketed in 1948 and is currently the most commonly used local anesthetic in dentistry worldwide, though other amide local anesthetics were introduced into clinical use such as; mepivacaine 1957, prilocaine 1960 and bupivacaine 1963. In 1969, articaine was synthesized by the chemist Muschaweck and was approved in 1975 as a local anesthetic in Germany. The use of reversible local anesthetic chemical agents is the most common method to achieve pain control in dental practice.[3] Some ideal properties of local anesthetics are mentioned in Table 1.
Table 1.
Ideal properties of local anesthetics
Pharmacology
Local anesthesia is induced when propagation of action potentials is prevented, such that sensation cannot be transmitted from the source of stimulation, such as tooth or the periodontium, to the brain. Local anesthetics work by blocking the entry of sodium ions into their channels, thereby preventing the transient increase in permeability of the nerve membrane to sodium that is required for an action potential to occur. Structurally, local anesthetics have specific fundamental features in common. These include a lipophilic group, joined by an amide or ester linkage to a carbon chain which, in turn, is joined to a hydrophilic group. Local anesthetics are classified by these amide or ester linkages.
Blood levels
The blood level of local anesthetic agent following injection is a function of both rate of absorption from the site of injection and uptake into the systemic circulation, and its removal through distribution from the vascular compartment into tissue compartments, and elimination via metabolic and excretory pathways. If toxic levels are reached or exceeded, local anesthetics may cause toxic signs and symptoms, which are mainly referable to the central nervous system and to the cardiac vascular system. Pharmacokinetic parameters, including maximum serum levels, time of maximum serum levels and elimination half time, are important to estimate the risk of systemic intoxication following injection and to recommend maximal dose in single and repeated injection. The absorption and subsequent blood level of local anesthetic agents are related to the total dose of drug administered. For most agents, there is a linear relationship between the amount of drug administered and the resultant peak of anesthetic blood level. The peak of anesthetic blood level does not appear to be related to either the concentration or volume of the local anesthetic solution employed. The vasocontrictor (e.g. 1:200,000 epinephrine) significantly reduces the peak of blood levels of lidocaine and mepivacaine, while the peak levels of bupivacaine and prilocaine appear not to be influenced by the addition of a vasoconstrictor substance.
Failure of anesthesia
Failure of local anesthetics to achieve profound analgesia may be related to inaccurate anatomic placement of local anesthetic solution, use of inadequate amount of anesthetic solution, allowing insufficient time for the solution to diffuse to be effective, injection of solution into inflamed or infected tissues, and finally use of an outdated or improperly stored anesthetic solution.
It is recommended that a local anesthetic not be injected into an infected tissue because of the risk of spreading the infection and the increased probability of achieving less than effective anesthetic results owing to the low pH within the infected tissue maintaining the ionized, non lipid-soluble state to the anesthetic.
Adverse reactions
Complications of local anesthetic administration include both local effects and systemic effects.[4]
Allergic reactions and toxicity
Patient reports of allergic reactions to local anesthetics are fairly common, but investigation shows that most of these are of psychogenic origin.[5,6] True allergy to an amide is exceedingly rare, whereas the ester procaine is somewhat more allergenic. A patient may be allergic to other compounds in the anesthetic cartridge. For example, methylparabens are preservatives necessary for multidose vials and were present in dental cartridges in the past. They are no longer included as dental cartridges are single-use items. Allergy to para-aminobenzoic acid would rule out use of esters and methylparabens. It may be best to avoid a vasoconstrictor if there is a true documented allergy to sulfites, as metabisulfite is added as an antioxidant whenever vasoconstrictor is present. Toxic complications as a result of an overdose of local anesthetic solution, resulting in dangerously high concentrations in the brain, are usually produced only by rapid injection directly into a blood vessel.[7] It should be remembered that for fit adults the recommended maximum safe dose of 2% lignocaine in 1:80 000 adrenaline is four-and-a-half 2 or 2.2 ml cartridges (180 to 198 mg lignocaine); for 3% prilocaine, and felypressin 0.03 i.u./ml, the maximum safe dose is 400 mg (six 2 ml cartridges).[8] Some studies have shown that intravascular injection may occur in between 3 and 12% of cases.[9] To avoid accidents with potentially hazardous results, routine aspiration is essential. As the anesthetic solutions of the amide type (e.g., lignocaine and prilocaine) rely on the liver for hydrolysis and metabolism before elimination, any patient with seriously impaired liver function is in danger of inadequate elimination of the solution: A normal volume of anesthetic will become potentially toxic in such people. The final route for elimination of the metabolized anesthetic solution is excretion in the urine and so any patient with impaired renal function will also be unable to eliminate these products and be predisposed to toxic accumulation.
