Summary
Transvenous occlusion of an affected sinus has become a standardized curative treatment for dural sinus arteriovenous fistula. A 57-year-old man with a left sigmoid sinus isolated dural AVF was successfully treated with tansarterial followed by transvenous embolization. Follow-up angiography one year and two months thereafter showed complete disappearance of the dural AVF. However, one year later, superior parasagittal sinus dural arteriovenous fistula had newly developed, for which the etiology and a careful point for follow-up are here discussed.
Key words: etiology, dural arteriovenous fistula, superior saggital sinus, transvenous embolization
Introduction
Transvenous embolization (TVE) may be an affective treatment for dural AVFs associated with dural sinus 1,2. On the other hand, in regard to the occurrence of dural AVF chronic venous hypertension is essential factor. However, for dural AVF patients with complete occlusion defined by angiography, insufficient attention may have been paid to venous pressure.
Case Report
A 57-year-old man who felt dizziness only after putting on swimming cap underwent examination after entering brain dock and was referred to our hospital. Neurological examination showed no abnormal findings, but bruit was evident at left sided posterior auricular portion. Angiography revealed an isolated dural arteriovenous fistula (AVF) in the left sigmoid sinus (figure 1). Cortical venous reflux was remarkable. Initially transarterial embolization for the left occipital and middle meningeal arteries was performed, then TVE was tried, but conventional access to the lesion from the confluence via contralateral sinus and also the left internal jugular vein failed because of interference of the rigid thrombus. The external jugular vein participated as draining vein, but severe stenosis interfered with advancement of the catheter. Therefore, direct puncture to the left external jugular vein beyond the stenosis was performed under road mapping, which was successful (figure 2) and the dural AVF could be completely occluded with platinum coils.
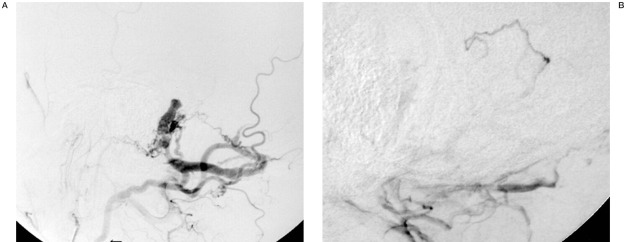
Figure 1.
Left external carotid angiogram (lateral view) A) Early phase and B) late phase) showing an isolated dural AVF in the sigmoid sinus, draining into cortical vein and left external jugular vein via the deep cervical vein. The proximal part of the left jugular vein is tortuous and narrow (arrow).
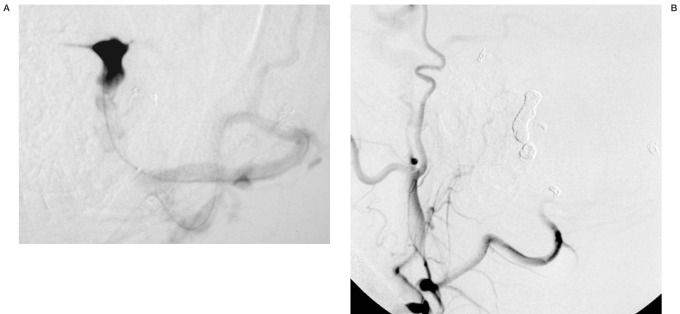
Figure 2.
A) Venogram (lateral view) of the isolated sinus achieved by direct puncture of the left external jugular vein beyond the narrowing part. B) A left external carotid angiogram after transvenous embolization.
Follow-up angiography one year and two months after the treatment showed disappearance of the dural AVF (figure 3). Thereafter, he started weight training without informing his chief physician. One year after beginning training, he suffered a headache and blurred vision and was again admitted to our hospital. Angiography showed persistent disappearance of the previously treated dural AVF at the left transverse-sigmoid sinus, but a dural AVF at the para-superior sagittal sinus (SSS) had newly developed (figure 4). SSS was present defined by a right internal carotid angiogram. Transarterial embolization for the right occipital artery and left superficial temporal artery was performed because the superior sagittal sinus was patent.
