Abstract
Background
Older women have a higher prevalence of systolic hypertension than do men; however, whether or not this relates to arterial properties, such as distensibility coefficient (DC), is not known. We examined whether the association of carotid artery DC with age differed by sex in the Multi-Ethnic Study of Atherosclerosis (MESA).
Methods
B-mode ultrasound-measured carotid diameters and brachial pressures were obtained from 6359 participants (53% female, 38% white, 12% Chinese, 27% black, 22% Hispanic, aged 45–85 years) of the MESA baseline examination. The within-individual slopes of 2log(diameter) vs. blood pressure fit using mixed models (MM) are interpreted as the DC, and interaction terms are interpreted as differences in DC. The MM calculation allows for correction of the confounding caused by the association of age, sex, and race with blood pressure, the denominator in the calculation of DC.
Results
DC was associated with age, sex, and race (all p<0.001). Women had a greater age-related lowering of DC compared to men (2.52×10−5 vs. 2.16×10−5/mm Hg lower DC per year of age, p=0.006). Mean diameter of carotid arteries was greater with age (p<0.001); this association also was significantly stronger in women compared to men (0.24% vs. 0.14% larger mean carotid diameter per year of age, p<0.001).
Conclusions
Greater stiffening and enlargement of arteries are seen in older women compared to older men. This implies that the afterload on the heart of older women is likely to be greater than that among older men.
Introduction
The stiffening of arteries throughout life is thought to underlie the pathogenesis of such diseases as hypertension1 and heart failure2 that are associated with aging. Older women have a greater prevalence of hypertension than do older men.3 It is not known, however, if this difference of aging by sex is because of sex differences in the stiffness of arteries at different ages.
The material properties of arteries (related to stiffness and compliance) may be measured invasively,4 but this is not possible in large studies where sex by age interaction can be assessed. Therefore, direct noninvasive imaging of arteries is often used. The systolic and diastolic diameters of the carotid artery obtained by ultrasound and the simultaneous measure of systolic and diastolic brachial artery pressure5 allow the investigator to determine the distensibility coefficient (DC) in the linear approximation. If epidemiologic associations of these material properties with other variables are sought, however, variables that are associated with only one or the other of the component variables (i.e., systolic or diastolic diameters, systolic or diastolic pressures) may erroneously appear to be associated with the material properties of the arteries.6 Because the diameters and pressures are a part of a nonlinear calculation of DC, usual linear regression methods to adjust for confounding is not appropriate. A recent publication shows association of incident coronary disease and stroke with carotid artery stiffness measures, and this association is either fully or greatly attenuated by linear adjustment by blood pressure (BP) measures, likely due to overadjustment.7
We have analyzed Multi-Ethnic Study of Atherosclerosis (MESA) data using mixed model (MM) statistical methods that appropriately correct for such confounding to test for differences in the material properties of arteries between groups using these methods. Our aim is to determine if there is a difference in the relationship of age with the distensibility of arteries by sex, adjusting for BP levels in the population-based MESA.
Materials and Methods
Study population
We used baseline data from the MESA. The design of MESA, a study of the prevalence and progression of subclinical atherosclerosis, has been described previously.8 Briefly, 6814 individuals, all free of clinical cardiovascular disease (CVD) at baseline, aged 45–85 years, of four ethnicities (Caucasian, Chinese, Hispanic, and African American), were enrolled at six U.S. sites. Of these, 6359 participants had carotid ultrasound data adequate for the calculation of carotid artery distensibility and compliance.
