Abstract
Background:
The Ministry of Health in Jamaica recommends that cervical cancer screening be undergo by women 25-54 years old. The age range is based on international standards, but this is in need for revision based on the parish of St. Thomas.
Aims:
The study aimed to evaluate the perception and practice of Pap smear and the sexual practices of women in St. Thomas in order to aid policy.
Patients and Methods:
This is a cross-sectional descriptive study of 210 women (15-54 years) from St. Thomas, Jamaica.
Results:
Eighty eight percent of the sample had done a Pap smear and 24% indicated that they did this at least once every 12 months. The Pap smear results revealed that 83.2% of the sample was normal and 11.5% of the participants knew that their Pap smear was abnormal. Eighty percent of those with abnormal Pap smear were aged between 20-35 years. Sixty percent indicated that they did not believe they were infected with any STDs, but the Pap smear results showed that 76.4% of them had STDs. Eighty-three percent of the sample indicated having one sexual partner; 22.1% indicated that they began having sex before 15 years; 71% began having sex at 15-20 years; 76% of the sample used a condom and 12% reported that they had never practiced safe sex.
Conclusion:
This study finds that the age interval for conducting Pap smear screening should be lowered to 20 years for women in the parish of St. Thomas, Jamaica.
Keywords: Pap smears, screening interval, sexual behavior, STDs, age of first sexual experience
Introduction
In 2007, life expectancy for females in Jamaica was 74 years, which was greater than that of females in low income countries (i.e. 58 years). This report highlights that there is a need to examine the health, healthy lifestyle practices and the perception of females in Jamaica. Statistics for Latin America and the Caribbean reveal the highest rates of stomach and cervical cancers in the world, with the highest recorded being in Venezuela, and Trinidad and Tobago[2]. Statistics for 2002 showed an incidence of almost 470,610 and of this number 233,375 deaths were due to cervical cancers in women around the globe, with 4 out of every 5 occurred in less developed countries[2]. Statistics on Jamaica for 1999 showed that 2,697 cancer-related deaths occurred in the nation, which represented 17.7% of all mortalities. The mortality rate for cancer of the cervix was 15.8 per 100,000 females, which was 6.6 times more than that for Caucasian females in the USA, and 2.8 times more than that for African-American females[3]. A recently conducted study by Ivey et al.[4] found that cancers were among the top five leading causes of mortality in the English and Dutch-speaking Caribbean between 1985 and 2000.
Recently a study conducted in Jamaica revealed that the prevalence of cancers in the island was 0.5%, an indication that overall cancer is not a public health problem in the nation compared to hypertension, diabetes mellitus and obesity[5]. However, when the cancer prevalence was disaggregated according to gender, 2.7 times more females in Jamaica self-reported being diagnosed with cancers compared to males. This suggests that cancer is a public health problem in Jamaica. Although the prevalence of self-reported cancers is outside of the 10 top leading health conditions in Jamaica[5], it is among the top 10 leading causes of mortality[6]. Statistics from the Planning Institute of Jamaica (PIOJ) and the Statistical Institute of Jamaica (STATIN)[7] show that the health care-seeking behaviour among females on average was 68.5% in 2007. Wilks et al.'s research for 2007/2008 found that the rate of cancer in Jamaicans aged 65-74 years was 2.1% which was 3.5 times more than in those aged 55-64 years, 1.2 times more than in those of 45-54 years, 7 times more than in those 35-44 years, and 21 times more than in those of 25-34 years. Concurrently, Wilks et al.'s also showed that 58.8% of Jamaican females aged 15-74 years had taken a blood pressure test in the last 6-month period, with people in the lower socio-economic status having the lowest health care-seeking behaviour among the social hierarchies (low, 44.2%; middle, 46.7%, and high, 55.2%). Cancer screening was missing from the statistics on health care-seeking behaviour among Jamaicans inWilks et al.'s study.