Psychogenic reactions
Anxiety-induced events are by far the most common adverse reaction associated with local anesthetics in dentistry. These may manifest in numerous ways, the most common of which is syncope. In addition, they may present with a wide variety of symptoms, including hyperventilation, nausea, vomiting and alterations in heart rate or blood pressure. Psychogenic reactions are often misdiagnosed as allergic reactions and may also mimic them, with signs such as urticaria, edema and bronchospasm.
Methemoglobinemia
This uncommon adverse reaction is associated most notably with prilocaine but may also occur with articaine or the topical anesthetic benzocaine. Methemoglobinemia is induced by an excess of the metabolites of these drugs and manifests as a cyanotic appearance that does not respond to the administration of 100% oxygen. Cyanosis becomes apparent when methemoglobin levels are low, but symptoms of nausea, sedation, seizures and even may result in coma when levels are very high.[10] Prilocaine, articaine and benzocaine are best avoided in patients with congenital methemoglobinemia.
Facial nerve palsy
The most common neurological complication following an inferior alveolar nerve block is a facial nerve palsy.[11–16] Patients with a peripheral facial nerve palsy exhibit the following signs:
Generalized weakness of the ipsilateral side of the face, inability to close the eyelids, obliteration of the nasolabial fold, drooping of the corner of the mouth and deviation of the mouth to the unaffected side.
Facial nerve palsy following inferior alveolar nerve block may appear immediately or be delayed. The immediate (transient) palsy generally recovers within 3 h of administration of the local anesthetic. It is probably due to anesthesia of the facial nerve trunk as a result of an abnormal nerve anatomy such as passage of the nerve along the deep surface of the parotid gland. Alternatively, it may be caused by a congenital abnormality such as the gland failing to envelop the nerve and its divisions, thus increasing its chances of direct exposure to local anesthetic solution. Delayed-onset facial palsy occurs after several hours (and in some cases many days) after the administration of the anesthetic. Some hypotheses have been put forward to explain this:
The anesthetic solution or its breakdown products stimulate the sympathetic plexus associated with the external carotid artery. From the external carotid artery, fibers of this plexus continue in association with the stylomastoid artery as it passes into the parotid gland. The stimulation of the stylomastoid sympathetic plexus causes a delayed reflex spasm of the vasa nervorum of the facial nerve, leading to ischaemic neuritis and secondary edema. The origin of these sympathetic fibers is in the superior cervical ganglion which gives rise to lateral, medial and anterior branches. Of these, it is the anterior branches that pass onto the common and external carotid arteries to form plexuses that accompany the blood vessels.[11]
The mechanical action of the needle itself may lead to stimulation of the sympathetic plexus associated with the external carotid artery.[13]
Paresthesia
Prolonged anesthesia or paresthesia of the tongue or lip are known risks of surgical procedures such as extractions but may also occur following nonsurgical dentistry. Most of these reactions are transient and resolve within 8 weeks, but they may become permanent. Articaine and prilocaine were reported as more likely than other anesthetics to be associated with paresthesia, a difference that was statistically significant when their distribution of use was taken into account.[17] Other causes of persistent paraesthesia include direct nerve damage following injection of local anesthetic contaminated with sterilizing agents or the development of hemorrhage or hematoma around the nerve sheath leading to necrosis of the neural tissue. Direct inferior nerve trauma feels like an electric shock, sometimes causing the patient to suddenly jerk their head. The practitioner should cease the injection immediately if this occurs.[18]
Hematoma
The damage of a blood vessel by the tip of a needle may lead to bleeding into the tissues, resulting in the formation of a hematoma. Significant bleeding may produce swelling, act as an irritant to the tissues, and causes pain and trismus. Theoretically, the localized collection of blood becomes an ideal culture medium for bacteria, although infection of a hematoma is unusual.
