Abstract
Background/Objectives
Advance Care Planning (ACP) allows patients to state preferences for their end of life care but these preferences are frequently ignored. Following a Patient-Centered ACP interview (PC-ACP), patients’ preferences were compared to care received at end of life.
Design
A randomized controlled trial was conducted with patients with Congestive Heart Failure or End-stage Renal Disease and their surrogates who were randomized to receive either PC-ACP or usual care.
Setting
Two centers in Wisconsin with associated clinics/dialysis units provided patients.
Participants
Of the 313 patients and their surrogates who completed entry data, 110 died.
Intervention
During PC-ACP the trained facilitator assessed the patient and surrogate understanding of and experiences with the illness, provided information about disease-specific treatment options and their benefits and burden, assisted in documentation of patient treatment preferences, and assisted the surrogates in understanding the patient’s preferences and their role.
Measurements
Preferences were documented and then compared to the care received at end of life determined by surrogate interviews or medical charts.
Results
Patients (74%) frequently continued to make their own decisions about care to the end. The experimental group had fewer (1/62) but not significantly so cases where the patients could not get their wishes met about CPR than control (6/48). Significantly more experimental patients withdrew from dialysis than control.
Conclusions
Patients and their surrogates were generally willing to discuss preferences with a trained facilitator. Most patients received the care they desired at end of life or altered their preferences to be in accord with the care they could receive. A larger sample with surrogate decision makers is needed to detect significance.
Keywords: Advance Care Planning, End-of-life care, Chronic illness
INTRODUCTION
While advance care planning is strongly recommended and is helpful to family members1, research on patient preferences and the care received at the end of life have revealed a number of issues. Mismatches between preferences and care have been documented2. Patients or caregivers may not be ready to have advance care planning discussions3. As a person’s health changes, preferences may change4, 5 and some will have a greater acceptance of life-prolonging treatments6.
In this paper, we report choices for end-of-life care expressed during a patient-centered advance care planning (PC-ACP) intervention in patients with end-stage congestive heart failure (CHF) and renal disease (ESRD). Previously, we reported that the surrogate had a significantly better understanding of patient preferences following the intervention than those who received usual care7. The aims of this study were to: 1) identify patient choices for care in situations that frequently occur using Patient-Centered Advance Care Planning (PC-ACP) compared to usual care, and 2) for those patients who died, assess whether their end of life care was in accord with their choices stated on study intake.
METHOD
The study was approved by the Institutional Review Board of the University of Wisconsin-Madison, Gundersen Clinic, Ltd., as well as the IRBs of all the cooperating sites. The design was a randomized, stratified (by setting and disease), post-test only control group design.
Settings
The study was conducted at two centers in Wisconsin. The LaCrosse center was headquartered at Gundersen Lutheran Health System and recruited CHF patients from an outpatient, multispecialty clinic, and ESRD patients from two nephrology clinic/dialysis units at Gundersen Lutheran and Franciscan Skemp Healthcare. The Madison center recruited CHF patients from cardiac rehabilitation and CHF clinics at UW Health and from Aurora St. Luke’s in Milwaukee; ESRD patients were recruited from two dialysis clinics affiliated with St. Mary’s Hospital Medical Center in Madison, WI.
Participants
The patient and their surrogate healthcare decision maker were recruited as a pair. Eligible patients had a diagnosis of CHF or ESRD, were receiving medical care, and had clinical symptoms that indicated a risk of serious complication or death in the next two years. Patients with CHF had a New York Heart Association classification of II, III, or IV. Patients with ESRD had a serum albumin concentration less than 3.7 g/dL and a serious comorbidity.
Clinic staff, trained by the research staff, screened for eligible patients. If patients agreed, research staff explained the study, determined if there was a willing surrogate decision-maker, and obtained informed consent.
Measures
Pre-measures were demographic data, functional status (both activities of daily living (ADL) and instrumental activities of daily living (IADL), and presence of advance directives (ADs). An estimate of a 90% chance of the patient being alive in 6-12 months if care stayed the same was obtained from both patient and surrogate. Then pairs of eligible patients and surrogates were randomized to the experimental PC-ACP group or the control group using the sealed-envelope method.