Cancer screening for cervical cancer aims to detect, treat and address malignant epithelial changes before any invasion takes place. This is carried out through a Pap smear, which is named after George Papanicolau who, along with Herbert Traut, described the use of the vaginal smear in a book published in 1943 and an atlas in 1954[8]. Almost 5% of cervical cancer mortality occurred in women under 35 years of age[9], and 41.8 per 100,000 deaths were owing to cervical cancer in Jamaica compared with 41.4 per 100,000 in Barbados[10]. According to PAHO[10], the afore-mentioned cervical cancer rates for Jamaica and Barbados are the highest in the Americas, suggesting the need for cancer screening in females in both Jamaica and Barbados. A study which used data for 3 decades (i.e. 1958-1987) found that of the total of 19,228 malignant neoplasms recorded for Kingston and St. Andrew, Jamaica, 20% were cervical neoplasms[11]. Another study for the period 1958-1970 revealed that carcinoma of the cervix accounted for 21% of all deaths in women caused by malignant neoplasms, and that the highest incidence of carcinoma of the cervix was found in older women[12]. Poverty, early age of sexual intercourse, smoking behaviour, high pregnancy rates among rural women and non-attendance for Pap smear examinations are evident in rural areas in Jamaica which may have contributed to the high rates of cervical cancer. Clearly the afore-mentioned statistics have highlighted the public health problem posed by cervical cancer in Jamaican females and so it is important to examine the data that exists on the subject in rural areas.
A very important question is “should cervical cancer screening be allowed for women ages 25 - 54 years or women in all age groups, including women with a history of genital warts, human papilloma virus, and annually by women with risk factors previously identified by a Pap smear?” The Ministry of Health in Jamaica recommends that a particular age cohort of women should undergo a Pap smear examination[13], but has the time come to lower the previous marker based on new information which has emerged in St. Thomas. Using a denominator of 1,787 to compute the prevalence of abnormalities may give true statistics of the issue, but the socio-psychological issues surrounding choices (or the lack of) are still unanswered by the statistics from the Clinics. The current study will not pre-determine those who should be screened for cervical cancer using Pap smears, but will examine knowledge, attitude and practices regarding cervical cancer and Pap smears among women ages 15-54 years in St. Thomas.
Patients and Methods
Sample and data
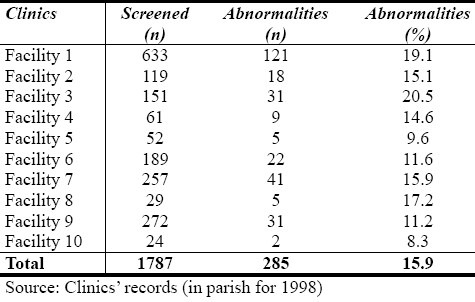
This study utilized data from a rural area in Jamaica, namely the parish of St. Thomas. It is bordered to the north by Portland, to the east by the Caribbean Sea and to the southeast by Kingston and St. Andrew (Figure 1). The parish covers 742.8 square kilometers, and its terrain is mostly flat. Statistics from STATIN estimated that the parish's population for 2007 was 93,887 people (i.e. 3.5% of Jamaica's human population), with 50.3% of the population being females. Using the estimate proportion of the Jamaican female population aged 15 through 54 years, 27,322 females (ages 15-54 years old) were estimated to dwell in the area in 2007, but the Public Health Department of the parish estimated that 15,018 females should undergo a Pap smear annually. In 1998, the records for the parish revealed that 12% did a Pap smear examination (n = 1,787) and 15.9% recorded abnormalities (Table 1).
Table 1.
Number of women screened by Pap smear and percent with abnormalities
This study was conducted in 2007. It is a cross-sectional descriptive study of 210 women (15-54 years) from the parish of St. Thomas in Jamaica. The parish has a population of 93,887 people, and is divided into four health districts. There are a total of 16 health centres in the parish - one Type 4; three Type 3; four Type 2 and eight Type 1 health centres; and one Type C hospital. The hospital provides surgical, maternity, medical and paediatric care, as well as psychiatry, laboratory and pharmacy services. The current study did a random sample of women from all the health centres in the parish. Every 10th woman who attended a 4-week clinic for post-natal and/or routine family planning visits in the afore-mentioned health centres was interviewed. The study was approved by the University of the West Indies Medical Faculty's Ethics Committee. All participants gave their written informed consent to actively participate in the study, and they were also informed that they could discontinue the process at any time convenient to them.