Total body hemiparesis
Inadvertent intravascular injection of local anesthetic with subsequent retrograde internal movement in branches of the internal carotid artery has been suggested as a mechanism for a reported case of total body hemiparesis 15 min following inferior dental nerve block. This comprised ptosis, occipital and neck stiffness, anesthesia of the right side of the face with dysphasia, and led to complete aphasia and a right hemiparesis. The effects lasted for approximately 45 min and were attributed to excess pressure created during the administration of the injection leading to a retrograde flow into the internal carotid artery.[19]
Malignant hyperthermia
Malignant hyperthermia can occur when patients with genetic susceptibility to this condition are exposed to inhalational general anesthetics or succinylcholine, but not to local anesthetics. Previous recommendations, now known to be wrong, precluded the use of specific local anesthetics in these patients. Today it is well accepted that all local anesthetics are safe for patients who are susceptible to malignant hyperthermia.
Adverse effects of epinephrine
Depending on the dose, sympathomimetic amines can evoke a variety of systemic reactions. The major systemic effects of injected sympathicomimetic amines involve the cardiovascular system. Cardiovascular responses of epinephrine often include tachycardia, mild hypertension, and occasionally premature ventricular contractions. The majority of adverse reactions are mild and short of duration.
Horner's syndrome
A rare complication following an inferior dental nerve block, reported by Campbell et al.,[20] is the development of Horner's syndrome. This arose due to penetration of the local anesthetic through the lateral pharyngeal and prevertebral spaces, causing blockade of the stellate ganglion.
The features of the syndrome include: Flushing of the face on the same side, ptosis of the eyelids, vasodilatation of the conjunctiva; pupillary constriction and (occasionally) a rash over the neck, face, shoulder and arm of the ipsilateral side.
Paralysis of combinations of cranial nerves
Use of techniques such as Gow-Gates may result in local anesthetic, which is deposited in a superior position, gaining access to the cavernous sinus following inadvertent intravenous injection. Consequently, reports have been made of transient paralysis of combined cranial nerves III, IV and VI, leading to immobility of the ipsilateral eyeball, diplopia, ptosis of the eyelid and—in contrast to Horner's syndrome—a dilated pupil.
Careful aspiration and direction of the needle to an area with fewer large-bore blood vessels such as the lateral aspect of the condyle are recommended to avoid this complication.[21]
Temporary blindness
Temporary blindness has been reported following posterior alveolar nerve block due to a large quantity of local anesthetic under great pressure diffusing through the inferior orbital fissure and coming into contact with the optic nerve.[22]
Sudden unilateral deafness
There has also been a report of sudden unilateral deafness following dental procedures involving inferior dental nerve blocks. The suggested explanation implies that the venous systems within the mandibular region provide access for the anesthetic to the middle ear and that this, due to the added vasoconstrictor, results in localized vasospasm of the cochlear division of the internal auditory artery, leading to dysfunction of the cochlear nerve.[23]
Cardiovascular disease patients
The patients with ischemic heart disease (angina pectoris, previous myocardial infarction) or who have had previous cardiac surgery or circulatory dysfunction such as cardiac failure, show higher plasma levels of lidocaine when compared with healthy subjects given the same dose. Therefore, it is recommended that the maximum safe dose be halved in such patients.[24] Low plasma potassium levels and acidosis also potentiate adverse effects of local anesthetics on the myocardium.[4] The role of the dental practitioner is to maintain an airway, ensure the patient is breathing and monitor cardiac activity. Whilst performing these primary measures the practitioner should summon help and contact the nearest casualty department. Placing the patient supine and administering oxygen will allow monitoring of vital signs (pulse, respiration and blood pressure). Convulsions, which occur in some cases, may need to be treated with a slow (over 2 min) intravenous infusion of 10 mg diazepam. The rectal route is an alternative when intravenous access is difficult.
Endocarditis risk
Injections such as the intraligamentary injection can force bacteria into the systemic circulation and cause bacterial endocarditis.
Local anesthetics during pregnancy
All local anesthetics cross the placenta to some degree.[25–27] Highest concentrations in the fetal circulation follow injection of prilocaine, and the lowest follow bupivacaine, with lidocaine in between.[28,29] Felypressin, which is a derivative of vasopressin and is related to oxytocin, has the potential to cause uterine contractions. Although this is a highly unlikely effect at the low dose of felypressin used in local anesthetics, it is best avoided during pregnancy. Lidocaine with epinephrine is commonly used for pregnant dental patients. Although high-dose vasoconstrictors used to manage significant hypotension may be a concern for pregnant patients, the doses of epinephrine used in local anesthetic formulations for dentistry are so low that they are unlikely to significantly affect uterine blood flow. The benefits of epinephrine or levonordefrin at the concentrations found in dental anesthetic cartridges justify their use.