The Statement of Treatment Preferences (STP) developed by Briggs and Hammes8 was used to document the treatment preferences of patients in four situations. The STP includes four situations, (1) Facing a prolonged hospital stay, requiring ongoing medical interventions AND chance of survival is low (e.g. <5%); (2) a good chance of survival, facing permanent, severe functional impairment (could not walk, talk) that would require 24 hour nursing care; and (3) a good chance of survival; facing permanent, severe cognitive impairment (did not know who I was or who I was with) that would require 24 hours nursing care and cardiopulmonary arrest. In the first three situations, patients chose from three options, “to continue all treatment”, “to stop all treatment to prolong my life”, and “don’t know”. In the fourth situation, cardiopulmonary arrest, the patient chose “do not attempt CPR” or “attempt resuscitation”. The Statement of Treatment Preferences was completed upon entry into the study for control pairs and following the PC-ACP for the experimental group.
For those patients who died, surrogates were interviewed by phone and medical records from the site of death were obtained to determine; 1) whether the patient was decisional at the end of life, 2) whether the patient’s preferences had changed and 3) what care was received in the days prior to death.
USUAL CARE
For all sites, usual care included standard advance directives (AD) counseling, assessment of an AD on admission to the organization, and/or questions if they would like more information.
INTERVENTION – PC-ACP
The PC-ACP is an interview with patient and a surrogate, delivered by a trained facilitator and lasting 1 to 1 ½ hours. The interview was derived from previous work by Briggs and Hammes8. PC-ACP is designed to assess the patient and surrogate understanding of and experiences with the illness, provide information about disease-specific treatment options and their benefits and burden, to assist in documentation of patient treatment preferences, and to assist the surrogate in understanding the patient’s preferences and prepare surrogates to make decisions that honor those preferences. The PC-ACP ends with the documentation of patient preferences for care using the Statement of Treatment Preferences form (STP).
The interview is theoretically supported by the representational approach to patient education9 described in detail elsewhere 10. The interview is organized by five stages: 1) Assessment of the patient’s understanding of his or her current medical condition, prognosis and potential future medical events. 2) Exploring misconceptions about future medical decision-making. 3) Reviewing the rationale for future medical decisions. 4) Helping the patient understand potential complications and possible future treatment decisions using the STP. The facilitator may introduce replacement information to correct misconceptions. 5) Facilitator summarization of the conclusions reached, the need for future discussions as situations and preferences change, and the value of the discussion for the patient and surrogate.
PC-ACP Facilitation Training
The PC-ACP facilitators were trained in the content, techniques, and delivery of the study intervention and were observed during the study. The selected nurses, social workers and chaplains received reading materials, classes with return demonstration, video-taping, competency evaluation and feedback.
Data analysis
Kappa statistics were used to estimate odds of patient choices. The choice to continue treatment or “don’t know” was used as the index value and the odds ratios of the choice “to stop treatment” were calculated. Logistic regression was used to determine the relationship of demographic variables such as age, education and site for each situation presented to patients and surrogates. The models were then expanded to assess possible interactions between treatment and select covariates of patient age, disease, patient functional status, patient educational level, and site.
To determine whether a patient received care at the end of life in accord with the patient’s wishes, as expressed on the STP, the data collected after death was reviewed. There were four instances where there was neither surrogate nor medical record information. Two reviewers blinded to group determined what treatment was received by the patient. That treatment was compared to the patient preferences concerning low chance of survival and cardiopulmonary arrest on the STP If the treatment differed from the patient preference on the STP, two blinded reviewers reviewed the data to determine if patient preferences changed. If preferences did not change, the reviewers described the reason care was not in accord with patient wishes. There was 90% agreement between the two reviewers. Cases in dispute were discussed by the reviewers and consensus reached in about 50% of these cases. For 14 cases in which, the reviewers could not determine the care received or there was still a discrepancy, an independent expert, a Palliative Care Practitioner with research and clinical experience, reviewed the data. The independent reviewer referred six cases to an expert interdisciplinary panel (clinicians and faculty with expertise in gerontology and palliative care) which made the final determinations of what care was received.
