Summary
We report a case of bilateral common carotid artery dissection due to strangulation successfully treated by stent placement, with a review of the literature. A 61-year-old woman was strangled by an apron strap. She was admitted to our hospital with tetraparesis, because of spinal cord injury. On the next day, her left hemiparesis aggravated and left facial palsy newly appeared. Diffusion weighted magnetic resonance imaging (MRI) showed new ischemic lesions in the right cerebral hemisphere. Aortography revealed bilateral common carotid artery dissection. Moreover, thrombus or intimal flap was recognized in the right common carotid artery. The right common carotid dissection was fixed with deployment of self expanding stents to prevent the aggravation of ischemic stroke at that time.
The contralateral lesion was also treated ten days later because small ischemic lesions were newly recognized in the left hemisphere on MRI. No new neurological deficit appeared after bilateral carotid artery stenting. Her paraparesis completely improved two months after the spinal cord injury. Carotid artery stenting using self expanding stents was especially effective as the treatment for bilateral carotid artery dissection.
Key words: common carotid artery, dissection, bilateral, carotid artery stenting, strangulation
Introduction
Carotid artery dissection (CAD) is rare, occurring spontaneously or secondary to trauma. Schievink reported that the annual incidence rate of CAD was 2.6 per 100,000 1. Davis also reported CAD as occurring only in 0.08% of blunt trauma patients 2. Although CAD has been often missed in cases with few symptoms, it is increasing in young people in relation to the recent increase in motor-vehicle accidents.
Traumatic CAD is caused by sports, violence or traffic accidents, and can occur in unilateral or bilateral common carotid arteries. It sometimes causes cerebral infarction and results in poor outcome. On the other hand, spontaneous CAD occurs in unilateral common or internal carotid artery, and sometimes spontaneously cures.
CAD has been treated medically or surgically until endovascular therapy was introduced. Anticoagulation is recommended as the standard medical treatment. On the other hand, surgical treatment such as arterial bypass is technically difficult and carries the risk of lower cranial nerve injury 3-5. Therefore, endovascular stent placement has recently been proposed as an alternative especially for bilateral lesions.
This paper describes a rare case of bilateral traumatic CAD secondary to strangulation treated by stent placement, and discusses our strategy of treatment with a review of the literature.
Case Report
A 61-year-old woman was caught in a conveyer belt. At that time, her neck was strangled by a strap of her apron (figure 1). She became unconscious and her pulse and respiration were weak. On admission to our hospital, she was conscious with tetraparesis 2,5 and hypesthesia in her extremities. A brain CT scan showed no abnormal lesions, but cervical MR scan revealed intramedullary abnormal intensity in the C5/6 spinal cord. She was diagnosed as spinal cord injury and received high-dose steroid therapy (1000 mg/day) after admission. On the next day, however, her left hemiparesis aggravated to 1,5, including left facial palsy, and carotid bruit was audible at her right neck. Magnetic resonance angiography showed dissection of the bilateral common carotid arteries, and diffusion-weighted MRI revealed new ischemic lesions in the right hemisphere (figure 2A). Diagnostic angiography confirmed dissection of bilateral common carotid arteries, and showed a defect of contrast medium distal to the right dissected lesion suggesting thrombus or intimal flap (figure 2B). We considered that cerebral infarction was caused by artery-toartery embolism from the right common carotid artery dissection. To prevent further embolism or acute occlusion of the dissected common carotid artery, we performed stent placement for the right common carotid artery simultaneously.
Figure 1.
Photograph of the patient on admission. Her neck is strangled by an apron strap.