Local anesthetics in children
Available data suggest that the adverse reactions in pediatric patients are commonly caused by inadequate dosage reduction.[30] Maximum recommended doses of local anesthetics is based upon the weight of the child, usually expressed as milligrams per kilogram of body weight. For very obese children, the maximum dose should be calculated on the basis of lean body weight or ideal weight, not the true body weight. The specific number of milligrams per kilogram used for calculating the maximum recommended dose differs among the various local anesthetics. Given the concerns regarding toxicity, selection of a low concentration solution appears prudent. Thus, 2% lidocaine with epinephrine 1:100,000 may be the ideal local anesthetic for a child. Bupivacaine is best avoided in children because of its long duration of soft-tissue anesthesia. There should be no concerns regarding prolonged duration of action due to vasoconstrictor, as it has been shown that soft-tissue anesthesia does not differ significantly between 2% lidocaine with epinephrine 1:100,000 and 3% mepivacaine plain or 4% prilocaine plain.[31]
CONCLUSION
The selection of a local anesthetic for intraoral injection must include considerations of efficacy, safety, and individual patient and operative needs. Drug selection has to consider both components of the anesthetic solution. The local anesthetic agent must have a high intrinsic activity and a low systemic toxicity. The complications due to the local anesthetic solution itself demands a knowledge of the pharmacology of the drugs used and an awareness that it is important to obtain an accurate medical history.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rosenberg ES. A computer-controlled anesthetic delivery system in a periodontal practice: Patient satisfaction and acceptance. J Esthet Restor Dent. 2002;14:39–46. doi: 10.1111/j.1708-8240.2002.tb00146.x. [DOI] [PubMed] [Google Scholar]
- 2.Robinson PD, Pitt Ford TR, McDonald F. London: Reed Educational and Professional Publishing; 2000. Local anesthesia in dentistry. [Google Scholar]
- 3.Haas DA. An update on local anesthetics in dentistry. J Can Dent Assoc. 2002;68:546–51. [PubMed] [Google Scholar]
- 4.Chen AH. Toxicity and allergy to local anesthesia. J Calif Dent Assoc. 1998;26:683–92. [PubMed] [Google Scholar]
- 5.Gall H, Kaufmann R, Kalveram CM. Adverse reactions to local anesthetics: Analysis of 197 cases. J Allergy Clin Immunol. 1996;97:933–7. doi: 10.1016/s0091-6749(96)80067-4. [DOI] [PubMed] [Google Scholar]
- 6.Rood JP. Adverse reaction to dental local anesthetic injection —‘allergy’ is not the cause. Br Dent J. 2000;189:380–4. doi: 10.1038/sj.bdj.4800776. [DOI] [PubMed] [Google Scholar]
- 7.Aldrete JA, Narang R, Sada T, Tan Liem S, Miller GP. Reverse carotid flow: A possible explanation for some reactions to local anesthetics. J Am Dent Assoc. 1977;94:1142–5. doi: 10.14219/jada.archive.1977.0365. [DOI] [PubMed] [Google Scholar]
- 8.Meechan J. How to avoid local anesthetic toxicity. Br Dent J. 1998;184:334–5. doi: 10.1038/sj.bdj.4809619. [DOI] [PubMed] [Google Scholar]
- 9.Schiano AM, Strambi RC. Frequency of accidental intravascular injections in dental practice. Oral Surg. 1964;17:178. doi: 10.1016/0030-4220(64)90138-0. [DOI] [PubMed] [Google Scholar]
- 10.Wilburn-Goo D, Lloyd LM. When patients become cyanotic: Acquired methemoglobinemia. J Am Dent Assoc. 1999;130:826–81. doi: 10.14219/jada.archive.1999.0306. [DOI] [PubMed] [Google Scholar]
- 11.Tiwari IB, Keane T. Hemifacial palsy after inferior dental block for dental treatment. Br Med J. 1970;1:798. doi: 10.1136/bmj.1.5699.798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gray RL. Peripheral facial nerve paralysis of dental origin. Br J Oral Surg. 1978-79;16:143–50. doi: 10.1016/0007-117x(78)90024-0. [DOI] [PubMed] [Google Scholar]
