Abstract
This study examined a threshold model which proposes that social support exhibits a curvilinear association with adjustment and distress, such that support in excess of a critical threshold level has decreasing incremental benefits. Women diagnosed with a first occurrence of breast cancer (N = 154) completed survey measures of perceived support (Social Provisions Scale), quality of life (Functional Living Index-Cancer), adjustment (Psychological Adjustment to Illness Scale) and psychological distress (Brief Symptom Inventory) approximately three weeks after surgical treatment and 8–16 months later. Consistent with a threshold model, multiple regression analyses suggested a significant curvilinear relationship between social support and distress at Time 1 and Time 2; and between social support and adjustment at Time 2. Consistent with this model, the significant bivariate correlations between social support and outcomes were accounted for almost entirely by women in the lowest quartile of support. Social support among women in the highest three quartiles was unrelated or only marginally related to adjustment and distress.
Keywords: breast cancer, social support, threshold effects, adjustment to chronic illness, distress
In the United States over 230,000 women are diagnosed with a first occurrence of breast cancer each year. The lifetime risk of a woman developing breast cancer is currently over 12%. Thanks to earlier detection and more effective treatment, the 5-year survival rate has increased from 63% in the early1960s to 90% in 2007. The 5-year survival rate for cancer that has not spread to local lymph nodes has now reached 98% (American Cancer Society, 2011). Thus, the number of long-term breast cancer survivors has greatly increased in recent years, to over 2 million women in the U.S. A considerable body of research documents the benefits of social support in a broad range of cancer types (Uchino, Cacioppo, & Keicolt-Glaser, 1996), as well as specifically for women with breast cancer (for reviews see Bettencourt, Schlegel, Talley, & Molix, 2007; Nausheen, Gidron, Peveler, & Moss-Morris, 2009). The benefits of social support include tangible assistance, advice, emotional reassurance, and facilitation of immune function that may decrease risk of cancer recurrence (Lutgendorf et al., 2005).
In contrast to this large body of research, much less attention has been focused on the role of unsupportive behaviors and negative interpersonal interactions in undermining the adjustment of women during and after treatment for breast cancer. However, a large community study found that negative interactions with partner or friends were more predictive of depressive symptoms than positive interactions (Schuster, Kessler, & Aseltine, 1990). Research indicates unsupportive interactions are also associated with psychological distress in breast cancer patients (e.g., Koopman, Hermanson, Diamond, Angell, & Spiegal, 1998), and that negative interactions with one’s partner have more potential to harm emotional adjustment than positive interactions facilitate adjustment or well-being (Coyne & Anderson, 1999; Manne, Taylor, Dougherty, & Kemeny, 1997). It appears that support from family and friends may compensate for an unsupportive partner, but breast cancer survivors who lack support from all three sources (partner, family, and friends) may be especially vulnerable to adjustment problems and distress (Manne et al., 2003). A growing body of research suggests that a lack of support reciprocity with one’s partner often exacerbates coping difficulties in the context of a range of life-threatening illness in which both the patient and the other partner face unique stressors (Berg & Upchurch, 2007; Walsh, 2005). In heterosexual couples, women may experience special challenges because they are predisposed to prefer support-based coping strategies (“tend and befriend”) in contrast to the male preference for “flight or fight” responses (Taylor et al., 2000). Some evidence suggests that social support from religious congregations is frequently perceived as having a mixture of positive and negative impact by recipients (Ellison, Krause, Shepherd, & Chaves, 2009).
Detailed studies of the nature of these unsupportive interactions suggest that one pattern involves avoidance of the patient or criticism of her coping efforts (Manne & Glassman, 2000). These interactions may be especially damaging if, instead of receiving affirmative support from a relationship usually expected to be a source of comfort (e.g. family member or partner), the person in this close relationship withdraws from or criticizes the cancer patient (Norton et al., 2005). Research suggests that a second pattern of unsupportive interaction occurs when the support provider genuinely intends to be supportive, but the interaction has an unintended negative effect. In a recent survey, the most frequently rated interactions of this type were dismissive or trivializing statements from erstwhile supporters such as “someone told me to be strong, to keep my chin up, or that I shouldn’t let it bother me” or “someone said I should look on the bright side” (Figueiredo, Fries, & Ingram, 2004, p. 100).
A third type of unsupportive interaction occurs when friends or family members offer a type of support that might be well-received and perceived as helpful in a different situation but is not the type of support that the breast cancer patient needs in the current circumstances. Reynolds and Perrin (2004) defined “support commission” mismatch as occurring when a type of support is offered that the recipient does not want. These researchers compared positive support match, satisfaction with support, and support commission mismatch in a multiple regression predicting psychological adjustment for breast cancer survivors. Support commission mismatch was a significant unique predictor of poor adjustment, after controlling for positive support and satisfaction with support. Based on their literature review and on the findings of their study, Reynolds and Perrin (2004, p. 430) concluded that much social support research is based on three potentially faulty measurement assumptions: (a) each item of the assessment instrument taps an aspect of support that is positively valued by the respondent, (b) the person who provides the support always has “uniformly good intentions,” and (c) the provider and recipient agree on what constitutes helpful and desired support.
We propose a fourth item for inclusion in this list of assumptions to be questioned, namely, that each unit increment in perceived social support is associated with a corresponding proportional unit increase in well-being or adjustment throughout the entire range of perceived social support. Studies that adopt this “linearity assumption” use statistical regression methods to test direct or buffering effects of social support. Significant bivariate correlations (direct effects) are almost invariably interpreted as suggesting that more perceived support leads to fewer symptoms or better adjustment (e.g. Manne et al., 1997). Significant multiple regression interactions (buffering effects) are typically interpreted as suggesting that support has an ameliorating effect and lessens the association between the stressor and stress symptom (e.g. Penninx et al., 1998). However, it is equally valid to interpret the same findings as indicating that a low level of support may undermine adjustment, increase symptoms of distress or, in interaction analyses, exacerbate the negative impact of a stressor. These quite different interpretations must be considered equally valid for social support studies that collect data at one time point and use linear regression analyses.
Problems with the linearity assumption become apparent as we consider the practical meaning of the full range of scores from a widely used measure of perceived support such as the Social Provisions Scale (SPS, Cutrona & Russell, 1987, 1990). Subjects respond to the 24 items of this instrument using a 4-point Likert format (1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree). The SPS contains items such as, “There are people I can depend on to help me if I really need it” or “I feel a strong emotional bond with at least one other person.” At the response midpoint of 2.5, respondents are as likely to disagree as agree with these items. Thus, scores below the SPS midpoint of 2.5 do not represent moderate levels of support, but instead represent a range in which participants tend to disagree that they have support. Cutrona and Russell (1987) reported a mean of 3.48 in a sample of 1700 undergraduates, school teachers, and nurses. Thus, the scale midpoint is more than two SD units below the mean in a large normative sample. As scores drop below 2.5 (i.e., an average “disagree” response), individuals in this range are best described as perceiving that they have very little support. Low scores for some individuals might also be consistent with unsupportive, interactions in close personal relationships, but because the SPS only allows respondents to agree/disagree with statements about the presence of supportive others, the scale is not capable of directly assessing detrimental relationships. Although it is unclear precisely where a critical cutoff point may lie along a range of SPS scores, a threshold model implies the possibility that the experiences of breast cancer survivors who tend to disagree with items on a measure of perceived social support may be qualitatively different than those who tend to agree.