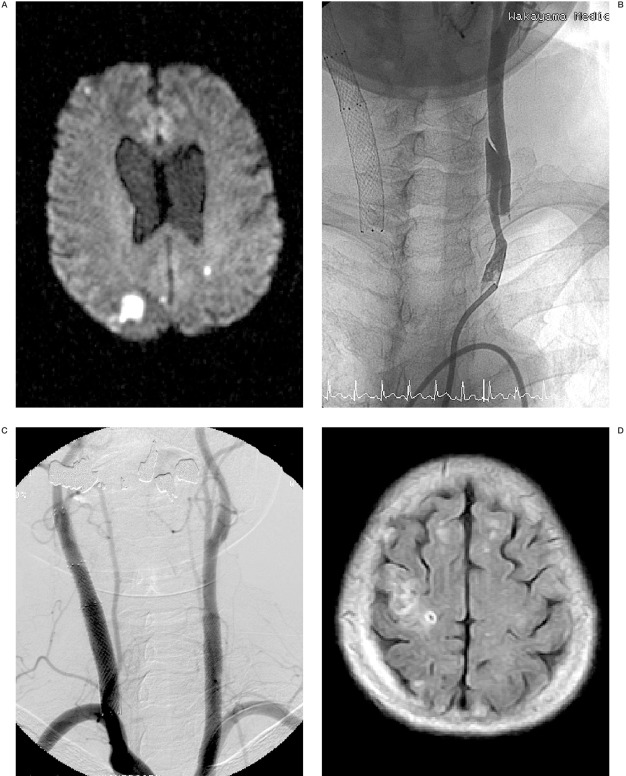
Figure 2.
A) Diffusion-weighted magnetic resonance imaging (DWI) one day after the onset, showing new ischemic lesions in the right hemisphere. B) Aortogram one day after the trauma, showing bilateral common carotid dissection. Thrombus or intimal flap is recognized in the right common carotid artery (CCA). C) Right carotid angiograms after stent placement (right oblique view), revealing good patency of the right CCA.
Under local anesthesia, a 9F guiding catheter was advanced into the right common carotid artery (CCA). As the dissected lesion was too long to cover with a single stent, two stents were necessary to cover the entire lesion. A guard wire (PercuSurge system; Medtronic, Inc., Minneapolis, MN) was navigated into the right internal carotid artery beyond the dissection, and primary stenting was performed with an 8x40 mm SMART stent (Cordis Endovascular, Miami Lakes, FL) for the distal part of dissection under distal protection. Then, a 9x60 mm SMART stent was deployed in the proximal part in overlapped fashion. These two stents covered the entire lesion and the thrombus or intimal flap disappeared immediately (figure 2C). After stenting, anticoagulation therapy (heparin 10,000 units/day) was maintained for ten days. Her neurological symptoms did not change perioperatively.
Table 1.
Literature review of carotid artery dissection.
| Case No. |
Authors and Year | Age/Sex | Epiology of Dissection | Side | Treatment | Time Interval after Onset |
Initial Symptoms |
|---|---|---|---|---|---|---|---|
| 1 | Anne et Al, 2002 | 24/f | motor vehicle accident | bilateral | anticoagulation | 1 day | GCS 8,Lt hemiplegia |
| 2 | Anne et Al, 2002 | 25/f | motor vehicle accident | bilateral | anticoagulation | 6 days | drowsiness, Rt hemiparesis,Rt Honer |
| 3 | Bejjani et Al, 1999 | 53/m | direct blow | rt | stenting | 3 months | Lt hemiparesis |
| 4 | Bejjani et Al, 1999 | 18/m | gunshot | rt | stenting | 8 days | Lt hemiparesis |
| 5 | Bejjani et Al, 1999 | 33/f | motor vehicle accident | It | stenting | 1 day | Rt hemiplegia |
| 6 | Bejjani et Al, 1999 | 55/f | lift a heavy load | rt | stenting | 2 weeks | Lt neck pain,headache |
| 7 | Doietal.,2004 | 21/m | motor vehicle accident | rt | stenting | 2 hours | JCS 20,Lt hemiparesis |
| 8 | Duncan et Al, 2000 | 39/m | motor vehicle accident | bilateral | anticoagulation | a few hours | Lt hemiplegia |
| 9 | Fabrizio et Al, 2004 | 17/m | motor vehicle accident | bilateral | stenting | ? | Lt hemiparesis |
| 10 | Khaqan et Al, 1996 | 41/f | motor vehicle accident | bilateral | anticoagulation | 1 day | Lt lower limb paresis |
| 11 | Malek et Al,2OOO | 37/f | domestic abuse | bilateral | stenting | 3 months | Rt hand weakness and numbness |
| 12 | Malek et Al,2OOO | 43/f | domestic abuse | bilateral | stenting | 3 months | Lt hemiparesis |
| 13 | Malek et Al,2OOO | 24/f | domestic abuse | bilateral | anticoagulation | 6 months | JCS 300 |
| 14 | Malek et Al,2OOO | 37/f | hanging injury | It | stenting | 3 months Rt | hemiparesis, leg numbness, and dysphagia |
| 15 | Malek et Al,2OOO | 44/f | motor vehicle accident | It | stenting | 4 months | dysphasia, Rt arm weakness, and numbness |