RESULTS
Sample
There were 338 patients who were enrolled in the study; of these, 313 patients and their surrogates completed data collection following the intervention. Those patients or surrogates who did not complete the study withdrew (n=23), or died before the completion of the intervention (n=2). Of those completing, 134 were CHF patients from the LaCrosse Center and 45 from the Madison Center. ESRD patients were from LaCrosse (n=98) and from Madison (n=36). The ADL and IADL scores for experimental and control patients were remarkably similar across disease groups. Surrogates were on the average in their late 50’s, predominately female, married and Protestant. About 65% of the patients thought they had a 90% chance of being alive in 6-12 months if care stayed the same but only 56% to 63% of the surrogates thought so.
Of those 313 patients, 110 died before the end of the study. The demographics of the decedents were similar to those in the full sample. Control (n=48) and Experimental (n=62) decedents were close to 70 years of age, and usually married, white, and Protestant.
Patient preferences
The patient preferences, whether to continue treatment in a low chance of survival or to attempt resuscitation or not, are presented in Table 1. There is a tendency for the experimental group to choose less aggressive care than control but the difference is not statistically significant. Variables that might influence patient choices on the Statement of Treatment Preferences were examined with a logit regression for these two preferences. ADL, IADL, study site, education, and interaction of the intervention with disease and site were not significant in the logit regression model.
Table 1.
Choices Of Patients On Statement Of Treatment Preferences If A Low Chance Of Survival Was Predicted And For CPR
| Low chance of survival | Control n=153 | Intervention n=160 | ||||
|---|---|---|---|---|---|---|
| Renal n=64 | CHF n=89 | Combined | Renal n=70 | CHF n=88 | Combined | |
| Continue all treatment | 17 (26.6%) |
15 (16.9%) |
32 (20.9%) |
15 (21.4%) |
10 (11.4%) |
25 (15.6%) |
| Stop all treatment | 35 (54.7%) |
65 (73.0%) |
100 (65.4%) |
51 (72.9%) |
71 (80.7%) |
122 (76.3%) |
| Don’t know | 12 (18.7%) |
9 (10.1%) |
21 (13.7%) |
4 (5.7%) |
7 (7.9%) |
11 (6.9%) |
| CPR | Control n=153 | Intervention n=160 | ||||
| Renal n=64 |
CHF n=88 |
Combined n=152 |
Renal n=70 |
CHF n=88 |
Combined n=158 |
|
| Attempt resuscitation | 34 (53.1%) |
40 (45.5%) |
74 (48.7%) |
23 (32.8%) |
36 (40.9%) |
59 (37.3%) |
| Do not attempt resuscitation | 12 (18.8%) |
22 (25.0%) |
34 (22.4%) |
19 (27.1%) |
19 (21.6%) |
38 (24.0%) |
| Do not attempt resuscitation if the treating physician believes the chance of surviving is low | 18 (28.1%) |
26 (29.5%) |
44 (28.9%) |
27 (38.6%) |
34 (38.6%) |
61 (38.6%) |
Post Death Data
Evaluation of concordance of patient preferences and care at EOL
Although the intervention was used to support surrogate decision making as well as clarify patient wishes, 74% (n=81), of the patients made their own decisions until death and therefore received care in accord with their wishes. The remainder of the patients (n=29) required further assessment to determine effect of the intervention. Days from entry into the study to death ranged from 19-997 (control) and 5-1010 (intervention). The mean days to death did not significantly differ between control (M=362.25, SD 288.42) and experimental (M=388.84, SD 255.69) patients.
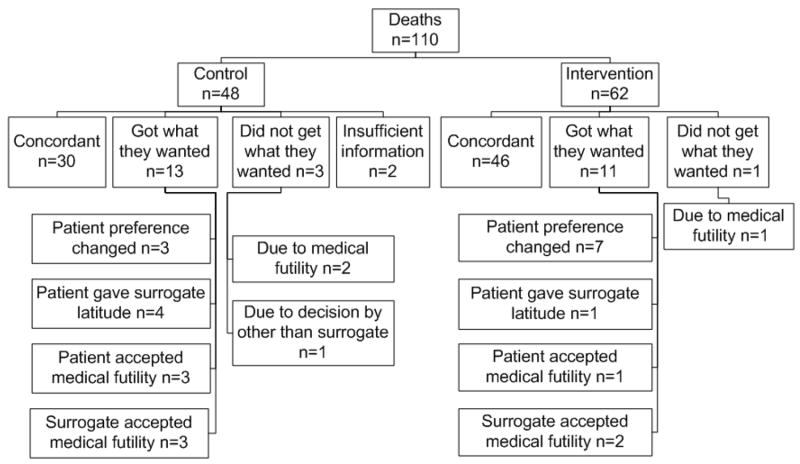
In the situation of a low chance of survival the patient’s care was concordant with initial wishes or a change by the patient or surrogate (because of the patient’s condition) yielded concordance in most cases (See Figure 1). The intervention group’s initial choices matched the care they received for 46 of the 62 patients (74.1%) and for the control group in 30 of 48 patients (62%). The intervention group had only one case where the patient’s wishes were not met because of futility. The control group had three cases.