B-mode ultrasound and brachial BP measurements
Detailed methods have been published previously.9 A 20-second B-mode ultrasound recording including a longitudinal section of the distal right common carotid artery was acquired using a Logiq 700 machine (General Electric Medical Systems). Single measures of brachial systolic and diastolic BPs were obtained simultaneously (DINAMAPP System, GE Medical systems). This single measurement corresponded well with a three-measure average of seated BP (Pearson correlation coefficients: systolic 0.78, diastolic 0.74, pulse pressure 0.78). Ultrasound images were analyzed and interpreted by the MESA ultrasound reading center, located at Tufts Medical Center, Boston, MA, which used edge-detection software to extract the carotid artery diameters in the images. Systolic and diastolic diameters were determined as the largest and smallest diameters during the cardiac cycle. For the DC (calculated using the linear approximation in Supplementary Table S1 available online at www.liebertonline.com), the repeat-study class correlation coefficient was 0.71, and the repeat-reading class correlation was 0.68.9
Statistical methods
The traditional method of calculating DC is as follows:
 |
1 |
where D represents the diameter of the artery, P represents the BP within the artery, Δ represents the difference between systolic and diastolic measurements, and  represents the appropriate mean value of the diameter. In practice,
represents the appropriate mean value of the diameter. In practice,  may be approximated to the systolic or diastolic diameter.5
may be approximated to the systolic or diastolic diameter.5
We used MM regression where diameters and BP were modeled; thus, DC and differences in DC were estimated within the model, appropriately adjusted for confounders. This allows for disentangled estimation of the associations of independent variables with diameter alone and with distensibility. This contrasts with calculation of DC outside the statistical model, when the association and confounding of diameter and distensibility are entangled.
Differences in DC were estimated in the multivariate model, which allowed for adjustment for the confounding of BP by covariates. For a single binary covariate (e.g., F=0 if male, 1 if female), the model would be specified as:
 |
2 |
for the ith condition (diastole or systole) of the jth individual. Random effects are estimated for the average log-diameters (log-diameter at the average of the systolic and diastolic pressure for each individual) and the slope of the log-diameter to pressure slope for every individual, which is determined using diastolic and systolic pressure (γ and η, respectively). The coefficients β3 and β4 can be interpreted as the fixed-effect association of the binary covariate with the mean diameter and the fixed-effect difference in slopes (i.e., the material properties of the artery) associated with the covariate. This specification can be generalized to any categorical or linear continuous covariate.
A detailed explanation of the MM regression is provided as Supplementary material (available online at www.liebertonline.com). Models with age (centered at 65 years), sex, race, and height were evaluated. First-order (two-way) interactions between age, sex, and race were also evaluated. Only significant interactions (p<0.05) were retained.
The MM-estimated DC for every individual from best linear unbiased predicted (BLUP) values was compared with the traditionally calculated DC. The mean of the MM DC was numerically close to the mean of traditionally calculated DC (0.0025 vs. 0.0025), although the standard deviation (SD) was smaller (0.0006 vs. 0.0011), showing a shrinkage of variation due to the MM estimation. The Spearman correlation of the traditionally calculated DC with model-fitted DC was 0.81. In sensitivity analysis, the final regression models were further adjusted for education (as a proxy for socioeconomic status [SES]) and the use of BP medications to check for possible confounding. Another model excluding individuals using BP medications was also evaluated.
Results
Population characteristics
The MESA population has been described previously.10 The demographic and clinical profile of the participants included in this analysis are shown in Table 1.
Table 1.
Demographic and Cardiovascular Risk Characteristics of Sample, by Race/Ethnicity
| Caucasian American | Chinese American | African American | Hispanic American | |
|---|---|---|---|---|
| n | 2435 | 773 | 1732 | 1419 |
| Age (years) | 62.6±10.3 | 62.4±10.4 | 62.3±10.1 | 61.3±10.3 |
| Males | 1176 (48%) | 377 (49%) | 773 (45%) | 693 (49%) |
| Height (cm) | 169.0±9.7 | 161.6±8.6 | 168.3±9.7 | 161.9±10.3 |
| SBP (mm Hg) | 123.4±20.5 | 124.4±21.6 | 131.8±21.7 | 126.6±21.8 |
| DBP (mm Hg) | 70.2±10.0 | 71.9±9.4 | 74.6±10.2 | 71.6±10.1 |
| Antihypertensive use | 632 (26%) | 214 (28%) | 819 (47%) | 415 (29%) |
| Type 2 DM | 144 (6%) | 104 (13%) | 302 (18%) | 243 (17%) |
| Current smokers | 285 (12%) | 44 (6%) | 306 (18%) | 190 (13%) |
| TC (mg/dL) | 195.5±35.2 | 192.4±34.7 | 189.5±36.4 | 197.8±37.3 |
| HDL-C (mg/dL) | 52.1±15.5 | 49.7±12.9 | 52.5±15.3 | 47.6±13.1 |
Mean±standard deviation (SD) or number (%).