The patient rejected open surgery and was followed conservatively in our outpatient clinic. Follow-up MRA showed gradual decrease of the dural AVF and his headaches are decreasing without blurred vision.
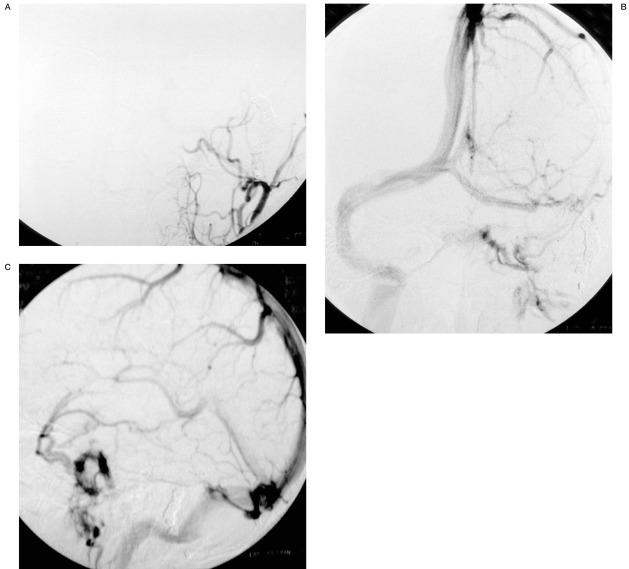
Figure 3.
Follow-up left external carotid angiograms (anterior-posterior view) A) artertial phase, B) venous phase) (lateral view) C) venous phase) one year and two months after the TVE showing persistent disappearance of the dural AVF.
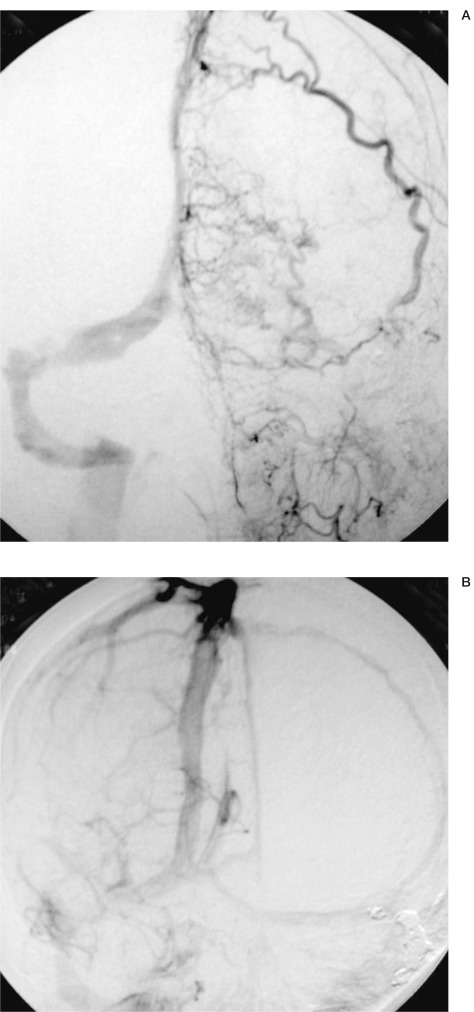
Figure 4.
A:) A left external carotid angiogram showing persistent disappearance of the previously treated dural AVF at the left sigmoid sinus and a newly developed dural AVF at the superior sagittal sinus supplied by the left superficial temporal artery. B) A right internal carotid angiogram (venous phase), showing left transverse sinus and superior sagittal sinus.
Discussion
Houser et Al 3 first reported two cases of transverse dural arteriovenous malformation as an acquired lesion, one one year and the other four years after angiographic demonstration of sigmoid or transverse sinus occlusion. Subsequently, Chaundary et Al 4 reported four acquired dural AVFs, from three weeks to three years after trauma, with sinus thrombosis in two out of the four and skull fracture in the other two.