Rejecting the linearity assumption opens the possibility that perceived social support, as it is typically measured, may exhibit a nonlinear relationship with adjustment and with distress. Although many nonlinear relationships are possible, one specific variant was the focus of this study. We examined a curvilinear relationship in which breast cancer survivors respond differently to a given increment through the range of perceived social support. In the threshold model shown in Figure 1, at the lowest range of social support we expected a given increment to have a very large positive effect on adjustment. However, as an individual receives higher levels of support, we expected the same unit of increase to have decreasing benefits. After reaching a threshold level of support, we expected further increments to produce little incremental benefit.
Figure 1.
Hypothesized threshold function of social support and adjustment.
To identify studies that investigated similar models, a search of the PsycINFO database was conducted for citations indexed with the term “social support” and either “threshold,” “nonlinear,” or “curvilinear.” A total of 28 empirical articles published in peer-reviewed journals over the past 25 years were identified. Of these, only three studies were relevant – even marginally – to the model we propose. A prospective study of nearly 3,500 Japanese American men over the age of 70 found that mortality rates were progressively lower for men in successively higher quartiles of social network support. However, the increment of improvement grew less with each higher quartile, a finding the authors interpreted as consistent with a dose-response threshold model of social support (Ceria et al., 2001). In the second study, adult children and their elderly parents were surveyed. Social support from offspring exhibited a curvilinear relationship with parents’ mood. Increasing levels of support were associated with higher positive mood up to a threshold, beyond which point greater support was associated with less positive mood (Silverstein, Chen, & Heller, 1996). In the third study, a threshold model of support was explicitly investigated in a sample of firefighters who lived together while on duty, and thus had unique opportunities as co-workers to support one another (Jordan Varvel et al., 2007). Significant curvilinear effects were observed for a specific type of support. For firefighters below the median in Reassurance of Worth (a subscale of the SPS), there was a significant negative correlation with perceived stress. However, for those above the median this relationship was not significant. These findings are consistent with a model in which support beyond a minimum threshold does not confer additional benefits.
Whether a linear model or threshold model best fits the relationship of social support to adjustment in breast cancer survivors is not an esoteric question. To the contrary, the answer has profound implications for interventions that provide social support. For example, if a linear model best describes the support-adjustment relationship, then all women can be expected to benefit from programs designed to boost their perceptions of support regardless of their initial level of support. However, a threshold model implies that priority for scarce intervention resources should be given to women who are below a critical cutoff. Breast cancer survivors who perceive support above this level are likely to receive little added benefit from the intervention. Resources could be better deployed by serving more patients who are below the threshold. Therefore, the purpose of this study was to examine whether a threshold model provided a better fit than a simple linear model to describe the relation of perceived social support to symptoms of psychological distress and positive indicators of adjustment to chronic illness for breast cancer survivors shortly after their treatment.
Method
Participants
Women with an initial diagnosis of breast cancer were recruited from treatment centers and hospitals serving more than 40 counties in the central region of a Midwestern state. The area is predominantly rural, with the largest city having a population of 90,000. Surveys were distributed to women during their first post-surgery visit to the clinic, which occurred approximately three weeks after their initial diagnosis. A total of 203 women were assessed at Time 1. Of these, 154 (76%) provided data at Time 2 when they returned to the clinic for a routine follow-up appointment 8–16 months later. The mean age of these 154 patients at Time 1 was 58.97 years (SD = 12.33, range = 29–89 years). In terms of ethnic identification, four (2.6%) indicated “African American,” one (0.6%) indicated “Hispanic” and the remaining 149 (97%) indicated “White Non-Hispanic.” With regard to relationship status, 70% reported they were currently married, 10% divorced or separated, 11% widowed, and 8% single. Patients were screened to ensure that this was the first occurrence of breast cancer. In terms of cancer stage, 13% were diagnosed as Stage 0, 42% Stage I, 26% Stage II, 11% Stage III, 3% Stage IV, and for 5% the stage was not recorded in the records available to us. Every patient received diagnostic biopsy, as well as subsequent lumpectomy or mastectomy surgery. Following surgery 19% received both chemotherapy and radiation, 32% received chemotherapy only, 18% received radiation only, and the remaining 31% received neither radiation nor chemotherapy. The mean interval between Time 1 and Time 2 data collection was 53 weeks (SD = 5.6 weeks, range = 33 to 70 weeks; 75% were assessed between 48 and 60 weeks after Time 1). This study was part of an ongoing longitudinal project whose purpose was to track the occurrence of lymphedema and assess adjustment and distress over a seven-year period after treatment for breast cancer.
Measures
Social support
The Social Provisions Scale (SPS, Cutrona & Russell, 1987, 1990) is a 24-item measure of perceived social support. Respondents use a 4-point Likert-type scale (1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree) and are directed to “think about your current relationships with friends, family members, co-workers, community members, and so on.” Higher scores indicate more perceived support. Cutrona and Russell (1987) reported that a confirmatory factor analysis resulted in support for their six-factor structure in a mixed sample of college students, teachers, and nurses. In the current study the entire scale was administered but the Opportunity for Nurturance items were not included in calculations of the total score.1 For the resulting 20-item Social Provisions Scale – Modified (SPS-M) internal reliability (coefficient alpha) was .89 at Time 1 and .92 at Time 2 in this study. In previous studies evidence of validity was provided by positive correlations of total SPS score with cancer patents’ adjustment (Holland, & Holahan, 2003; Roberts, Lepore, & Helgeson, 2006) and immune function (Lutgendorf et. al. 2005).
Quality of life
The Functional Living Index-Cancer (FLIC,Schipper, Clinch, McMuray, & Levitt, 1984) is a 22-item self-report instrument designed to assess the domains of psychological adjustment, physical adjustment to cancer treatment aftereffects (e.g. nausea, pain), capacity to maintain daily activities and leisure pursuits, and perceptions of cancer as having imposed “disruption” or “hardship” on one’s self and family. Each item uses a 7-point response scale that is tailored to the specific item and anchored only at the endpoints. The contrasting anchors capture the range of a patient’s response. For example, a question about how well one is managing pain (e.g., “How much is pain or discomfort interfering with your daily activities?”) is anchored by 1 = not at all to 7 = a great deal. The time frame varies from item to item, and includes “today,” “the past two weeks,” or “the past month.” Higher scores indicate a higher quality of life. Schipper et al., report construct validity in the form of correlations in the expected direction with the Beck Depression Inventory and the General Health Questionnaire in a sample of cancer patients. Only the total scale score was used in this study. Internal consistency (coefficient alpha) was .89 and .90 for Time 1 and Time 2, respectively.
