Abstract
Background:
The prevalence of denture stomatitis has been shown to vary from 15 to 65% in complete denture wearers. Satureja hortensis L. has been considered to have antinociceptive, anti-inflammatory, antifungal and antimicrobial activities in vitro and exhibits strong inhibitory effect on the growth of periodontal bacteria. The aim of this study was to evaluate the efficacy of a 1% gel formulation of S. hortensis essential oil for the treatment of denture stomatitis.
Materials and Methods:
A randomized, controlled clinical trial study was conducted on 80 patients (mean age 62.91±7.34) in two parallel groups treated either with S. hortensis essential oil 1% gel or placebo applied two times daily for two weeks. Denture stomatitis was diagnosed by clinical examination and paraclinical confirmation with sampling the palatal mucosa for Candida albicans. Data were analyzed using Chi-squared or Student's t tests.
Results:
The erythematous lesions of palatal area were significantly reduced (P<0.0001) in the treatment group who applied 1% topical gel of S. hortensis essential oil and Candida colonies count were reduced significantly (P=0.001).
Conclusion:
Topical application of the essential oil of S. hortensis could be considered as an effective agent for the treatment of denture stomatitis.
Keywords: Candida albicans, denture stomatitis, Satureja hortensis
INTRODUCTION
Denture stomatitis is an oral pathology in denture-bearing patients, especially under the maxillary prosthesis.[1,2] The prevalence of it has been shown to vary from 15 to 65%.[3] It usually manifests itself as an erythematous, edematous mucosa underlying and confined to the area covered by a complete upper denture.[4] Candida species are considered the primary causative agents of denture stomatitis.[2,4–6] The formation of Candida biofilms reduces the susceptibility of yeasts to antifungal agents.[1,7]
It seems that resistance of pathogenic fungi to antifungal agents has increased. Because of this side effects to common antifungal drugs,[1,4] novel fungal therapies with fewer side effects on humans are urgently required for effective management of candidiasis infections, so there are many studies on the use of herbal antifungal essential oils and extract.[1,4,8–13]
In several studies, about the antifungal effect of essential oils, specific anti-Candida activity of many aromatic plants has been described. The phenolic major components of these plants have been suggested to have a potent antifungal activity.[14–16]
Different species of the Satureja spp. are used in traditional medicine, food and pharmaceutical industries.[17] Some investigations suggest that the essential oil of the S. hortensis L. has antinociceptive,[18,19] anti-inflammatory,[18,19] antifungal[20,21] and antimicrobial activities[21–25] and a recent study has also demonstrated that growth of periodontal bacterial inhibition effect.[18,26] The main compounds in the essential oil of Satureja spp. are carvacrol, γ-terpinene and p-cymene.[21,24,25,27] To date, many diverse activities of carvacrol such as antimicrobial, antifungal, antitumor, analgesic, antispasmodic, anti-inflammatory are shown and discussed elsewhere.[15,18,25,28,29]
The aim of the present study was to evaluate the efficacy of S. hortensis essential oil gel for the treatment of denture stomatitis.
MATERIALS AND METHODS
This double-blind clinical trial was conducted in dental clinics affiliated to the Isfahan University of Medical Sciences Isfahan, Iran, from July 2010 until May 2011. Eighty complete denture wearers with denture stomatitis were enrolled. Forty outpatients (19 males and 21 females) were included in the study as case group, and 40 (12 males and 28 females) were included in the control group.
All patients who were wearing complete dentures for more than one year and suffered from type II or III palatal lesions according to Newton's classification[30] were included in this study. Accordingly moderate palatal lesions (Type II) were defined as a generalized inflammation of the denture-bearing area, and the severe one (Type III) was defined as a hyperplasic palatal surface of the palatal area. However patients who had diabetes mellitus, immunity suppression or systemic diseases, used antibiotic, antifungal drugs or antiseptic mouth wash within one month before the study as well as during the treatment course, had not followed the medical procedure during treatment and suffered of changing within the structure in denture, were excluded from the study.
All patients were examined by a specialized dentist and all demographic data, full medical and dental history for each patient were recorded.