Figure 1.
Patient outcomes compared to patient choices related to low chance of survival
In the situation of cardiopulmonary arrest, 27 of 62 experimental patients (43.5%) and 17 of 48 control patients (35.4%) had CPR outcomes matching initial preferences. Most received the care they desired or had altered their preferences over time. Almost 1/3 (33/110) of the patients changed their mind about their preferences for CPR. In the experimental group only one patient did not have his preferences matched, while the control group had 6 patients whose preferences were not matched (See Figure 2). Because of sample sizes, these differences were not significant.
Figure 2.
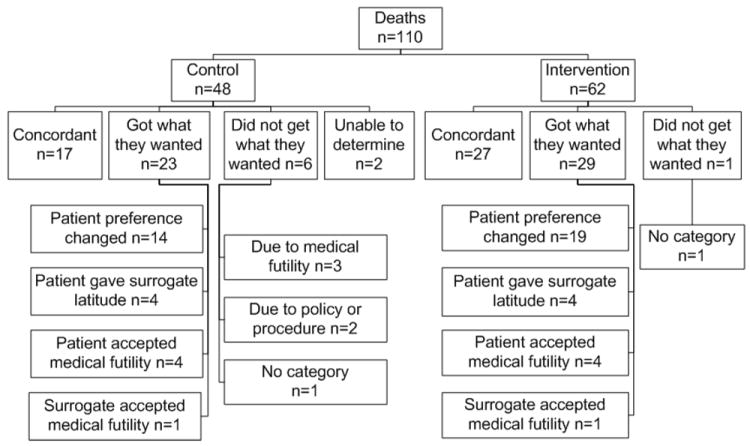
Patient outcomes compared to patient choices related to Cardiopulmonary resuscitation
For the ESRD patients, there was a significant difference between groups in that more experimental patients (37.7%) chose to withdraw from dialysis than control (17%). This choice was not specifically addressed in the interview, although the purpose of the interview was clarifying preferences and facilitating patient decision making.
DISCUSSION
We attempted to set up a study in which PC-ACP was evaluated to assess whether patients were more likely to receive the end-of-life care they desired assisted by surrogate decision makers. The potential impact of the results was reduced since we had anticipated more deaths during the study period (198 versus the 110 seen). We also anticipated about 50% of the patients would make their own decisions versus the 74% in the study
Other research has demonstrated that a person’s choices for end-of life treatment may change over time. If the patient is not able to express their modified wishes near the time of death, the healthcare team usually relies on a surrogate decision-maker. At the end of our intervention the need for the patient and surrogate to continue to discuss the issues was mentioned. During the post-death interview some of the experimental surrogates described the changes communicated by the patient in subsequent discussions.
One serious concern is whether or not advance care planning such as that offered in this intervention will steer patients toward less intervention as they near the end of their lives. The results of this study indicate a trend towards intervention patients choosing less intervention-intensive care, but not statistically so. Also, there was no difference in length of life between groups, suggesting that the choices following ACP alone do not shorten life. There was a significantly higher number of intervention ESRD patients choosing to withdraw from dialysis. Perhaps receiving dialysis is seen as a default position unless the ability to choose interventions is explored.
Limitations
Generalizability is limited since only one state was involved, and the sample was mostly Caucasian, similar to residents of Wisconsin. Only two chronic illnesses were used; however, these are commonly occurring. The results may not generalize to other illnesses or to younger individuals.
The intervention was given once without a booster. Although an assessment for a change in preference was abandoned early in the study, it might have functioned as a booster. Perhaps a periodic assessment by the primary care provider would strengthen the effect of the intervention. The variable time from intervention to death was unavoidable but may have weakened effectiveness.