Dural AVFs not associated with dural sinus, injury or/and skull fracture, may develop in the process repair of the dura mater and links with dural sinus thrombosis are frequently recognized. Some authors 5-7 have proposed a pathogenesis involving second dural AVF development in the recanalizing process with stagnating venous outflow and thrombosis of efferent venous structure due to the first dural AVF. On the other hand, Terada et Al 8 from an experimental study, concluded that chronic venous hypertension of two to three months duration, without associated venous or sinus thrombosis, can induce new AVF's affecting the dural sinuses. In the present case also, thrombosis of the SSS was not demonstrated. Dural AVFs may develop with addition of some factors, but venous hypertension may be the main cause of development of dural AVF associated with dural sinus.
The underlying mechanism can be explained in terms of pre-existing anastomotic channels (physiologic AV shunts) in the dura mater 9,10 which are tiny vascular channels in normal condition, but become opened and dilated to compensate for venous hypertension.
With reports of multiple dural AVF 7,11-17, the majority are located on the same side, including a high frequency of SSS, which is very interesting with regard to the pathogenesis. Barnwell et Al. 5 reported seven patients with multiple fistulas associated with venous obstruction. Disturbance of the venous circulation and hypertension have been suggested as essential factors for dural AVF development, especially when locating far from sinus occlusion, with or without thrombosis. Halbach et Al 13 reported SSS dural AVF to be comparatively rare (7/65:11%) in dural AVFs, a direct contribution of direct head injury and thrombosis being evident in three of seven. The present case suffered no head injury or sinus thrombosis and the occurrence was more than two years after occlusion with left sigmoid sinus coil embolization. Newly developed dural AVF of SSS were at a distance from the occluded sinus.
Some dural AVFs occur with remarkable predominance. For example, dural AVFs of the cavernous sinus occur predominantly in women, especially in post-menoposal cases or in comparative young adults after abortion or delivery. Decrease in female hormone levels might be related to the development of dural AVF in the cavernous sinus 18. Anterior fossa dural AVFs, in contrast, show a remarkable male dominance, and occur without sinus occlusion and injury. The etiology is unknown, but sex hormone might again be related. The other major dural AVFs occur with no remarkable sex bias.
TVE may be an effective treatment for dural AVFs localized in the sinus, paticulary with regard to aggressive lesions featuring cortical venous reflux 1,2, but for patient with complete occlusion defined by angiography, insufficient attention may have been paid to venous pressure. New development of dural AVF after TVE for dural AVF has been reported 19-24 (Table 1). Time until new developments after sinus packing is reported to be range from four months to 30 months (average: ten months). All except one case 24 developed after cavernous sinus packing for dural AVF or direct fistula.
Table 1.
Literature review of new development of dural AVF after endovascular sinus packing for dural AVF.
| Autors Year |
Patient Age (yrs), Sex |
Initial dural AVF |
Approach route |
Newly developed dural AVF |
Months until fistula development |
|---|---|---|---|---|---|
| Nakagawa et al, 1992 |
43, F | lt CC | lt SOV | lt TS | 6 |
| Yamashita et al, 1993 |
54, F | lt CC | lt IPS | lt SS | 12 |
| Makiuchi et al, 1998 |
CC | lt IPS failed lt SOV | lt SS | 6 | |
| Kubota et al, 1999 |
43, F | lt CC | lt IPS | lt JB | 4 |
| Kawaguchi 1999 |
72, F | lt CC | lt IPS | lt SS | 30 |
| Kiyosue et al, 2002 |
62, M | lt paraTS | lt JV | lt SS | 5 |
| 66, F | lt CC | lt IPS failed Lt SOV | lt JB | 5 | |
| Present study | 57, M | lt TS | lt External JV | para SSS | 26 |
|
CC: cavernous sinus, SOV: superior ophthalmic vein, TS: transverse sinus, IPS: inferior petrosal vein, JB: jugular bulb, SS: Sigmoid sinus, SSS: superior sagittal sinus, JV: jugular vein *: direct fistula (tear in the vessel) | |||||
Kiyosue et Al 24 reported two cases, of which one has developed on the sigmoid sinus after transvenous embolization of a paratransverse sinus dural AVF. They mentioned that angiogenesis (expression of vascular endothelial growth factor and basic fibroblast growth factor) resulted in hypoxia due to venous hypertension as a result of venous occlusion created by the initial transvenous embolization, which might be essential for new development of a dural AVF.