Using a sampling error of ± 3% and a confidence interval of 95%, the calculated sample for selection was 270 females. The sample was stratified by area of work, area of residence, and a table of random numbers was used to select the actual respondents, thereby facilitating independence of response. In cases where the selected person was not available a minimum of three call-back visits would be made to that person's place of work or home. On occasions when an individual was selected and she could not participate, no other person was used to replace the individual. In the Jamaican sampling, STATIN used a two-stage stratified random sampling design. Stage one is the selection of Primary Sampling Units (PSUs), and the second stage is a selection of dwellings (PIOJ, STATIN). A PSU is an electoral district (ED) or a combination of EDs. An ED comprises a minimum of 100 dwellings in a rural area and 150 dwellings in an urban area. The ED denotes an independent geographic locality sharing common boundaries with contiguous EDs. In another survey, the researchers used 36 persons per ED to calculate a representative sample of the nation[14,15]. St. Thomas has 4 EDs, which means that using 36 persons per ED the sample should be 144 respondents. In a recently conducted national survey, Wilks et al.[5] found that 30 people from each PSU could be used to constitute a nationally representative sample of Jamaica. Hence, based on previous surveys, the current study is sufficient to generalize on the parish because it is of representative sample size[14,15]. For this study, the sample was stratified by area of work, area of residence, and a Kish Random Selection Method of sub-sampling was used to select the actual respondents, thereby facilitating independence of response[16]. For this survey, the response rate was 77.0% (n = 208), of which 1.3% of the data were lost during data cleaning. This is in keeping with surveys conducted by PIOJ and STATIN[7], and Wilks et al.[15]. For the survey study 77.8% of the sample was female, which is similar to one by Wilks et al.[15] in which the female sample was 75.9%. Ministry of Health in Jamaica statistics revealed that more than 70% of females annually have been seeking medical care since 1990[17], and with PIOJ and STATIN[7] data revealing that an average of almost 70% of females have been seeking medical care since 1989 (for a 4-week period), it follows that a survey at hospitals and clinics over a 3-month period would be a good representation for most females in a particular geographic region in the island. No female was interviewed more than once, in order to ensure that there was no double-counting of information.
A 37-item self-administered questionnaire was used to collect the data. The instrument was sub-divided into general demographic profiles of the sample family history; health-seeking behaviour; perception of cervical cancer examination and choice of method in cervical cancer examination. Trained nurses or nurse guides were used to perform the Pap smear of those who volunteered to participate in this study. The results of the Pap smear were entered on a sheet of paper with a code to identify the participant, which was later transferred to the questionnaire completed by the corresponding females. The respondents were informed of the results of the Pap smear. After the code was verified as the result of the personal information for a particular individual who answered the questionnaire, the instrument was coded and entered by two independent individuals and then cross-referenced for accuracy. The identifiers on the questionnaires which corresponded to the Pap smear sheet were then removed from the questionnaire, and this, along with the Pap smear result sheets, destroyed, in order to protect the privacy of the respondents as well as to uphold the confidentiality of the research.
Test-retest reliability of the questionnaire was conducted about a month prior to the main study. The instrument was vetted by academics from the University of the West Indies, Mona, Jamaica. Then 10 respondents aged 20-60 years from the Well-Women Clinic held every Wednesday evening at the Glen Vincent Polyclinic were interviewed on two separate occasions, about seven days apart. The reliabilities were determined by the percentage of agreement. Modifications were made to the final instrument based on the recommendations, queries and issues raised by the participants in order to obtain clarity and conciseness of questions. The mean time for completing a questionnaire was 15 minutes (± 5).
Members of a graduate class were employed to collect data as field workers. All field workers were trained in interviewing techniques, customer service and data collection over a four-week period. The interviewers were on hand to assist respondents with reading or other difficulties such as sight issues. They were trained not to interpret or paraphrase questions. Questionnaires were also distributed by community health aides, and these individuals were trained in data collection and surveying etiquette of questionnaire data collection. The criteria for exclusion and inclusion were based on (1) being female, (2) 25-54 years of age, and (3) residing in the parish of St. Thomas.