| 16 | Noguchi et Al, 1992 | 50/f | hanging injury | rt | carotidendoartectmy | 2 years | Lt arm 4/5, hypoesthesia |
| 17 | Okada et Al, 1999 | 30/f | motor vehicle accident | It | bypass surgery | 7 months | Rt hemiparesis |
| 18 | Okada et Al, 1999 | 42/f | motor vehicle accident | rt | bypass surgery | 2 days | Lt hemiparesis |
| 19 | Okada et Al, 1999 | 58/f | motor vehicle accident | rt | bypass surgery | 10 years | Lt hemiparesis |
| 20 | Okada et Al, 1999 | 41/f | hanging injury | rt | bypass surgery | 2 years | dizzines |
| 21 | Okada et Al, 1999 | 42/m | direct blow | rt | bypass surgery | 2 years | Lt hemiparesis |
| 22 | Okuchi et Al, 1999 | 29/m | motor vehicle accident | rt | anticoagulation | 11days | JCS 200 |
| 23 | Scavee et Al, 2001 | 53/m | motor vehicle accident | rt | stenting | 6 weeks | dizziness,neck pain |
| 24 | Stahlfeld et Al, 2002 | 39/m | ride on a rollar coaster | rt | anticoagulation | 3 weeks | headache, Lt eye pain, Lt temporoparietal numbness/ |
The contralateral lesion was also treated ten days after onset, because diffusion weighted MRI on the fourth day showed a new ischemic lesion in the left parietal lobe in spite of anticoagulation (figure 3A). Carotid artery stenting was performed in the same manner as the first. After distal protection, an 8x60-mm Xpert stent (Abott Vascular Devices Chicago Illinois USA) was deployed to cover the entire lesion of the CCA dissection (figure 3B,C).
Figure 3.
A) DWI 4 days after the onset, showing new high intensity spot in the parieto-occipital lobe. B) Left carotid angiogram 13 days after the accident showing the dissection in the left CCA. C) Aortogram after stent placement revealing disappearance of the dissection in the bilateral CCA. D) Fluid attenuated inversion recovery (FLAIR) magnetic resonance imaging 60 days after the onset, showing minor infarction in the right hemisphere.
She was treated with an antiplatelet drug (biaspirin 100 mg/day)after the stent placement for the left carotid lesion. Her paraparesis improved to full strength two months after the injury. Angiography at the 23rd day revealed widely patent CCA without any thrombus in the bilateral common carotid artery, and follow-up MRI at the 60th day showed no new cerebral infarction in the brain (figure 3D).
Discussion
The etiology of CAD caused by neck trauma is generally considered as follows. (A) The CCA is stretched by neck hyperextension during rotatory movement of head. (B) The CCA is compressed to the lateral mass of the atlas and transverse processes of the spine during contralateral flexion of the neck. (C) The CCA is directly injured by a blow 6. We reviewed 43 patients who had diagnosis of traumatic CAD from 1988 to 2004, and found that CAD caused by (A) or (B) had a tendency to occur in the unilateral internal carotid artery. As for the cause of CAD, it was often associated with motorcar or bicycle accidents. On the other hand, CAD due to strangulation was reported to be rare. In our case, bilateral CAD was considered due to direct injury to the common carotid artery at the neck. As her neck was strangled by her apron strap, bilateral CCAs were easily compressed by the strap.