A gel formulation of the essential oil of S. hortensis was prepared at the school of Pharmacy, Isfahan University of Medical Sciences. We formulated a carboxy methyl cellulose, Carbomer 934 (Merck®, Germany) and Plastibase (Jaber ebne Hayyan®, Tehran, Iran) gel base as placebo and the same gel base containing 1% of essential oil of the S. hortensis L. (Barij® Essence Company, Kashan, Iran) for the use of patients in this study.
At the first visit, erythema of the palatal mucosa was assessed visually, and the palatal mucosa were examined for the presence of yeasts by cultivating the samples on sabouraud dextrose agar plates with sterile swabs and were inoculated over the culture media, then incubated at 37°C and after 48 h the colonies were counted. The presence of one colony or more were considered as a positive result.[4]
Patients were randomly received either 1% gel of S. hortensis essential oil (cases) or placebo (controls) according to their profile numbers and the random figure tables. They were instructed to apply thin layer gel equals 1 cm on the base of the denture and the palatal mucosa twice daily (morning and night) for a period of two weeks. All patients were asked to keep the recommended hygienic instructions during treatment course. After 14 days, clinical and mycological evaluation was repeated to determine the efficacy of S. hortensis essential oil 1% gel.[1,4] If clinical alterations in the severity and extension of lesions were not observed, as well as any reduction in colony counts were seen, we reported it as no improvement. When the erythema surface of the palatal surface and colony counts were reduced, we considered it as partial improvement and in case of total elimination of erythematous lesions and the absence of any colonies, it was reported as complete improvement.
On days 14 and 21 after the first visit, all patients were assessed for treatment, local adverse reactions and asked as to whether they have experienced any adverse reactions.
The study protocol was approved by the board of ethics for human research at Isfahan University of Medical Sciences. All patients have completed informed consent form prior to the study, and no patient was deprived from the normal ordinary treatment if he/she refused for participation in the study.
All data were analyzed using SPSS® for windows (v.18). We have used χ2 test for analyzing qualitative data and Student's t test for quantitative data, considering P<0.05 as significant.
RESULTS
Eighty patients with the mean (±SD) age of 62.91±7.34 completely fulfilled the study protocol and 49 out of them were females. Participants’ demographic characteristics are summarized in Table 1. All patients of the two study groups were matched in terms of age, gender, colony count of C. albicans on palatal sample, duration of denture wearing, removal of denture during at night and Newton's type of denture stomatitis [Table 1]. And 77.5% of control group and 67.5% of the case group did not remove their denture during the night. According to this data, no significant differences was seen between the severity of lesions in both groups (P=0.317).
Table 1.
Baseline characteristics and the outcome of treatment with Savory essential oil in the study patients
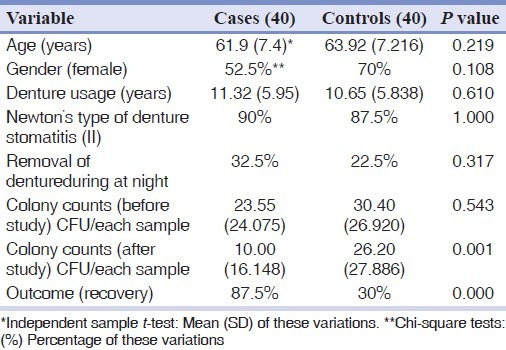
In this study, the most common form of observed denture stomatitis lesions in both groups (cases and controls) was in Newton's Type II classification.[30]
Figure 1 shows the change in the inflammatory state of the palatal mucosa before and after treatment with the topical drug and placebo in cases and control groups respectively.
Figure 1.
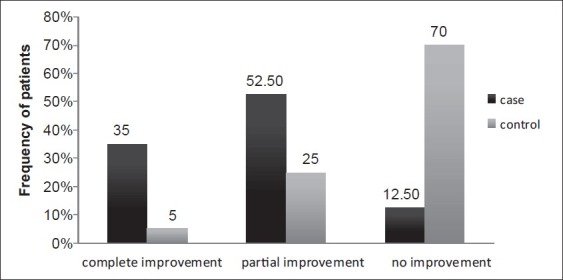
Inflammation changes of palatal mucosa in case and control groups
Patients in the intervention arm of the study (cases) who applied 1% gel of S. hortensis for two consecutive weeks had a statistically significant improvement in colony count of Candida (P=0.001) and the erythema of palatal mucosa (P=0.000) [Figure 1].