Data analysis
The data were double entered using SPSS, verified and cleaned. The response rate was 77.0%, and 1.3% of the data was lost during cleaning. Data were stored, retrieved and analyzed, using SPSS for Windows (16.0) (SPSS Inc; Chicago, IL, USA). Percentages were used to provide background information on demographic characteristics of the sample, knowledge of cervical cancer and self-reported information on cancer screening. Chi-square tests were utilized to examine whether statistical associations existed between non-metric dependent and independent variables. A P-value of 5% (i.e. 95% confidence interval) was used to determine statistical associations between variables.
Results
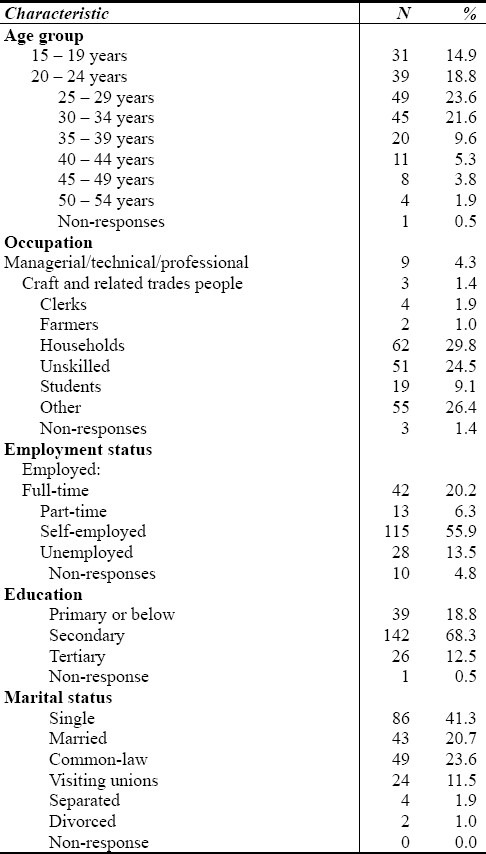
In examining the socio-demographic of the sample, the majority were in the 25-29 year age group; self-employed; acquired secondary education and were single women (Table 2). The mean gravidity for the sample was 2.9 (± 1.9). Only 0.5% of the sample indicated that they had never been pregnant; 24.3% had one pregnancy; 25.2% had two pregnancies; and 9% had at least 6 pregnancies. Seventy-three percent of the sample had 1-3 children; 7.5% had more than 6 children and 2% had not given birth. The mean number of children for the sample was 2.6 (± 1.8).
Table 2.
Demographic characteristics of sample
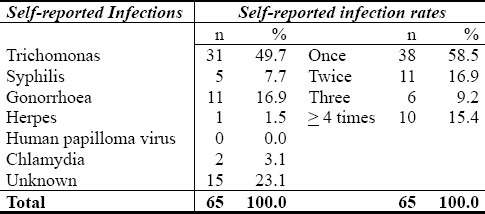
A little over two-thirds of the sample (67.4%) received knowledge about Pap smears from nurses in the Clinics (Table 3). Of the participants who undergo Pap smear, 83.2% of them had normal results (Table 4). The most common sexual transmitted disease (STD) among the participants was Trichomonas; 31.3% of the participants stated that they knew that they had STDs and provided information on the particular STDs and the frequencies of occurrence (Table 5). A cross-tabulation between the age cohort of first sexual intercourse and STD results showed a significant statistical association between the two variables (P = 0.037). Of those who indicated that their first sexual encounter was less than 15 years, 67.4% of them had STDs compared to 80.3% who began having sex at 15-20 years, and 100% of those who were 21 years or over.
Table 3.
Pap smear information
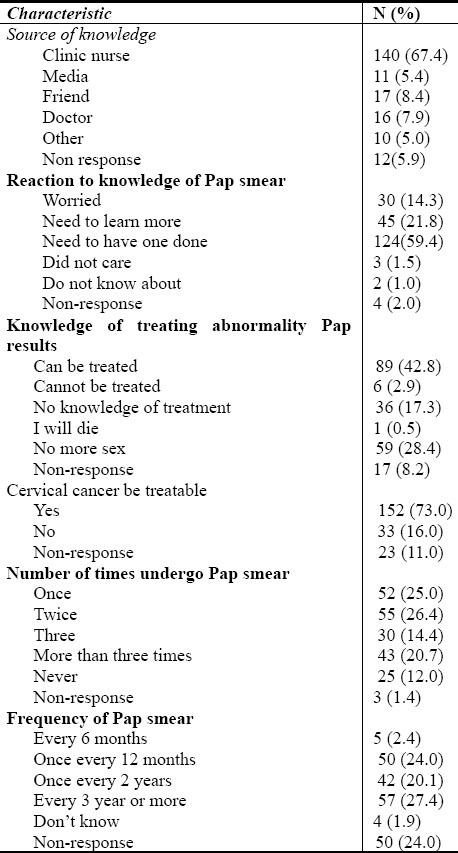
Table 4.