There were a number of issues affecting the amount and quality of the data obtained after the patient’s death. One issue was that was that the surrogates did not see themselves as making decisions. They did not recognize that their support of the patient choices was a decision. There were also issues in obtaining medical records from non-study sites. Some patients did not have a medical record since they died at home. Others were in institutions reluctant to release records.
Clinical and Research Implications
Patients and surrogates were usually appreciative to have such discussions. They asked why no one had raised these issues earlier. Reluctance of health professionals to hold these sensitive discussions should be reduced with training. Routinizing the discussions requires the designation of an individual to hold the discussions, allowing time, and periodically checking to see if preferences have changed.
Additional research to describe the factors that influence a patient’s end-of-life care choices is warranted. Future research will need to assess the impact of a booster for the initial discussion. Also the impact of the dissemination of the preferences beyond just the immediate surrogate could be beneficial.
Since many patients continued to make their own decisions, the process of advance care planning needs to not just prepare the surrogate but also the patient to make these future decisions. When we are doing disease-specific planning, we are really helping prepare both the surrogate and the patient to face future decisions in a more informed and prepared way.
Acknowledgments
This study was supported by 1 R01 HS013374-01 from the Agency of Health care Research and Quality awarded to Dr. Kirchhoff. Dr. Hammes and Ms. Briggs are employed by the Gundersen Lutheran Medical Foundation, Inc. which owns the rights to the Respecting Choices® program. Dr. Kehl was supported by grant 1UL1RR025011 from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources, National Institutes of Health during the final year of this project. Drs. Kirchhoff, Kehl and Brown at the Madison site were responsible for data management and analysis.
Authors, Karin T. Kirchhoff, Bernard J. Hammes, and Linda A. Briggs are asked to speak on this topic, and may have other grants funded as for this study. Hammes and Briggs do training workshops on the intervention which is housed in their institution.
Sponsor’s Role: None
Footnotes
Author Contributions: All authors participated in manuscript preparation and submission.
Conflict of Interest
Dr. Brown has no conflicts of interest.
References
- 1.Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cosgriff JA, Pisani M, Bradley EH, et al. The association between treatment preferences and trajectories of care at the end-of-life. J Gen Intern Med. 2007;22:1566–1571. doi: 10.1007/s11606-007-0362-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fried TR, O’Leary JR. Using the experiences of bereaved caregivers to inform patient- and caregiver-centered advance care planning. J Gen Intern Med. 2008;23:1602–1607. doi: 10.1007/s11606-008-0748-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danis M, Garrett J, Harris R, et al. Stability of choices about life-sustaining treatments. Ann Intern Med. 1994;120:567–573. doi: 10.7326/0003-4819-120-7-199404010-00006. [DOI] [PubMed] [Google Scholar]
- 5.Lynn J, Arkes HR, Stevens M, et al. Rethinking fundamental assumptions: SUPPORT’s implications for future reform. Study to understand prognoses and preferences and risks of treatment. J Am Geriatr Soc. 2000;48:S214–221. doi: 10.1111/j.1532-5415.2000.tb03135.x. [DOI] [PubMed] [Google Scholar]
- 6.Fried TR, Byers AL, Gallo WT, et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med. 2006;166:890–895. doi: 10.1001/archinte.166.8.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirchhoff KT, Hammes B, Kehl KA, et al. Impact of a disease-specific planning intervention on surrogate understanding of patient goals for future medical treatment. J Am Geriatr Soc. 2010;58:1233–1240. doi: 10.1111/j.1532-5415.2010.02760.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Briggs L, Hammes B. Disease specific - Patient centered advance care planning (DS-ACP) manual. La Crosse, WI: Gundersen Lutheran Medical Foundation, Inc., 2002; 2008. [Google Scholar]
- 9.Donovan HS, Ward S. A representational approach to patient education. J Nurs Scholarsh. 2001;33:211–216. doi: 10.1111/j.1547-5069.2001.00211.x. [DOI] [PubMed] [Google Scholar]
- 10.Briggs L. Shifting the focus of advance care planning: Using an in-depth interview to build and strengthen relationships. J Palliat Med. 2004;7:341–349. doi: 10.1089/109662104773709503. [DOI] [PubMed] [Google Scholar]