Abstract
Biliary leakage is a known complication after biliary surgery. In this report, we describe an uncommon treatment of a common biliary complication, wherein we used percutaneous transhepatic injection of N-butyl cyanoacrylate (NBCA) to treat a biliary leak in an 83-year-old patient.
Keywords: Biliary drainage, biliary leakage, N-butyl cyanoacrylate, percutaneous embolization, transhepatic embolization
Introduction
Bile leakage is a well-known and dreaded complication of open or laparoscopic cholecystectomy (LC), major liver surgery, and blunt abdominal injury.[1] With the advent of treatment by endoscopic sphincterotomy and drainage using either an endoprosthesis or nasobiliary catheter, surgery is now avoided in the majority of cases.[2–7] However, up to 10% of patients with biliary leaks after LC do not respond to initial endoscopic therapy.[8] Those with more severe ductal injury and large leaks are especially likely to require surgery.[9] In the past few years, some alternatives to surgery have been used to control bile leakage, such as injection of fibrin and ethanol, but these have their own problems and complications.[10,11] Recently, N-butyl-2-cyanoacrylate (NBCA) has being used with this intent. NBCA is a tissue glue monomer that instantly polymerizes and solidifies upon contact with body fluids at neutral pH.[12] This substance is routinely used in plastic surgery, radiology, neurosurgery, and general surgery and was first used for obliteration of bleeding gastric varices.[12] NBCA has recently been approved in Europe for endoscopic hemostasis and sealing of fistulae (Glubran 2™, GEM, Viareggio, Italy).[13] In the literature, only six cases have been reported of biliary leakage treated percutaneously with NBCA.[14,15] We would like to discuss one patient where we used NBCA to seal a biliary leakage in a patient with a carcinoma of the papilla of Vater who did not respond to standard endoscopic drainage methods.
Case Report
An 83-year-old male with a carcinoma of the papilla of Vater was treated with a 10F polyethylene stenting (Olympus, Mt Waverley, Australia) of the main biliary duct during endoscopic retrograde cholangiopancreatography. When a stent release was attempted, it was not completely released and remained folded; it was not possible to remove it endoscopically. So a percutaneous transhepatic cholangiogram was performed through the puncture of right intrahepatic biliary system. It revealed an intrahepatic biliary dilatation of both distal systems. An external–internal drainage was positioned. After several cholangiogram controls, stent positioned by endoscopists was removed and two new covered stents (9 × 80 mm) were deployed (Smart, Cordis; Miami Lakes, FL). An internal drainage was maintained. A control cholangiogram revealed bile leakage from the VI–VII segmental biliary duct, communicating with the main biliary tree. The leakage probably originated from the posterior ducts, and it was caused from percutaneous puncture. Conservative treatment was attempted, with maintenance of internal drainage for 15 days, but the leakage associated with a biloma persisted internally [Figure 1]. The patient had pain, fever, and elevated inflammatory indices. Using a different percutaneous access, through the right lobe itself, a superselective approach to the site of the leakage was obtained, using another biliary radicle, which was dilated enough. A 2.8F microcatheter (Progreat™; Terumo, Tokyo, Japan) was used using a 5F catheter (Cobra, Cordis, Miami Lakes, FL) and an hydrophilic guidewire (Terumo, Tokyo, Japan). Embolization was performed with three fibered 0.018-inch platinum micro-coils (VortX™; Boston Scientific) with nominal configured diameters of 2 mm × 3 mm, pushed with saline solution injection. The leakage was only slightly reduced. The microcatheter was preliminary flushed by a nonionic dextrose solution and then the tissue adhesive agent NBCA (Glubran 2™, GEM), mixed with iodized oil (Lipiodol™; Guebert, Aulnay-sous-Bois, France) in a ratio of 1:2 for opacification, was injected [Figure 2]. A total of 2 ml of NBCA was administered. This solution completely filled the leakage tract within a few seconds. A postprocedural cholangiogram confirmed the absence of any complication and the disappearance of the leakage [Figure 3]. The patient was discharged after 1 week with an 8F internal–external biliary drain open, allowing bile drainage and permitting easy access for repeat radiologic follow-up. At the last follow-up visit (3 months after the procedure), the drainage was removed, and no evidence of recurrence was noticed [Figure 4], and also biloma was reabsorbed.