Pap smear results
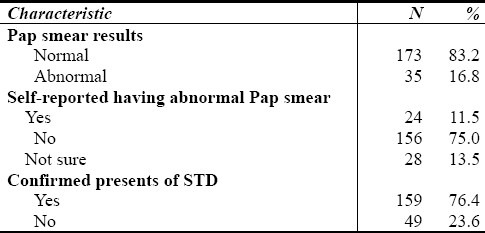
Table 5.
Self-reported infected with STDs and self-reported infection rate
Eighty-three percent of the sample indicated one sexual partner; 15.0% of the sample had more than one sexual partner, with 46.2% of those with more than one sexual partners having three or more; 22.1% indicated that they started having sex before 15 years; 71% started between 15 and 20 years; 76% used a condom; 3.4% professed abstinence; 9.6% indicated other and 11.1% did not respond to the question. In addition, 74% indicated that they practiced safe sex sometimes; 12% reported that they had never practiced safe sex; and only 11% of the sample indicated that they always practiced safe sex. Approximately one-tenth (10.3%) were informed about their diagnosis of STD(s) when they received the Pap smear results; 17.7% at the time when the results of a vaginal swab was given; 50.8% from a nurse and 14% from their partners. There were participants (18.3%) who indicated that their partner was having sexual relations with other persons, while 44.6% reported that they did not know.
Discussion
The current study goes beyond the provision of statistics on the prevalence rates of those who undergo a Pap smear, to critical issues which surround the lifestyle practices of women between 15 and 54 years of agein St. Thomas. The study revealed that the participants were housewives and unskilled women; unemployed; single and less than 30 years old. In addition, less than 1% had never been pregnant; 73% had 1-3 children; 11% always practiced safe sex; at most 93% had their first sexual encounter before age 21 years; 5.2% had more than one sexual partner; 76.4% had an STD; 17% had abnormal Pap smear results, and only 12% had never undergo a Pap smear. The results of this study which shows high prevalence of STDs, risky lifestyles and poor choices suggest that there is a public health problem in St. Thomas.
Statistics from PIOJ and STATIN[7] showed that 71.3% of poverty occurs in rural parishes, and there are marginally more females (8.0%) in poverty than males (7.2%). Furthermore, PIOJ and STATIN data reveal that between 3.0 and 3.4% rural residents reported an illness compared to peri-urban and urban residents. Unemployment and poverty as well as low socio-economic status account for the inappropriate choices of women in the parish. Marmot[18] reported that poverty explains the lower nutritional intake, poor physical milieu and, as Sen[19,20] indicated, poverty is more than material deprivation; it is also about social, political and economic deprivation and opportunities. It could be suggested that based on the findings of this study that the high unemployment of women (15-54 years), including housewives and unskilled female labour, makes them vulnerable and at the dictates of their male partners. Poverty retards people's choices, and this is evident among women ages 15-54 years in St. Thomas, accounting for the high prevalence of STDs among the participants, increased number of children, and unsafe sexual practices. With high levels of unemployment, low skills as most were housewives, women were at a disadvantaged compared with their male counterparts, in sexual and reproductive practices and lifestyle choices, because the power lies with the males who have very little desire to use condoms when engaged in sexual activities.
While the Pap smear examination found that the prevalence of abnormal results was 17%, the test has highlighted a public health concern which has not being recorded in any public health statistics for the parish. The current findings concur with the statistics from the Clinics in the parish with a 1% difference between the medical records and data from this research. The knowledge level of women in the sample regarding Pap smears is high, and so are the numbers of those who have done a test. The challenge for public health practitioners and policy makers is to increase the frequency at which the Pap smears are done by women in the parish and thereby lower STD rates. It is important that women are empowered to take control of their sexual practices and their bodies within the context of poverty, low social standing and less material resources than their male counterparts. Another challenge for public health specialists is in lowering the parity of women in the parish, as the mean parity of 2.9 per women is more than that of the nation (2.5 per women)[1,21]. There is also a challenge to increase the age of initial sexual encounters for women, and safe sexual practices among the current cohort of women in the parish.
