Abstract
Aims:
To find the diagnostic yield of a pleuroscopic pleural biopsy and to find the complication rates.
Settings and Design:
Institutional based prospective study.
Materials and Methods:
Sixty-eight consecutive patients who had undiagnosed exudative pleural effusion were recruited for pleuroscopy from September 2007 to August 2010.
Results:
A total of 68 patients (55 males and 13 females; mean age 49 years) underwent pleuroscopy. Malignancy was diagnosed in 24 patients, 22 patients had non-specific inflammation, tuberculosis was found in 16 patients, empyema was found in 2 patients, 1 patient had sarcoidosis, 1 patient had normal pleura and it was non-diagnostic in 2 patients. The diagnostic yield was 97%. There were no major complications, only four patients had minor complication like subcutaneous emphysema (three patients) and prolonged air leak (one patient).
Conclusions:
Pleuroscopy is a safe, simple, and valuable tool in the diagnosis of undiagnosed exudative pleural effusion with minimal complication rates.
KEY WORDS: Pleuroscopy, pleural effusion, pleural biopsy
INTRODUCTION
The accurate diagnosis of pleural effusion is challenging because even after thoracocentesis and/or closed pleural biopsy, 25-40% of pleural effusion[1,2] remains undiagnosed. Pleuroscopy also referred to as medical thoracoscopy is generally described as the evaluation of the pleural space. A visual inspection of the pleural space, drainage of pleural effusion, and performance of pleural biopsies are the commonly performed procedures during pleuroscopy. This study seeks to find the diagnostic yield of a pleuroscopic pleural biopsy and to find its complication rates.
MATERIALS AND METHODS
The present study was an institutional-based prospective study done at department of respiratory medicine, Apollo hospitals, Chennai. The study period was from September 2007 to August 2010. The inclusion criterion was patient with unilateral exudative pleural effusion with negative or unsuccessful blind pleural fluid analysis.
All the subjects were interviewed, examined, and investigated according to pro forma that was pre-designed. Informed consent was secured from the patients for participation in the study. At admission in all the patients hemogram, TC, DC, ESR, blood sugar, blood urea and serum creatinine, PT, PTT, INR, HIV and HBsAg tests were done. Chest X-ray PA view, CT and ultrasound chest were done. Diagnostic pleural aspiration was done and fluid was analyzed for sugar, protein, LDH, cell count, cytology, ADA, Gram stain, AFB smear, and culture.
Instrument
The semi-rigid pleuroscope consists of a handle that is similar to a standard flexible bronchoscope and a shaft that measures 7 mm in outer diameter and 27 cm in length. The shaft is made up of two sections, a 22 cm proximal rigid portion and a 5 cm flexible distal end. The flexible tip is movable by a lever on the handle, which allows two-way angulations capability of 160° up and 130° down. It also has a 2.8-mm working channel that accommodates biopsy forceps, needles, and other accessories and is compatible with various electrosurgical and laser procedures. The other advantage of the semi-rigid pleuroscope is that it interfaces easily with existing processors and light sources made by the manufacturer for flexible video bronchoscopy.
Procedure
Although pleuroscopy can be done under conscious sedation, in our institute we prefer to do it under general anesthesia as patients were more comfortable with the later. The option of anesthesia was given to the patients, and a majority of them preferred general anesthesia (65 out of 68). The patients were first placed in the lateral decubitus position with affected side up and the arm rose above the head. Patient's vital parameters, ECG, blood pressure, and oxygenation by means of pulse oximetry were monitored. General anesthesia or conscious sedation with intravenous narcotics and benzodiazepine were administered and titrated to patient comfort without compromising respiration.
The port of entry is usually at the midaxillary line between fourth and sixth intercostals spaces. Local anesthesia is administered to the skin, subcutaneous tissue, muscle, and parietal pleura. A 1-2 cm skin incision is made with a scalpel, which is followed by a blunt dissection of intercostal muscles until the pleural space is reached. A disposable flexible trocar of an inner diameter of 8 mm is inserted through the chest wall. This is followed by the insertion of the pleuroscope through the trocar. Pleural biopsy samples (usually 8-10) were obtained from the parietal pleura with biopsy forceps, particularly where it appears abnormal. After obtaining satisfactory biopsy specimens, pleuroscope was removed, followed by trocar. A chest tube (24F) was introduced through the same space and connected to the underwater seal. Chest X-ray was taken in the immediate post-operative period. The chest tube was removed the next day, if there was good lung expansion and fluid drainage was minimal.