Yamashita et Al 21 reported a patient newly developed sigmoid sinus dural AVF after successful TVE of a cavernous dural AVF for which they discussed the pathogenesis of second dural AVF. They argued that manipulation of a catheter and guide wire to negotiate a path to the inferior petrosal sinus may inadvertently injure the intima of the sigmoid sinus, and hence induce thrombosis, which may eventually lead to a dural AVF. All eight reported cases occurred with the transvenous route of sinus packing.
In the present case, TVE was performed via direct puncture of the external jugular vein and the catheter did not injure the para-SSS, called the accessory sinus by Piske et Al 25. They mentioned this to be one compartment of the SSS. The SSS was patent in our patient defined by internal carotid angiography. However, transvenous embolization was undergone via the ipsilateral jugular vein and contralateral transverse sinus for our isolated dural AVF. Right transverse sinus irregularity suggested thrombosis to be present on the angiogram at the time of new development of the dural AVF. Venous hypertension may be accerelated by such contralateral sinus stenosis. More likely, the weight training for one year might have been directly associated with development of the secondary dural AVF in our case.
Dehydration induced by the training or an original tendency hypercoagulability, not defined on examination, might be associated with thrombus formation.
Newton et Al 26 mentioned in five of eleven dural AVF patients that onset of the fistula may have been related to straining or heavy lifting. Especially in patients undergoing TVE, venous pressure may readily become raised, so that they should be guided to avoid straining actions such as with constipation, coughing, head standing and also lifting heavy weight. A posture to keep the head up during sleeping may also be recommended to improve the venous circulation. Anticoagulants or antiplatelet therapy may be needed for patients after TVE and in such cases careful attention should be paid long term by radiological and clinical examination.
References
- 1.Halbach VV, Higashida R, et al. Transvenous embolization of dural fistulas involving the cavernous sinus. Am J Neuroradiol. 1989;10:377–383. [PMC free article] [PubMed] [Google Scholar]
- 2.Halbach VV, Higashida RT, et al. Tranvenous embolization of dural fistulas involving the transvenous and sigmoid sinuses. Am J Neuroradiol. 1989;10:393–399. [PMC free article] [PubMed] [Google Scholar]
- 3.Houser OW, Cambell JK, et al. Arteriovenous malformation affecting the transverse dural venous sinus: an aquired lesion. Mayo Clin Proc. 1979;54:651–661. [PubMed] [Google Scholar]
- 4.Chaundary MY, Sachdev VP, et al. Dural arteriovenous malformation of the major venous sinus. Am J Neuroradiol. 1982;3:13–19. [PMC free article] [PubMed] [Google Scholar]
- 5.Barnwell ST, Halbach VV, et al. Multiple dural arteriovenous fistulas of the cranium and spine. Am J Neuroradiol. 1991;12:441–445. [PMC free article] [PubMed] [Google Scholar]
- 6.Handa J, Yoneda S, Handa H. Venous sinus occlusion with a dural arteriovenous malformation of the posterior fossa. Surg Neurol. 1975;4:433–437. [PubMed] [Google Scholar]
- 7.Kuwayama N, Takaku A, et al. Multiple dural arteriovenous malformations, report of two cases. J Neurosurg. 1989;71:932–934. doi: 10.3171/jns.1989.71.6.0932. [DOI] [PubMed] [Google Scholar]
- 8.Terada T, Higashida RT, et al. Development of acquired arteriovenous fistulas in rats due to hypertension. J Neurosurg. 1994;80:884–889. doi: 10.3171/jns.1994.80.5.0884. [DOI] [PubMed] [Google Scholar]
- 9.Aminoff MJ. Vascular anomalies in the intracranial dura mater. Brain. 1973;96:601–612. doi: 10.1093/brain/96.3.601. [DOI] [PubMed] [Google Scholar]