With 22% of the sample stating that their initial sexual encounter was when they were less than 15 years, public health practitioners need to ask themselves whether Pap smears should be recommended for females less than 15 years of age. The unhealthy lifestyle behaviour among women in the parish is such that there could be an HIV/AIDS pandemic in the parish in the future. The current findings also revealed that of those women who knew that they had an STD, 23.1% indicated that they did not know that the infection could include HIV/AIDS, as well as others which the women did not wish to reveal in a study. Furthermore, 76.4% of the sample showed signs and experienced symptoms of a STD, but only 31.3% knew that they had it. This suggests possibly their male partner's promiscuity and how the infrequent use of condoms results in more women being unaware of being infected with a STD. Pap smears, therefore, are providing women with an opportunity to being aware about the sexual lifestyle of their partners, their STD status, and the normality or abnormality of the Pap smear results.
Thirty-four percent of females in Jamaica (in 2007/08) indicated that they had never undergo a Pap smear[5], indicating that there is more adherence to Pap smear screening in St. Thomas than in the nation as a whole, but 14.5% of women in Jamaica stated that they had contracted an STD, and 2.4% in the last 12 months. With respect to sexual partners, 31.5% of females (ages 15 - 74 years) indicated that they had not had a sexual partner in the last 12 months, 6.8% had two partners, 1.5% had 3-5 partners and 0.1% more than 10 partners. Those findings, compared to the current study, highlight less promiscuous sexual behaviour of women in St. Thomas (ages 15 - 54 years), but possibly promiscuous sexual practices of their male partners. However the prevalence of condom usage is greater in St. Thomas among women (15 - 54 years) compared with 41.2% for females in the entire nation[5]. The issue here is infrequent condom usage, not the prevalence of usage, as knowledge of its usage and vulnerability to contracting STDs are not influencing the frequency of usage that will protect women from STDs and pregnancy. Another issue which emerges from the current study is the percentage of people in the sample who are probably infected with HIV/AIDS and are unaware of it, similar to the high percentage infected with other STDs[22]. Data from the Ministry of Health in Jamaica showed that 63% of those with HIV/AIDS in the nation were not aware of their status[17], and the risky sexual practices of women in St. Thomas there could cause in the future a HIV pandemic in the parish.
A study done in 1999 found that 29% and 9% of men and women respectively indicated that they had had STDs, and the researchers saw this as a public health concern at the time[23]. The findings of the current study therefore highlight a possible pandemic of STDs in St. Thomas, and emphasizes that low socio-economic status is associated with risky sexual behaviour. Figueroa et al.[23] found a significant statistical association between lower socio-economic status and higher numbers of sexual partners. This also gives credence to the high prevalence of STDs, large number of children, and frequently unsafe sexual practices among the participants, who were mostly unemployed housewives and students. The prevalence of abnormal Pap smear results in St. Thomas was 17%, which is greater than that for Jamaica since 2000[13], indicating that the number of pregnancies, early sexual encounters, multiple partners, STDs, and other risky unhealthy sexual behaviours are accounting for this difference. The mean percentage of abnormal Pap smears for Jamaica up to 2007 was 8.4% which highlights the exponential difference in the lifestyle behaviour and choices of women in St. Thomas compared to women in the entire nation.
A study in Botswana[24] revealed that inadequate knowledge of cancer screening is a barrier to its utilization. One of the paradoxes of this research is the relatively low knowledge of Pap smears, but there is a high utilization of this method of cervical cancer screening among women in St. Thomas. On the other hand, the women in our study indicated that if they were told about this by medical practitioners (nurse or medical doctor), they would be more likely to undergo the Pap smear. In Sweden 95% of women surveyed had undergo a Pap smear[25], which is 7% more than that of the women in St. Thomas. Despite the obvious benefits of Pap smears, this is the first study of its kind in St. Thomas, and it provides significant insights into STDs, parity and sexual lifestyle behaviour. Therefore, women in the parish of St. Thomas and in other parts of Jamaica should undergo Pap smears annually.