DISCUSSION
Denture stomatitis is an inflammatory process of the oral mucosa associated with the presence of Candida or other microorganisms and factors, such as denture wearing and long term antibiotic therapy. Candida albicans represents the most common causative agent of the oral candidiasis.[13,31]
Candida albicans is a part of the normal flora of mouth in human, and the density of growths of Candida may have a role in candidial infections. In this way, the rational use of antifungal agents in the treatment of these clinical conditions seems to be justifiable.[4,13]
In this study, all patients of the two study groups were matched in terms of age, gender, colony count of C. albicans on palatal sample, duration of denture wearing, removal of denture during at night and Newton's type of denture stomatitis [Table 1]. In agreement with many other studies, predisposing local factors include poor denture hygiene, continual and night time wearing of removable dentures.[32–34]
Patients in the intervention arm of the study (cases) who applied 1% gel of S. hortensis for two consecutive weeks had a statistically significant improvement in colony count of Candida (P=0.001) [Table 1] and the erythema of palatal mucosa (P=0.000) [Figure 1].
As mentioned in other study,[1] For oral topical drug administrations, it is necessary to note that the constant flow of saliva, and the mobility of the involved tissues may cause a rapid decline in therapeutic concentration of drug and consequently result in treatment failure. In this case, selection of buccal mucoadhesive formulations, such as these orabase formulations, can help to overcome these problems.
In our study, spicy odor of the essential oil was the only minor complaint of patients which is comparable to similar oral topical gels.[35] However the topical formulation which we used could be corrected and developed in further pharmaceutical studies. We have not observed any other reportable side effects in patients receiving the herbal gel.
Due to the increasing resistance of micro-organisms against antifungal agents and their side effects, formation of Candida biofilm and generally positive attitude of patients for natural treatment, novel herbal antifungal therapies with fewer side effects on humans are rational for effective management of candidiasis infections. There are studies on the use of herbal antifungal and especially anti candidial characteristics of some essential oils.[8–13]
Satureja is one of the aromatic plants with a wide spectrum of pharmacologic properties.[18,20]
Another species of this plant, S. khuzestanicais has been shown to have analgesic, antiseptic, antioxidant, antimicrobial, antiviral, antifungal, anti-inflammatory, anti-nociceptive, antidiabetic and anti-hyperlipidemic effects.[19,36,37] S. hortensis is used as a drug in traditional medicine and as a food additive in food industries.[17] Evidences for antinociceptive, anti-inflammatory, antifungal and antimicrobial activities of the essential oil S. hortensis are reported previously elsewhere.[18,20,26,38] Essential oil of S. hortensis L. exhibits a strong inhibitory effect on the growth of periodontal bacteria.[18,26] Hence, researchers have studied the chemical composition of extracts and essential oils isolated from this aromatic plant.[21,25] The phenolic major components of them have been suggested to have a potent antifungal activity.[14–16] Carvacrol, γ-terpinene and p-cymene are major components of Satureja spp.[19,21] Many pharmacologic activities of the essential oil of Satureja such as antimicrobial, antifungal, antitumor, analgesic, antispasmodic, anti-inflammatory effects are attributed to the chemical structure of these phenolic compounds.[15,28,29]
In this study, reduction in the number of Candida and erythematous surface in both of two arms may be justifiable because of the effect of the standard hygienic recommendations (e.g., cleaning the dentures and denture brushing, removal of denture overnight) during the study which is consistent when compared with previous one.[13] On the other hand, because of coverage of the palatal mucosa with the denture, especially during the night, antimicrobial effect of saliva which has an important role in the maintenance of oral health is attenuated.[11]
In our study, reduction of the erythema surface was more significant in the treatment group which supports previous reports on above mentioned pharmacological effects.