Figure 1.

Cholangiogram shows biliary leakage (arrows) after conservative treatment
Figure 2.
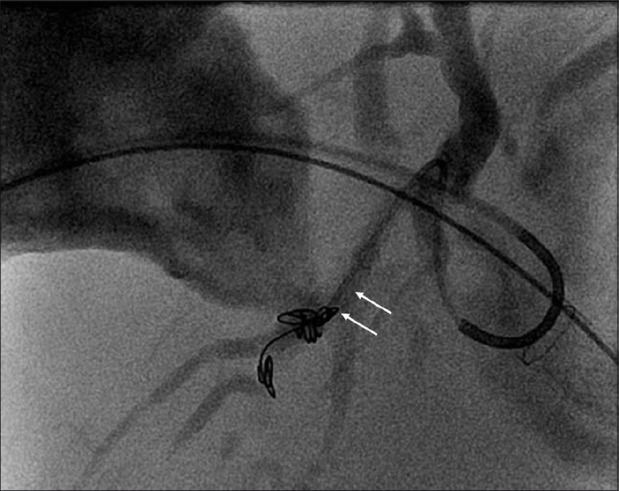
Superselective embolization of biliary leakage with NBCA (arrows)
Figure 3.

Postprocedural cholangiogram shows the disappearance of the leakage (arrows)
Figure 4.

Cholangiogram performed after 3 months shows the absence of recurrence. The drainage was removed
Informed consent was obtained before each procedure. Before any percutaneous procedure, the patient receives intravenous antibiotic, 1.5 g cefuroxime (Cefurex™, Salus Researches S.p.A, Italy), as a one-time dose.
Discussion
Biliary leakage occurs most frequently after hepatobiliary surgery, especially open or LC, but is also seen after liver resection or liver transplantation, after endoscopic or interventional radiological maneuvers, or after severe hepatic trauma.[14,16,17] Many of these biliary tract injuries may go unrecognized at the time of surgery and have a delayed presentation.[18] Nonoperative management of these patients can be successful, and interventional radiology has a major role to play in delineating the anatomy of the injury and controlling ongoing bile duct injury.[18]
In the literature, there is a description of the use of fibrin glue for the treatment of communication between an abscess cavity and an aberrant posterior segment hepatic duct that was injured in a LC; however, the bile discharge in that case was not reduced and the cavity and fistula could not be closed.[19]
There are three main materials that have been studied as potential sealants of the biliary tract: fibrin,[10] ethanol, and NBCA. Matsumoto et al.[20] reported a case in which multiple ethanol injections were performed to close a biliary-cutaneous fistula from an isolated small bile duct of the left caudate lobe after resection of the right caudate lobe for hepatocellular carcinoma. Sadakari et al.[21] described a case of intractable bile leakage after hepatectomy, which was successfully treated by percutaneous transhepatic portal embolization with ethanol. Ethanol is not advised when there is communication with the remainder of the biliary tree[11] as there may be seepage of the ethanol into the biliary tree, which could lead to irreversible damage.[22] Flushing, fever, leukocytosis, mild increases of aminotransferase levels, and systemic hypotension may occur with ethanol injection.[11,21,22] Ethanol injection may also cause necrosis of the bile duct epithelium.[21]
NCBA, a low-viscosity monomer used as tissue adhesive glue, is a promising solution to biliary chemical embolization. When in contact with organic fluids (i.e., bile), this substance undergoes rapid polymerization and solidification. It provides a permanent embolization and hence, due to an inflammatory tissue response, a long-term occlusion in vessels of various size resulting in vessel thrombosis or tissue atrophy.[14,15,17]
Vu et al.,[14] based on their experience with six patients, suggested the placement of a coil at the neck of the fistula and subsequent administration of NBCA from an external approach as the most effective way to prevent recurrence of biliary fistulas.