Adjustment
The Psychosocial Adjustment to Illness Scale-Self Report (PAIS-SR, Derogatis, 1986; Derogatis & Derogatis, 1990) is a 46-item self-report instrument used to assess a patient's adjustment to the experience of a chronic, potentially life-threatening illness. Each item uses a 4-point multiple choice response format with different responses used in different clusters of items. The time frame for every item is “the past 30 days.” The original PAIS-SR included seven conceptually-derived subscales. Although the developers reported results of confirmatory factor analyses, these findings have been questioned and an alternative factor structure has been proposed based on a broader sample of men and women with different types of cancer (Merluzzi & Martinez Sanchez, 1997). Consequently, we used only the total scale score in this study. Higher scores indicate better adjustment. However, in calculating this total we excluded four items from the Sexual Relations subscale because 45% of our sample had missing values for one or more of these items. In this study, for the 42 remaining items of modified PAIS (PAIS-M), internal reliability (coefficient alpha) was .91 and .93 for Time 1 and Time 2, respectively.
Psychological symptoms
The Brief Symptom Inventory (BSI, Derogatis, 1993) is a shortened version of the Symptom Checklist-90 and is a widely used global indicator of psychological functioning. The BSI lists 53 symptoms to which participants respond indicating how much they were distressed in the last 30 days by each complaint, using a 5-point frequency type scale (0 = not at all, 4 = extremely). The BSI items are used to calculate a total Global Severity Index. Higher scores indicate more reported symptoms. Derogatis and Spencer (1982) report test-retest reliability (two-week interval) of .90 for the total Global Severity Index, as well as considerable evidence of convergent, divergent, and predictive reliability in both community and clinical samples. Internal reliability (coefficient alpha) at was .94 and .95 at Time 1 and Time 2, respectively.
Procedure
Patients over the age of 18 who had received a diagnosis of breast cancer were referred by surgical and medical oncologists, or by other health care providers. These patients were personally invited to participate by telephone when their pre-op assessment was scheduled, soon after their post-surgery follow-up appointment was scheduled, or in person at the time of their clinic visit. Patients were also informed about the study through flyers in clinic waiting areas that provided a telephone number to call. The research was described as a study of “the ways women cope with breast cancer.” The Time 1–Time 2 retention rate of 76% was achieved in large part because data collection was coordinated with the patients' routine follow-up clinic visits, and they earned modest financial incentives ($25) for participation. Because there was considerable variation in scheduling of these medical follow-up appointments, the interval between the two data collection points varied from 8–16 months. Survey packets were given to patients during their clinic visit, with stamped pre-addressed envelopes used to return the completed data. One patient with impaired vision was assisted though an in-person interview instead of completing the survey in her home.
Results
Preliminary Analyses
Examination of missing data indicated that less than 4% of all items for all cases were missing. Among all patients, 23% had no missing data. Inspection of the items most frequently missing for the remaining 77% revealed that 30% of the women did not answer four or more items of the PAIS (apart from the Sexual Relations subscale). Four of the most frequently missing items were connected with lost time from work due to illness, job performance, or job satisfaction. SPSS version 19.0 analysis of missing data patterns suggested that women with these items missing were significantly more likely to be older than the women who did answer these items. Perhaps a substantial number of the women with this pattern of missing data found that these items were not relevant to them because they were not formally employed. Little’s test was not significant, indicating that the pattern of data was not missing completely at random, χ2 (df = 22965) = 310.277, p = 1.0. Following suggestions for best practices in handling this pattern of missing data (Schlomer, Bauman, & Card, 2010) a multiple imputation (MI) procedure was used to estimate missing data values. Simulation analyses suggest that MI performs significantly better than mean substitution or pairwise deletion (Schlomer et al.). We used the MI procedure available in SPSS 19.0. Five imputed data sets were created using available data to estimate missing values. Subsequent analyses were conducted on all five datasets, with results automatically pooled.
The procedure suggested by Tabachnick and Fidell (2007) was used to screen the data for multivariate outliers. Four variables (social support, quality of life, adjustment to illness, and psychological symptoms) at Time 1 and Time 2 were used to calculate Mahalanobis distance for each patient. Seven cases exceeded the recommended cutoff of p < .001. Inspection of these cases revealed no apparent problems with data coding or inattentive responding and they were included in subsequent analyses. Next we used a series of four t-tests to compare the 154 patients who provided Time 2 data with the 49 who did not, with respect to the Time 1 data that both groups provided. There were no significant differences in Time 1 social support, psychological symptoms, quality of life, or adjustment to cancer, ts(201) < 0.84, ps = ns. The largest effect size for the difference between the two groups was in psychological distress (BSI scores), d = 0.11. Remaining analyses were conducted only with the 154 women who provided Time 1 and Time 2 data.
Table 1 shows that the mean level of social support for our sample at Time 1 and Time 2, was 3.60 and 3.54, respectively. These item means are within about one SD unit from the maximum possible score of 4.0, and thus raise some question about the representativeness of this sample. We located 11 studies that used the SPS with cancer patients. Six of these did not report any M or SD information. Two of the remaining five assessed breast cancer patients. In Drageset and Lundstrom (2003) the item mean was 3.75, and in Halland and Holaran (2003) the item mean was 3.71 for the 20 items excluding Opportunity for Nurturance. We found three additional studies that reported M and SD for samples of other types of cancer patients. Lutgendorf et al. (2005) used only the SPS Attachment subscale and reported a mean of 3.67 with 42 women diagnosed with ovarian cancer. The remaining studies reported means only for the total SPS scale, including Opportunity for Nurturance. Roberts et al. (2006) reported means of 3.66 and 3.69 in two measurements of 89 men with prostate cancer. Shell, Carolan, Zhang, and Menese (2008) studied 59 patients with lung cancer (34% women) and reported means of 3.33 at Time 1 and 3.26 at Time 2. Thus, Snell et al. was the only one of the five studies of cancer patients we could locate that reported SPS means lower than ours. Thus, although the mean SPS scores in our sample are high relative to the scale midpoint, they are not atypical (and tend to actually be lower) than other published studies of cancer patients.
Table 1.