In conclusion, this study showed that the gel formulation of the essential oil of S. hortensis could be an effective agent for the treatment of denture stomatitis and may be considered safe regarding its nutraceutical and folklore usage. However, further studies are needed to investigate other therapeutic aspects of this essential oil for maintaining oral health.
ACKNOWLEDGEMENTS
This research was the result of a doctor of pharmacy thesis project which was supported financially by the vice-chancellery of research at the Isfahan University of Medical Sciences. It was designed and conducted by the Isfahan Clinical Toxicology Research Centre (http://ctrc.mui.ac.ir). The authors would like to thank the academic faculty members of the school of Dentistry at the Isfahan University of Medical Sciences and all the colleagues and staff of the Professor Torabinejad Dental Research Center for their valuable endeavors and support.
Footnotes
Source of Support: This project was financially supported by the Vice-chancellery for Research and Technology of the Isfahan University of Medical Sciences, Isfahan, Iran
Conflict of Interest: Authors had no conflict of interest, including personal or financial relationships with organizations that might inappropriately influence, or be perceived to influence the work.
REFERENCES
- 1.Santos VR, Gomes RT, de Mesquita RA, de Moura MD, Franca EC, de Aguiar EG, et al. Efficacy of Brazilian propolis gel for the management of denture stomatitis: A pilot study. Phytother Res. 2008;22:1544–7. doi: 10.1002/ptr.2541. [DOI] [PubMed] [Google Scholar]
- 2.Casaroto AR, Lara VS. Phytomedicines for Candida-associated denture stomatitis. Fitoterapia. 2010;81:323–8. doi: 10.1016/j.fitote.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Uludamar A, Ozkan YK, Kadir T, Ceyhan I. In vivo efficacy of alkaline peroxide tablets and mouthwashes on Candida albicans in patients with denture stomatitis. J Appl Oral Sci. 2010;18:291–6. doi: 10.1590/S1678-77572010000300017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amanlou M, Beitollahi JM, Abdollahzadeh S, Tohidast-Ekrad Z. Miconazole gel compared with Zataria multiflora Boiss. gel in the treatment of denture stomatitis. Phytother Res. 2006;20:966–9. doi: 10.1002/ptr.1986. [DOI] [PubMed] [Google Scholar]
- 5.Zomorodian K, Haghighi NN, Rajaee N, Pakshir K, Tarazooie B, Vojdani M, et al. Assessment of Candida species colonization and denture-related stomatitis in complete denture wearers. Med Mycol. 2011;49:208–11. doi: 10.3109/13693786.2010.507605. [DOI] [PubMed] [Google Scholar]
- 6.Salerno C, Pascale M, Contaldo M, Esposito V, Busciolano M, Milillo L, et al. Candida-associated denture stomatitis. Med Oral Patol Oral Cir Bucal. 2011;16:e139–43. doi: 10.4317/medoral.16.e139. [DOI] [PubMed] [Google Scholar]
- 7.Redding S, Bhatt B, Rawls HR, Siegel G, Scott K, Lopez-Ribot J. Inhibition of Candida albicans biofilm formation on denture material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:669–72. doi: 10.1016/j.tripleo.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 8.Mahdavi-Omran S, Esmailzadeh S. Comparison of anti-Candida activity of thyme, pennyroyal, and lemon essential oils versus antifungal drugs against Candida species Jundishapur. J Microbiol. 2009;2:53–60. [Google Scholar]
- 9.Camele I, De Feo V, Altieri L, Mancini E, De Martino L, Luigi Rana G. An attempt of postharvest orange fruit rot control using essential oils from Mediterranean plants. J Med Food. 2010;13:1515–23. doi: 10.1089/jmf.2009.0285. [DOI] [PubMed] [Google Scholar]