- 10.Kerber CW, Newton TH. The macro and microvasculature of the dura mater. Neuroradiology. 1973;6:175–179. doi: 10.1007/BF00335317. [DOI] [PubMed] [Google Scholar]
- 11.Barnwell ST, Halbach VV, et al. Dural arteriovenous fistulas involving the inferior petrosal sinus: angiographic findings in six patients. Am J Neuroradiol. 1990;11:511–516. [PMC free article] [PubMed] [Google Scholar]
- 12.Grady MS, Pobereskin L. Arteriovenous malformations of the dura mater. Surg Neurol. 1987;28:135–140. doi: 10.1016/0090-3019(87)90087-5. [DOI] [PubMed] [Google Scholar]
- 13.Graeb DA, Dolman C. Radiological and pathological aspects of dural arteriovenous fistulas, case report. J Neurosurg. 1986;64:962–967. doi: 10.3171/jns.1986.64.6.0962. [DOI] [PubMed] [Google Scholar]
- 14.Halbach VV, Higashida R, et al. Treatment of dural arteriovenous malformations involving the superior sagittal sinus. Am J Neuroradiol. 1988;9:337–343. [PMC free article] [PubMed] [Google Scholar]
- 15.Houser OW, Baker HL, et al. Intracranial dural arteriovenous malformations. Radiology. 1972;105:55–64. doi: 10.1148/105.1.55. [DOI] [PubMed] [Google Scholar]
- 16.Kataoka K, Taneda M. Angiographic disappearance of multiple dural arteriovenous malformations, case report. J Neurosurg. 1984;60:1275–1278. doi: 10.3171/jns.1984.60.6.1275. [DOI] [PubMed] [Google Scholar]
- 17.Newton TH, Weidner W, Greitz T. Dural arteriovenous malformation in the posterior fossa. Radiology. 1968;90:2735. doi: 10.1148/90.1.27. [DOI] [PubMed] [Google Scholar]
- 18.Kurata A, Miyasaka Y, et al. Spontaneous carotid cavernous fistulas with special reference to the influence of estradiol decrease. Neurol Res. 1999;21:631–639. doi: 10.1080/01616412.1999.11740988. [DOI] [PubMed] [Google Scholar]
- 19.Nakagawa H, Kubo S, et al. Shifting of dural arteriovenou malformations from the cavernous sinus to the sigmoid sinus to the transverse sinus after transvenous embolization. Surg Neurol. 1992;37:30–38. doi: 10.1016/0090-3019(92)90062-r. [DOI] [PubMed] [Google Scholar]
- 20.Yamashita k, Taki W, et al. Development of sigmoid dural arteriovenous fistulas after transvennous embolization of cavernous dural arteriovenous fistulas. Am J Neuroradiol. 1993;14:1106–1108. [PMC free article] [PubMed] [Google Scholar]
- 21.Machiuchi T, Takasaki K, et al. A case of sigmoid sinus dural arteriovenous fistula after treated cavernous dural arteriovenous fistula. Interventional Neuroradiology. 1998;4(Suppl 1):219–222. doi: 10.1177/15910199980040S145. [DOI] [PubMed] [Google Scholar]
- 22.Kubota Y, Ueda T, et al. Development of a dural arteriovenous fistula around the jugular valve after transvenous embolization of cavernous dural arteriovenous fistula. Surg Neurol. 1999;51:174–176. doi: 10.1016/s0090-3019(97)00420-5. [DOI] [PubMed] [Google Scholar]
- 23.Kawaguchi T, Kawano T, et al. Dural fistula of the transverse sigmoid sinus after transvenous embolization of the carotid cavernous fistula. Brain and Nerve. 1999;51:1065–1069. [PubMed] [Google Scholar]
- 24.Kiyosue H, Tanoue S, et al. Recurrence of dural arteriovenou fistula in another location after selective transvenous coil embolization: report of two cases. Am J Neuroradiol. 2002;23:689–692. [PMC free article] [PubMed] [Google Scholar]
- 25.Piske RL, Campos CMS, et al. Dural sinus compartment in dural arteriovenous shunts: a new angioarchitectural feature allowing superselective transvenous dural sinus occlusion treatment. Am J Neuroradiol. 2005;26:1715–1722. [PMC free article] [PubMed] [Google Scholar]
- 26.Newton TH, Hoyt WF. Dural arteriovenous shunts in the region of the cavernous sinus. Neuroradiology. 1970;1:71–81. [Google Scholar]