Means, Standard Deviation and Correlations between Time 1 and Time 2 Variables
| ---- Time 1 ---- | ---------- Time 2 ---------- | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| Time 1 | ||||||||
| 1. Social support (SPS-M) | -- | .26** | .29** | −.26** | .65** | .15 | .31** | −.31** |
| 2. Quality of life (FLIC) | -- | .74** | −.47** | .32** | .53** | .57** | −.53** | |
| 3. Adjustment to illness (PAIS-M) | -- | −.63** | .41** | .48** | .69** | −.64** | ||
| 4. Psychological symptoms (BSI) | -- | −.32** | −.26** | −.44** | .85** | |||
| Time 2 | ||||||||
| 5. Social support (SPS-M) | -- | .34** | .53** | −.44** | ||||
| 6. Quality of life (FLIC) | -- | .73** | −.50** | |||||
| 7. Adjustment to illness (PAIS-M) | -- | −.69** | ||||||
| 8. Psychological symptoms (BSI) | -- | |||||||
Note. N = 154. SPS-M = Social Provisions Scale-Modified, FLIC = Functional Living Index-Cancer, PAIS-M = Psychological Adjustment to Illness Scale-Modified, BSI = Brief Symptom Inventory.
p < .05
p < .01
Social Support and Adjustment
Table 1 also presents correlations among social support and outcomes at Time 1 and Time 2. The first row shows that social support at Time 1 was significantly associated with all three outcome variables at Time 1, and at Time 2 with adjustment to illness (PAIS-M) and psychological symptoms (BSI), but not quality of life (FLIC). The fifth row of this table shows that Time 2 social support was significantly correlated with all three outcome measures at Time 2. Table 2 shows repeated measures t-tests of change over time for these variables. Both quality of life (FLIC) and adjustment to illness (PAIS) significantly increased over the 8–16 months that passed from Time 1 to Time 2, but counter to this trend of improvement, psychological symptoms (BSI) also significantly increased. The strongest gains were seen in quality of life d = 1.05. Perhaps this is not surprising given that some of the FLIC items assessed side effects of cancer treatment such as nausea and discomfort that are would not be expected to persist. Gains in long term adjustment to illness were also evident as improvement in PAIS-M scores, d = 0.42. Note that perceived social support significantly decreased from Time 1 to Time 2. However, the effect size was comparatively small, d = −0.14.
Table 2.
Change in Psychosocial Variables
| Post- treatment |
One year follow-up |
|||||
|---|---|---|---|---|---|---|
| Time 1 | Time 2 | Effect size | ||||
| Psychosocial Variable | M | SD | M | SD | t (120) | Cohen’s d |
| Social Support (SPS-M) | 3.60 | 0.40 | 3.54 | 0.44 | −2.28* | −0.14 |
| Quality of Life (FLIC) | 5.07 | 0.84 | 5.90 | 0.74 | 13.49** | 1.05 |
| Adjustment to Illness (PAIS-M) | 2.82 | 0.34 | 2.97 | 0.37 | 6.49** | 0.42 |
| Psychological Symptoms (BSI) | 0.20 | 0.32 | 0.29 | 0.36 | −5.67** | −0.26 |
Note. N = 154. SPS-M = Social Provisions Scale-Modified, FLIC = Functional Living Index – Cancer, PAIS-M = Psychological Adjustment to Illness Scale-Modified, BSI = Brief Symptom Inventory. All measures except BSI are scaled so that higher scores indicate better adjustment.
p < .01
p < .05
Because the cancer stage of women varied considerably, one-way ANOVAs were conducted to determine whether this variable should be controlled in subsequent analyses. Due to their relatively small numbers the five women with Stage IV disease were combined with the 17 who were diagnosed with Stage III cancer to create a single Stage III/IV group. No significant differences were found across groups for social support at Time 1, F(3,150) = 1.05, p = .37; or Time 2, F(3,150) = 0.12, p = .95. No significant differences were found for psychological symptoms (BSI) at Time 1, F(3,150) = 0.97, p = .41; or Time 2, F(3,150) = 1.94, p = .14. However, quality of life (FLIC) was significantly different across cancer stage groupings at Time 1, F(3,150) = 3.52, p < .05; and Time 2, F(3,150) = 3.22, p < .05; as was adjustment to illness (PAIS-M) at Time 1, F(3,150) = 3.48, p < .05; and Time 2, F(3,150) = 5.29, p < .01. Scheffe post hoc tests suggested that these differences were due to significantly lower adjustment of State III / IV women relative to Stage I, and significant lower adjustment of women in Stage II women relative to those in Stage I. Consequently, cancer stage was controlled in subsequent analyses. Finally, to check for possible confounding effects, the length of the interval between Time 1 and 2 was correlated with all Time 2 variables. None of these relationships were significant, rs < .09.
Testing the Threshold Model
Although social support and outcome variables were significantly skewed, our hypothesis about threshold effects of social support depended on the shape of the distribution. Therefore, transformation of these data to achieve a normal distribution would not be appropriate for testing this hypothesis. Hierarchical multiple regression was used to test for a nonlinear relationship between social support and outcomes. Because FLIC and PAIS-M scores were highly correlated at Time 1 (r = .74) and Time 2 (r = .73), to reduce the number of analyses they were standardized and combined to form a single index of adjustment to cancer. Psychological symptom (BSI) scores were retained as a separate outcome because the correlations were lower (rs ranged from .47 to .69), and because unlike PAIS-M and FLIC scores, BSI scores did not improve over time.
Results are shown in Table 3. In the first two analyses Time 1 scores for one of the outcome variables, adjustment to illness or psychological symptoms, served as the criterion variable. Similarly, in the last two analyses Time 2 outcome variables served as the criteria. Following a procedure suggested by Cohen, Cohen, West, and Aiken (2003), social support scores were centered to reduce multicollinearity. Cancer stage was entered as a control variable in the first step, and social support was entered in the second step of each analysis to account for the linear relationship. In the third step, the square of centered SPS-M scores was entered to test for a curvilinear relationship. A significant increment in R2 for the final step provides evidence of a nonlinear relationship. Results shown in Table 3 indicate a significant nonlinear relationship between social support and psychological symptoms at both Time 1 and Time 2, and for the adjustment composite (FLIC/PAIS-M) at Time 2, but not Time 1. Thus, three of the four analyses were consistent with a threshold model. The R2 increment in these three analyses was substantial, ranging from .04–.05.
Table 3.
Multiple Regression Analysis of Threshold Model of Social Support
| Adjusted | Delta | F | |||
|---|---|---|---|---|---|
| R | R2 | R2 | R2 | changea | |
| Analysis A: Time 1 adjustment (FLIC/PAIS-M composite) | |||||
| 1. Cancer stage | .22 | .05 | .04 | .05 | 7.26** |
| 2. SPS-M | .37 | .14 | .13 | .09 | 13.68** |
| 3. SPS-M2 (second order) | .37 | .14 | .12 | .00 | 0.04 |
| Analysis B: Time 1 psychological symptoms (BSI) | |||||
| 1. Cancer stage | .05 | .00 | .00 | .00 | 0.38 |
| 2. SPS-M | .36 | .13 | .12 | .13 | 21.88** |
| 3. SPS-M2 (second order) | .42 | .17 | .15 | .04 | 6.90** |
| Analysis C: Time 2 adjustment (FLIC/PAIS-M composite) | |||||
| 1. Cancer stage | .16 | .03 | .02 | .03 | 4.06* |
| 2. SPS-M | .49 | .24 | .23 | .21 | 41.38** |
| 3. SPS-M2 (second order) | .52 | .27 | .26 | .04 | 7.69** |
| Analysis D: Time 2 psychological symptom s (BSI) | |||||
| 1. Cancer stage | .05 | .00 | .00 | .00 | 0.44 |
| 2. SPS-M | .48 | .23 | .22 | .23 | 44.47** |
| 3. SPS-M2 (second order) | .53 | .28 | .26 | .05 | 9.71** |
Note. N = 149. SPS-M = Social Provisions Scale-Modified (without Opportunity for Nurturance subscale), BSI = Brief Symptom Inventory, PAIS-M = Psychological Adjustment to Illness Scale - Modified, FLIC = Functional Living Index – Cancer,
df = (1,147) for Step 1, df = 1,146 for Step 2, df = 1,145 for Step 3).