- 10.Vasconcelos LC, Sampaio MC, Sampaio FC, Higino JS. Use of Punica granatum as an antifungal agent against candidosis associated with denture stomatitis. Mycoses. 2003;46:192–6. doi: 10.1046/j.1439-0507.2003.00884.x. [DOI] [PubMed] [Google Scholar]
- 11.Rosato A, Vitali C, Gallo D, Balenzano L, Mallamaci R. The inhibition of Candida species by selected essential oils and their synergism with amphotericin B. Phytomedicine. 2008;15:635–8. doi: 10.1016/j.phymed.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Ozcan MM, Chalchat JC, Arslan D, Ates A, Unver A. Comparative essential oil composition and antifungal effect of bitter fennel (Foeniculum vulgare ssp.piperitum) fruit oils obtained during different vegetation. J Med Food. 2006;9:552–61. doi: 10.1089/jmf.2006.9.552. [DOI] [PubMed] [Google Scholar]
- 13.Pinto TM, Neves AC, Leao MV, Jorge AO. Vinegar as an antimicrobial agent for control of Candida spp.in complete denture wearers. J Appl Oral Sci. 2008;16:385–90. doi: 10.1590/S1678-77572008000600006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chami N, Chami F, Bennis S, Trouillas J, Remmal A. Antifungal treatment with carvacrol and eugenol of oral candidiasis in immunosuppressed rats. Braz J Infect Dis. 2004;8:217–26. doi: 10.1590/s1413-86702004000300005. [DOI] [PubMed] [Google Scholar]
- 15.Baser KH. Biological and pharmacological activities of carvacrol and carvacrol bearing essential oils. Curr Pharm Des. 2008;14:3106–19. doi: 10.2174/138161208786404227. [DOI] [PubMed] [Google Scholar]
- 16.Naeini A, Khosravi AR, Chitsaz M, Shokri H, Kamlnejad M. Anti-Candida albicans activity of some Iranian plants used in traditional medicine. J Mycol Med. 2009;19:168–72. [Google Scholar]
- 17.Hadian J, Azizi A, Tabatabaei MF, Naghavi MR, Jamzad Z, Friedt W. Analysis of the genetic diversity and affinities of different Iranian Satureja species based on SAMPL markers. Planta Med. 2010;76:1927–33. doi: 10.1055/s-0030-1250063. [DOI] [PubMed] [Google Scholar]
- 18.Hajhashemi V, Ghannadi A, Pezeshkian SK. Antinociceptive and anti-inflammatory effects of Satureja hortensis L.extracts and essential oil. J Ethnopharmacol. 2002;82:83–7. doi: 10.1016/s0378-8741(02)00137-x. [DOI] [PubMed] [Google Scholar]
- 19.Amanlou M, Dadkhah F, Salehnia A, Farsam H, Dehpour AR. An anti-inflammatory and anti-nociceptive effects of hydroalcoholic extract of Satureja khuzistanica Jamzad extract. J Pharm Pharm Sci. 2005;8:102–6. [PubMed] [Google Scholar]
- 20.Boyraz N, Ozcan M. Inhibition of phytopathogenic fungi by essential oil, hydrosol, ground material and extract of summer savory (Satureja hortensis L.) growing wild in Turkey. Int J Food Microbiol. 2006;107:238–42. doi: 10.1016/j.ijfoodmicro.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Gulluce M, Sokmen M, Daferera D, Agar G, Ozkan H, Kartal N, et al. In vitro antibacterial, antifungal, and antioxidant activities of the essential oil and methanol extracts of herbal parts and callus cultures of Satureja hortensis L. J Agric Food Chem. 2003;51:3958–65. doi: 10.1021/jf0340308. [DOI] [PubMed] [Google Scholar]
- 22.Sahin F, Karaman I, Gulluce M, Ogutcu H, Sengul M, Adiguzel A, et al. Evaluation of antimicrobial activities of Satureja hortensis L. J Ethnopharmacol. 2003;87:61–5. doi: 10.1016/s0378-8741(03)00110-7. [DOI] [PubMed] [Google Scholar]
- 23.Saharkhiz MJ, Zomorodian K, Rezaei MR, Saadat F, Rahimi MJ. Influence of growth phase on the essential oil composition and antimicrobial activities of Satureja hortensis. Nat Prod Commun. 2011;6:1173–8. [PubMed] [Google Scholar]