DBP, diastolic blood pressure; DM, diabetes mellitus, using American Diabetes Association 2003 criteria; HDL-C, high-density lipoprotein cholesterol; SBP, systolic blood pressure; TC, serum total cholesterol.
Age, sex, and race associations of the distensibility coefficient
The MM simultaneously assesses the association of covariables with mean arterial diameter and the D.C. Age, sex, race, and the age-sex interaction had significant associations in the regression analysis (Table 2). In addition, the arterial diameter at the average of systolic and diastolic pressures is larger in older persons, but this association is significantly greater in women than men. Ethnic differences in diameter are also seen, with Chinese having the smallest diameter and Hispanics having the largest diameter. Supplementary Table S2 (available online at www.liebertonline.com) shows that adjusting for the traditional risk factors, smoking, total cholesterol, and high-density lipoprotein cholesterol (HDL-C) levels, and current diabetes, does not change the levels of significance for any of these results. Supplementary Table S3 (available online at www.liebertonline.com) shows various models assessing the association of carotid diameters and pressures with age, sex, and race. These traditional linear models with DC as the dependent variable include BP as a covariate, which results in overadjustment.
Table 2.
Association of Age, Sex, and Race with Carotid Artery Distensibility Coefficient and Diameter
| |
Difference in DC (2*slope) mm Hg−1 |
% Larger carotid diameter (intercept) |
|---|---|---|
| Covariate | Beta coefficients (95% CI) | |
| Sex (male vs. female) at 65 years of age | 8.24 (0.62-15.8)×10−5 | 4.83 (3.99-5.69)% |
| Age (difference per year among females) | −5.04 (−5.38-−4.70)×10−5 | 0.24 (0.20-0.28)% |
| Difference in age-associated slope between men and women | 7.14 (2.10-12.2)×10−6 | −0.10 (−0.15-−0.04)% |
| Height (difference per cm of height) | 3.08 (−0.98-7.14)×10−6 | 0.19 (0.15-0.24)% |
| White | Reference | Reference |
| Chinese vs. White | −1.88 (−2.81-−0.96)×10−4 | −3.77 (−2.78-−4.75)% |
| African American vs. White | −3.06 (−3.70-−2.42)×10−4 | −0.09 (−0.81-0.62)% |
| Hispanic vs. White | −2.81 (−3.55-−2.07)×10−4 | 1.15 (0.33-1.97)% |
| Overall test for race/ethnicity | p=7.6×10−23 | p=1.1×10−13 |
Intercept: mixed model intercept coefficient corresponding to group difference between geometric means in percent; slope: mixed model slope coefficient corresponding to distensibility coefficient difference by group; 2*slope=difference in distensibility coefficient; to allow for judging of magnitude of coefficients, the standard deviation (SD) of distensibility coefficient=1.1×10−3; for example, the beta coefficient for age in women is −5.04×10−5/mm Hg. This means that, on average, keeping other covariates constant, if 2 women differ 1 year in age, the older would have DC lower by −5.04×10−5/mm Hg, which corresponds to 0.045 SD units. The SI unit for distensibility, kPa−1=7.5 mm Hg−1.
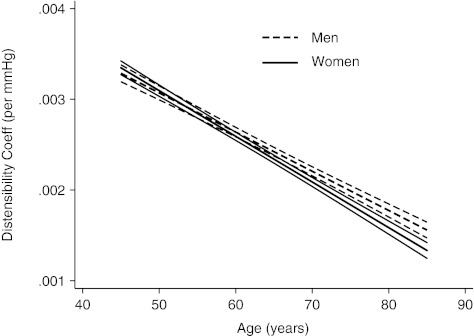
The age-sex interaction found in the mixed model is graphically illustrated in Figure 1, where model-calculated DCs, adjusted for race distribution and mean height (166 cm) are plotted against age among women and men. In both men and women, the DCs are lower with greater age. Although the DCs in men and women have similar values in the age range 45–60 years (confidence intervals [CI] overlap), at older ages, the DCs in women are lower than those in men. Because numerical measures of DC are not intuitive, Figure 1 illustrates the sex interaction in age equivalents. A difference of 10 chronologic years results in a reduced distensibility equivalent of 11.6 years in women compared to 10 years in men.