Gorich et al.[16] described their experience of percutaneous embolization of bile duct fistulas with Ethibloc™ (Ethicon, Somerville, NJ) and isobutyl-2-cyanoacrylate in four patients. They observed unintentional spillage of isobutyl-2-cyanoacrylate in the bile duct in one of the four patients. They also reported that a coaxial catheter became glued to the bile duct wall in one patient after an isobutyl-2-cyanoacrylate embolization.[16]
If the patient is unable to undergo percutaneous embolization for the biliary leak, continued percutaneous drainage is also an option. However, this too is not without complications. Bleeding episodes can occur after catheter removal and metabolic acidosis may develop secondary to continued bile loss from the drainage catheter.[23]
We could find only two reports in literature describing biliary leakage treated with percutaneous insertion of NBCA: the series of patients (six patients) treated by Vu et al.[14] and a case report by Lauterio et al.[15] The success of the procedure in our patient is further evidence of the efficacy and safety of using percutaneous insertion of NBCA glue in biliary injuries. Further studies are needed to confirm the efficacy and safety of this approach and to determine whether it can reduce hospital stay and treatment costs.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Albasini JL, Aledo VS, Dexter SP, Marton J, Martin IG, McMahon MJ. Bile leakage following laparoscopic cholecystectomy. Surg Endosc. 1995;9:1274–8. doi: 10.1007/BF00190158. [DOI] [PubMed] [Google Scholar]
- 2.O’Rahilly S, Duignan JP, Lennon JR, O’Malley E. Successful treatment of a post-operative external biliary fistula by endoscopic papillotomy. Endoscopy. 1983;15:68–9. doi: 10.1055/s-2007-1021469. [DOI] [PubMed] [Google Scholar]
- 3.Burmeister W, Koppen MO, Wurbs D. Treatment of a biliocutaneous fistula by endoscopic insertion of a nasobiliary tube. Gastrointest Endosc. 1985;31:279–81. doi: 10.1016/s0016-5107(85)72185-2. [DOI] [PubMed] [Google Scholar]
- 4.Sauerbruch T, Weinzierl M, Holl J, Pratschke E. Treatment of postoperative bile fistulas by internal endoscopic biliary drainage. Gastroenterology. 1986;90:1998–2003. doi: 10.1016/0016-5085(86)90273-8. [DOI] [PubMed] [Google Scholar]
- 5.Kozarek RA, Traverso LW. Endoscopic stent placement for cystic duct leak after laparoscopic cholecystectomy. Gastrointest Endosc. 1991;37:71–3. doi: 10.1016/s0016-5107(91)70628-7. [DOI] [PubMed] [Google Scholar]
- 6.Chow S, Bosco JJ, Heiss FW, Shea JA, Qaseem T, Howell D. Successful treatment of post-cholecystectomy bile leaks using nasobiliary tube drainage and sphincterotomy. Am J Gastroenterol. 1997;92:1839–43. [PubMed] [Google Scholar]
- 7.Sugiyama M, Atomi Y, Matsuoka T, Yamaguchi Y. Endoscopic biliary stenting for treatment of persistent biliary fistula after blunt hepatic injury. Gastrointest Endosc. 2000;51:42–4. doi: 10.1016/s0016-5107(00)70385-3. [DOI] [PubMed] [Google Scholar]
- 8.Ryan ME, Geenen JE, Lehman GA, Aliperti G, Freeman ML, Silverman WB, et al. Endoscopic intervention for biliary leaks after laparoscopic cholecystectomy: A multicenter review. Gastrointest Endosc. 1998;47:261–6. doi: 10.1016/s0016-5107(98)70324-4. [DOI] [PubMed] [Google Scholar]