When CAD occurs, thrombus may be formed near the dissection, and causes distal embolism or acute occlusion. In cases of traumatic CAD, it is well known that there are more cases with focal signs caused by cerebral embolism than those with headache alone 7. In 25 cases whose initial symptoms were reported in the literature, hemiparesis was identified in 19 cases, and headache was only in two patients 5-16. According to the interval from accident to onset of symptoms, it has been considered that neurological signs due to CAD generally occur within 24 hours 14. In our review of the literature, however, symptoms occurred within 24 hours only in two out of 25 cases. On the other hand, in 11 out of 23 patients, symptoms occurred after a few months, and most of these patients suffered from cerebral ischemia. Therefore, we should consider that it is necessary to look for cerebral embolism for a long time, even in asymptomatic patients.
In general, CAD has been treated medically, especially in asymptomatic cases. Heparin was continued for about one week, and followed by oral anticoagulant with warfarin for three to six months. When frequent transient ischemic attack or cerebral infarction occurs, surgical treatment should be considered 3,17,18. Surgical treatment includes interposition of the saphenous vein graft, extracranial to intracranial arterial bypass, and carotid endarterectomy. In seven out of 25 cases in our review, surgical treatments were selected, and five of them received reconstruction with vein graft. Okada et Al reported the outcome of surgical treatment was poor in their series 5. As the reason for poor results, it was considered that surgery must be performed under anticoagulation and the rate of graft vessel patency was low. Moreover, especially in a case of bilateral CAD as our case, surgery may cause laryngeal nerve palsy bilaterally. On the other hand, stent placement was done for ten out of 25 cases and their results were good in all cases. Recently, stent placement proved to be good for high-risk patients for carotid endarterectomy in the SAPPHIRE study 19. Therefore, stent placement is considered more suitable than direct surgery, as a treatment for bilateral CAD.
Carotid artery stenting allows immediate disappearance of dissected lumen with reperfusion to ischemic brain. In particular, sthe elf-expanding stent we used in our case can resolve dissection by compressing the intimal flap to the vessel wall. Since the vessel wall of traumatic dissected carotid artery does not have atheromatous plaque as seen in cases of atherosclerotic carotid artery stenosis, the risk of embolic complication and restenosis seems low, and strong medication is considered unnecessary after stenting.
At present, although guidelines for treatment of CAD are lacking, we consider it is better to perform stent placement for traumatic CAD in symptomatic cases as soon as possible. Even in asymptomatic case, there is a possibility of causing cerebral embolism in the chronic phase as shown in previous reports. Therefore, we consider that it is reasonable to perform stent placement when new lesions are detected on MRI.