- 24.Mihajilov-Krstev T, Kitic D, Stojanovic-Radic Z, Zlatkovic B. Antimicrobial activity of Satureja hortensis L.essential oil against pathogenic microbial strains. Arch Biol Sci. 2010;62:159–66. [Google Scholar]
- 25.Mihajilov-Krstev T, Radnović D, Kitić D, Zlatković B, Ristić M, Branković S. Chemical composition and antimicrobial activity of Satureja hortensis L.essential oil. Cent Eur J Biol. 2009;4:411–6. [PubMed] [Google Scholar]
- 26.Gursoy UK, Gursoy M, Gursoy OV, Cakmakci L, Kononen E, Uitto VJ. Anti-biofilm properties of Satureja hortensis L.essential oil against periodontal pathogens. Anaerobe. 2009;15:164–7. doi: 10.1016/j.anaerobe.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 27.Ben Arfa A, Combes S, Preziosi-Belloy L, Gontard N, Chalier P. Antimicrobial activity of carvacrol related to its chemical structure. Lett Appl Microbiol. 2006;43:149–54. doi: 10.1111/j.1472-765X.2006.01938.x. [DOI] [PubMed] [Google Scholar]
- 28.Razzaghi-Abyaneh M, Shams-Ghahfarokhi M, Yoshinari T, Rezaee MB, Jaimand K, Nagasawa H, et al. Inhibitory effects of Satureja hortensis L. essential oil on growth and aflatoxin production by Aspergillus parasiticus. Int J Food Microbiol. 2008;123:228–33. doi: 10.1016/j.ijfoodmicro.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 29.Dikbas N, Kotan R, Dadasoglu F, Sahin F. Control of Aspergillus flavus with essential oil and methanol extract of Satureja hortensis. Int J Food Microbiol. 2008;124:179–82. doi: 10.1016/j.ijfoodmicro.2008.03.034. [DOI] [PubMed] [Google Scholar]
- 30.Newton AV. Denture sore mouth: A possible aetiology. Br Dent J. 1962;112:357–60. [Google Scholar]
- 31.Marcos-Arias C, Vicente JL, Sahand IH, Eguia A, De-Juan A, Madariaga L, et al. Isolation of Candida dubliniensis in denture stomatitis. Arch Oral Biol. 2009;54:127–31. doi: 10.1016/j.archoralbio.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 32.Kulak Y, Arikan A. Aetiology of denture stomatitis. J Marmara Univ Dent Fac. 1993;1:307–14. [PubMed] [Google Scholar]
- 33.Bilhan H, Sulun T, Erkose G, Kurt H, Erturan Z, Kutay O, et al. The role of Candida albicans hyphae and Lactobacillus in denture-related stomatitis. Clin Oral Investig. 2009;13:363–8. doi: 10.1007/s00784-008-0240-6. [DOI] [PubMed] [Google Scholar]
- 34.Gendreau L, Loewy ZG. Epidemiology and etiology of denture stomatitis. J Prosthodont. 2011;20:251–60. doi: 10.1111/j.1532-849X.2011.00698.x. [DOI] [PubMed] [Google Scholar]
- 35.Meechan JG. Intra-oral topical anaesthetics: Review. J Dent. 2000;28:3–14. doi: 10.1016/s0300-5712(99)00041-x. [DOI] [PubMed] [Google Scholar]
- 36.Vosough-Ghanbari S, Rahimi R, Kharabaf S, Zeinali S, Mohammadirad A, Amini S, et al. Effects of Satureja khuzestanica on Serum Glucose, Lipids and Markers of Oxidative Stress in Patients with Type 2 Diabetes Mellitus: A Double-Blind Randomized Controlled Trial. Evid Based Complement Alternat Med. 2010;7:465–70. doi: 10.1093/ecam/nen018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abdollahi M, Salehnia A, Mortazavi SH, Ebrahimi M, Shafiee A, Fouladian F, et al. Antioxidant, antidiabetic, antihyperlipidemic, reproduction stimulatory properties and safety of essential oil of Satureja khuzestanica in rat in vivo: A oxicopharmacological study. Med Sci Monit. 2003;9:BR331–5. [PubMed] [Google Scholar]
- 38.Özcan M, Boyraz N. Antifungal properties of some herb decoctions. Eur Food Res Technol. 2000;212:86–8. [Google Scholar]