FIG. 1.
Fitted age-distensibility coefficient relationship for men (dashed lines) and women (solid lines), adjusted for race and mean height (166 cm), and their 95% confidence intervals calculated using mixed model analysis.
In sensitivity analyses, there was no difference in significant associations in the MM after addition of education and use of BP medications to the model. When analyses were restricted to 4279 individuals who were not using BP medications, all associations remained significant except for one: the difference between DC of men compared to women at age 65 was no longer significant (beta=3.59×10−5, p=0.16); however, the magnitude of the point estimate was similar to that tabulated for the main analysis. The association of traditionally calculated DC with age, sex, race, and the age-sex interaction is contrasted with the MM results in the supplementary material (available online at www.liebertonline.com).
Discussion
We have shown significant sex-age interaction in association with both DC and mean carotid artery diameter in a large well-characterized multi-ethnic population-based study. Our findings are consistent with those of Redfield et al.,11 who found that vascular and systolic and diastolic ventricular elastance was more steeply associated with age in women than men in Olmsted County, Minnesota.
Using appropriate MM statistical methods, we were able to show associations of DC with covariates with two distinct advantages over using traditional calculations of DC: (1) the associations in our models were adjusted for BP levels, which is not possible for traditionally calculated DC, where BPs are part of the nonlinear calculation and (2) using our analytic model, the MM also provides estimates of association with mean carotid artery diameter, which has been shown to be associated with carotid atherosclerosis.12 Our results show that MM analysis can detect significant associations that have been previously published using within-participant calculation of DC9 in the same study dataset.
Although our analysis reproduced the findings of Blaha et al.9 for some covariates, we also contribute several important new findings. We have shown interethnic differences in mean carotid artery diameters that have not been reported previously. Whereas the sex differences in arterial diameters are expected, the age-sex interaction is novel. Older women have larger arterial diameters than young women, and this age association is steeper than the age association among men. Also, the age-sex interaction in DC means that older women have stiffer arteries than older men. To give a sense of the magnitude of the differences, we use the unadjusted hazard ratios for stroke associated with lower distensibility reported by Yang et al.7: because of differences in DC, women who are 10 years older would have a 30.4% higher hazard of stroke than their younger counterparts, whereas men with the same age difference would have a 25.6% higher hazard of stroke. In addition, the afterload on the heart of older women is likely to be greater than that among older men. This may help to explain why older women predominate among patients with heart failure with preserved systolic function.13 It may also have a part in explaining why although the absolute mortality rate is higher in men than women, the rate of increase of total heart disease mortality in men >45 years rises less steeply than in women.14
Because this is a cross-sectional, observational study, we are circumspect about clinical and treatment-related implications of this finding. It is noteworthy that current antihypertensive drugs of choice have somewhat lower effectiveness in women compared to men in the prevention of death in heart failure.15 It is possible that drugs that improve arterial distensibility might be more efficacious in prevention of heart failure mortality in women.16
Strengths and limitations
The large multi-ethnic database of both men and women with a large range of ages collected using rigorous measurement standards is a significant strength of this study. A limitation of this study is that the arterial diameter imaging was of the carotid artery, but pressure measurement was performed in the brachial artery. There was no invasive gold standard measurement of distensibility. However, the aim of study was to analyze the kind of noninvasive measurement practical in large-scale studies, such as MESA, which have been reported in current published literature,9 rather than comparison with a gold standard measurement.
Conclusions
We have shown sex and ethnic differences in the diameter and distensibility of the carotid artery, with adjustment for confounding by BP. Furthermore, we have shown a sex-age interaction that can be hypothesized to have worse consequences of arterial stiffness among older women compared to older men. The biologic underpinnings of these strong findings and whether they translate into differences in heart failure and other cardiovascular outcomes remain to be determined by future research.