The Ministry of Health in Jamaica in keeping with their own findings, research findings outside of Jamaica and recommendations from scholars[26,27] as well as the National Health Service (NHS), argued that those women ages 25-54 years should undergo a Pap smear at least once every 5 years. The NHS stated that cervical cancer screening should be for women of 25-54 years, which is not in keeping with findings from Sasieni et al.[27] who recommended 20-64 years. The NHS[28] cited that in young women the cervix is usually normal, and abnormal treatment can be consequential for childbearing. This is not a sufficient rationale for the non-screening of the cervix among young females. The current study concurs with Sasieni et al.[27] which found that abnormal cervix occurred among women of 20-35 years, which highlights a potent justification for women younger than 25 years in Jamaica to undergo a Pap smear. The Ministry of Health in Jamaica[29] has promoted the need for living a healthy life, and sexual behaviour undoubtedly plays a major part in these practices, with an irresponsible sexual lifestyle clearly accounting for the prevalence of STDs among women. Although this study cannot argue that women are promiscuous in the parish of St. Thomas, there are clear signs of possibly infrequent condom use, and promiscuous behaviour in intimate relationships. The risk of non-screening among women younger than 25 years whose sexual behaviour, STD status, young age of initial sexual encounter and irregular condom use are of grave concern may lead to premature mortality. There are clear indicators that a 5-year delay for those who are likely to have an abnormal Pap smear result in the patient being diagnosed with advanced cancer which may not respond well to treatment.
Conclusion
Public health requires research findings to guide policy formulation and intervention programmes. The current findings highlight the fact that there is a public health problem brewing in St. Thomas and that there is an immediate need to have behavioural measures taken, as the current risky lifestyle of women cannot continue without causing a health pandemic in the parish. A ny public health intervention programme in St. Thomas must address the issue of poverty and unemployment, as anything less than a multi-dimensional programme will not significantly change the behaviour of women or that of men.
The Ministry of Health (Jamaica), recommends that Pap smears should be carried out on women 25-54 years, but this study finds that the age interval for conducting screening examinations needs to be lowered to 20 for women in St. Thomas. With the high infrequent condom use among the participants, leading to a high vulnerability to STDs, public health practices need to begin an education campaign geared towards men in the parish, and this requires research on the cohort as it relates to sexual practices, attitudes and knowledge of their unhealthy lifestyle practices.
Footnotes
Conflict of interest There is no conflict of interest to report.
References
- 1.World health statistics, 2009. Geneva: WHO; 2009. World Health Organization. [Google Scholar]
- 2.Washington: PAHO; 2007. Pan American Health Organization. Health in the Americas, 2002, Volume 7 - Countries; pp. 281–285. [Google Scholar]
- 3.Blake G, Hanchard B, Mitchell K, et al. Jamaica cancer mortality statistics, 1999. West Indian Med J. 2002;51:64–67. [PubMed] [Google Scholar]
- 4.Ivey MA, Legall G, Boisson EV, Hinds A. Mortality trends and potential years of life lost in the English and Dutch-speaking Caribbean, 1985-2000. West Indian Med J. 2008;57:122–131. [PubMed] [Google Scholar]
- 5.Wilks R, Younger N, Tulloch-Reid M, McFarlane S, Francis D. Kingston: Tropical Medicine Research Institute, University of the West Indies, Mona; 2008. Jamaica health and lifestyle survey 2007-8. [Google Scholar]
- 6.Demographic statistics, 2007. Kingston: Statistical Institute of Jamaica; 2008. Statistical Institute of Jamaica. [Google Scholar]
- 7.Jamaica survey of living conditions, 2007. Kingston: Planning Institute of Jamaica; 2008. Planning Institute of Jamaica, Statistical Institute of Jamaica. [Google Scholar]
- 8.Persaud V. The early incidence of cancer of the uterine cervix in community screening programmes. West Indian Med J. 1997;26:105–115. [PubMed] [Google Scholar]
- 9.NHS Cancer Screening Programs. Cervical cancer–incidence, mortality and risk factors. [Accessed April 7, 2009]. at http://www.cancerscreening.nhs.uk/cervical/cervical-cancer.html .