References
- 1.Schievink WI, Mokri B, Whisnant JP. Internal carotid artery dissection in a community, Rochester, Minnesota, 1987-1992. Stroke. 1993;24:1678–1680. doi: 10.1161/01.str.24.11.1678. [DOI] [PubMed] [Google Scholar]
- 2.Duncan MA, Dowd N, et al. Traumatic bilateral internal carotid artery dissection following airbag deployment in a patient with fiblomuscular dysplasia. Br J Anaesth. 2000;85:476–478. doi: 10.1093/bja/85.3.476. [DOI] [PubMed] [Google Scholar]
- 3.Benjjani GK, Monsein LH, et al. Treatment of Symptomatic Cervical Carotid Dissection with Endovascular Stents. Neurosurgery. 1999;44:755–761. doi: 10.1097/00006123-199904000-00037. [DOI] [PubMed] [Google Scholar]
- 4.Cohen JE, Leker RR, et al. Emergent Stenting to Treat Patients with Carotid Artery Dissection. Stroke. 2003;34:254–257. doi: 10.1161/01.STR.0000101915.11128.3D. [DOI] [PubMed] [Google Scholar]
- 5.Okada Y, Shima T, et al. Traumatic dissection of the common carotid artery after blunt injury to the neck. Surg Neurol. 1999;51:513–20. doi: 10.1016/s0090-3019(98)00102-5. [DOI] [PubMed] [Google Scholar]
- 6.Noguchi K, Matsuoka Y, et al. A case of common carotid artery stenosis due to hanging. No Shinkei Geka. 1992;20:1185–1188. [PubMed] [Google Scholar]
- 7.Lucas C, Moulin T, et al. Stroke Patterns of Internal Carotid Artery Dissection in 40 Patients. Stroke. 1998;29:2646–2648. doi: 10.1161/01.str.29.12.2646. [DOI] [PubMed] [Google Scholar]
- 8.Chomel A, Verneh M, et al. Traumatic bilateral dissections of the internal carotid artery: An infrequent diagnosis not to be missed. J Neurosurg Anesthesiol. 2002;14 doi: 10.1097/00008506-200210000-00007. N° 4. [DOI] [PubMed] [Google Scholar]
- 9.Anson J, Crowell RM. Cervicocranial arterial dissection. Neurosurgery. 1991;29:89–96. doi: 10.1097/00006123-199107000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Doi A, Deguchi J, et al. Traumatic Internal Carotid Artery Dissection Due to Compression by a Helmet Strap. No Shinkei Geka. 2004;32:1279–1282. [PubMed] [Google Scholar]
- 11.Fabrizio F, Fillippo MS, et al. Stent Repair of Bilateral Post-Traumatic Dissections of the Internal Carotid Artery. J Endovascular. 2004;11:517–521. doi: 10.1583/04-1207.1. [DOI] [PubMed] [Google Scholar]
- 12.Leys D. Cevical artery dissections. Eur Neurol. 1997;37:3–12. doi: 10.1159/000117396. [DOI] [PubMed] [Google Scholar]
- 13.Malek AM, Higashida RT, et al. Patient?presentation, angiographic features and treatment of strangulation- induced bilateral dissection of the cervical internal carotid artery. J Neurosurg. 2000;92:481–487. doi: 10.3171/jns.2000.92.3.0481. [DOI] [PubMed] [Google Scholar]
- 14.Mokri B, Piepgras DG, Wayne HO. Traumatic dissections of the extracranial internal carotid artery. J Neurosurg. 1988;68:189–197. doi: 10.3171/jns.1988.68.2.0189. [DOI] [PubMed] [Google Scholar]
- 15.Scavee V, De Wispelaere JF, et al. Pseudoaneurysm of the internal carotid artery: treatment with a covered stent. Cardiovasc Intervent Radiol. 2001;24:283–285. doi: 10.1007/s00270-001-0012-z. [DOI] [PubMed] [Google Scholar]
- 16.Watridge CB, Muhlbauer MS, Lowery RD. Traumatic carotid artery dissection: diagnosis and treatment. J Neurosurg. 1989;71:854–857. doi: 10.3171/jns.1989.71.6.0854. [DOI] [PubMed] [Google Scholar]
- 17.Malek AM, Higashida RT, et al. Endovascular Management of Extracranial Carotid Artery Dissection Achieved Using Stent Angioplasty. Am J Neuroradiol. 2000;21:1280–1292. [PMC free article] [PubMed] [Google Scholar]
- 18.Uno M, Ueda S, et al. Management and long-term follow-up results in patients with carotid artery dissection. No Shinkei Geka. 1997;25:417–423. [PubMed] [Google Scholar]
- 19.Yadav JS, Wholey MH, et al. Protected Carotid-Artery Stenting versus Endarterectomy in High-Risk Patients. N Engl J Med. 2004;351:1493–1501. doi: 10.1056/NEJMoa040127. [DOI] [PubMed] [Google Scholar]