Supplementary Material
Acknowledgments
This research was supported by contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung, and Blood Institute. We thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at www.mesa-nhlbi.org. D.V. was supported by grant Number UL1 RR 025005 from the National Center for Research Resources, a component of the National Institutes of Health.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Safar ME. Systolic hypertension in the elderly: Arterial wall mechanical properties and the renin-angiotensin-aldosterone system. J Hypertens. 2005;23:673–681. doi: 10.1097/01.hjh.0000163130.39149.fe. [DOI] [PubMed] [Google Scholar]
- 2.Kass DA. Age-related changes in venticular-arterial coupling: Pathophysiologic implications. Heart Fail Rev. 2002;7:51–62. doi: 10.1023/a:1013749806227. [DOI] [PubMed] [Google Scholar]
- 3.Martins D. Nelson K. Pan D. Tareen N. Norris K. The effect of gender on age-related blood pressure changes and the prevalence of isolated systolic hypertension among older adults: Data from nhanes III. J Gend Specif Med. 2001;4:10–13. , 20. [PubMed] [Google Scholar]
- 4.Salvi P. Lio G. Labat C. Ricci E. Pannier B. Benetos A. Validation of a new non-invasive portable tonometer for determining arterial pressure wave and pulse wave velocity: The Pulsepen device. J Hypertens. 2004;22:2285–2293. doi: 10.1097/00004872-200412000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Reneman RS. Meinders JM. Hoeks AP. Non-invasive ultrasound in arterial wall dynamics in humans: What have we learned and what remains to be solved? Eur Heart J. 2005;26:960–966. doi: 10.1093/eurheartj/ehi177. [DOI] [PubMed] [Google Scholar]
- 6.Laurent S. Cockcroft J. Van Bortel L, et al. Expert consensus document on arterial stiffness: Methodological issues and clinical applications. Eur Heart J. 2006;27:2588–2605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 7.Yang EY. Chambless L. Sharrett AR, et al. Carotid arterial wall characteristics are associated with incident ischemic stroke but not coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2012;43:103–108. doi: 10.1161/STROKEAHA.111.626200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bild DE. Bluemke DA. Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: Objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 9.Blaha MJ. Budoff MJ. Rivera JJ, et al. Relationship of carotid distensibility and thoracic aorta calcification: Multi-Ethnic Study of Atherosclerosis. Hypertension. 2009;54:1408–1415. doi: 10.1161/HYPERTENSIONAHA.109.138396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McClelland RL. Chung H. Detrano R. Post W. Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: Results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 11.Redfield MM. Jacobsen SJ. Borlaug BA. Rodeheffer RJ. Kass DA. Age- and gender-related ventricular-vascular stiffening: A community-based study. Circulation. 2005;112:2254–2262. doi: 10.1161/CIRCULATIONAHA.105.541078. [DOI] [PubMed] [Google Scholar]
- 12.Montalcini T. Gorgone G. Gazzaruso C. Sesti G. Perticone F. Pujia A. Large brachial and common carotid artery diameter in postmenopausal women with carotid atherosclerosis. Atherosclerosis. 2008;196:443–448. doi: 10.1016/j.atherosclerosis.2006.11.040. [DOI] [PubMed] [Google Scholar]
- 13.Bursi F. Weston SA. Redfield MM, et al. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–2216. doi: 10.1001/jama.296.18.2209. [DOI] [PubMed] [Google Scholar]
- 14.Vaidya D. Becker DM. Bittner V. Mathias RA. Ouyang P. Ageing, menopause, and ischaemic heart disease mortality in England, Wales, and the United States: Modelling study of national mortality data. BMJ. 2011;343:d5170. doi: 10.1136/bmj.d5170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shekelle PG. Rich MW. Morton SC, et al. Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: A meta-analysis of major clinical trials. J Am Coll Cardiol. 2003;41:1529–1538. doi: 10.1016/s0735-1097(03)00262-6. [DOI] [PubMed] [Google Scholar]
- 16.Zieman SJ. Melenovsky V. Clattenburg L, et al. Advanced glycation endproduct crosslink breaker (alagebrium) improves endothelial function in patients with isolated systolic hypertension. J Hypertens. 2007;25:577–583. doi: 10.1097/HJH.0b013e328013e7dd. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.