p < .05
p < .01
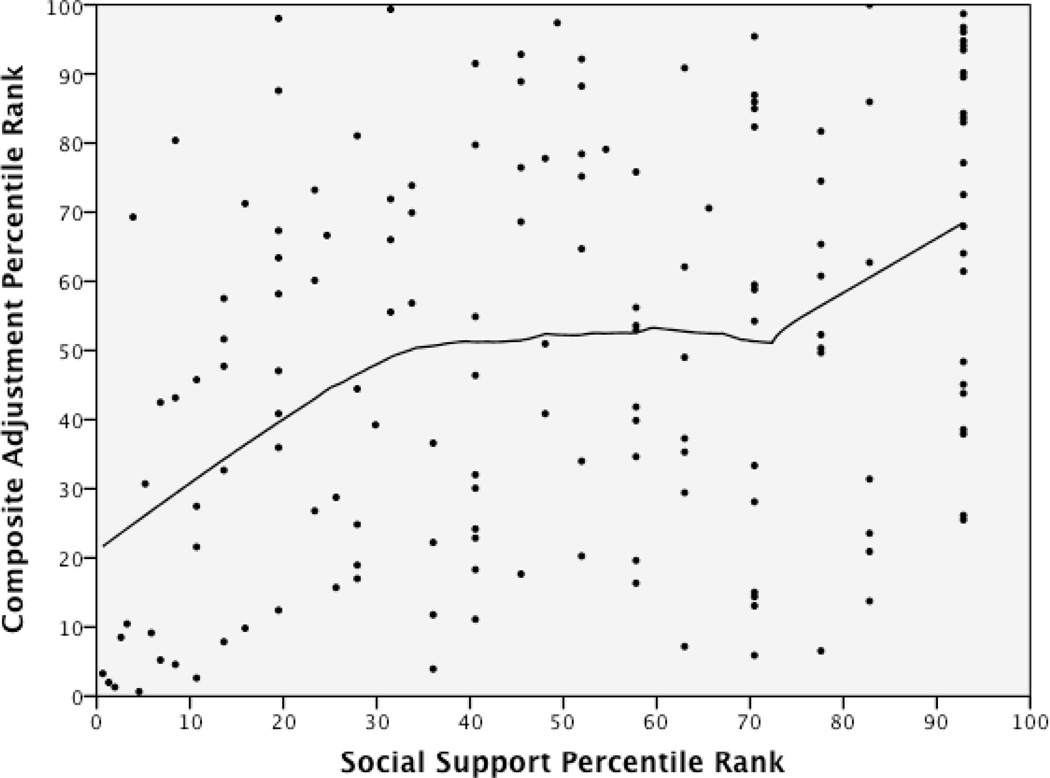
To further investigate the specific form of a nonlinear regression, Cohen et al. (2003, p. 198) suggest fitting a locally weighted scatterplot smoothing (LOWESS) curve to the data. This nonparametic procedure fits a polynomial (usually of the first or second order) to a moving subset of data using a locally weighted least squares criterion. The LOWESS curve is a data smoothing procedure similar to a moving average, except that instead of the arithmetic mean and equal weighting of every point in the “bandwidth” for the moving average, a polynomial regression is calculated with relatively higher weight assigned to the nearest neighbor data points in the subset (Cleveland & Devlin, 1988). SPSS version 19.0 was used to produce Figure 2, using a bandwidth smoothing parameter of .50 (i.e. 50% of the data were used in calculating the local polynomial regression for each data point). Social support is graphed on the x-axis, with composite adjustment (FLIC/PAIS-M) on the y-axis. Both variables were converted to percentile ranks before graphing to spread the scores along the entire axes. Figure 2 shows the curve corresponding to Analysis C from Table 3, that is, social support and composite adjustment at Time 2. (LOWESS curves based on the other two significant analyses from Table 3 appear quite similar, and are not presented). In all three cases the curves slope upward until about the 25th percentile of social support. This level of support marks a threshold above which the relationship between support and overall adjustment starts to markedly flatten. Between the 25th and 75th percentiles of support the curve is essentially flat. The 25th percentile corresponds to an SPS-M score at Time 1 of 3.37, and at Time 2 of 3.27. Table 4 shows correlations of social support with composite adjustment and psychological symptoms at Time 1 and Time 2 for the total sample, for the top three quartiles, and for the bottom quartile of social support. These results show that the significant correlations observed in the total sample can be accounted for almost entirely by women in the lowest quartile of support.
Figure 2.
Time 2 composite adjustment as a function of perceived social support.
Table 4.
Correlations between Adjustment and Social Support by Social Support Quartile
| Adjustment to Illness | Psychological Symptoms | |
|---|---|---|
| Social Support Quartile | FLIC/PAIS-M Composite | BSI |
| Time 1 | ||
| Total sample (N = 154) | .29** | −.26** |
| Highest three quartiles (n = 116) | .04 | .01 |
| Lowest quartile (n = 38, SPS-M ≤ 3.37) | .16 | −.23 |
| Time 2 | ||
| Total sample (N = 154) | .47** | −.44 |
| Highest three quartiles (n = 114) | .17 | −.17 |
| Lowest quartile (n = 40, SPS-M ≤ 3.27) | .59** | −.40* |
Note. Quartile cutting scores are for the Social Provisions Scale – Modified, (i.e., excluding the Opportunity for Nurturance subscale). Cutoff scores did not fall exactly at the 25% point due to tied scores.
p < .05
p < .01
Although these results are generally quite consistent with the threshold model, one unexpected finding that can be seen in Figure 2 is the resumption of an upward trend beginning at about the 75th percentile of support. (This pattern is evident in all three significant curvilinear plots). The threshold model predicts an increasingly flattened curve after the threshold point, as shown in Figure 1. Finally, although the ANOVA analyses indicated there was no difference in social support by cancer stage, perhaps women below the threshold we identified (i.e. in the lowest quartile) might be overrepresented in a particular cancer stage. Chi-square analysis suggested that women in the lowest quartile of support were represented in the same proportion as the other three quartiles of women in each of the cancer stages, chi-square (df = 4, N = 154) = 1.56, p = 0.82.