RESULTS
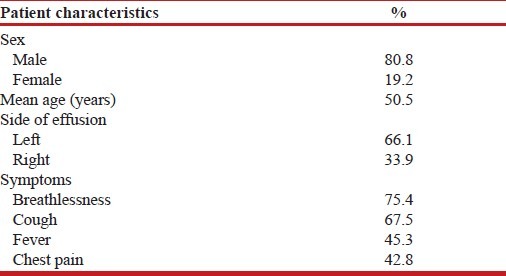
A total of 68 patients underwent pleuroscopy from September 2007 to August 2010. The indications in all these patients were unilateral undiagnosed exudative pleural effusion. Characteristics of the patients are given in Table 1. The mean age of the patients was 50.5 years. There were 55 males and 13 females. 45 patients (66%) had left-sided pleural effusion.
Table 1.
Patients characteristics
Pleuroscopic findings
Nodules were found in 33 patients, 26 patients had adhesions, 8 patients had sago grain appearance, and 1 patient had normal pleura.
Out of 68 patients, 24 patients had malignancy, 16 patients had tuberculosis, 22 patients had non-specific inflammation, 2 patients had empyema, 1 patient had sarcoidosis, 1 patient had normal pleura and it was non-diagnostic in 2 patients. The diagnostic yield for a pleuroscopic pleural biopsy was 97%.
In 24 patients who had malignancy, 15 patients had Metastatic adenocarcinoma, three patients had Mesothelioma, three patients had undifferentiated carcinoma, one patient had Lymphoma, one patient had Metastatic clear cell carcinoma and one patient had Metastatic squamous cell carcinoma.
In 22 patients who had Non specific inflammation eight patients had chronic inflammation, seven patients had fibrinous exudates, four patients had sub acute inflammation and three patients had lymphohistiocytic infiltrates.
There were no major complications, only four patients had minor complications like subcutaneous emphysema (3 patients) and prolonged air leak (1 patient).
DISCUSSION
Pleural effusions are common problem in the pulmonary practice. If a pleural biopsy specimen is needed, a physician must usually choose between a blind pleural biopsy and a Pleuroscopic biopsy. In our institute we did pleuroscopy, because most of our patients were referred (>85%) and they are already on anti TB drugs for more than 3 weeks duration with no clinical improvement and blind closed pleural biopsy has an diagnostic yield of only 50-60% for combined tuberculosis and malignancy.[2,3]
The use of fiberoptic bronchoscopes in the pleural space has been reported previously. Despite providing better views at the apex and paravertebral gutters, it was difficult to control and the diagnostic yield was low. The semirigid pleuroscope used in our study offers a solution to some of these problems. It has been designed to combine the flexibility of the conventional bronchoscope and the rigidity of conventional thoracoscope. The rigid body allows for easy steering within the pleural cavity. Having a similar design to the fiberoptic bronchoscope, it was more readily accepted by the respiratory physicians. It also has a 2.8-mm working channel that accommodates biopsy forceps, needles, and other accessories and is compatible with various electrosurgical and laser procedures. The other advantage of the semi-rigid pleuroscope is that it interfaces easily with existing processors and light sources made by the manufacturer for flexible video bronchoscopy.
In our series, we had 68 cases of unilateral exudative pleural effusion, with no diagnosis on pleural fluid aspiration. A total of 68 procedures were performed in 68 patients.
The semi-rigid pleuroscope allows for the visualization of abnormal areas and for a direct biopsy. The single incision into the chest that is needed for placement of the pleuroscope is not much larger than that made for the incision of the Abrams or cope needle. The direct visualization of the pleural surfaces had an advantage in arriving diagnosis. As in our study, nodules were found in 33 patients, adhesions were seen in 26 patients, and 8 patients had sago grain appearance, when we compared with the final histopathological examination reports >70% of patients who had nodules had malignant lesion, >96% of patients who had adhesion had chronic or sub-acute inflammation (non-malignant lesion) and 100% of patients who had sago grain nodules had tuberculosis.
In addition to visualization of pleural cavity and to take a biopsy of an abnormal area, it allows for the complete removal of pleural fluid without any additional complication like re-expansion pulmonary edema which are more common following closed thoracocentesis when more than 1.5 L of pleural fluid was removed in single sitting. The re-expansion pulmonary edema does not occur following pleuroscopy because during the removal of pleural fluid, some amount of air enters through the trocar which has an 8 mm inner diameter, whereas pleuroscope has only a 7 mm outer diameter.
The diagnostic yield in our study was 97%. This was comparable with most other studies like, Munavvar et al.,[4] Wang et al.,[5] Blanc et al.,[6] Law et al.,[7] Tscheikuna,[8] Diacon et al.,[9] and McLean et al.[10] Since follow up was not part of the protocol, we did not followed up patients with non-specific inflammation. The non-diagnostic in two patients was due to the absence of pleural tissue in the biopsy.