- 13.Ling KC. Peripheral facial nerve paralysis after local dental anesthesia. Oral Surg Oral Med Oral Pathol. 1985;60:23–4. doi: 10.1016/0030-4220(85)90208-7. [DOI] [PubMed] [Google Scholar]
- 14.Miles EG. Facial palsy in the dental surgery. Case report and a review. Aust Dent J. 1992;37:262–5. doi: 10.1111/j.1834-7819.1992.tb04741.x. [DOI] [PubMed] [Google Scholar]
- 15.Bernsen PL. Peripheral facial nerve palsy after local upper dental anesthesia. Eur Neurol. 1993;33:90–1. doi: 10.1159/000116910. [DOI] [PubMed] [Google Scholar]
- 16.Shaib A, Lee MA. Recurrent peripheral facial nerve palsy after dental procedures. Oral Surg Oral Med Oral Pathol. 1990;70:738–40. doi: 10.1016/0030-4220(90)90011-g. [DOI] [PubMed] [Google Scholar]
- 17.Haas DA, Lennon D. A 21 year retrospective study of reports of paresthesia following local anesthetic administration. (323-6, 329-30).J Can Dent Assoc. 1995;61:319–20. [PubMed] [Google Scholar]
- 18.Malamed SF. 3rd ed. St Louis: Mosby-Year Book; 1990. Handbook of Local Anesthesia; pp. 160–218. (245-57). [Google Scholar]
- 19.Weinberg A, Shohat S, Stabholz A, Findler G. Transient hemiparesis following mandibular nerve anesthesia. Dental Traumatology. 1985;1:116–9. doi: 10.1111/j.1600-9657.1985.tb00573.x. [DOI] [PubMed] [Google Scholar]
- 20.Campbell RL, Mercuri LG, van Sickels J. Cervical sympathetic block following intraoral local anesthesia. Oral Surg Oral Med Oral Pathol. 1979;47:223–6. doi: 10.1016/0030-4220(79)90144-0. [DOI] [PubMed] [Google Scholar]
- 21.Fish LR, McIntire DN, Johnson L. Temporary paralysis of cranial nerves III, IV and VI after a Gow-Gates injection. J Am Dent Assoc. 1989;119:127–30. doi: 10.14219/jada.archive.1989.0137. [DOI] [PubMed] [Google Scholar]
- 22.Cooley RL, Cottingham AJ., Jr Ocular complications from local anaesthetic injections. Gen Dent. 1979;27:40. [PubMed] [Google Scholar]
- 23.Farrell RW, Pemberton MN, Parker AJ, Buffin JT. Sudden deafness after dental surgery. BMJ. 1991;303:1034. doi: 10.1136/bmj.303.6809.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Preshaw PM, Rowson JE. The use of lignocaine local anesthetic. Br Dent J. 1996;181:240. doi: 10.1038/sj.bdj.4809220. [DOI] [PubMed] [Google Scholar]
- 25.Pertl C, Heinemann A, Pertl B, Lorenzoni M, Pieber D, Eskici A, et al. The pregnant patient in dental care.Survey results and therapeutic guidelines. Schweiz Monatsschr Zahnmed. 2000;110:37–46. [PubMed] [Google Scholar]
- 26.Lawrenz DR, Whitley BD, Helfrick JF. Considerations in the management of maxillofacial infections in the pregnant patient. J Oral Maxillofac Surg. 1996;54:474–85. doi: 10.1016/s0278-2391(96)90125-1. [DOI] [PubMed] [Google Scholar]
- 27.Avraamides EJ, Craen RA, Gelb AW. Anesthetic management of a pregnant, post liver transplant patient for dental surgery. Anaesth Intensiv Care. 1997;25:68–70. doi: 10.1177/0310057X9702500112. [DOI] [PubMed] [Google Scholar]
- 28.Johnson CG. Local anesthetics and pregnancy. J Am Dent Assoc. 1985;110:302. doi: 10.14219/jada.archive.1985.0340. [DOI] [PubMed] [Google Scholar]
- 29.Watson AK. Local anesthetics in pregnancy. Br Dent J. 1989;166:36. doi: 10.1038/sj.bdj.4806702. [DOI] [PubMed] [Google Scholar]
- 30.Hunter ML, Hood CA, Hunter B, Kingdon A. Oral health advice: Reported experience of mothers of children aged 5 years and under referred for extraction of teeth under general anesthesia. Int J Pediatr Dent. 1998;8:13–27. doi: 10.1046/j.1365-263x.1998.00056.x. [DOI] [PubMed] [Google Scholar]
- 31.Hersh EV, Hermann DG, Lamp CJ, Johnson PD, MacAfee KA. Assessing the duration of mandibular soft tissue anesthesia. J Am Dent Assoc. 1995;126:1531–6. doi: 10.14219/jada.archive.1995.0082. [DOI] [PubMed] [Google Scholar]