Discussion
The purpose of this study was to explore a threshold model of social support that contrasts with the linear assumptions typical of most social support research. The linearity assumption holds that each unit increase of support is associated with a corresponding increase in adjustment (or decrease in symptoms) across the full range of scores in the social support measure. Instead, we proposed that only at the lowest ranges of perceived social support does each added increment correspond to large increments in adjustment (or decreases in symptoms). We hypothesized a threshold, or point of diminishing returns beyond which additional increments of perceived support correspond to little, if any, benefit. The threshold model was supported in three different approaches to data analysis. First, results of hierarchical multiple regression analyses suggested a significant non-linear association for social support with adjustment to illness and psychological distress at Time 2, and with psychological distress at Time 1. Second the three LOWESS curves corresponding to these three significant hierarchical regression analyses conform to the general shape we expected, especially for the range of support scores below the 75th percentile. The example shown in Figure 2 exhibits the marked flattening we expected after the threshold value of support is reached. Finally, analyses comparing the lowest quartile of support to the top three quartiles suggest that at both Time 1 and Time 2 almost all of the significant support-adjustment or support-distress association in the full sample is accounted for by women in the lowest quartile of support. In general for the top three quartiles combined, social support is essentially unrelated to adjustment.
Thus, this study provided very strong support for the threshold model. In fact, the only quantitative analysis that failed to support the model involved adjustment to illness (composite PAIS-M and FLIC) at Time 1. Breast cancer patients within one month of diagnosis have probably had far too little time to adjust to their illness, and thus perhaps it is not surprising that a threshold effect of support does not appear in connection with adjustment to illness until Time 2. These findings underscore the importance of assessing both positive adjustment to illness and psychological distress, because these are not merely opposite poles of the same continuum. Clearly, results of this study suggest that adjustment to illness shows the greatest improvement from Time 1 to Time 2.
Although very little research has explored threshold or “dose-response” effects of social support, the findings of this study are broadly consistent with the three studies that have been conducted (Ceria et al., 2001; Silverstein et al., 1996; Jordan Varvel et al., 2007). In the most relevant of these, Jordan Varvel et al. reported a threshold effect that appeared at the median in their sample of firefighters, and the effect was observed for only one type of social support assessed by the SPS, namely, Reassurance of Worth. These differences in findings highlight the importance of inspecting plots such as the LOWESS curve shown in Figure 2 to pinpoint the threshold value for a particular sample experiencing a specific type of stressful life event. The reemergence of an upward trend in these curves at the 75th percentile of support was not expected. It may be due to a combination of response bias and ceiling effects. At Time 1, 27% of the women reported one of the three highest possible SPS-M mean scores (4.0, 3.95, or 3.90). At Time 2, 26% of the women reported one of these three scores. These women may have had a tendency to use the extremes of any response scale, and to describe both their support and functioning in very favorable terms.
Unfortunately, the data we collected do not allow us to determine the degree to which perceptions of women below the threshold are due to merely the absence of support, or due also to the presence of conflicted, unsupportive relationships. Recent studies highlight the importance of the latter possibility. A daily diary study reported “reverse buffering effects” for social support from breast cancer patients’ partners. For women with the highest levels of concerns about emotional and physical issues, compared to women with lower levels of concerns, the association between support from partner and desirable outcomes was weaker (Gremore et al., 2011). A growing body of research points to the breast cancer survivor’s partner as both a source of support and an additional source of stress that can harm adjustment (e.g., Berg & Upchurch, 2007; Coyne & Anderson, 1999; Manne et al., 1997).
A number of important limitations in this study must be acknowledged. The sample was highly rural and was overwhelmingly European American in ethnicity. Thus, generalizability is limited for populations of breast cancer patients with different demographic characteristics. A number of contextual factors such as insurance coverage, the number of dependants requiring a patient’s care, and her prognosis may have interacted with social support, adjustment and distress. None of these contextual factors were assessed in this study, but qualitative studies highlight the importance of these factors, and underscore the disparities in health care services and outcomes experienced by ethnic minority breast cancer patients (Ashing-Giwa et al., 2004; Buki et al., 2008; Galvan, Buki, & Garces, 2009). All patients were volunteers. Those who learned about the research from waiting room flyers were self-selected, and it is impossible to know the number who learned about the study but decided not to participate. The follow-up period was 8–16 months. It remains unclear whether the tentative conclusions based on these data will continue over longer periods. Using data that are highly skewed (positively for psychological distress, negatively for social support and adjustment) violates important statistical assumptions for regression and MANOVA. Nevertheless, we could not perform transformations because the basic hypotheses of this study concerned the shape of the distribution. Strengths of this study included its longitudinal design and low attrition rate between Time 1 and Time 2 data collections.
Future Research
Threshold effects using the Social Provisions Scale have now been observed in two quite different samples, the current study of women after treatment for breast cancer and a study of male firefighters (Jordan Varvel et al., 2007). More research is needed to explore threshold effects in other samples of breast cancer patients, as well as groups of men and women experiencing various stressors. We suggest archival social support data should be reanalyzed to look for nonlinear relationships that were not examined previously, and that researchers planning new studies of social support consider the possibility of threshold effects. The SPS is by far the most widely used self-report measure of social support, but perhaps a revision or expansion of items is needed to address potential problems with ceiling effects, and to directly assess the presence of unsupportive, conflicted relationships.
The basis for the modest but statistically significant decline in perceived social support we observed over the year between Time 1 and Time 2 should be explored further. Perhaps after an initial outpouring of support following a woman’s diagnosis and early treatment, a decline is inevitable, because few social networks can sustain this high level of support. Alternatively, the decline may represent withdrawal and distancing of friends and family from cancer patients, which previous research has found to be detrimental (Manne et al., 2003). It is clear that the coping challenges for many breast cancer survivors continue for many years after their treatment has been completed (Armer, 2005). A longitudinal study identified four distinct trajectories of change and adjustment in breast cancer patients (Henselmans et al., 2010). One of the four groups, representing about 15% of the sample, in contrast to the other three groups, exhibited chronically high distress at each measurement point. Unfortunately, perceived support was not assessed in this study, but a low sense of personal mastery was the feature that distinguished this group from the other three. Research is needed to investigate the role of social support and social competencies in these trajectories of adjustment.
New studies should be planned not only as investigations of the affirmative benefits of support but, by attending to the full implications of a significant correlation between adjustment and support, also as studies of the detrimental effects of a lack of social support. Similarly, studies are needed of persons who are undergoing the same stressful life circumstances, comparing those in the lowest and highest range of the distribution of perceived support to determine whether they represent extremes of the same continuum, or are qualitatively different in some critical respect. Investigators must guard against making the three potentially faulty measurement assumptions described by Reynolds and Perrin (2004): (a) not all items in an instrument assess types of support that are valued by a particular individual, (b) not all persons who provide support have uniformly beneficent intentions toward the recipient, and (c) providers and recipients do not always agree on what constitutes helpful support. To these three the current study adds a fourth caution: (d) do not assume that support and adjustment have a linear relationship.