In our series, out of 68 patients, there were no major complications, only 4 patients (5.8%) had minor complications like subcutaneous emphysema (3 patients) and prolonged air leak (1 patient). This was comparable with most other studies like in Menzies et al.,[11] Francois et al.,[6] Munavvar et al.,[4] and Law et al.[7] studies.
The biopsy size from the rigid thoracoscope is larger than that with the semi-rigid instrument; this has been quoted as a reason for the superiority of the former. However, smaller biopsy size does not necessarily translate to the inferior diagnostic yield, because from our study and from other studies like in Munavvar et al.,[4] Ernst et al.[12] and in Khan et al.,[13] the diagnostic yield has been excellent.
In all, pleuroscopy is a valuable tool in the diagnosis of undiagnosed exudative pleural effusion. It is a simple and safe method with high diagnostic yield and with low complication rates.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Light RW. Clinical practice. Pleural effusion. N Engl J Med. 2002;346:1971–7. doi: 10.1056/NEJMcp010731. [DOI] [PubMed] [Google Scholar]
- 2.Poe RH, Israel RH, Utell MJ. Sensitivity, Specificity and predictive value of closed pleural biopsy. Arch Intern Med. 1984;144:325–8. [PubMed] [Google Scholar]
- 3.Prakash US, Relman H. Comparison of needle biopsy with cytologic analysis for the evaluation of pleural effusion; analysis of 414 cases. Mayo Clin Proc. 1985;60:158–64. doi: 10.1016/s0025-6196(12)60212-2. [DOI] [PubMed] [Google Scholar]
- 4.Munavvar M, Khan MA, Edwards J, Waqaruddin Z, Mills J. The autoclavable semirigid thoracoscope; the way forward in pleural disease. Eur Respir J. 2007;29:571–4. doi: 10.1183/09031936.00101706. [DOI] [PubMed] [Google Scholar]
- 5.Wang Z, Tong ZH, Li HJ, Zhao TT, Li XY, Xu LL, et al. Semi-rigid thoracoscopy for undiagnosed pleural effusion; a comparative study. Chin Med J. 2008;121:1384–9. [PubMed] [Google Scholar]
- 6.Blanc FX, Atassi K, Bignon J, Housset B. Diagnostic value of medical thoracoscopy in pleural disease: A 6-year retrospective study. Chest. 2002;121:1677–83. doi: 10.1378/chest.121.5.1677. [DOI] [PubMed] [Google Scholar]
- 7.Law WL, Chan JW, Lee S, Ng CK, Lo CK, Ng WK, et al. Pleuroscopy: Our initial experience in Hong Kong. Hong Kong Med J. 2008;14:178–84. [PubMed] [Google Scholar]
- 8.Tscheikuna J. Medical thoracoscopy: Experience in siriraj hospital. J Med Assoc Thai. 2006;89:S62–6. [PubMed] [Google Scholar]
- 9.Diacon AH, van de Wal BW, Wyser C, Smedema JP, Bezuidenhout J, Bolliger CT, et al. Diagnostic tools in tuberculous pleurisy: A direct comparative study. Eur Respir J. 2003;22:589–91. doi: 10.1183/09031936.03.00017103a. [DOI] [PubMed] [Google Scholar]
- 10.McLean AN, Bicknell SR, McAlpine LG, Peacock AJ. Investigation of pleural effusion: An evaluation of the new Olympus LTF semiflexible thoracofiberscope and comparison with Abram's needle biopsy. Chest. 1998;114:150–3. doi: 10.1378/chest.114.1.150. [DOI] [PubMed] [Google Scholar]
- 11.Menzies R, Charbonneau M. Thoracoscopy for the diagnosis of pleural disease. Ann Intern Med. 1991;114:271–6. doi: 10.7326/0003-4819-114-4-271. [DOI] [PubMed] [Google Scholar]
- 12.Ernst A, Hersh CP, Herth F, Thurer R, LoCicero J, 3rd, Beamis J, et al. A novel instrument for the evaluation of the pleural space: An experience in 34 patients. Chest. 2002;122:1530–4. doi: 10.1378/chest.122.5.1530. [DOI] [PubMed] [Google Scholar]
- 13.Khan MA, Ambalavanan S, Munavvar M. A comparison of the diagnostic yield of rigid and semirigid thoracoscopes. Eur Respir J. 2006;28:50. doi: 10.1097/LBR.0b013e31824ee45b. [DOI] [PubMed] [Google Scholar]