- 10.Health conditions in the Caribbean. Washington DC: PAHO; 1997. Pan American Health Organization; pp. 141–142. [Google Scholar]
- 11.Brooks SHE, Wolf C. Thirty year cancer trend in Jamaica. West Indian Med J. 1991;40:134–138. [PubMed] [Google Scholar]
- 12.Persaud V. Incidence of cancer of the uterine cervix in Kingston, Jamaica, 1958-1970. West Indian Med J. 1974;23:8–14. [PubMed] [Google Scholar]
- 13.Cervical cancer screening in the primary health care setting. Kingston: Health Promotion and Protection Division, Ministry of Health; 2004. Ministry of Health (Jamaica) [Google Scholar]
- 14.Ataman SL, Cooper R, Rotimi C, McGee D, Osotimehin B, Kadiri S, et al. Standardization of blood pressure measurement in a international comparative study. J Clin Epidemiol. 1996;49:869–877. doi: 10.1016/0895-4356(96)00111-4. [DOI] [PubMed] [Google Scholar]
- 15.Wilks R, Younger N, Mullings J, et al. Factors affecting study efficiency and item non-response in health surveys in developing countries: The Jamaica National Healthy Lifestyle Survey. BMC Med Research Methodology. 2007;7:1–14. doi: 10.1186/1471-2288-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kish L. A procedure for objective respondent selection within the household. J of the Am Statistical Association. 1949;44:380–387. [Google Scholar]
- 17.Kingston: Ministry of Health; 1991-2008. Jamaica. Ministry of Health. Ministry of Health annual report 1990-2007. [Google Scholar]
- 18.Marmot M. The influence of Income on Health: views of an Epidemiologist.Does money really matter? Or is it a marker for something else? Health Affairs. 2002;21:31–46. doi: 10.1377/hlthaff.21.2.31. [DOI] [PubMed] [Google Scholar]
- 19.Sen AK. New York: Anchor Books; 1999. Development as freedom. [Google Scholar]
- 20.Sen A. Poverty: an ordinal approach to measurement. Econometrica. 1979;44:219–231. [Google Scholar]
- 21.Kingston: STATIN; 2002. Statistical Institute of Jamaica (STATIN). Demographic statistics, 2001. [Google Scholar]
- 22.Washington D.C: PAHO; 2007. Pan American Health Organization. Health in the Americas, 2007 Volume II - Countries; pp. 448–464. [Google Scholar]
- 23.Figueroa JP, Fox K, Minor K. A behaviour risk factor survey in Jamaica. West Indian Med J. 1999;48(1):9–15. [PubMed] [Google Scholar]
- 24.McFarland DM. Cervical cancer and Pap smear screening in Botswana: Knowledge and perception. Int Nursing Review. 2003;50:167–175. doi: 10.1046/j.1466-7657.2003.00195.x. [DOI] [PubMed] [Google Scholar]
- 25.Idestrom M, Milson I, Anderson-Ellstrom A. Knowledge and attitude about pap smear screening program: a population-base study of women age 20 - 59 years. Acta Obstetricia et Gynecologica Scandinavica. 2002;81:962–967. doi: 10.1080/j.1600-0412.2002.811011.x. [DOI] [PubMed] [Google Scholar]
- 26.Arbyn M, Kyrgiou M, Simoens C, et al. Perinatal mortality and other severe adverse pregnancy outcomes associated with treatment of cervical intraepithelial neoplasia: meta-analysis. BMJ. 2008;337:1284. doi: 10.1136/bmj.a1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sasieni P, Adams J, Cuzick J. Benefits of cervical screening at different ages: evidence from the UK audit of screening histories. British Journal of Cancer. 2003;89:88–93. doi: 10.1038/sj.bjc.6600974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Health Service (NHS) Cervical screening programme. [Accessed November 20, 2009]. at www.cancerscreening.nhs.uk/cervical .
- 29.Kingston: Health Promotion and Protection Division, Ministry of Health; 2004. Ministry of Health. National policy for the promotion of healthy lifestyle in Jamaica. [Google Scholar]