Implications for Counseling and Health Care
The findings of this study require confirmation in future studies, but the results do offer some tentative suggestions about how to structure interventions. It appears that breast cancer patients with perceived social support in approximately the lowest quartile may benefit from interventions designed to increase social support. Women above this threshold would not be harmed by receiving the same intervention, but our results suggest that they are unlikely to experience a similar level of benefit. From a resource management standpoint, the findings of this study suggest that interventions targeted at women in the lowest range of perceived support may be more cost effective than a generic social support strategy aimed at all patients. Evidence from a randomized clinical trial of breast cancer patients assigned to two different support group interventions suggested that women who initially reported high support from their partners were not helped by information-focused support groups and may have actually been harmed by the emotion-focused support variant of the intervention (Bolger, Foster, Vinokur, & Ng, 1996). In contrast, women who lacked support from their partners appeared to benefit equally from information and emotion-focused support; thus, it can be an inefficient use of resources to offer the same type of support-based intervention to all breast cancer patients. A previous study of some of the same patients who participated in this study found that problem-solving style, especially personal control, was associated with emotional adjustment, but not with adaptation to illness at Time 2 <<citation to current authors>>. Further studies are needed to answer the “what works for whom” question with respect to effective psychosocial interventions (c.f. Helgeson, Cohen, Schultz, & Yasko, 2000).
Even if only one generic version of the support group is available but multiple meeting times are offered, it might be wise to cluster women with similar profiles of social support needs into the same group, to the extent possible. We strongly suggest that contextual factors be considered if multiple groups can be offered, such as the availability of health insurance and other forms of tangible support, as well as the presence of a supportive partner. The optimal matching model of social support (Cutrona & Russell, 1990) holds that different types of support are not interchangeable. For example, patients who lack support from their partner may not be helped by an informative presentation on ways of maintaining good nutrition during chemotherapy – although this presentation may be exactly what a different patient needs. Different types of support may have different thresholds, or no threshold at all (Jordan Varvel, 2007). Because individual needs for particular types of support are likely to be somewhat idiosyncratic, an effective strategy might be to build into every psychoeducational group a module to teach patients about the social provisions matching model, together with specific strategies and associated skills for recruiting each type of support. An important general principle is to design groups that meet the needs of the whole person, not only her health-related concerns.
Supplementary Material
Acknowledgments
This research was supported by the National Institutes of Health, grant 1 R01 NR05342-01 and the University of Missouri PRIME fund (Armer: PI), as well as funds from the University of Missouri, Ellis Fischel Cancer Center. The authors wish to thank Julie Peterson, Robin Shook, Dr. Bob Stewart, and Dr. Richard Madsen for data set and biostatistical assistance and the other members of the Lymphedema Research team including research nurses, research assistants, and clinical collaborators at Ellis Fischel Cancer Center and, most importantly, the breast cancer survivors participating in this study.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/cou
None of the authors have a financial or other conflict of interest that might potentially bias the reporting of these results.
Unlike the other five SPS subscales, Opportunity for Nurturance assesses support provided by the patient to others. Some research suggests that this type of support is unrelated to perceptions of stress (Jordan Varvel et al., 2007), and may be positively linked to psychological distress, especially for women (Mallinckrodt, 1989). In cancer patients high Opportunity for Nurturance may indicate one or more relationships that require more support from the patient than she receives in return. Because lack of support reciprocity has been linked to poor adjustment in chronic illness (Berg & Upchurch, 2007), we expected that Opportunity for Nurturance would not be beneficial. In supplemental tables available at this online link ________ correlations between SPS subscales and adjustment at Time 1 and Time 2 are shown. These results confirm our decision to exclude Opportunity for Nurturance data in this study. The subscale was not significantly related to any of the three indicators of adjustment or distress at either time point, whereas each of the other SPS subscales was significantly linked to positive outcomes.
Contributor Information
Brent Mallinckrodt, Department of Psychology, University of Tennessee.
Jane M. Armer, Sinclair School of Nursing, University of Missouri
P. Paul Heppner, Department of Educational, School, and Counseling Psychology, University of Missouri.
References
- American Cancer Society. Cancer facts and figures 2011. New York: American Cancer Society; 2011. [Google Scholar]
- Armer JM. The problem of post-breast cancer lymphedema: Impact and measurement issues. Cancer Investigation. 2005;23:76–83. [PubMed] [Google Scholar]
- Ashing-Giwa KT, Padilla G, Tegero J, Kraemer J, Wright K, Coscarelli A, Clayton S, Williams I, Hills D. Understanding the breast cancer experience of women: A qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho-Oncology. 2004;13:408–428. doi: 10.1002/pon.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Bettencourt BA, Schlegel RJ, Talley AE, Molix LA. The breast cancer experience of rural women: A literature review. Psycho-Oncology. 2007;16:875–887. doi: 10.1002/pon.1235. [DOI] [PubMed] [Google Scholar]
- Bolger N, Foster M, Vinokur AD, Ng R. Close relationships and adjustment to a life crisis: The case of breast cancer. Journal of Personality and Social Psychology. 1996;70:284–294. doi: 10.1037//0022-3514.70.2.283. [DOI] [PubMed] [Google Scholar]
- Buki LP, Garces DM, Hinestrosa MC, Kogan L, Carrillo IY, French B. Latina breast cancer survivors’ lived experiences: Diagnosis, treatment, and beyond. Cultural Diversity and Ethnic Minority Psychology. 2008;14:163–167. doi: 10.1037/1099-9809.14.2.163. [DOI] [PubMed] [Google Scholar]
- Ceria CD, Masaki KH, Rodriguez BL, Chen R, Yano K, Curb JD. The relationship of psychosocial factors to total mortality among older Japanese-American men: The Honolulu Heart Program. Journal of the American Geriatric Society. 2001;49:725–731. doi: 10.1046/j.1532-5415.2001.49148.x. [DOI] [PubMed] [Google Scholar]
- Cleveland WS, Devlin SJ. Locally-weighted regression: An approach to regression analysis by local fitting. Journal of the American Statistical Association. 1988;83:596–610. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Coyne JC, Anderson KK. Marital status, marital satisfaction, and support processes among women at high risk for breast cancer. Journal of Family Psychology. 1999;13:629–641. [Google Scholar]
- Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors. Advances in personal relationships. Greenwich, CT: JAI Press; 1987. pp. 37–67. [Google Scholar]
- Cutrona CE, Russell DW. Type of social support and specific stress: Toward a theory of optimal matching. In: Sarason BR, Sarason IG, Pierce GR, editors. Social support: An interactive view. New York: Wiley; 1990. pp. 319–366. [Google Scholar]