- 9.Bergman JJ, van den Brink GR, Rauws EA, de Wit L, Obertop H, Huibregtse K, et al. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut. 1996;38:141–7. doi: 10.1136/gut.38.1.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brady AP, Malone DE, Deignan RW, O’Donovan N, McGrath FP. Fibrin sealant in interventional radiology: A preliminary evaluation. Radiology. 1995;196:573–8. doi: 10.1148/radiology.196.2.7617880. [DOI] [PubMed] [Google Scholar]
- 11.Kusano T, Kida H, Nishiwaki Y, Ikematsu Y, Goto K, Kuroda H, et al. Percutaneous sclerotherapy for intractable external biliary fistula after hepatectomy. Int Surg. 2003;88:72–5. [PubMed] [Google Scholar]
- 12.Soehendra N, Nam VC, Grimm H, Kempeneers I. Endoscopic obliteration of large esophagogastric varices with bucrylate. Endoscopy. 1986;18:25–6. doi: 10.1055/s-2007-1013014. [DOI] [PubMed] [Google Scholar]
- 13.Seewald S, Groth S, Sriram PV, Xikun H, Akaraviputh T, Mendoza G, et al. Endoscopic treatment with biliary leakage with n-butyl-2 cyanoacrylate. Gastrointest Endosc. 2002;56:916–9. doi: 10.1067/mge.2002.129873. [DOI] [PubMed] [Google Scholar]
- 14.Vu DN, Strub WM, Nguyen PM. Biliary duct ablation with n-butyl cyanoacrylate. J Vasc Interv Radiol. 2006;17:63–9. doi: 10.1097/01.RVI.0000195399.68445.DD. [DOI] [PubMed] [Google Scholar]
- 15.Lauterio A, Slim A, Aseni P, Giacomoni A, Di Sandro S, Corso R, et al. Percutaneous transhepatic bile duct ablation with n-butyl cyanoacrylate in the treatment of a biliary complication after split liver transplantation. J Transplant. 2009;2009:824803. doi: 10.1155/2009/824803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Görich J, Rilinger N, Sokiranski R, Siech M, Vogel J, Wikström M, et al. Percutaneous transhepatic embolization of bile duct fistulas. J Vasc Interv Radiol. 1996;7:435–8. doi: 10.1016/s1051-0443(96)72884-1. [DOI] [PubMed] [Google Scholar]
- 17.Seewald S, Groth S, Sriram PV, Xikun H, Akaraviputh T, Mendoza G, et al. Endoscopic treatment of biliary leakage with n-butyl-2 cyanoacrylate. Gastrointest Endosc. 2002;56:916–9. doi: 10.1067/mge.2002.129873. [DOI] [PubMed] [Google Scholar]
- 18.Lichtenstein S, Moorman DW, Malatesta JQ, Martin MF. The role of hepatic resection in the management of bile duct injuries following laparoscopic cholecystectomy. Am Surg. 2000;66:372–6. discussion 377. [PubMed] [Google Scholar]
- 19.Ohtsuka T, Chijiiwa K, Yamaguchi K, Akashi Y, Matsunaga H, Miyoshi A. Posterior hepatic duct injury during laparoscopic cholecystectomy finally necessitating hepatic resection: Case Report. JSLS. 1999;3:323–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Matsumoto T, Iwaki K, Hagino Y, Kawano K, Kitano S, Tomonari K, et al. Ethanol injection therapy of an isolated bile duct associated with a biliary cutaneous fistula. J Gastroenterol Hepatol. 2002;17:807–10. doi: 10.1046/j.1440-1746.2002.02661.x. [DOI] [PubMed] [Google Scholar]
- 21.Sadakari Y, Miyoshi A, Ohtsuka T, Kohya N, Takahashi T, Matsumoto K, et al. Percutaneous transhepatic portal embolization for persistent bile leakage after hepatic resection: Report of a case. Surg Today. 2008;38:668–71. doi: 10.1007/s00595-007-3667-5. [DOI] [PubMed] [Google Scholar]
- 22.Kyokane T, Nagino M, Sano T, Nimura Y. Ethanol ablation for segmental bile duct leakage after hepatobiliary resection. Surgery. 2002;131:111–3. doi: 10.1067/msy.2002.118711. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman SL, Kadir S, Mitchell SE, Chang R, Kinnison ML, Cameron JL, et al. Percutaneous transhepatic biliary drainage for bile leaks and fistulas. AJR Am J Roentgenol. 1985;144:1055–8. doi: 10.2214/ajr.144.5.1055. [DOI] [PubMed] [Google Scholar]