- Derogatis LR. The Psychosocial Adjustment to Illness Scale (PAIS) Journal of Psychosomatic Research. 1986;33:77–91. doi: 10.1016/0022-3999(86)90069-3. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. The brief symptom inventory (BSI): Administration, scoring and procedures manual. 3rd Ed. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Derogatis LR, Derogatis MF. The Psychosocial Adjustment to Illness Scale: Administration, scoring, and procedures manual-II. Towson, MD: Clinical Psychometric Research; 1990. [Google Scholar]
- Derogatis LR, Spencer PM. The brief symptom inventory (BSI) administration, scoring and procedures manual-I. Baltimore: Johns Hopkins University School of Medicine; 1982. [Google Scholar]
- Drageset S, Lindstrom TC. The mental health of women with suspected breast cancer: The relationship between support, anxiety, coping and defense in maintaining mental health. Journal Psychiatric and Mental Health Nursing. 2003;10:401–409. doi: 10.1046/j.1365-2850.2003.00618.x. [DOI] [PubMed] [Google Scholar]
- Ellison CG, Krause NM, Shepherd BC, Chaves MA. Size, conflict and opportunities for interaction: Congregational effects on members’ anticipated support and negative interaction. Journal for the Scientific Study of Religion. 2009;48:1–15. [Google Scholar]
- Figueiredo MI, Fries E, Ingram KM. The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psychooncology. 2004;13:96–105. doi: 10.1002/pon.717. [DOI] [PubMed] [Google Scholar]
- Galvan N, Buki LP, Garces DM. Suddenly a carriage appears: Social support needs of Latina breast cancer survivors. Journal of Psychosocial Oncology. 2009;27:361–382. doi: 10.1080/07347330902979283. [DOI] [PubMed] [Google Scholar]
- Gremore TM, Baucom DH, Porter LS, Kirby JS, Atkins DC, Keefe FJ. Stress buffering effects of daily spousal support on women’s daily emotional and physical experiences in the context of breast cancer concerns. Health Psychology. 2011;30:20–30. doi: 10.1037/a0021798. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Cohen S, Schultz R, Yasko J. Group support interventions for women with breast cancer: Who benefits from what? Health Psychology. 2000;19:107–114. doi: 10.1037//0278-6133.19.2.107. [DOI] [PubMed] [Google Scholar]
- Henselmans I, Helgeson VS, Seltman H, de Vries J, Sanderman R, Ranchor AV. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychology. 2010;29:100–108. doi: 10.1037/a0017806. [DOI] [PubMed] [Google Scholar]
- Holland KD, Holahan CK. The relation of social support and coping to positive adaptation to breast cancer. Psychology & Health. 2003;18:15–29. [Google Scholar]
- Koopman C, Hermanson K, Diamond S, Angell K, Spiegal D. Social support, life stress, pain and emotional adjustment to advanced breast cancer. Psychooncology. 1998;7:101–111. doi: 10.1002/(SICI)1099-1611(199803/04)7:2<101::AID-PON299>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- Jordan Varvel S, He Y, Shannon JK, Tager D, Bledman RA, Chaichanasakul A, Mendoza MM, Mallinckrodt B. Multidimensional, threshold effects of social support in firefighters: Is more support invariably better? Journal of Counseling Psychology. 2007;54:458–465. [Google Scholar]
- Lutgendorf SK, Sood AK, Anderson B, McGinn S, Maiseri H, Duo M, Sorosky JI, De Geest K, Ritchie J, Lubaroff DM. Social support, psychological distress, and natural killer cell activity in ovarian cancer. Journal of Clinical Oncology. 2005;23:7105–7113. doi: 10.1200/JCO.2005.10.015. [DOI] [PubMed] [Google Scholar]
- Mallinckrodt B. Social support and the effectiveness of group therapy. Journal of Counseling Psychology. 1989;36:170–175. [Google Scholar]
- Manne S, Glassman M. Perceived control, coping efficacy, and avoidance coping as mediators between spousal unsupportive behaviors and psychological distress. Journal of Health Psychology. 2000;19:155–164. doi: 10.1037//0278-6133.19.2.155. [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Sherman M, Glassman M, Ross S, Goldstein L, Fox K. Buffering effects of family and friend support on associations between partner unsupportive behaviors and coping among women with breast cancer. Journal of Social and Personal Relationships. 2003;20:771–792. [Google Scholar]
- Manne SL, Taylor KL, Dougherty J, Kemeny N. Supportive and negative responses in the partner relationship: Their association with psychological adjustment among individuals with cancer. Journal of Behavioral Medicine. 1997;20:101–125. doi: 10.1023/a:1025574626454. [DOI] [PubMed] [Google Scholar]
- Merluzzi TV, Martinez Sanchez M. Perceptions of coping behaviors by persons with cancer and health care providers. Psycho-Oncology. 1997;6:197–203. doi: 10.1002/(SICI)1099-1611(199709)6:3<197::AID-PON270>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- Nausheen B, Gidron Y, Peveler R, Moss-Morris R. Social support and cancer progression: A systemic review. Journal of Psychosomatic Research. 2009;67:403–415. doi: 10.1016/j.jpsychores.2008.12.012. [DOI] [PubMed] [Google Scholar]
- Norton TR, Manne SL, Rubin S, Hernandez E, Corlson J, Bergman C, Rosenblum N. Ovarian cancer patients’ psychological distress: The role of physical impairment, perceived unsupportive family and friend behaviors, perceived control, and self esteem. Journal of Health Psychology. 2005;24:143–152. doi: 10.1037/0278-6133.24.2.143. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, van Tilburg TA, Boeke JP, Deeg DJH, Kriegsman DMW, van Eijk JTM. Effects of social support and personal coping resources on depressive symptoms: Different for various chronic diseases. Journal of Health Psychology. 1998;17:551–558. doi: 10.1037//0278-6133.17.6.551. [DOI] [PubMed] [Google Scholar]
- Reynolds JS, Perrin NA. Mismatches in social support and psychosocial adjustment to breast cancer. Journal of Health Psychology. 2004;23:425–430. doi: 10.1037/0278-6133.23.4.425. [DOI] [PubMed] [Google Scholar]
- Roberts KJ, Lepore SJ, Helgeson V. Social-cognitive correlates of adjustment to prostate cancer. Psycho-Oncology. 2006;15:183–192. doi: 10.1002/pon.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schipper H, Clinch J, McMurray A, Levitt M. Measuring the quality of life of cancer patients: the functional living index- cancer: development and validation. Journal of Clinical Oncology. 1984;5:472–483. doi: 10.1200/JCO.1984.2.5.472. [DOI] [PubMed] [Google Scholar]
- Schuster TL, Kessler RC, Aseltine RH. Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology. 1990;18:423–438. doi: 10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- Shell JA, Carolan M, Zhang Y, Meneses KD. The longitudinal effects of cancer treatment on sexuality in individuals with lung cancer. Oncology Nursing Forum. 2008;32:73–79. doi: 10.1188/08.ONF.73-79. [DOI] [PubMed] [Google Scholar]
- Silverstein M, Chen X, Heller K. Too much of a good thing? Intergenerational social support and the psychological well-being of older parents. Journal of Marriage & the Family. 1996;58:970–982. [Google Scholar]
- Schlomer GL, Bauman S, Card N. Best practices for missing data management in counseling psychology. Journal of Counseling Psychology. 2010;57:1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. Needham Heights, MA: Allyn & Bacon; 2007. [Google Scholar]
- Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RAR, Updegraff JA. Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review. 2000;107:441–429. doi: 10.1037/0033-295x.107.3.411. [DOI] [PubMed] [Google Scholar]
- Uchino BN, Cacioppo JT, Keicolt-Glaser JK. The relationship between social support and physiological processes: A review with emphasis on underlying mechanisms and implications for health. Psychological Bulletin. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- Walsh SR, Manuel JC, Avis NE. The impact of breast cancer on younger women’s relationship with their partner and children. Families, Systems & Health. 2005;23:80–93. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.